w w w . r b h h . o r g
Revista
Brasileira
de
Hematologia
e
Hemoterapia
Brazilian
Journal
of
Hematology
and
Hemotherapy
Original
article
Left
ventricular
hypertrophy
in
children,
adolescents
and
young
adults
with
sickle
cell
anemia
Gustavo
Baptista
de
Almeida
Faro,
Osvaldo
Alves
Menezes-Neto,
Geodete
Santos
Batista,
Antônio
Pereira
Silva-Neto,
Rosana
Cipolotti
∗UniversidadeFederaldeSergipe(UFS),Aracaju,SE,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received11March2014 Accepted2July2015 Availableonline26July2015
Keywords:
Sicklecellanemia Leftventricularfunction Leftventriculardysfunction Echocardiography
a
b
s
t
r
a
c
t
Objective:Theaimsofthisstudyweretoestimatethefrequencyofleftventricular hypertro-phyandtoidentifyvariablesassociatedwiththisconditioninunder25-year-oldpatients withsicklecellanemia.
Methods:Across-sectionalstudywasperformedofchildren,adolescentsandyoungadults withsicklecellanemiasubmittedtoatransthoracicDopplerechocardiography.Themass oftheleftventriclewasdeterminedbytheformulaofDevereuxetal.withcorrectionfor height,andthepercentilecurvesofgenderandagewereapplied.Individualswithrheumatic andcongenitalheartdiseasewereexcluded.Thepatientsweredividedintotwogroups accordingtothepresenceorabsenceofleftventricularhypertrophyandcomparedaccording toclinical,echocardiographicandlaboratoryvariables.
Results:Atotalof37.6%ofthepatientshadleftventricularhypertrophyinthissample.There wasnodifferencebetweenthegroupsofpatientswithandwithouthypertrophyaccording topathologicalhistoryorclinicalcharacteristics,exceptpossiblyfortheuseofhydroxyurea, moreoftenusedinthegroupwithoutleftventricularhypertrophy.Patientswithleft ven-tricularhypertrophypresentedlargerleftatriaandlowerhemoglobinandhematocritlevels, reticulocyteindexandahigheralbumin:creatinineratioinurine.
Conclusion:Left ventricular hypertrophy was observed in more than one-third of the youngpatientswithsicklecellanemiawiththisfindingbeinginverselycorrelatedtothe hemoglobinandhematocritlevels,andreticulocyteindexanddirectlyassociatedtoahigher albumin/creatinineratio.Itispossiblethathydroxyureahadhadaprotectiveeffectonthe developmentofleftventricularhypertrophy.
©2015Associac¸ãoBrasileiradeHematologia,HemoterapiaeTerapiaCelular.Published byElsevierEditoraLtda.Allrightsreserved.
∗ Correspondingauthorat:CampusdaSaúde,HospitalUniversitário,Av.CláudioBatista,s/n,Sanatório,49000-000Aracaju,SE,Brazil.
E-mailaddress:rosanaci@yahoo.com(R.Cipolotti).
http://dx.doi.org/10.1016/j.bjhh.2015.07.001
Introduction
Sicklecell anemia(SCA)isamultisystemicdisease charac-terizedbyacuteepisodesofpainandprogressivelesionsof targetorgans.Itisoneofthemostcommonandmostsevere monogenicdisordersintheworld.InBrazil,itisestimatedthat 3500childrenarebornwithsicklecellanemiaeachyear,thatis 1:1000livebirths,andisthusaseriouspublichealthproblem.1
Cardiovasculardiseaseisafrequentclinicalmanifestationof peoplewithsicklecellanemia.
Eccentric left ventricular hypertrophy (LVH), dilation of thechambers, biventricular dysfunction,pulmonary hyper-tensionandmyocardialischemiaaretheprincipalfindings.2–5
PatientswithSCAfrequentlyhavesevereanemiathatresults in increased cardiac output with minimal or no increase in cardiac frequency thereby causing dilatation ofthe left ventricle6 correlated to the hemoglobin (Hb) level.7,8 The
dilatedleftventricleadaptstothechronicvolumeoverloadby hypertrophy,thickeningtheheartmuscleandstretchingthe myofibrilsofthemuscle.Hypertrophyallowstheleftventricle toadapttothechronicvolumeoverload,initiallypreserving diastoliccomplianceandmaintainingthefillingpressureat normallevels.9TheliteratureshowsthatLVHisacommon
condition insickle cell anemia afterthe second decade of life.10DiagnosedbytransthoracicDopplerechocardiography,
theprevalenceofLVH varies between13 and 86%.7,10–14 In
chroniccases,LVHpresentswithdiastolic3,15,16andsystolic
dysfunction.3,15
Giventhehighmorbimortality,thepresentarticleaimed toestimatethefrequencyofLVHinchildren,adolescentsand youngadultswithsicklecellanemiaanddeterminevariables associatedtothiscondition.
