SOCIEDADE BRASILEIRA DE ORTOPEDIA E TRAUMATOLOGIA
w w w . r b o . o r g . b r
Review
Article
The
use
of
bone
morphogenetic
proteins
(BMP)
and
pseudarthrosis,
a
literature
review
夽
Oberdan
Ribeiro
Gonc¸alves
de
Oliveira,
Saul
Pinheiro
Rebouc¸as
Martins
∗,
Wyvison
Gomes
de
Lima,
Marília
Maia
Gomes
HospitalDomHélderCâmara,DepartamentodeCirurgiaOrtopédica,Recife,PE,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received5February2016 Accepted7March2016 Availableonline22June2016
Keywords:
Bonemorphogeneticprotein2 Bonemorphogeneticproteins7 Pseudarthrosis
a
b
s
t
r
a
c
t
Bonemorphogeneticproteins(BMP)aremulti-functionalgrowthfactorstopromotebone healingwiththeproposaloflessmorbiditycomparedtotheusualmethodsofbonegraft harvest.Pseudoarthrosisoccurwhenthefusionattemptfails,asolidfusionisnotachieved, orthereismotionacrossthesegmentleadingtoit,anditcanbeclinicallysymptomaticas pain,deformity,neurocompression,orhardwarefailure.BMPsareusedatspinalfusionas atoolforthetreatmentofdegenerative,traumatic,neoplasticandinfectiousconditionsof thespine.ThisreviewshowsthattheuseofBMPSiseffectiveandsecurewhencompared withiliaccrestbonegraft(ICGB);however,dependingofthelocationofusage(cervicalspine, lumbarspineorsacrum)andthemedicalstatusofthepatient(presenceofcomorbidities, tobaccousage),itismorelikelytoexhibitcomplications.Therefore,theuseoftheseproteins mustbeaninformeddecisionofpatientandphysicianpreferences.
©2016SociedadeBrasileiradeOrtopediaeTraumatologia.PublishedbyElsevierEditora Ltda.ThisisanopenaccessarticleundertheCCBY-NC-NDlicense(http:// creativecommons.org/licenses/by-nc-nd/4.0/).
O
uso
de
proteínas
morfogenéticas
ósseas
(BMP)
e
pseudoartroses,
uma
revisão
de
literatura
Palavras-chave:
Proteínasmorfogenéticasósseas2 Proteínamorfogenéticaóssea7 Pseudoartrose
r
e
s
u
m
o
Proteínasmorfogenéticasdoosso(Bonemorphogeneticproteins[BMP])sãofatoresde cresci-mentomultifuncionaisquepromovemcicatrizac¸ãoóssea,propondomenoscomorbidades comparadoaos métodosusuais de colheitade enxerto ósseo. Pseudoartrosesocorrem quandoatentativadefusãoósseafalha,umafusãosólidanãoéatingidaouquandohá movimentac¸ãodosegmento quelevaà pseudoartrose, quepode serclinicamente sin-tomáticacomdor,deformidade,neurocompressãooufalhanacolocac¸ãodematerialde síntese.AsBMPssãousadas emfusãocolunar comoferramentaparaotratamento de
夽
WorkperformedattheDepartmentofOrthopaedicSurgery,HospitalDomHélderCâmara,Recife,PE,Brazil. ∗ Correspondingauthor.
E-mail:larycruz@hotmail.com(S.P.Martins). http://dx.doi.org/10.1016/j.rboe.2016.03.005
rev bras ortop.2017;52(2):124–140
125
traumadegenerativo,condic¸õesneoplásicaseinfecciosasdacoluna.Apresenterevisãoda literaturamostraqueousodeBMPséefetivoeseguroquandocomparadocomenxerto ósseoilíaco.Noentanto,adependerdolocaldeuso(colunacervicaloulombarousacro) edoestadomédicodopaciente(presenc¸adecomorbidades,tabagismo)émaispropício oaparecimentodecomplicac¸ões.Portanto,ousodessasproteínasdeveserdecididoapós umadecisãoconjuntadepreferênciasmédicasedopaciente.
©2016SociedadeBrasileiradeOrtopediaeTraumatologia.PublicadoporElsevier EditoraLtda.Este ´eumartigoOpenAccesssobumalicenc¸aCCBY-NC-ND(http:// creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
Bone morphogenetic proteins (BMP) are multi-functional growthfactors thatbelong tothe transforminggrowth fac-torbeta(TGF-beta)superfamily,theywereintroducedinthe medicalscenariotopromotebonehealingwiththeproposal oflessmorbiditycomparedtotheusualmethodsofbonegraft harvest;itistheonlyboneinducerwithlevelIofclinical evi-dence.TheFoodandDrugAdministration(FDA)approvedits useinJulyof2002foranteriorapproaches oflumbarspine fusionprocedures.
Thespinalfusionisatoolforthetreatmentofdegenerative, traumatic,neoplasticandinfectiousconditionsofthespine, it canbeachieved withinterbody fusion, posterioror pos-terolateralfusionandcircumferencialfusion.Themostused examplesofBMP’sarerecombinanthumanBMP-2(rhBMP-2 isapprovedforanteriorlumbarinterbodyfusions–ALIF)and recombinanthumanBMP-7(rhBMP-7hasreceiveda human-itariandevice exemptionforrevisionposterolateral lumbar fusionoperation).
ImplantscontainingBMP’sarepromisingtoitssafetyandit isaseffectiveasiliaccrestbonegraft(ICBG).Adoptingtheuse ofitbringshighcostsandithassafetyconcernswithreported complicationspecificstoitsuse,includingosteolysis,ectopic boneformation,radiculitis,cervicalsofttissueswellingand pseudoarthrosis.
NowadaysthegreatestuseofBMPisforofflabeltreatments as anadjunt to allograftor autograftbone – often replac-ingtheuseofICBGinmandibularreconstruction,unspecific oralandmaxillofacialfacialsurgeries,cervicalspinefusion, pseudoarthrosisfusion.Butitisstillintheneedoffurther investigationrelatedtoitscollateraleffects.
Pseudoarthrosis occur when the fusion attempt fails, a solid fusion is not achieved, or there is motion across the segment leading to it, and it can be clinically symp-tomatic aspain, deformity, neurocompressionor hardware failure.Therearetwotypes:hypertrophic/hypercascularand atrophic/avascular,thelastoneisapplicableosteoinductive treatmentwithBMP.Thisreviewintendstocorrelateand clar-ifytheuseofBMP’sanditsbiasonpseudoarthrosis,whenit isacorrectionorcausefactor.
Methods
Aqualitativesystematicreviewofarticlesabouttheuse of BoneMorphogeneticProteininPseudarthrosiswasdeveloped onabasisofpreselecteddata.Itwasperformedasearchof
literaturefromtheonlinedatabaseBVSandSCOPUSfrom Jan-uary2006toNovember2015.Thesearchwasfocusedfromthe followingterms:(1)‘Pseudarthrosis’{MedicalSubject Head-ings} [MeSH term]; and (2) ‘Bone Morphogenetic Proteins’ {MedicalSubjectHeadings}[MeSHterm],thesetermswere chosentodefineourcentralmatterofthepaperandallarticles wereevaluatedwithrigortopropersampling.
Theanalysisofthearticles followspredefinedeligibility criteria. Weadoptthefollowinginclusion criteria:(1) origi-nalarticleswithfulltextonlineaccess;(2)Fromtherelevant sourcetitles:‘Spine’,‘Injury’,‘SpineJournal’,‘JournalofBone andJointSurgerySeriesA’,‘JournalofNeurosurgerySpine’and ‘Journal ofOrthopaedicResearch’; (3)Observational, experi-mentalorquasi-experimentalstudies;(4)WritingsinEnglish only;(5)StudieswhichfocusontheuseofBMPin pseudarthro-sis.
Exclusion criteria were: (1) other projects, suchas case reports,caseseries,literaturereviewandcomments,(2)The non-original studies, including editorials, comments, pref-aces,briefcommentsandlettertotheeditor;(3)Productions thatdidnotaccomplishtheproposedtheme;and(4)the arti-clesinwhichtheobjectiveofthestudydidnotmatchedthe themepurposedbythesystematicreviewinquestion.
We found applicable 85 articles that, when screened, resultedin24articlesthatmetthe criteriaofevidenceand wereincludedinthisreview(Table1).
Discussion
BMPsweredevelopedwiththegoalofimprovingclinical out-comesthroughthepromotionofbonyhealingandreducing morbidityfromICBG(stillconsidered‘goldstandard’to multi-levelspinefusion).1,2Spinalfusionprocedureisindicatedfor
avarietyofpathologicalstatesincludingspinalinstability sec-ondarytotrauma,infection,orneoplasmaswellasintractable axialpaincausedbydegenerativedisorders.3Achievingfusion
isdifficultbecauseofpoorlocalbonequalityandlongfusions haveanegativevariablethatinhibitsasolidfusion,andthe BMPisbeenresearchedasapotentialsolutionforthis prob-lem.
r
e
v
b
r
a
s
o
r
t
o
p
.
