JPediatr(RioJ).2016;92(5):429---431
www.jped.com.br
EDITORIAL
Predictors
of
dengue
severity
夽
,
夽夽
Preditores
de
gravidade
da
dengue
Scott
B.
Halstead
UniformedUniversityoftheHealthSciences,DepartmentofPreventiveMedicineandBiometrics,Bethesda,UnitedStates
Pone et al., in a study published in this Journal, have attemptedtoidentifyhistoricalorobservablesignsor symp-toms thatreliablypredict worseningof denguediseasein children.1Insodoing,theyhavecoinedanewterm‘‘serious
dengue disease’’ and adopted a new clinical outcome metric, ‘‘treatment modality.’’ The ‘‘treatment modali-ties’’chosenincludeadministrationof‘‘amines,inotropes, colloids, mechanical ventilation, non-invasive ventilation, peritoneal dialysis or hemodialysis.’’ Lethargy, abdominal distension,pleuraleffusion,andhypoalbuminemiawerethe mostreliable markersofseriousdenguediseaseidentified in145childrenhospitalizedinRiodeJaneiroin2007---2008, whohaddirectorindirectevidenceofrecentdengue infec-tion.The authorsare amongthosewhowould agree that amoreaccurateidentification ofdenguepredictors would bestbederivedfromlargeprotocol-basedprospective stud-ies of physiologically characterized laboratory confirmed dengueillnesses.
There is considerable historical precedent for this effort.Ever sincethe 1950s,whenit wasrecognizedthat denguevirusescausedasevereandoftenfatalacutefebrile diseaseofchildren,it hasbeen thegoalofresearchersto describethe pathophysiologyof denguedisease aimingto provide better treatment and to identifypredictive early warning markers toimprove triage.2,3 This wasthe
moti-vationbehindthecreationof thecasedefinitions,dengue hemorrhagic fever/dengue shock syndrome (DHF/DSS), in wide use since their adoption by WHO in 1975, and the new case definitions introduced in 2009.4,5 In the 1960s,
夽 Please cite this article as: HalsteadS. Predictors of dengue
severity.JPediatr(RioJ).2016;92:429---31.
夽夽VerartigodePoneetal.inpages464---71. E-mail:halsteads@erols.com
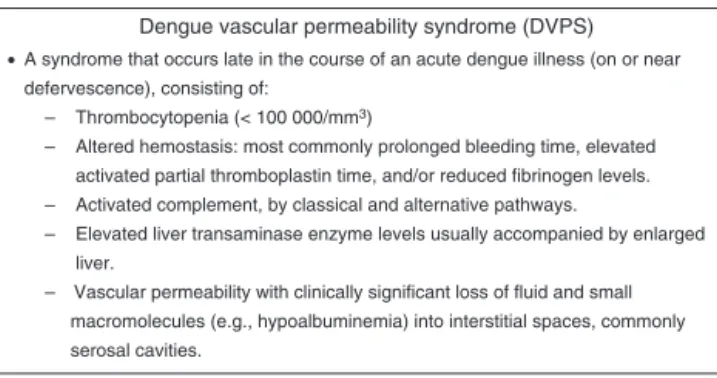
dengue research programs in Southeast Asia found that children were dying of a new clinical entity, the dengue vascularpermeabilitysyndrome (DVPS;Fig.1), character-ized by a complex of physiologic abnormalities affecting multiple organ systems including the liver, blood coagu-lation, complement, hematopoiesis, serum proteins, and the vascular system that reach a maximal expression at defervescence.3,6---10 It soon was well understood that
children with DVPS benefitted from early, physiologically relevantfluidresuscitation.6Itwasalsoobservedthatthe
fluid leak varied in severity from child to child and that aphysiologicallyirreversiblepenaltymightoccur injusta matterofhoursduetofailuretomaintainadequateblood volume.5,11---13
ThesignsandsymptomsofdengueandDVPSchangefrom daytoday.Thosethatprecedeshockhavebeenidentifiedas ‘‘warningsigns.’’Warningsignsofdengueinfectionswere describedlongago.SilerandSimmons,whorecordeddaily clinicalandlaboratoryfeaturesofseveralhundred experi-mentaldengueillnessesmostlyinseronegativeyoungadult maleUSArmyvolunteers,observedaprofoundmid-illness dengueleukopenia.14,15 More importantly,they found this
leukopenia consisted of two components, a reduction in circulatinglymphocytesandadestructionofmature poly-morphonuclearleukocytes.Thelatterproducedadiagnostic ‘‘cross,’’wheretherewere greaternumbers of immature thanmaturepolysinbloodsmears.15Ithasbeenspeculated