Method
Studydesignandpopulation
Across-sectionalstudywasconductedofpatients between theagesof7and25withSCAasconfirmedbyelectrophoresis, regularlytreatedinareferralcenter.Allpatientswereinsteady state,andweresubmittedtooutpatienttransthoracicDoppler echocardiography.Theexclusioncriteriawerethepresenceof rheumaticorcongenitalheartdisease.Patientswere consec-utivelyenrolledandallocatedintwogroupsaccordingtothe presenceorabsenceofLVH.
TransthoracicDopplerechocardiography
Echocardiographic examinations were performed using a Nemio®XG(Toshiba)devicebyoneexperienced
echocardio-grapher. Patients were placed in the left lateral decubitus positionwithoutsedationtoperformtheechocardiographic measurementsinparasternal and apicalacoustic windows following the recommendations of the American Society ofEchocardiography.17 At leastthree cycles were analyzed
for each variable. The electrocardiographic exam was per-formed concurrently with laboratory tests. The evaluation ofthe left ventricle was obtainedusing the variables:end diastolic thickness of the interventricular septum (IVS),
end-diastolicthicknessoftheposteriorwalloftheleft ven-tricle(LVPW),left ventricularend-diastolicdiameter(LVDD) and left ventricularend-systolic diameter(LVSD). The rela-tive wallthickness(RWT) was obtainedusing the formula: RWT=(IVS+LVPW)/LVDD. The left ventricular mass index (LVMI)wascalculatedusingtheformulaproposedbyDevereux etal.18inwhich:
LVMI(g)=0.8{1.04[(IVS+LVDD+LVPW)3−3LVDD]}+0.6
Subsequentlytheresultwascorrectedfortheheight18,19and
appliedtospecificpercentilecurvesforgenderandage.20LVH
wasdiagnosedwhentheLVMIwashigherthanthe95th per-centileforgenderandage.20
Demographicandclinicaldata
Data regarding the age, gender, anthropometry (weight, height),informationregardingthediagnosis (ageat diagno-sis,electrophoresisresults),previoususeofhydroxyureaand pathological history (leg ulcers, gallstones, stroke, surgical splenectomy, priapism, acute chest syndrome, hospitaliza-tions, transfusionsand painful crisesinthe previous year) werecollectedthroughinterviewsandfrommedicalcharts.
Laboratorydata
Data on the blood count, reticulocyte index (corrected by hematocrit),lactatedehydrogenaseandtotalbilirubinlevels, ferritin,serumcreatinineandurea,albumin:creatinineratioin urineand24-hourcreatinineclearancewerecollectedduring theweekpriortotheechocardiographyinordertocorrelate themwithLVH.
Ethicalconsiderations
Thisstudy ispart ofclinicalresearch insicklecell anemia approvedbytheResearchEthicsCommitteeofthe Universi-dadeFederaldeSergipe(number0173.0.107.000-09).Patients over 18 years old and the guardians of under 18-year-old patientssignedinformedconsentforms.
Data
analysis
Theresultswere analyzedusingthe StatisticalPackagefor theSocialSciencesforWindowsversion17.0(SPSS,Chicago IL).Categoricalvariableswereanalyzedusingthechi-squared distribution or Fisher’s exact test. The Student’s t-test or Mann–Whitneytestwereusedtocomparenumericalvariables betweenthegroups.Alogisticalregressionmodelwasusedto evaluatetheprotectiveeffectofhydroxyureaafterthe elimi-nationofpossibleconfusingvariables.Thelevelofsignificance wassetforp-values<0.05.
Results
Table1–Demographicandclinicalcharacteristicsofsicklecellanemiapatientswithandwithoutleftventricular hypertrophy.