2
0
1
7;
5
2(2)
:124–140
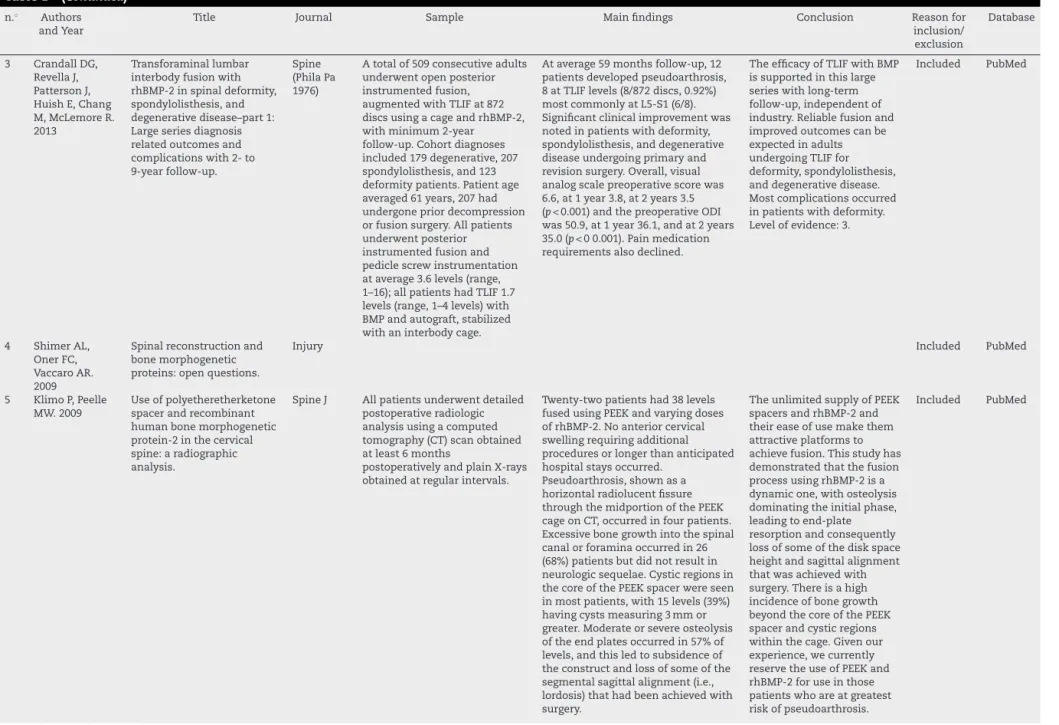
Table1–Theuseofbonemorphogeneticproteinsandpseudarthrosisreview.
n.◦ AuthorsandYear Title Journal Sample Mainfindings Conclusion Reasonfor
inclu-sion/exclusion
Database
1 DagostinoPR, WhitmoreRG, SmithGA, MaltenfortMG, RatliffJK.2014
Impactofbone morphogenetic proteinsonfrequency ofrevisionsurgery,use ofautograftbone,and totalhospitalcharges insurgeryforlumbar degenerativedisease: reviewofthe NationwideInpatient Samplefrom2002to 2008.
SpineJ Studydesign:NationwideInpatient Sample(NIS)retrospectivecohort assessmentof46,452patientsfrom 2002to2008.Patientsample:All patientswhounderwentlumbar arthrodesisproceduresfor degenerativespinaldisease. Outcomemeasures:UseofBMP, revisionsurgerystatusasa percentageoftotalprocedures,and autograftharvestinlumbarfusion procedurescompletedfor degenerativediagnoses.Methods: Demographicand
geographic/practicedata,hospital charges,andlengthofstayofall NISpatientswiththoracolumbar andlumbosacralprocedurecodes fordegenerativespinaldiagnoses wererecorded.Codesforautograft harvest,useofBMP,andrevision surgerywereincludedin multivariableregressionanalysis.
Theassessmentfound46,452 patientsfrom2002to2008
undergoingthoracolumbarorlumbar arthrodesisproceduresfor
degenerativedisease.Assuminga representativesample,thiscohort modelsmorethan200,000US patients.Therewassteadygrowthin lumbarspinefusionandintheuseof BMP.TheuseofBMPincreasedfrom 2002to2008(oddsratio[OR],1.50; 95%confidenceinterval[CI], 1.48–1.52).Revisionprocedures decreasedoverthestudyperiod(OR, 0.94;95%CI,0.91–0.96).Theuseof autograftdecreasedsubstantially afterintroductionofBMPbutthen returnedtobaselinelevels;therewas nonetchangeinautograftusefrom 2002to2008.TheuseofBMP correlatedwithsignificantincreases inhospitalcharges($13,362.39; standarddeviation±596.28,
p<.00001).TheuseofBMPin degenerativethoracolumbar procedurespotentiallyaddedmore than$900milliontohospitalcharges from2002to2008.
Therewasanoverall decreaseinratesof revisionfusion proceduresfrom 2002to2008. IntroductionofBMP didnotcorrelate withdecreaseinuse ofautograftbone harvest.UseofBMP correlatedwith substantialincrease inhospitalcharges. Thesmalldecrease inrevisionsurgeries recorded,combined withlackof significantchangein autograftharvest rates,mayquestion thefinancial justificationforthe useofBMP.
Included PubMed/BVS
2 CrandallDG, RevellaJ, PattersonJ,Huish E,ChangM, McLemoreR. 2013
Transforaminal lumbarinterbody fusionwithrhBMP-2in spinaldeformity, spondylolisthesis,and degenerative disease–part2:BMP dosage-related complicationsand long-termoutcomesin 509patients.
Spine (PhilaPa 1976)
TLIFwithrhBMP-2wasperformed at872discsin509consecutive adultswhounderwentopen posteriorinstrumentedfusionand hadminimum2-yearfollow-up; diagnosesincludeddegenerative disease(179),spondylolisthesis (207),deformity(123).Patientage averaged61years:12%were smokersand41%hadrevision surgery.TLIFwasperformedat1.7 levels:singlelevel:229,2levels: 201,3levels:74,4levels:5.Local autograftwasusedforbackfill aroundandbehindeach rectangularcage.Varyingdosesof interbodyBMPwereusedatan average7.3mgperdisk(range: 2–12mgperdisk).
At5yearsaveragefollow-up,8 patientsdevelopedpseudoarthrosis atlevelsofTLIF(8of872discs, 0.92%).Seroma(0.4%)andectopic bonegrowth(0.6%)weretoo infrequenttobeassociatedwitha particularBMPdose.Deepinfection was2.6%overall(1.7%ofthe degenerativegroup).Symptomatic osteolysisorcagesubsidencedidnot occur.Significantlong-term improvementwasnotedinclinical andfunctionaloutcomescompared withpreoperation.
Five-yearfollow-up afterTLIFwithBMP, independentof industry,confirms effectivearthrodesis inshortandlong fusions,both primaryand revision.Most complications occurredin deformitypatients. BMP-related complications (seroma,ectopic bone)wererare. Levelofevidence:3.
r
e
v
b
r
a
s
o
r
t
o
p
.
2
0
1
7;
5
2(2)
:124–140
127
Table1–(Continued)
n.◦ Authors andYear
Title Journal Sample Mainfindings Conclusion Reasonfor
inclusion/ exclusion
Database
3 CrandallDG, RevellaJ, PattersonJ, HuishE,Chang M,McLemoreR. 2013
Transforaminallumbar interbodyfusionwith rhBMP-2inspinaldeformity, spondylolisthesis,and degenerativedisease–part1: Largeseriesdiagnosis relatedoutcomesand complicationswith2-to 9-yearfollow-up.
Spine (PhilaPa 1976)
Atotalof509consecutiveadults underwentopenposterior instrumentedfusion, augmentedwithTLIFat872 discsusingacageandrhBMP-2, withminimum2-year follow-up.Cohortdiagnoses included179degenerative,207 spondylolisthesis,and123 deformitypatients.Patientage averaged61years,207had undergonepriordecompression orfusionsurgery.Allpatients underwentposterior instrumentedfusionand pediclescrewinstrumentation ataverage3.6levels(range, 1–16);allpatientshadTLIF1.7 levels(range,1–4levels)with BMPandautograft,stabilized withaninterbodycage.
Ataverage59monthsfollow-up,12 patientsdevelopedpseudoarthrosis, 8atTLIFlevels(8/872discs,0.92%) mostcommonlyatL5-S1(6/8). Significantclinicalimprovementwas notedinpatientswithdeformity, spondylolisthesis,anddegenerative diseaseundergoingprimaryand revisionsurgery.Overall,visual analogscalepreoperativescorewas 6.6,at1year3.8,at2years3.5 (p<0.001)andthepreoperativeODI was50.9,at1year36.1,andat2years 35.0(p<00.001).Painmedication requirementsalsodeclined.
TheefficacyofTLIFwithBMP issupportedinthislarge serieswithlong-term follow-up,independentof industry.Reliablefusionand improvedoutcomescanbe expectedinadults undergoingTLIFfor deformity,spondylolisthesis, anddegenerativedisease. Mostcomplicationsoccurred inpatientswithdeformity. Levelofevidence:3.
Included PubMed
4 ShimerAL, OnerFC, VaccaroAR. 2009
Spinalreconstructionand bonemorphogenetic proteins:openquestions.
Injury Included PubMed
5 KlimoP,Peelle MW.2009
Useofpolyetheretherketone spacerandrecombinant humanbonemorphogenetic protein-2inthecervical spine:aradiographic analysis.
SpineJ Allpatientsunderwentdetailed postoperativeradiologic analysisusingacomputed tomography(CT)scanobtained atleast6months
postoperativelyandplainX-rays obtainedatregularintervals.
Twenty-twopatientshad38levels fusedusingPEEKandvaryingdoses ofrhBMP-2.Noanteriorcervical swellingrequiringadditional proceduresorlongerthananticipated hospitalstaysoccurred.
Pseudoarthrosis,shownasa horizontalradiolucentfissure throughthemidportionofthePEEK cageonCT,occurredinfourpatients. Excessivebonegrowthintothespinal canalorforaminaoccurredin26 (68%)patientsbutdidnotresultin neurologicsequelae.Cysticregionsin thecoreofthePEEKspacerwereseen inmostpatients,with15levels(39%) havingcystsmeasuring3mmor greater.Moderateorsevereosteolysis oftheendplatesoccurredin57%of levels,andthisledtosubsidenceof theconstructandlossofsomeofthe segmentalsagittalalignment(i.e., lordosis)thathadbeenachievedwith surgery.
TheunlimitedsupplyofPEEK spacersandrhBMP-2and theireaseofusemakethem attractiveplatformsto achievefusion.Thisstudyhas demonstratedthatthefusion processusingrhBMP-2isa dynamicone,withosteolysis dominatingtheinitialphase, leadingtoend-plate resorptionandconsequently lossofsomeofthediskspace heightandsagittalalignment thatwasachievedwith surgery.Thereisahigh incidenceofbonegrowth beyondthecoreofthePEEK spacerandcysticregions withinthecage.Givenour experience,wecurrently reservetheuseofPEEKand rhBMP-2foruseinthose patientswhoareatgreatest riskofpseudoarthrosis.
r
e
v
b
r
a
s
o
r
t
o
p
.