thatleukopeniaandthrombocytopeniamightberelatedto aremarkablephenomenonthatregularlyoccursindengue infectionsbeforetheonsetoffever,aprofoundsuppression ofallcellularelementsinthebonemarrow.16,17InThailand,
threeearlywarningsignswereusedinpatienttriage: throm-bocytopenia and a positive tourniquet test were thought toherald dengue vascular permeability, while a fingertip microhematocrit was taken to establish a baseline value
http://dx.doi.org/10.1016/j.jped.2016.06.004
430 HalsteadSB
Dengue vascular permeability syndrome (DVPS)
•A syndrome that occurs late in the course of an acute dengue illness (on or near defervescence), consisting of:
– Thrombocytopenia (< 100 000/mm3)
– Altered hemostasis: most commonly prolonged bleeding time, elevated activated partial thromboplastin time, and/or reduced fibrinogen levels. – Activated complement, by classical and alternative pathways.
– Elevated liver transaminase enzyme levels usually accompanied by enlarged liver.
– Vascular permeability with clinically significant loss of fluid and small macromolecules (e.g., hypoalbuminemia) into interstitial spaces, commonly serosal cavities.
Figure1 Denguevascularpermeabilitysyndrome(DVPS).
tomonitorhemoconcentration.18Becauseplateletnumbers
decline and hematocrits rise quickly, multiple measure-mentsmustbeperformedanddiseaseseverityeventuallyis mostaccuratelyscoredusingmodalhighorlowvalues.Some workersfoundthathighlevelsofaspartateaminotransferase identifiedthosechildrenwhoproceededtoDVPS.18Careful
physiologicalcharacterizationofdengueillnessesinchildren hasresulted in significant improvement in treatment and sharplyreducedcasefatalityrates.11,19
There has been considerable disagreement about the utility of most warning signs or laboratory tests in wide useforpredictingtheoutcomeofdengueinfections.20 One
approachtoidentifypredictorshasbeentolookforuniversal componentsin DSS. A meta-analysisidentified the signifi-cantassociationsofshockasage,femalesex,neurological signs, nausea/vomiting, abdominal pain, gastrointestinal bleeding, hemoconcentration, ascites, pleural effusion, hypoalbuminemia, hypoproteinemia, hepatomegaly, levels ofalaninetransaminaseandaspartatetransaminase, throm-bocytopenia,prothrombintime,activatedpartial thrombo-plastintime,fibrinogenlevel,primary/secondaryinfection, andDENV-2.21Thevastexpansionofdengueinfection
glob-allyhasplacedgreatstressonclinicalfacilities,generating further efforts to improve patient triage by validating early warningsigns.22---25 One such study willenroll
7000---8000 children with a febrile disease who are admitted to outpatient departments in eight dengue-endemic countries.22 Thislarge prospectivestudy,nowinprogress,
includes three sites in Brazil. As of December 2015, a totalof7096participantshadbeen enrolled,withdengue confirmed in 2510/5996 (42%). Enrolment will continue until June 2016. It is hoped that sufficient numbers of children withacute dengue infections will proceed on to severedengue,providingunequivocallaboratoryorclinical predictors,specificallyforDSS.
Conflicts
of
interest
Theauthordeclaresnoconflictsofinterest.
References
1.PoneSM,HökerbergYH,deOliveiraRV,DaumasRP,PoneTM, PoneMV,etal.Clinicalandlaboratorysignsassociatedto seri-ousdenguediseaseinhospitalizedchildren.JPediatr(RioJ). 2016;92:464---71.
2.QuintosFN,LimLE,JulianoL,ReyesA,LacsonP.Hemorrhagic feverobservedamongchildreninthePhilippines.PhilippinJ Pediatr.1954;3:1---19.