Leftventricularhypertrophy Total p-value
Yes No
Age(years) 14.07±5.55 15.60±5.70 15.03±5.67 0.17
Gender–n(%)
Male 23(41.1) 33(58.9) 56(51.4) 0.57
Female 18(34) 35(66) 53(48.6)
Ageatdiagnosis(months) 61.42±41.18 74.46±48.76 69.28±46.09 0.21
HemoglobinS(%) 80.52±15.33 83.93±11.27 82.56±13.06 0.27
HemoglobinF(%) 5.52±6.62 4.90±5.87 5.15±6.15 1.00
Ulcers–n(%) 3(7.5) 13(19.7) 16(15.1) 0.07
Cholelithiasis–n(%) 9(22.5) 27(40.9) 36(34) 0.08
Stroke–n(%) 4(10) 12(18.2) 16(15.1) 0.20
Splenectomy–n(%) 6(15) 7(10.6) 13(12.3) 0.72
Priapism–n(%) 1(4.5) 2(6.3) 3(5.6) 0.64
ACS–n(%) 23(59) 49(75.4) 72(69.2) 0.12
Hydroxyurea(yes)–n(%) 3(7.5) 16(24.2) 19(17.6) 0.02
Hydroxyurea(monthsofuse) 34.67±3.21 32.50±16.01 32.84±14.68 0.82
Hospitalizations/year 0.72±1.23 0.91±1.36 0.84±1.31 0.47
Paincrises/year 0.51±0.91 0.74±1.23 0.66±1.13 0.44
Transfusions/year 0.77±1.25 1.48±2.74 1.22±2.32 0.31
ACS:acutechestsyndrome.
patients.Themeanage,andtheproportionsofHbSandHbF weresimilarbetweenpatientswithorwithoutLVH.Themain complicationsresultingfromSCAwereacutechestsyndrome (69.2%), cholelithiasis (34%), stroke (15.1%) and leg ulcers (15.1%).Patientspresentedonaverage0.84±1.31episodesof hospitalization/yearand0.66±1.13paincrisesthatrequired hospitalization/yearandreceived1.22±2.32unitsofpacked redbloodcells/year;therewerenosignificantdifferencesin respecttothesevariables betweenthetwogroups. Hydrox-yureawascontinuouslyusedby17.6%ofthe109patients,7.5% inthegroupwithLVHand24.2%inthegroupwithoutLVH (p-value=0.02).Thedurationofhydroxyureausewassimilar betweenthetwogroups(Table1).
PatientswithLVHpresentedgreaterLVDD,LVSD,end dia-stolicthicknessoftheIVS,end-diastolicthicknessoftheLVPW andlargerdiametersoftheaorticrootandoftheleftatria. End-diastolicvolume,ejectionfractionandthesystolicshortening fractionweresimilarbetweenthetwogroups(Table2).
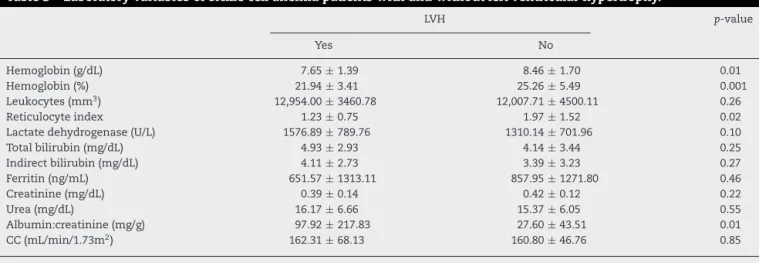
The group with LVH presented lower Hb levels (7.65±1.39g/dL vs. 8.46±1.70g/dL; p-value=0.01), hema-tocrit concentrations (21.94±3.41% vs. 25.26±5.49%;
p-value=0.001),reticulocyteindex(1.23±0.75vs.1.97±1.52;
p-value=0.02) and a higher 24-h albumin:creatinine ratio in urine (97.92±217.83mg/dL vs. 27.60±43.51mg/dL;
p-value=0.01). Hemolysis markers (lactate dehydroge-nase,indirectbilirubinandferritin)andcreatinineclearance werestatisticallysimilarinbothgroups(Table3).Thelogistic regression model did not confirm any protective effect of hydroxyureainthissample.