2
0
1
7;
5
2(2)
:124–140
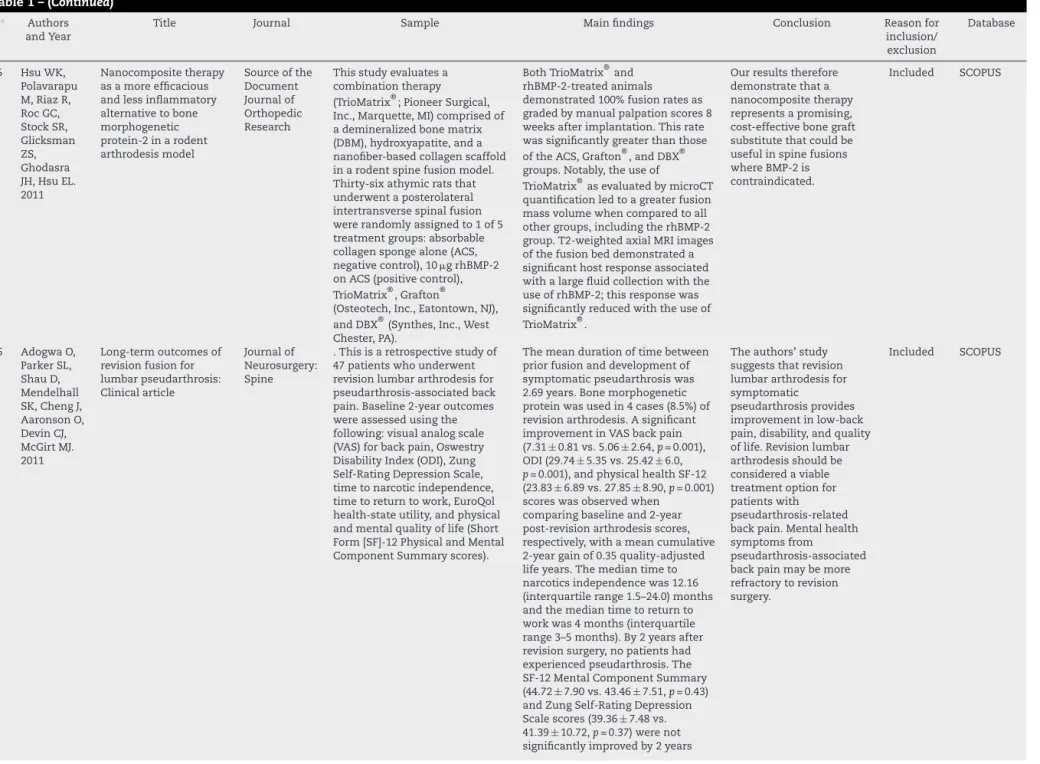
Table1–(Continued) n.◦ Authors
andYear
Title Journal Sample Mainfindings Conclusion Reasonfor
inclusion/ exclusion
Database
6 AnnisP,Brodke DS,SpikerWR, DaubsMD, LawrenceBD. 2015
ThefateofL5-S1with low-doseBMP-2and pelvicfixation,withor withoutinterbodyfusion, inadultdeformity surgery
Spine Retrospectivereviewof61 consecutivepatientswith minimum2-yearfollow-upata singleinstitution.Allpatients hadanisolatedposterior approach,5ormorelevels fusedincludingL5–S1,useof pelvicfixation,andnoprior L5-S1procedures.Thepatients weredividedin2groupsfor comparisononthebasisofthe useofaninterbodycage/fusion attheL5–S1level.Revision ratesandimplant-related complicationswerealso reported.
ThefusionrateatL5–S1was97% (59/61),withnodifferencebetween theinterbodyandnointerbody fusiongroups(97%vs.96%,p=1.0). Therewerenosignificant differencesintheradiographical parametersordeformitycorrection betweenthegroups.Themean amountofBMP-2usedinthe interbodygroupwas4.1mg(2–10), 2.5mg(0–8)inthediskspace,and 1.6mg(0–4)intheinterbodycage, whereastherewasnodifferencein theamountofrecombinanthuman bonemorphogenicprotein-2placed posterolaterallybetweenthe2 groups(interbodyfusion=1.6vs. non-interbodyfusion=2.0mg,
p=0.08)alongwithautograftand allograft.Theoverallrevisionrate forL5–S1nonunionwas1.6%.
Theuseoflowdoseof BMP-2attheL5–S1level incombinationwith sacropelvicfixation achievedsatisfactory fusionratesinadult deformitysurgery.No additionalbenefitwas encounteredbyadding aninterbodycage.
Included SCOPUS
7 TheologisAA, TabaraeeE,Lin T,LubickyJ, DiabM.2015
Typeofbonegraftor substitutedoesnotaffect outcomeofspinefusion withinstrumentationfor adolescentidiopathic scoliosis
Spine Children(10–18yr)withAIS whounderwentdeformity correctionviaaposterior approachwereidentifiedinthe SpinalDeformityStudyGroup database.Allhadaminimumof 2-yearfollow-up.Patientswere subdividedinto3groupsbased onbonegraftused:AIC, allograft,andbonesubstitute (BS).Clinicaldataincluded patientdemographics, operativedetails,postoperative analgesicuse,and
perioperativecomplications. Lenkecurvetypeandcurve magnitudechangeswere radiographicallyanalyzed.The ScoliosisResearchSociety-30 questionnairewasusedto assessclinicaloutcomes.
461patientsmetinclusioncriteria (girls:381,boys:80;averageage 14.7±1.7)andconsistedof152AIC patients(124girls,28boys),199 allograftpatients(167girls,32boys), and110BSpatients(90girls,20 boys).Therewasnodifferencein age(p=0.41)orgender(p=0.82).The BSgrouphadsignificantlysmaller preoperativecurvesandshorter operativetimes.Postoperatively, patientswhoreceivedBShad significantlylongerhospitalstays, usedhigherquantitiesof patient-controlledintravenous analgesiaandusedepidurals longer.TheAICgroupused patient-controlledintravenous analgesiasignificantlylonger.There werenodifferencesbetweenthe groupsinregardstocurvetype, numberoflevelsfused, postoperativeinfections, pseudarthrosis,reoperationsfor anyindication,andScoliosis ResearchSociety-30scoresatthe latestfollow-up.
Outcomesafterprimary posteriorspinalfusion withinstrumentationare notinfluencedbytypeof bonegraftorsubstitute.
r
e
v
b
r
a
s
o
r
t
o
p
.
2
0
1
7;
5
2(2)
:124–140
129
Table1–(Continued)
n.◦ Authors andYear
Title Journal Sample Mainfindings Conclusion Reasonfor
inclusion/ exclusion
Database
8 LinaIA, Puvanesarajah V,LiauwJA,Lo SF, Santiago-DieppaDR, HwangL,Mao A,BydonA, WolinskyJP, SciubbaDM, GokaslanZ, HolmesC, WithamTF. 2014
Quantitativestudyof parathyroidhormone(1-34) andbonemorphogenetic protein-2onspinalfusion outcomesinarabbitmodel oflumbardorsolateral intertransverseprocess arthrodesis
Spine Forty-eightmaleNewZealand whiterabbitsunderwentbilateral posterolateralintertransverse processarthrodesissurgeryatthe L5–L6level.Animalsweredivided into6groups.Twogroupswere treatedwithautograftaloneor autograftandPTH(1-34),whereas theother4groupsweretreated withlow-doserhBMP-2alone, high-doserhBMP-2alone,oreither dosecombinedwithPTH(1-34). Allanimalswereeuthanized6 weeksaftersurgery.TheL4–L7 spinalsegmentwasremovedand assessedusingmanualpalpation, computedtomography(CT),and biomechanicaltesting.
CTassessmentsrevealedfusionin 50%ofautograftcontrols,75%of autograftPTH(1-34)animals,87.5% inthe2groupstreatedwith low-doserhBMP-2,and100%inthe 2groupstreatedwithhigh-dose rhBMP-2.CTvolumetricanalysis demonstratedthatallgroups treatedwithbiologicshadfusion massesthatwereonaverage significantlylargerthanthose observedinthecontrolgroup (p<0.0001).Biomechanicaldata demonstratednostatistical differencebetweencontrols,PTH (1-34),andlow-doserhBMP-2inany testingorientation.PTH(1-34)did notincreasebendingstiffnesswhen usedadjunctivelywitheither low-doseorhigh-doserhBMP-2.
Althoughintermittent teriparatideadministration resultsinincreasedfusion massvolume,itdoesnot improvebiomechnical stiffnessoveruseof autograftalone.When deliveredconcurrentlywith high-andlow-dose rhBMP-2,teriparatide providednostatistically significantimprovementin biomechanicalstiffness. Levelofevidence:N/A
Included SCOPUS
9 NandyalaSV, Marquez-Lara A,FinebergSJ, PeltonM,Singh K.2014
Prospective,randomized, controlledtrialof
silicate-substitutedcalcium phosphateversusrhBMP-2 inaminimallyinvasive transforaminallumbar interbodyfusion
Spine Fifty-twopatientsundergoinga single-levelunilateralMISTLIF wereevenlyrandomizedinto2 cohortsasfollows:theActifuse cohortreceivedActifusecombined with5mLofbonemarrowaspirate (n=26;50%),whereastherhBMP cohortreceived4.2mgofrhBMP-2 (n=26;50%).AprehocG*Power analysisyieldedasamplesizeof
n=26thatwasdetermined througha2-taileddistribution calculation.Computed tomographicanalysiswas performedat6monthsand1year postoperatively.Pre-and
postoperativevisualanalogscale scoreswereobtainedtoassessthe clinicaloutcomes.Arthrodesis wasdeterminedby2separate, blindedorthopedicsurgeonsanda boardcertifiedradiologist.
At1-yearfollow-up,65%(17/26)of theActifusecohortand92%(24/26) oftherhBMP-2cohort
demonstratedaradiographical arthrodesis(p=0.01).Inbothstudy cohorts,the1-yearpostoperative visualanalogscalescores significantlyimproved(p<0.001). Pseudarthrosisratesat1yearwere 35.0%(9/26)and7.7%(2/26)forthe ActifuseandrhBMP-2groups, respectively(p=0.01,OR=6.35,95% CI=1.22–33.1).Agreaterreoperation ratewasnotedintheActifuse cohort(35.0%,9/26)comparedwith theBMP-2cohort(7.7%,2/26;
p=0.01).OnepatientwithBMP-2 alsoexperiencedsymptomatic neuroforaminalbonegrowth(3.8%,
n=1/26).