3.HalsteadSB,CohenSN.Denguehemorrhagicfeverat60years: earlyevolutionofconceptsofcausationandtreatment. Micro-biolMolBiolRev.2015;79:281---91.
4.WorldHealthOrganization(WHO).Technicalguidesfor diagno-sis,treatment,surveillance,preventionandcontrolofdengue haemorrhagicfever.Geneva:WHO;1975.
5.World Health Organization (WHO). Dengue: guidelines for diagnosis,treatment prevention and control.Geneva: WHO; 2009.
6.CohenSN,HalsteadSB.Shockassociated withdengue infec-tion. I. Clinical and physiologic manifestations of dengue hemorrhagic fever in Thailand, 1964. J Pediatr. 1966;68: 448---56.
7.WeissHJ,HalsteadSB.Studies ofhemostasis inThai hemor-rhagicfever.JPediatr.1965;66:918---26.
8.Pathogeneticmechanismsindenguehaemorrhagicfever:report ofaninternationalcollaborativestudy.BullWorldHealthOrgan. 1973;48:117---33.
9.BokischVA, TopFH Jr,Russell PK,DixonFJ, Müller-Eberhard HJ.The potentialpathogenicrole ofcomplement indengue hemorrhagic shock syndrome. N Engl J Med. 1973;289: 996---1000.
10.Halstead SB. Pathogenesis of dengue: dawn of a new era. F1000Research. 2015;4:F1000 Faculty Rev-1353. doi:10.12688/f1000research.7024.1.
11.NimmannityaS.Clinicalspectrumandmanagementofdengue haemorrhagicfever.SoutheastAsianJTropMedPublicHealth. 1987;18:392---7.
12.WorldHealthOrganization(WHO).Denguehaemorrhagicfever: diagnosis,treatment,preventionand control.2 ed.Geneva: WHO;1997.
13.World Health Organization (WHO). Guidelines for treatment of dengue/dengue haemorrhagic fever in small hospitals. New Delhi: WHO Regional Office for South East Asia; 1999.
14.SilerJF,HallMW,HitchensAP.Dengue:itshistory,epidemiology, mechanismof transmission,etiology,clinical manifestations, immunity,andprevention.PhilippineJSci.1926;29:1---304.
15.SimmonsJS,StJohnJH,ReynoldsFH.Experimentalstudiesof dengue.PhilippineJSci.1931;44:1---252.
16.NelsonER,BiermanHR,ChulajataR.Hematologicfindingsin the1960hemorrhagicfeverepidemic(dengue)inThailand.Am JTropMedHyg.1964;13:642---9.
17.Bierman HR, Nelson ER.Hematodepressive virus diseases of Thailand.AnnInternMed.1965;62:867---84.
18.Kalayanarooj S, Vaughn DW, Nimmannitya S, Green S, SuntayakornS, Kunentrasai N, et al. Early clinicaland lab-oratory indicators of acute dengue illness. J Infect Dis. 1997;176:313---21.
19.Kalayanarooj S. Clinical manifestations and management of dengue/DHF/DSS.TropMedHealth.2011;39:83---7.
20.Horstick O, Farrar J, Lum L, Martinez E, San Martin JL, EhrenbergJ,etal.Reviewingthedevelopment,evidencebase, andapplicationofthereviseddenguecaseclassification.Pathog GlobHealth.2012;106:94---101.
21.Huy NT, VanGiang T, ThuyDH, Kikuchi M,Hien TT, Zamora J, et al. Factors associated with dengue shock syndrome: a systematic review and meta-analysis. PLoS NeglTrop Dis. 2013;7:e2412.
22.JaenischT,TamDT,KieuNT,VanNgocT,NamNT,VanKinhN, etal.Clinicalevaluationofdengueandidentification ofrisk factorsforseveredisease:protocolforamulticentrestudyin 8countries.BMCInfectDis.2016;16:120.
Predictorsofdengueseverity 431
transmissionbyevidence-basedconsensus.PLoSNeglTropDis. 2012;6:e1760.
24.BhattS,GethingPW,BradyOJ,MessinaJP,FarlowAW,Moyes CL,etal.Theglobaldistributionandburdenofdengue.Nature. 2013;496:504---7.