Discussion
LVH was present in 37.6% ofthe patients included in the study.Therewasnodifferencebetweengroupswithrespectto
clinical,demographicorpathologicalaspects,withapossible exceptionfortheuseofhydroxyurea.PatientswithLVHhada largerleftatriaindexforbodysurfaceandlowerhemoglobin and hematocrit levels, and reticulocyte index and higher 24-halbumin:creatinineratioinurine.Markersofhemolysis (lacticdehydrogenase,indirectbilirubinandferritin)and cre-atinineclearancewereuniformlyhighinbothgroups.Using echocardiography,previousstudies haveshown thatLVHis acommonconditionofSCAadults8,9withaprevalencethat
rangesbetween13and86%,avariationrelatedtothedifferent criteriausedinthestudies.7,10–14Anatomopathological
stud-ies showfrequenciesforLVHof20–100% inSCApatients.21
Sicklecelldiseasepatientshavehigherratesofleft ventricu-larmasswhencomparedtoHbSheterozygotes,patientswith irondeficiencyanemiaandhealthypatients.2,8
In this study, no significant difference was identified betweenthegroupswithrespecttoageandageatdiagnosis. SeveralauthorshaveshownthatLVHisdirectlyrelatedtothe age3,7,8,15whereasanotherstudy10showedthatLVHismuch
morecommoninyoungpeople.Moreover,otherauthorsdid notfindanydifferenceinageamongpatientswithorwithout hypertrophy.12 Therewasnostatisticaldifferenceregarding
the percentageofHbS andHb Fatdiagnosis betweenthe groupsinthisstudy.Apreviousstudyshowedadirectly pro-portionalrelationshipbetweenleftventricularmassandHbS levels,7butnotwithHbF.11,22
Table2–Echocardiographicparametersofsicklecellanemiapatientswithandwithoutleftventricularhypertrophy.
Leftventricularhypertrophy p-value
Yes No
LVmassindex(g/m2)a 49.40±9.65 32.94±4.43 <0.001
Aorticroot(mm/m2)a 21.9±3 19.7±2.6 <0.001
Leftatrium(mm/m2)a 25.5±3.9 22±3.4 <0.001
LVdiastolicdiameter(mm/m2)a 44.6±7.7 36.7±5.3 <0.001
LVsystolicdiameter(mm/m2)a 27±5.1 22.2±3.9 <0.001
Interventricularseptum(mm/m2)a 6.5±1.2 5.2±0.7 <0.001
LVposteriorwall(mm/m2)a 6.6±1.3 5.3±0.8 <0.001
End-diastolicvolume(mm3/m2)a 34.77±26.32 26.25±11.93 0.09
Relativewallthickness(mm) 0.30±0.05 0.29±0.04 0.63
Systolicshorteningfraction(%) 0.39±0.05 0.39±0.07 0.73
Ejectionfraction(%) 0.69±0.64 0.69±0.64 0.99
SPAP(mmHg) 17.89±7.72 20.60±8.75 0.15
LV:leftventricle;SPAP:systolicpulmonaryarterypressure.
a Adjustedforbodysurface.
Table3–Laboratoryvariablesofsicklecellanemiapatientswithandwithoutleftventricularhypertrophy.
LVH p-value
Yes No
Hemoglobin(g/dL) 7.65±1.39 8.46±1.70 0.01
Hemoglobin(%) 21.94±3.41 25.26±5.49 0.001
Leukocytes(mm3) 12,954.00±3460.78 12,007.71±4500.11 0.26
Reticulocyteindex 1.23±0.75 1.97±1.52 0.02
Lactatedehydrogenase(U/L) 1576.89±789.76 1310.14±701.96 0.10
Totalbilirubin(mg/dL) 4.93±2.93 4.14±3.44 0.25
Indirectbilirubin(mg/dL) 4.11±2.73 3.39±3.23 0.27
Ferritin(ng/mL) 651.57±1313.11 857.95±1271.80 0.46
Creatinine(mg/dL) 0.39±0.14 0.42±0.12 0.22
Urea(mg/dL) 16.17±6.66 15.37±6.05 0.55
Albumin:creatinine(mg/g) 97.92±217.83 27.60±43.51 0.01
CC(mL/min/1.73m2) 162.31±68.13 160.80±46.76 0.85
CC:creatinineclearance.