Silicate-substituted calciumphosphatewas associatedwitha significantlylowerrateof arthrodesisthanrhBMP-2 inaMISTLIF.Thepatients withpseudarthrosisin bothcohortswereall clinicallysymptomatic withanunimprovedvisual analogscalescore. Additionalanalysisof Actifuseandothergraft enhancers/extendersare neededpriortothe utilizationforanMISTLIF
r
e
v
b
r
a
s
o
r
t
o
p
.
2
0
1
7;
5
2(2)
:124–140
Table1–(Continued) n.◦ Authors
andYear
Title Journal Sample Mainfindings Conclusion Reasonfor
inclusion/ exclusion
Database
10 HoffmannMF, JonesCB, SietsemaDL. 2013
Complicationsof rhBMP-2utilizationfor posterolaterallumbar fusionsrequiring reoperation:Asingle practice,retrospective caseseriesreport
Spine Journal
Inclusioncriteriawereposterolateral fusionwithrhBMP-2implantand ageequaltoorolderthan18years. Surgicalindicationsandtreatment wereperformedinaccordancewith thesurgeon’sbestknowledge, discretion,andexperience.Patients consentedtolumbardecompression andarthrodesisusingrhBMP-2.All patientswereeducatedand informedoftheoff-labelutilization ofrhBMP-2.Patientfollow-upwas performedatregularintervalsof2 weeks,6weeks,12weeks,6months, 1year,andlaterifrequiredor indicated.
Averageagewas59.2years,and bodymassindexwas30.7kg/mÂ. Numbersoflevelsfusedwere1 (414,35.8%),2(469,40.5%),3(162, 14.0%),4(70,6.0%),5(19,1.6%),6 (11,0.9%),7(7,0.6%),8(4,0.3%), and9(2,0.2%).Patientshaving complicationsrequiring reoperationwere117of1158 (10.1%):symptomaticnonunion requiringredofusionand instrumentation41(3.5%),seroma withacuteneuralcompression32 (2.8%),excessboneformationwith delayedneuralcompression4 (0.3%),andinfectionrequiring debridement26(2.2%).Nonunion wasrelatedtomalesexand previousBMPexposure.Seroma formationwassignificantlyhigher inpatientswithhigherdosesof rhBMP-2(p=.050)andwithmore than12mgofrhBMP-2(2=0.025). Bonereformationandneural compressionatthelaminectomy andforaminotomysitesoccurred inadelayedfashion.Infectionwas associatedwithobesityand respiratorydisease.Infectionswere notedwithagreaterBMPdose (p<.001),morethan12mg (2<0.001),fusionmorethanthree levels(2<0.001),andreexposedto BMP(2=0.023).
rhBMP-2utilizationfor posterolaterallumbar fusionshasalow symptomaticnonunion rate.PriorrhBMP-2 exposureandmalesex wererelatedto symptomaticnonunion formation.
rhBMP-2-associated neuralcompression acutelywithseroma formationanddelayed withforaminalbone formationisconcerning andassociatedwith higherrhBMP-2 concentrations.
r
e
v
b
r
a
s
o
r
t
o
p
.
2
0
1
7;
5
2(2)
:124–140
131
Table1–(Continued)
n.◦ Authors andYear
Title Journal Sample Mainfindings Conclusion Reasonfor
inclusion/ exclusion
Database
11 SinghK, NandyalaSV, Marquez-Lara A,ChaTD, KhanSN, FinebergSJ, PeltonMA.2013
Clinicalsequelaeafter rhBMP-2useina minimallyinvasive transforaminallumbar interbodyfusion
Spine Journal
Aretrospectivereviewof610 consecutivepatientsundergoingan MIS-TLIF(2007–2010)byasingle surgeonatourinstitutionwas performed(meanage48.7years, range26–82years).Allpatients underwentanMISlaminectomy withbilateralfacetectomy,single TLIFcage,unilateralpediclescrew fixation,and12mg(largekit)or 4.2mg(smallkit)ofrhBMP-2.The BMP-2collagen-soakedspongewas placedanteriorlyinthediskspace, followedbylocalbonegraft,and thenthecagewasfilledonlywith localboneandnoBMP-2.Patients wereevaluatedat6monthsand1 yearwithcomputedtomography (CT)scan.Thosedemonstrating neuroforaminalbonegrowth, osteolysis/cagemigration,or pseudarthrosiswerereviewed,and costdataincludingdirect cost/procedureforbothindexand revisionsurgerieswerecollected.
Ofthe573patients,10(1.7%) underwent15additional proceduresbasedonrecalcitrant radiculopathyandCTevidenceof neuroforaminalbonegrowth, vertebralbodyosteolysis,and/or cagemigration.Thirty-nine patients(6.8%)underwent reoperationforclinically
symptomaticpseudarthrosis.Bone overgrowthwasassociatedwith nerveimpingementand radiculopathyinall10patients (smallkit,n=9;largekit,n=1). Osteolysisandcagemigration occurredin2(20%)ofthesesame 10patients.Averagetotalcosts werecalculatedperprocedure ($19,224),andthecostsfor reoperationequaled$14,785per encounterforneuroforaminalbone growthand$20,267for
pseudarthrosis.
Symptomaticectopicbone formation,vertebral osteolysis,and pseudarthrosisare recognizedcomplications withtheuseofrhBMP-2in MIS-TLIFs.Potential causesincludeimproper dosageandaclosedspace thatpreventstheegressof thepostoperativeBMP-2 fluidcollection. Managementofthese complicationshasa substantialcostforthe patientandthesurgeon andneedstobe consideredwiththe off-labeluseofrhBMP-2.
Included SCOPUS
12 KimHJ, BuchowskiJM, ZebalaLP, DicksonDD, KoesterL, BridwellKH. 2013
RhBMP-2Issuperiorto iliaccrestbonegraftfor longfusionstothe sacruminadultspinal deformity
Spine Atotalof63consecutivepatients, from1997to2006,comprisedof31 patientsintheBMPgroupand32 patientsintheICBGgroup,operated onatasingleinstitutionwitha minimum4-yearfollow-up(4–14yr) wereanalyzed.Inclusioncriteria wereambulatorswhowere candidatesforlongfusions(thoracic astheupperlevel)tothesacrum. Exclusioncriteriawererevisions, neuromuscularscoliosis,ankylosing spondylitis,andpatientswhohad bothBMPandICBGusedforfusion. OswestryDisabilityIndexand3 domainsoftheScoliosisResearch Societyscorewereusedtoassess outcomes.
The2groupsweresimilarwith respecttoage,sex,smoking history,comorbidities,BMI, numberoffusionlevelsandCobb angles.EightpatientsintheBMP groupunderwentaposterioronly, whereas23underwentcombined anteriorandposterior(A/P) surgery.All32patientsintheICBG hadA/Pfusion.TheaverageBMP levelwas11.1mg(3–36mg).The ratepseudarthrosiswas6.4%(2/31) intheBMPand28.1%(9/32)inthe ICBGgroup(p=0.04)usingFisher exacttestandoddsratio=5.67.The fusionratesforBMPgroupwere 93.5%and71.9%fortheICBG group.OswestryDisabilityIndexes weresimilarbetweengroups. However,theBMPgroup demonstratedsuperiorsum compositeScoliosisResearch Societyscoresinpain,self-image andfunctiondomains(p=0.02).
BMPissuperiortoICBGin achievingfusioninlong constructsinadult deformitysurgery.The rateofpseudarthrosiswas significantlyhigherinthe ICBGgroupthanBMP group.Theconcentration anddosageof
recombinanthumanbone morphogeneticprotein2 (rhBMP-2)usedseemsto haveaneffectontherate offusionand
pseudarthrosisrate becausenopatient receivingmorethan5mg perlevelhadapparentor detectedpseudarthroses (n=20/20).
r
e
v
b
r
a
s
o
r
t
o
p
.
2
0
1
7;
5
2(2)
:124–140
Table1–(Continued)
n.◦ Authors andYear
Title Journal Sample Mainfindings Conclusion Reasonfor
inclusion/ exclusion
Database
13 FrenkelMB, CahillKS, JavaharyRJ, ZacurG,Green BA,LeviAD. 2013
Fusionratesinmultilevel, instrumentedanterior cervicalfusionfor degenerativediseasewith andwithouttheuseof bonemorphogenetic protein
Journalof Neuro-surgery: Spine
Theauthorsconducteda retrospectivecohortstudyof patientswhounderwent multilevel(2+level)anterior cervicalfusionsperformedfor degenerativediskdiseasewithor withouttheconcurrentuseof BMP-2from1997to2012.The dosagethroughoutthestudy rangedfrom2.1to0.26mg/level (mean1.0mg/level).Allpatients wereevaluatedpostoperativelyby meansofradiographsandCT scanstodeterminefusionstatus.
Theoverallfusionrateforthe patientstreatedwithoutBMP(n=23) was82.6%comparedwitha100% fusionrateinthegrouptreatedwith BMP(n=22)(p=0.04).The
pseudarthrosisratesincreasedwith numberoffusionlevelsinpatients whodidnotreceiveBMP,whereasall patientsinthegrouptreatedwith BMPhadsolidarthrodesis. Furthermore,therewere2 instrumentationfailuresinthe non-BMPgroup.Therewasadirect correlationbetweentheincidenceof complicationsandthedosageofBMP usedperlevel,withnocomplications reportedatdosesequaltoorless than1.1mg/level.
Theoverallrateofbony arthrodesiswasincreased followingtheuseofBMP inmultilevelanterior cervicalfusion.Traditional methodswithoutBMPhad ahighrateof
pseudarthrosis.The complicationsassociated withtheuseofBMP appearedtobedose relatedandoflow incidencewhenBMPis usedindosesequaltoor lessthan1.1mg/level.
Included SCOPUS
14 LuDC, TumialánLM, ChouD.2013
Multilevelanteriorcervical discectomyandfusion withandwithoutrhBMP-2: Acomparisonofdysphagia ratesandoutcomesin150 patients-Clinicalarticle
Journalof Neuro-surgery: Spine
Theauthorsretrospectively reviewed150patientrecords. Group1(BMPgroup)consistedof 100patientswhounderwent multilevelACDFwithPEEKcages filledwithrhBMP-2and instrumentedwithacervical plate.Group2(allograftgroup) includedamatchedcontrol cohortof50patientswho underwentmultilevelACDFwith allograftspacersandanterior platefixation(withoutrhBMP-2). Patientdemographicswerenot significantlydifferentbetween thegroups.Fusionwasassessed bymeansofdynamicradiographs and/orCTatroutineintervals. Complications,dysphagia incidence,standardized dysphagiascore,Nurickgrades, andfusionrateswereassessed.