effectgivenbyapossiblehigherfrequencyofblood transfu-sions.Likewise,patientswithhistoriesofstroke,priapismand acutechestsyndromeconstitutethegroupwithclassical indi-cationfortheuseofhydroxyurea,whichalsocontributesto increasedlevelsofhemoglobinandaproportionatedecrease inHbS,previouslydemonstratedasbeingdirectlyrelatedto increasesinleft ventricular massinSCApatients. Theleft atrium,apotentialmarkerofdiastolicdysfunction,was sig-nificantlylargerinpatientswithLVH,aresultconsistentwith previousstudies.13,14Systolicpulmonaryarterypressurewas
similarbetweenthegroupsinthisstudy,therebydisagreeing withtheliterature.14,23
LVHisinverselyrelatedtothehemoglobinconcentration, which is consistent withprevious studies.7,8,12 The
reticu-locyteindex, lower inpatients with LVH, may signal bone marrowexhaustion.Markersofhemolysis(lactic dehydroge-nase,indirectbilirubinandferritin)andcreatinineclearance wereuniformlyhighinbothgroups,possiblyduetothe pre-dominant haplotype in Brazil, Bantu, which is associated withthemostseveredisease.24Previousstudiesshowedthat
patientswhomoreoftenreceivedredbloodcelltransfusions hadlowerleftventricularmasses,12,25similartodatafoundin
thepresentstudy,inwhichnumerical,albeitnon-significant,
differenceswereobserved.LVHwasnotassociatedtoferritin levels, similar toa previous study.12 In one study patients
withLVH had ahighermean 24-h albumin:creatinineratio inurine,withsimilarglomerularfiltrationratesbetweenthe twogroups.12Patientsweredescribedaschronicallyanemic,
withestablishedrenalimpairment,dilation oftheleft ven-tricleandLVHinanotherstudy,26reinforcingthedifference
foundinthealbumin:creatinineratio,althoughtherewasno relationtotheglomerularfiltrationrate.Thisispossiblydue to the stateof hyperfiltration, characteristic of early renal injuryinSCApatients.Inonestudycardiacremodelingwas preventedwiththeuse ofenalapril innineSCApatients.27
Althoughtheassociation ofincreasedleft ventricularmass and diastolic dysfunctionis relatedto hypertensionin the generalpopulation, inSCA patientsthis association isdue to a combination of compensatoryhypertrophy ofthe left ventricle, secondary anemia and left ventricular dilatation along withsystemicvasculopathy. Directmyocardial injury andmicrovasculardiseasebyirondepositionhavebeen pos-tulatedaspossibleetiologiesforcardiacabnormalities.17The
ventriculardiastolic3,15,17andsystolicdysfunction3,15andhas
beendescribedasacauseofsuddendeathinSCApatients.10
Thisstudypresentslimitations.Thecriteriausedtodefine LVHaredesignedformoreethnicallyhomogeneous popula-tions.Moreover,arterialbloodpressureswerenotevaluated. The low number of patients using hydroxyurea may have interferedinthe adequate analysisofapossibleprotective role.
Conclusion
YoungSCApatientsinthis study hadahigh prevalenceof LVH(37.6%);thiswasassociatedwithlowerhemoglobinand hematocritlevelsandreticulocyteindexandahigher albu-min:creatinineratio.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1. Canc¸adoRD,JesusJA.SicklecelldiseaseinBrazil.RevBras HematolHemoter.2007;29(3):203–6.
2. Souza-JúniorJL,RodriguesAC,BuckPC,GuallandroSF,Mady C.Coronaryflowreserveinsicklecellanemia.ArqBras Cardiol.2007;88(5):552–8.
3. MartinsWA,MesquitaET,CunhaDM,FerrariAH,PinheiroLA, Romeo-FilhoLJ,etal.Cardiovascularchangesinsicklecell anemia.ArqBrasCardiol.1998;70(5):365–70.
4. GualandroSF,FonsecaGH,GualandroDM.Cardiopulmonary complicationsofsicklecelldisease.RevBrasHematol Hemoter.2007;29(3):291–8.
5. CipolottiR,CostaGB,LimaWH,FrancoRP,MelloEV,Dal FabbroAL,etal.Echocardiographiccharacteristicsofpatients withsicklecellanemiainSergipe,Brazil.JTropPediatr. 2001;47(2):73–6.
6. VaratMA,AdolphRJ,FowlerNO.Cardiovasculareffectsof anemia.AmHeartJ.1972;83(3):415–26.
7. LesterLA,SodtPC,HutcheonN,ArcillaRA.Cardiac abnormalitiesinchildrenwithsicklecellanemia.Chest. 1990;98(5):1169–74.
8. PoludasuS,RamkissoonK,SalciccioliL,KamranH,LazarJM. Leftventricularsystolicfunctioninsicklecellanemia:a meta-analysis.JCardFail.2013;19(5):333–41.
9. GrossmanW,JonesD,McLaurinLP.Wallstressandpatterns ofhypertrophyinthehumanleftventricle.JClinInvest. 1975;56(1):56–64.
10.JohnsonMC,KirkhamFJ,RedlineS,RosenCL,YanY,RobertsI, etal.Leftventricularhypertrophyanddiastolicdysfunction inchildrenwithsicklecelldiseasearerelatedtoasleepand
wakingoxygendesaturation.Blood.2010;116(1):16–21.
11.AhmedS,SiddiquiAK,SadiqA,ShahidRK,PatelDV,Russo LA.Echocardiographicabnormalitiesinsicklecelldisease. AmJHematol.2004;76(3):195–8.
12.ZilbermanMV,DuW,DasS,SarnaikSA.Evaluationofleft ventriculardiastolicfunctioninpediatricsicklecelldisease patients.AmJHematol.2007;82(6):433–8.
13.NaomanSG,NouraieM,CastroOL,NwokoloC, Fadojutimi-AkinsikuM,DiazS,etal.Echocardiographic findingsinpatientswithsicklecelldisease.AnnHematol. 2010;89(1):61–6.
14.BlancJ,StosB,DeMontalembertM,BonnetD,BoudjemlineY. Rightventricularsystolicstrainisalteredinchildrenwith sicklecelldisease.JAmSocEchocardiogr.2012;25(5):511–7.
15.DenenbergBS,CrinerG,JonesR,SpannJF.Cardiacfunctionin sicklecellanemia.AmJCardiol.1983;51(10):1674–8.
16.NaguehSF,AppletonCP,GillebertTC,MarinoPN,OhJK, SmisethOA,etal.Recommendationsfortheevaluationofleft ventriculardiastolicfunctionbyechocardiography.JAmSoc Echocardiogr.2009;22(2):107–33.
17.GordeukVR,SachdevV,TaylorJG,GladwinMT,KatoG,Castro OL.Relativesystemichypertensioninpatientswithsicklecell diseaseisassociatedwithriskofpulmonaryhypertension andrenalinsufficiency.AmJHematol.2008;83(1):15–8.
18.DevereuxRB,AlonsoDR,LutasEM,GottliebGJ,CampoE, SachsI,etal.Echocardiographicassessmentofleft ventricularhypertrophy:comparisontonecropsyfindings. AmJCardiol.1986;57(6):450–8.
19.HassellKL.Populationestimatesofsicklecelldiseaseinthe U.S.AmJPrevMed.2010;38Suppl.4:S512–21.
20.ReesDC,WilliamsTN,GladwinMT.Sickle-celldisease. Lancet.2010;376(9757):2018–31.
21.MartinC,CobbC,JohnsonC,TatterD,HaywoodLJ. Cardiovascularpathologyinsicklecelldisease.ClinRes. 1983;31:13A.
22.TidakeA,GangurdeP,TaksandeA,MahajanA,NathaniP.Left ventricularfunctionbyechocardiograminchildrenwith sicklecellanaemiainMumbai,WesternIndia.CardiolYoung. 2014;18:1–7.
23.RiberaMC,RiberaRB,KoifmanRJ,KoifmanS.
Echocardiographyinsicklecellanaemiapatientsunder20 yearsofage:adescriptivestudyintheBrazilianWestern Amazon.CardiolYoung.2015;25(1):63–9.
24.Galiza-NetoGC,PitombeiraMS.Molecularaspectsforsickle cellanemia.JBrasPatolMedLab.2003;39(1):51–6.
25.BatraAS,AchermanRJ,WongWY,WoodJC,ChanLS, RamiconeE,etal.Cardiacabnormalitiesinchildrenwith sicklecellanemia.AmJHematol.2002;70(4):306–12.
26.GoldbergN,LundinAP,DelanoB,FriedmanEA,SteinRA. Changesinleftventricularsize,wallthickness,andfunction inanemicpatientstreatedwithrecombinanthuman erythropoietin.AmHeartJ.1992;124(2):424–7.
27.LimaCS,UetiOM,UetiAA,FranchiniKG,CostaFF,SaadST. Enalapriltherapyandcardiacremodellinginsicklecell diseasepatients.ActaCardiol.2008;63(5):599–602.