Themeanfollow-upfortheBMP group(Group1)was35monthswhile themeanfollow-upfortheallograft group(Group2)was25months. Therewasacomplicationrateof13% intheBMPgroupcomparedwith8% intheallograftgroup(p<0.005). Therewasnosignificantdifferencein overalldysphagiaincidencebetween theBMPgroupandtheallograft group(40%vs44%,respectively;
p>0.05).However,therewasa significantdifferenceintheseverity ofdysphagia(usingtheSWAL-QOL dysphagiascoringsystem)between the2groups:0.757fortheBMPgroup versus0.596fortheallograftgroup (p<0.005).Insubgroupanalysis,the useofrhBMP-2significantly increasedtheseverityofdysphagiain patientsundergoing2-levelACDF (p<0.005).However,theseverityof dysphagiadidnotdiffersignificantly betweengroupswhen3-or4-level ACDFcaseswerecompared.There wasnopseudarthrosisinGroup1 (theBMPgroup)comparedwitha16% pseudarthrosisrateinGroup2(the allograftgroup)(p<0.05).Therewasa weakcorrelationbetweenthetotal rhBMP-2doseandthedysphagia score(Kendalltaurankcorrelation coefficient0.166,p=0.046).
TheuseofrhBMP-2in patientsundergoing 2-levelACDFsignificantly increasestheseverityof dysphagia(dysphagia score)withoutaffecting theoverallincidenceof dysphagia.However,there isnostatistically significantdifferencein theincidenceorseverityof dysphagiabetween patientsundergoing 3-levelor4-levelACDF treatedwithPEEK/rhBMP-2 andthosetreatedwith onlyallograft.Theuseof rhBMP-2appearstoreduce theriskofpseudarthrosis. Thisbenefitismost pronouncedinpatients whoundergo4-levelACDF andaresmokers.
r
e
v
b
r
a
s
o
r
t
o
p
.
2
0
1
7;
5
2(2)
:124–140
133
Table1–(Continued)
n.◦ Authors andYear
Title Journal Sample Mainfindings Conclusion Reasonfor
inclusion/ exclusion
Database
15 HsuWK, Polavarapu M,RiazR, RocGC, StockSR, Glicksman ZS, Ghodasra JH,HsuEL. 2011
Nanocompositetherapy asamoreefficacious andlessinflammatory alternativetobone morphogenetic protein-2inarodent arthrodesismodel
Sourceofthe Document Journalof Orthopedic Research
Thisstudyevaluatesa combinationtherapy (TrioMatrix®;PioneerSurgical, Inc.,Marquette,MI)comprisedof ademineralizedbonematrix (DBM),hydroxyapatite,anda nanofiber-basedcollagenscaffold inarodentspinefusionmodel. Thirty-sixathymicratsthat underwentaposterolateral intertransversespinalfusion wererandomlyassignedto1of5 treatmentgroups:absorbable collagenspongealone(ACS, negativecontrol),10grhBMP-2 onACS(positivecontrol), TrioMatrix®,Grafton®
(Osteotech,Inc.,Eatontown,NJ), andDBX®(Synthes,Inc.,West Chester,PA).
BothTrioMatrix®and rhBMP-2-treatedanimals demonstrated100%fusionratesas gradedbymanualpalpationscores8 weeksafterimplantation.Thisrate wassignificantlygreaterthanthose oftheACS,Grafton®,andDBX® groups.Notably,theuseof
TrioMatrix®asevaluatedbymicroCT quantificationledtoagreaterfusion massvolumewhencomparedtoall othergroups,includingtherhBMP-2 group.T2-weightedaxialMRIimages ofthefusionbeddemonstrateda significanthostresponseassociated withalargefluidcollectionwiththe useofrhBMP-2;thisresponsewas significantlyreducedwiththeuseof TrioMatrix®.
Ourresultstherefore demonstratethata nanocompositetherapy representsapromising, cost-effectivebonegraft substitutethatcouldbe usefulinspinefusions whereBMP-2is contraindicated.
Included SCOPUS
16 AdogwaO, ParkerSL, ShauD, Mendelhall SK,ChengJ, AaronsonO, DevinCJ, McGirtMJ. 2011
Long-termoutcomesof revisionfusionfor lumbarpseudarthrosis: Clinicalarticle
Journalof Neurosurgery: Spine
.Thisisaretrospectivestudyof 47patientswhounderwent revisionlumbararthrodesisfor pseudarthrosis-associatedback pain.Baseline2-yearoutcomes wereassessedusingthe following:visualanalogscale (VAS)forbackpain,Oswestry DisabilityIndex(ODI),Zung Self-RatingDepressionScale, timetonarcoticindependence, timetoreturntowork,EuroQol health-stateutility,andphysical andmentalqualityoflife(Short Form[SF]-12PhysicalandMental ComponentSummaryscores).
Themeandurationoftimebetween priorfusionanddevelopmentof symptomaticpseudarthrosiswas 2.69years.Bonemorphogenetic proteinwasusedin4cases(8.5%)of revisionarthrodesis.Asignificant improvementinVASbackpain (7.31±0.81vs.5.06±2.64,p=0.001), ODI(29.74±5.35vs.25.42±6.0,
p=0.001),andphysicalhealthSF-12 (23.83±6.89vs.27.85±8.90,p=0.001) scoreswasobservedwhen
comparingbaselineand2-year post-revisionarthrodesisscores, respectively,withameancumulative 2-yeargainof0.35quality-adjusted lifeyears.Themediantimeto narcoticsindependencewas12.16 (interquartilerange1.5–24.0)months andthemediantimetoreturnto workwas4months(interquartile range3–5months).By2yearsafter revisionsurgery,nopatientshad experiencedpseudarthrosis.The SF-12MentalComponentSummary (44.72±7.90vs.43.46±7.51,p=0.43) andZungSelf-RatingDepression Scalescores(39.36±7.48vs. 41.39±10.72,p=0.37)werenot significantlyimprovedby2years
Theauthors’study suggeststhatrevision lumbararthrodesisfor symptomatic
pseudarthrosisprovides improvementinlow-back pain,disability,andquality oflife.Revisionlumbar arthrodesisshouldbe consideredaviable treatmentoptionfor patientswith pseudarthrosis-related backpain.Mentalhealth symptomsfrom
pseudarthrosis-associated backpainmaybemore refractorytorevision surgery.
r
e
v
b
r
a
s
o
r
t
o
p
.
2
0
1
7;
5
2(2)
:124–140
Table1–(Continued)
n.◦ Authors andYear
Title Journal Sample Mainfindings Conclusion Reasonfor
inclusion/ exclusion
Database
17 Mannion RJ, Nowitzke AM,Wood MJ.2011
Promotingfusionin minimallyinvasive lumbarinterbody stabilizationwith low-dosebone morphogenicprotein-2 -Butwhatisthecost?
Spine Journal
Studydesign:Prospectiveobservational studyofconsecutivepatients
undergoingminimallyinvasivelumbar interbodyfusionwithpercutaneous pediclescrews.Patientsample:Thirty patientsagedbetween22and78years (mean53years).Outcomemeasures: Thin-slicelumbarcomputed
tomographyscanningwithmultiplanar reconstructionat6and12months postoperative.Methods:Thirty-six spinallevelswereinstrumentedintotal, ofwhichfourunderwentposterior lumbarinterbodyfusionand32 underwenttransforaminallumbar interbodyfusion.Bonegraftharvested locallywasplacedinthediskspacewith low-doseBMP-2(1.4mgperlevel).
Thirty-threeof36spinallevels showedcompletefusionata meanpostoperativescantimeof 7.1months.Twolevels
demonstratedpartialfusionat6 months,whichwascompleteat 12months.Therewasonecaseof nonunionat12months,which alsodemonstratedvertebralbody osteolysis.Despiteverylow-dose BMP-2,twocasesof
asymptomaticheterotopic ossificationwereobserved,and thereweretwocasesof perineuralcystformation,oneof whomrequiredrevisionofthe interbodycage.
TheuseofBMPwith autograftinthedisk spaceduringminimally invasivelumbar interbodyfusionis associatedwithahigh rateofearlyfusion.Even withverylow-doseBMP usedinthisstudy, complicationsrelatedto BMPusagewerenot avoidedcompletely.
Included SCOPUS
18 Mulconrey DS, Bridwell KH,Flynn J,Cronen GA,Rose PS.2008
BoneMorphogenetic Protein(RhBMP-2)asa substituteforiliaccrest bonegraftinmultilevel adultspinaldeformity surgery:Minimum two-yearevaluationof fusion
Spine Prospectiveanalysiswasperformedfor 98patients(308levels;meanage,51.4 years)whounderwentmultilevel anteriororposteriorspinalfusion(PSF) withminimum2-yearfollow-up (average,2.6years).Group1(10mg/level) contained47patients(109levels;2.33 levels/patient)whounderwentanterior spinalfusion(ASF):BMPonan absorbablecollagensponge(ACS)witha titaniummeshcage.Group2
(20mg/level)included43patients(156 levels;3.63levels/patient)withPSF:BMP onanACSwithlocalbonegraft(LBG) andbulkingagent[tricalcium phosphate/hydroxyapatite(TCP-HA)]. Group3(40mg/level)contained8 patients(43levels;5.38levels/patient) withPSF:rhBMP-2andTCP-HAwithno autologousbone.Confoundingnegative factorswerepresentinthestudy population:medicalcomorbidities(26%), tobaccouse(17%),revisionsurgery (34%),previouslaminectomy(51%),and preoperativepseudarthrosis(27%). Postoperativefilms(AP,lateral,oblique) wereevaluatedbyindependent observers.Averagefusiongradewas basedonapublishedscale.
Overallfusionratewas95%. (group191%,group297%,group 3100%).Noconfoundingfactor demonstratedadetrimental statisticalsignificancetofusion.
InmultilevelASF,BMP (10mg/level)generates fusionwithout autogenousbone.In multilevelPSF,BMP (20mg/level)withLBG andTCP-HAproduced fusion.BMP(40mg/level) andTCP-HAwithout LBGachievedfusion.In multilevelspinalfusion, rhBMP-2eliminatedthe necessityforiliaccrest bonegraftandyielded anexcellentfusionrate.
r
e
v
b
r
a
s
o
r
t
o
p
.
2
0
1
7;
5
2(2)
:124–140
135
Table1–(Continued)
n.◦ Authors andYear
Title Journal Sample Mainfindings Conclusion Reasonfor
inclusion/ exclusion
Database
19 Buttermann GR.2007
Prospective nonrandomized comparisonofan allograftwithbone morphogenicprotein versusaniliac-crest autograftinanterior cervicaldiscectomy andfusion
Spine Journal
Purpose:Theobjectiveofthispilot studywastocomparethesuccessof BMPcombinedwithboneallograft withiliacboneautograftinACDF patients.Studydesign/setting:The institutionalreviewboardapproveda prospectivebutnonrandomizedstudy of66consecutivepatientswhohad primaryone-tothree-levelACDFwith eitheriliac-crestboneautograftorBMP allograft(0.9mgBMPperlevel) followedprospectivelyovera2-to 3-yearperiod.Patientsample: Consecutivepatientswhohadprimary one-tothree-levelACDFwitheither iliac-crestboneautograft(n=36)or BMP-allograft(n=30).Patientsinboth iliacbonegraftandBMP-allograft groupshadcomparablepreoperative painanddisability.Outcome measures:Visualanalogscalepain, paindrawing,Oswestryindex,pain medicationuse,opinionoftreatment success,andneurologicalrecovery.
Giventhenonrandomizednature ofthestudy,thestudygroupswere notmatched.Withinthis
limitation,bothgroupsofpatients hadsimilarimprovementinall outcomescales(visualanalogscale pain,paindrawing,Oswestry index,painmedicationuse,and opinionoftreatmentsuccess)and neurologicalrecoveryoverthe2-to 3-yearfollow-upperiod.Patientsin theiliacbonegraftgrouphadtwo pseudarthrosesandtwo complicationsoftheiliac-crest donorsite.IntheBMP-allograft group,onepatienthada pseudarthrosis,but50%hadneck swellingpresentingasdysphagia, whichwassubstantiallymore commonthanthe14%presentin theiliacbonegraftgroup.Patients intheBMP-allograftgrouphad slightlyshortersurgerytime,but implantandhospitalizationcosts werehigher.
ACDFperformedwith BMP(0.9mgBMPper level)allograftisas effectiveasiliacbone graftintermsofpatient outcomesandfusion rates.Safetyconcerns relatedtoneckswelling andhigherinitialcosts wereassociatedwith patientsinthebone morphogenicprotein group.
Included SCOPUS
20 AllenRT, LeeYP, StimsonE, GarfinSR. 2007
Bonemorphogenetic protein-2(BMP-2)inthe treatmentofpyogenic vertebralosteomyelitis
Spine Between2003and2005,14patients whounderwentcircumferentialfusion forPVOwereincludedinthisstudy. Averagepatientagewas54years (range,27–77years).Eight(57%) patientshad3ormorevertebral bodiesinvolved.Diagnosticstudies includedradiographs,CT,MRI,and markersofinfection[(C-reactive protein(CRP),erythrocyte
sedimentationrate(ESR),whiteblood count(WBC)].Allpatientsunderwent anteriorfusionwithrhBMP-2inserted instructuralallograft(11patients)or titaniumcylindricalcages(3patients), followedbyposteriorinstrumented fusionwithautogenousiliaccrestgraft (8occurringonthesameday). Follow-upaveraged22months(range, 11–30months).Allwerestudiedwith plainradiographs,including
flexion-extensionlateralfilmsandfine cutCTscanswithreconstruction.Pain ratingswererecordedbyvisualanalog scores(VAS).
Clinicalresolutionofinfections, normalizationoflabvalues,and bonyfusion,basedondynamic radiographsandCTscans,were seeninallpatientsatlatest follow-up.Staphylococcusaureus wasthemostfrequentlyidentified organism(8patients).Four(29%) patientshadpositiveblood cultures(allMRSA).Predisposing comorbiditieswerepresentin12 patients.Sixpatientshadepidural abscesses.Eight(57%)patients presentedwithneurologicdeficits, rangingfromparaparesisto quadriplegia.Completerecovery wasseenin7(quadriplegia unchanged).At1year,meanVAS painscoresimprovedsignificantly (p<0.05)from7.9(range,3–10)to 2.8(range,0–6).Perioperative complications(non-BMPrelated) occurredin2patients.Therewere nosurgically-relateddeaths.
rhBMP-2use,in combinationwith antibioticsand circumferential instrumentedfusion, providesasafeand successfulsurgical treatmentofmedically nonresponsivePVO, withsolidfusions obtained,goodclinical results,andnoadverse sideeffectsfromthe BMP.
r
e
v
b
r
a
s
o
r
t
o
p
.
2
0
1
7;
5
2(2)
:124–140
Table1–(Continued)
n.◦ Authors andYear
Title Journal Sample Mainfindings Conclusion Reasonfor
inclusion/ exclusion
Database
21 UFurlan JC,Perrin RG, Govender PV, Petrenko Y, Massicotte EM, Ram-persaud YR,Lewis S,Fehlings MG.2007
Useofosteogenic protein-1inpatients athighriskforspinal pseudarthrosis:A prospectivecohort studyassessing safety,health-related qualityoflife,and radiographicfusion
Journalof Neuro-surgery: Spine
Outcomemeasuresincluded documentationofadverseevents, radiographicevaluationoffusionbyan independentmusculoskeletal radiologistblindedtotreatment,the OswestryDisabilityIndex(ODI),and the36-ItemShortFormHealthSurvey (SF-36).Thehealth-relatedqualityof life(HRQOL)assessments(ODIand SF-36)weregivenatbaselineandat3, 6,12,18,and24monthsafterthe surgicalOP-1implant.
Thestudyconsistedof17maleand13 femalepatients,withameanageof53years (range20–77years).Fourteenpatients underwentoperationsforcervicaldisease, and16forlumbardisease,withamedian postoperativefollow-upof24months(range 13–46months).Thereweresignificant improvementsinthephysicalhealth(from 28.7±1.5to34.2±3;p=0.025)andmental health(from43.7±2to47.5±3.1;p=0.015) summaryscoresontheSF-36.Themean postoperativeODIscoreat6,9,12,and18 monthswassignificantlylowerthanthe baselineODIscore,aftertakinginto considerationa10-pointmeasurementerror (p=0.0003,p=0.003,p=0.004,andp=0.032, respectively).At24months,however,the differencesinODIscoreswerenolonger significant.Ofthe30patients,24(80%)were deemedtohaveasolidfusion.Therewere noallergicreactionstoOP-1andno symptomaticpostoperativehematomas.
Ourresultssuggestthat theuseofOP-1issafe andmaycontributeto highfusionrates,as demonstratedby radiographs,reduced levelsofdisability,and improvedHRQOLin patientsconsideredto beatahighriskfor developinganonunion afterspinal
reconstructivesurgery.
Included SCOPUS
22 Lawrence JP,Waked W,Gillon TJ,White AP,Spock CR,Biswas D, Rosen-bergerP, TroianoN, AlbertTJ, GrauerJN. 2007
rhBMP-2(ACSand CRMformulations) overcomes pseudarthrosisina NewZealandwhite rabbitposterolateral fusionmodel
Spine Seventy-twoNewZealandwhite rabbitsunderwentposterolateral lumbarfusionwithiliaccrest autograft.Toestablishpseudarthroses, nicotinewasadministeredtoall animals.At5weeks,thespineswere exploredandallpseudarthroseswere redecorticatedandimplantedwithno graft,autograft,rhBMP-2/ACS,or rhBMP-2/CRM.At10weeks,fusions wereassessedbymanualpalpation andhistology.
Eightrabbits(11%)werelostto complications.At5weeks,66(97%)had pseudarthroses.At10weeks,attempted pseudarthrosisrepairswerefusedin1of16 ofnograftrabbits(6%),5of17autograft rabbits(29%),and31of31rhBMP-2rabbits (withACSorCRM)(100%).Histologic analysisdemonstratedmorematurebone formationintherhBMP-2groups.
The2rhBMP-2 formulationsledto significantlyhigher fusionratesand histologicbone formationthannograft andautograftcontrols inthispseudarthrosis repairmodel.
Included SCOPUS
23 WhiteAP, MaakTG, PrinceD, Vaccaro AR,Albert TJ, Hilibrand AS,Grauer JN.2006
Osteogenicprotein-1 inducedgene expression: Evaluationina posterolateralspinal pseudarthrosis model
Spine Messengerribonucleicacidwas isolatedfromnicotine-exposedNew Zealandwhiterabbitlumbar pseudarthrosesfollowingattempted nograft,autograft,andosteogenic protein-1pseudarthrosisrepairs. Reversetranscriptasepolymerase chainreactionwasusedtoassessthe expressionofangiogenin,
angiopoietin,intercellularadhesion molecule,platelet-derivedgrowth factor-,vascularendothelialgrowth factor,bonemorphogeneticproteins2 and7,typeIcollagen,andosteonectin. Glyceraldehyde-3-phosphate
dehydrogenasewasusedasa constitutivelyexpressedcontrol.
Levelsofgeneexpressionintheosteogenic protein-1groupwerehigherthanthoseof theautograftgroup,whichwerehigherthan thenograftgroupforthemajorityofthe genesstudied.
Intherabbit
pseudarthrosismodel, geneexpressiondata supportedthe hypothesisthat successful
pseudarthrosisrepairis relatedtotheinduction ofosteogenicand angiogeniccytokinesby osteogenicprotein-1.
rev bras ortop.2017;52(2):124–140
137
(approvedforanteriorlumbarinterbodyfusions–ALIF)and rhBMP-7 (has received a humanitarian device exemption approvalforrepairoflumbarpseudarthrosis).
ByJulyof2002,theFDAapprovedtheuseofrhBMP-2 com-binedwithabiologiccarrierofcollagen(bovinetypeIcollagen) asasubstituteforsinglelevelALIF.1,2,4–6AccordingtoNadyala
etal.7therhBMPsarecurrentlythemosteffective
osteobio-logicagentstoincreasetherateofarthrodesisbutareoften usedasanofflabelapplication.Mulconreyetal.1describes
sustainableresultsofsuccess,bymultiplecenters, demon-stratingtobesuperiortoICBGforALIF.Itsusehadarapidly increasingintheUnitedStates,despitetheinitialhighcosts.5
ThestudyofKlimoetal.8hasdemonstratedthatthefusion
processusingrhBMP-2isadynamicone,withosteolysis dom-inatingtheinitialphase,leadingtoend-plateresorptionand consequentlylossofsomeofthediskspaceheightand sag-ittalalignmentthatwasachievedwithsurgery.TherhBMP-7 hasbeen documented as apotential treatment alternative fordifferentdiseases,includingbonedisease,stroke, inflam-matory bowel disease, prostate cancer, and chronic renal disease.9 More explicitly, rhBMP-7 plays an important role
inboneformationbyinducingdifferentiationofpluripotent mesenchymalcellsintoactiveosteoblasts,Furlanetal.9
con-cludesthatitcaninduceastable,mature,posterolateralspinal fusionmassmorerapidlythananautologousbonegraft,and theresultingfusionmassmaybebiomechanicallystifferin theearlystages(upto3months)ofhealing.
BMP had a 98% vs. ICBG 76% offusion rate, once been extendedits use to off labelposterior spinal fusion, ante-rior/posteriorcervicalfusion.ToMulconreyetal.1atasingle
levelresearchof2years,BMPdemonstrate asuperior pos-terolateralspinal fusionrate (88%) than ICBG (73%). Those patientshaddecreasedbloodloss,shorterlengthofsurgery andshorterhospitalstay.1,10 AccordingtoHoffmannet al.5
rhBMP-2ismoreeffectivewitha reductioninradiographic nonunioncomparedwithBMP-7,demineralizedbonematrix, andactivatedgrowthfactor.
Itmustbeevaluatedallthevariablesinthespinalfusion, the detrimental factors to fusion are medical comorbidi-ties,tobacco use, preoperativepseudarthrosis, preoperative laminectomy,age,increasingnumberofsurgicallevels. Oth-ersareosteoporosis,minimallocalbonegraft,previousand longfusion.1Failureshavebeenattributedtopoorvascularity
ofascarredfusionbedandpersistenceofsystemicinhibitors, suchasnicotine.11ToFurlanetal.9thepopulationatriskfor
aspinalnonunionarepatientswithconnectivetissue disor-ders,individualswithahistoryofmajordiseasesthatcould adverselyaffectbonehealing,patientsreceivingmedications thatnegatively affectbonehealing,patients withahistory ofpreviousnonunion fusions, and/orpatientswithlimited availabilityorpoorqualityofautogenousbonegraft.
Singh et al.4 and Hsu et al.12 emphasizes that
apply-ing BMP is not without risk, the FDA in 2008 issued a public health warning to its use in cervical spine fusion alertingtowoundcomplications,dysphonia,dysphagiaand ectopic boneformation. Inthe lumbarspine, reports have demonstratedradiculitis,pseudarthrosis,seroma/hematoma formation, and heterotopic ossification with rhBMP-2 use. Apprehensionaboutitspro-oncogenicpotentialhaslimited
its use in the pediatric population, although this trend may be changing.2,5,12 Both Singh et al.4 and Hoffmann
et al.5 groupstheorizesthatthe lackofpostoperativedead
spaceinMinimallyinvasivetransforaminallumbarinterbody fusion(MIS-TLIFs)surgerymayleadtoaninflammatorystate because of the high concentration of BMP-2, resulting in edemaandseroma,theoreticallyinducingradiculitis, verte-bralosteolysisandneuroforaminalbonegrowth.4,5
Pyogenic vertebral osteomyelitis is oneofless common complicationsafterspinalfusion,presentlateorinpatients withmultiplemedicalmorbiditiessuchasdiabetes, HIVor rheumatoidconditions;theuseofBMPstocorrectthishostile environmentofpyogenicinfectionitisproveneffective man-agedbycircumferentialinstrumentedfusionincombination withantibiotics,accordingtoAllenetal.13ithasgoodevidence
ofbonyfusion,noinfectionrecurrenceandthepatientshad clinicalimprovement.
Hoffmannetal.5affirmsthatthereisnosignificant
authen-ticimmunologicantibodyresponsetorhBMP-2ortypeIbovine collagen,andthereexposuredoesnotleadtoasymptomatic antibodyformationaccordingtoserologytesting.
Pseudoarthrosis occur when the fusion attempt fails, a solid fusion isnot achieved, or thereis motionacross the segment leadingtoit,andit canbeclinicallysymptomatic as pain, deformity, neurocompressionor hardware failure. Therisksfactors are:osteoporosis, cervical kyphotic defor-mity,revisionfusionsurgery,multilevelsurgery,orahistory ofsmoking.10Adogwaetal.14suggeststhatrevisionsurgeryof
lumbararthrodesisforsymptomaticpseudarthrosisisaviable treatmentthatimproveslow-backpain,disabilityandquality oflife.Pseudarthrosisafterspinefusionleadstopoorclinical outcomesandasignificantcosttopatientsandthehealthcare system.12
ThestudyofLuetal.10saysitisinterestingtonotethat
amajority(63%)oftheallograftcohortpatientswho exhib-itedpseudarthrosisweresmokers, whereasall thepatients whowereintheBMPgrouphadasolidfusionregardlessof smoking status.Theuse ofrhBMP-2appearstoreducethe riskofpseudarthrosis,but this benefitismostpronounced inpatientstreatedwith4-levelanteriorcervicaldiscectomy fusion(ACDF)whoaresmokers.
Pseudoarthrosisisoneofthemostcommoncomplications after long adultspinal fusion to the sacrum and typically occurs at the thoracolumbar and lumbosacral junctions.15
Is a majorlimitation ofmultilevel anterior cervical fusion, traditionaltechniques havea20% ofpatientswho develop pseudarthrosis,onestrategyusedtohelpdecrease therate ofitistohaveposteriorinstrumentationtoincreasethe rigid-ityoftheconstruct,howeveritaddsmorbiditybyincreasethe timeofsurgery.Frenkeletal.16demonstratethatBMPusage
inanteriorcervical approachhasalmost100%rateofsolid arthrodesisregardlessoflevel, but its study does nothave statisticalsignificance.
AccordingtoSinghetal.46.8%ofpatientswhounderwent
patientswithahighprevalenceofsmokerscomparedwith theoneswhodidnotneedrevision(41.3%vs.26.7%,p<.054). Theneedforreviewprocedureforthosepatientscostsan aver-ageof$20,267(Americandollars)ofhospitaldirectcostsand physiciancharges.
PseudarthrosisatL5–S1isoneofthemostcommon com-plicationsoflong fusionstothesacruminadultdeformity surgery.Strategiesfordecreasingitincludeinterbodyfusion, use of BMP-2 at the lumbosacral junction, and the use of sacro-pelvicfixation, individually or in combination.17 The
repairin the lumbar spinepresents a challenging surgical problemwithhighfailureratesbeenreported,resultingfrom poorvascularityinascarredfusionbed,inadequateposterior bonysurfacearea,lossofsagittal alignment,and exposure toadversesystemicfactors suchasnicotine.Higherfusion rates were noted with rhBMP-7than autograftin this set-ting (82% vs. 42%) in those cases. Another potential bone graftalternativethathasbeenextensivelystudiedisrhBMP-2, demonstratedbyLawrenceetal.18toovercometheinhibitory
effectsofnicotine inamodelofprimaryspinalfusionand appearstobeaneffectivealternativeinitspreclinicalmodel forascenariowithinnumerousriskfactorsforpseudarthrosis repair.
Futurestudiesshouldbeconductedtoelucidatethe under-lying control over the observed gene expression involved inpseudarthrosis,theexpressionofcertainosteogenicand angiogenicgenesthathavebeenpreviouslydemonstratedto beinhibitedbynicotine.FortheWhiteetal.11 modelithad
up-regulationintheimplantationofosteogenicprotein-1at thepseudarthrosissite.Geneexpressiondatasupportedthe hypothesisthatthediscrepancyinfusionsuccessmaybedue toosteogenicprotein-1’sabilitytoup-regulateosteogenicand angiogeniccytokinesrequiredforfusion,and,thus,overcome nicotine’sinhibitionoflocalgeneexpression.
AccordingtoMulconreyetal.1rhBMP-2hastheabilityto
createsolidfusioninthepresenceofnegativevariablesand inmultilevelspinalfusion,eliminatingthenecessityforiliac crestbonegraft,toHoffmannetal.5non-unionratesinlumbar
spinefusionwithrhBMP-2arelow,ahighdosage(>12mg)is associatedwithhigherchanceofpostoperativeseromaand infectionrequiringinvasiveintervention,suchasreutilization ofit.
Frenkeletal.16indicatesthatcervicalfusionapproachwith
BMP its possible without increase in complication rates if usinglowerdosesofBMP,followingthesafetyconcernofthe FDAnotification,anymultilevelanteriorcervicalprocedure, evenwithoutBMP, canleadtodysphagiaandairway prob-lems.AlthoughaccordingtoLuetal.10theuseofrhBMP-2in
patientsundergoing2-levelACDFsignificantlyincreasesthe severityofdysphagia,withoutaffectingtheoverallincidence ofit.MIS-TLIFsshowedneuralcompromisebyacaseseries evaluated,1 althoughrhBMP-2iseffectiveforarthrodesisin
theunilateralMIS-TLIFthecomplicationofthisoff-labelusage are present – neuroforaminal bone growth, osteolysis and pseudarthrosis.4
Kim et al.15 confirms that BMP is superior to ICBG in
achievingfusioninlongconstructsinadultdeformitysurgery. The rate of pseudarthrosis was significantly higher in the ICBGgroupthanBMPgroup,theconcentrationanddosageof
rhBMP-2usedseemstohaveaneffectontherateoffusion and pseudarthrosisratebecause nopatient receivingmore than5mgperlevelhadapparentordetectedpseudarthrosis (n=20/20).
ToButtermann19(2008)BMPseemstohavegreater
indica-tioninpatientshavingthree-orgreater-levelACDF,patients whoareundergoingrevision,patientswhohavemorbid obe-sityordiabeticsandareatriskofbonegraftsitecomplications, andpatientswhohaveosteoporosisinwhichtheiliac-crest bonegraftitselfmaybesubjecttocollapseorexhibitsarisk ofsubsidence.
VeilleteandMcKee6agreethatforlumbarspinefusionthe
useofBMPshowedanincreasedfusionrate,withadecrease ofrevisionproceduresinthesameperiod,butithasno corre-lationwithdecreaseintheuseofICBGandtheuseofBMP correlates withsubstantial increaseinhospitalchargers. It mayquestionfinancialjustification.Kimetal.15justifythat
forlongfusionstothesacrumBMPusesignificantlydecreases pseudarthrosis ratesinthis patient populationwhen com-paredwithICBGalone.WhichcorroborateswithAnnisetal.17
studywheretheuseoflowdoseofBMP-2attheL5–S1levelin combinationwithsacro-pelvicfixationachievedsatisfactory fusionratesinadultdeformitysurgery.
Currently, most ofthe burdenof the increasedcosts is bornebythehospitalsandsurgeonproviders.However,over the longterm,thecostsmaybesimilarandhaveyettobe determined conclusively.19 Thefuture market forBMP-2in
lumbarfusionsurgerywilldependontheclinicalsignificance ofincreasedfusioninthecontextofpossiblesideeffectsand costconsiderations,aswellasthepotentialarrivalofnewer and saferfusion-promotingagents.20ToFrenkeletal.16 the
BMP-grouphasafasterfusionprogressina3-monthfollow-up thaninnon-BMPgroup.
Theefficacy ofTLIF with BMP issupportedinthe large series withlong-termfollow-up ofCrandalet al.21 Reliable
fusion and improved outcomes can be expected in adults undergoingTLIFfordeformity,spondylolisthesis,and degen-erativedisease.Mostcomplicationsoccurredinpatientswith deformity.
Furlanetal.9resultssuggestthattheuseofrhBMP-7issafe
andmaycontributetohighfusionrates,asdemonstratedby radiographs,reducedlevelsofdisability,andimprovedquality oflifeinpatientsconsideredtobeatahighriskfordeveloping anonunionafterspinalreconstructivesurgery.AtTheologis etal.22studyshowsnodifferenceinoutcomesbetween
rev bras ortop.2017;52(2):124–140
139
Crandalletal.23 five-yearfollow-upafterTLIFwithBMP,
confirmseffectivearthrodesisinshortandlongfusions,both primaryandrevisionsurgeries.Mostcomplicationsoccurred indeformitypatients,theBMP-relatedones(seroma,ectopic bone)wererare.
EvenwithverylowdoseBMPusedinthestudyofMannion etal.20complicationsrelatedtoBMPusagewerenotavoided
completely,itwasobservedasymptomaticheterotopic ossi-ficationand twocasesofperineuralcystformation, oneof whomrequiredrevision.Hoffmannetal.5pointsouttheneed
of additional research to determine dose dependency and geneticpredispositiontoreacttoBMPs,suchasover(ectopic boneandseroma)orunderreaction(nonunion).
Final
remarks
OurreviewshowsthattheuseofBMPsiseffectiveandsecure comparedto ICGB, but depending ofthe location ofusage (cervicalspine,lumbarspineorsacrum)andthemedical sta-tusofthepatient(presenceofcomorbidities,tobaccousage) its moreprobabletoexhibit complications,such as neuro-foraminalbone growth,osteolysis, pseudarthrosis, seroma, hematoma.ThisdatadeterminethattheusageofBMPsmust beanagreementbetweenpatientandphysician,aninformed decisiondiscussing thebenefits and risksofBMP foreach case.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1. MulconreyDS,BridwellKH,FlynnJ,CronenGA,RosePS.Bone MorphogeneticProtein(RhBMP-2)asasubstituteforiliac crestbonegraftinmultileveladultspinaldeformitysurgery: minimumtwo-yearevaluationoffusion.Spine(PhilaPa 1976).2008;33(20):2153–9.
2. DagostinoPR,WhitmoreRG,SmithGA,MaltenfortMG,Ratliff JK.Impactofbonemorphogeneticproteinsonfrequencyof revisionsurgery,useofautograftbone,andtotalhospital chargesinsurgeryforlumbardegenerativedisease:reviewof thenationwideinpatientsamplefrom2002to2008.SpineJ. 2014;14(1):20–30.
3. LinaIA,PuvanesarajahV,LiauwJA,LoS-L,Santiago-Dieppa DR,HwangL,etal.Quantitativestudyofparathyroid hormone(1-34)andbonemorphogeneticprotein-2onspinal fusionoutcomesinarabbitmodeloflumbardorsolateral intertransverseprocessarthrodesis.Spine(PhilaPa1976). 2014;39(5):347–55.
4. SinghK,NandyalaSV,Marquez-LaraA,ChaTD,KhanSN, FinebergSJ,etal.ClinicalsequelaeafterrhBMP-2useina minimallyinvasivetransforaminallumbarinterbodyfusion. SpineJ.2013;13(9):1118–25.
5. HoffmannMF,JonesCB,SietsemaDL.Complicationsof rhBMP-2utilizationforposterolaterallumbarfusions requiringreoperation:asinglepractice,retrospectivecase seriesreport.SpineJ.2013;13(10):1244–52.
6.VeilletteCJH,McKeeMD.Growthfactors–BMPs,DBMs,and buffycoatproducts:arethereanyprovendifferences amongstthem?Injury.2007;38Suppl.1:S38–48.
7.NandyalaSV,Marquez-LaraA,FinebergSJ,PeltonM,SinghK. Prospective,randomized,controlledtrialof
silicate-substitutedcalciumphosphateversusrhBMP-2ina minimallyinvasivetransforaminallumbarinterbodyfusion. Spine(PhilaPa1976).2014;39(3):185–91.
8.KlimoPJr,PeelleMW.Useofpolyetheretherketonespacer andrecombinanthumanbonemorphogeneticprotein-2in thecervicalspine:aradiographicanalysis.SpineJ. 2009;9(12):959–66.
9.FurlanJC,PerrinRG,GovenderPV,PetrenkoY,MassicotteEM, RampersaudYR,etal.Useofosteogenicprotein-1inpatients athighriskforspinalpseudarthrosis:aprospectivecohort studyassessingsafety,health-relatedqualityoflife,and radiographicfusion.JNeurosurgSpine.2007;7(5): 486–95.
10.LuDC,TumialánLM,ChouD.Multilevelanteriorcervical discectomyandfusionwithandwithoutrhBMP-2:a comparisonofdysphagiaratesandoutcomesin150patients –clinicalarticle.JNeurosurgSpine.2013;18(1):43–9.
11.WhiteAP,MaakTG,PrinceD,VaccaroAR,AlbertTJ,Hilibrand AS,etal.Osteogenicprotein-1inducedgeneexpression: evaluationinaposterolateralspinalpseudarthrosismodel. Spine(PhilaPa1976).2006;31(22):2550–5.
12.HsuWK,PolavarapuM,RiazR,RocGC,StockSR,Glicksman ZS,etal.Nanocompositetherapyasamoreefficaciousand lessinflammatoryalternativetobonemorphogenetic protein-2inarodentarthrodesismodel.JOrthopRes. 2011;29(12):1812–9.
13.AllenRT,LeeY,StimsonE,GarfinSR.Bonemorphogenetic protein-2(BMP-2)inthetreatmentofpyogenicvertebral osteomyelitis.Spine(PhilaPa1976).2007;32(26): 2996–3006.
14.AdogwaO,ParkerSL,ShauD,MendelhallSK,ChengJ, AaronsonO,etal.Long-termoutcomesofrevisionfusionfor lumbarpseudarthrosis:clinicalarticle.JNeurosurgSpine. 2011;15(4):393–8.
15.KimHJ,BuchowskiJM,ZebalaLP,DicksonDD,KoesterL, BridwellKH.RhBMP-2Issuperiortoiliaccrestbonegraftfor longfusionstothesacruminadultspinaldeformity.Spine (PhilaPa1976).2013;38(14):1209–15.
16.FrenkelMB,CahillKS,JavaharyRJ,ZacurG,GreenBA,LeviAD. Fusionratesinmultilevel,instrumentedanteriorcervical fusionfordegenerativediseasewithandwithouttheuseof bonemorphogeneticprotein.JNeurosurgSpine.
2013;18(3):269–73.
17.AnnisP,BrodkeDS,SpikerWR,DaubsMD,LawrenceBD.The fateofL5–S1withlow-doseBMP-2andpelvicfixation,withor withoutinterbodyfusion,inadultdeformitysurgery.Spine (PhilaPa1976).2015;40(11):E634–9.
18.LawrenceJP,WakedW,GillonTJ,WhiteAP,SpockCR,Biswas D,etal.rhBMP-2(ACSandCRMformulations)overcomes pseudarthrosisinaNewZealandwhiterabbitposterolateral fusionmodel.Spine(PhilaPa1976).2007;32(11):
1206–13.
19.ButtermannGR.Prospectivenonrandomizedcomparisonof anallograftwithbonemorphogenicproteinversusan iliac-crestautograftinanteriorcervicaldiscectomyand fusion.SpineJ.2008;8(3):426–35.
20.MannionRJ,NowitzkeAM,WoodMJ.Promotingfusionin minimallyinvasivelumbarinterbodystabilizationwith low-dosebonemorphogenicprotein-2–butwhatisthecost? SpineJ.2011;11(6):527–33.
degenerativedisease–part1:largeseriesdiagnosisrelated outcomesandcomplicationswith2-to9-yearfollow-up. Spine(PhilaPa1976).2013;38(13):1128–36.
22.TheologisAA,TabaraeeE,LinT,LubickyJ,DiabM.Typeof bonegraftorsubstitutedoesnotaffectoutcomeofspine fusionwithinstrumentationforadolescentidiopathic scoliosis.Spine(PhilaPa1976).2015;40(17):1345–51.
23.CrandallDG,RevellaJ,PattersonJ,HuishE,ChangM, McLemoreR.Transforaminallumbarinterbodyfusionwith rhBMP-2inspinaldeformity,spondylolisthesis,and degenerativedisease–part2:BMPdosage-related