SOCIEDADE BRASILEIRA DE ORTOPEDIA E TRAUMATOLOGIA
w w w . r b o . o r g . b r
Original
Article
A
retrospective
study
of
titanium
elastic
stable
intramedullary
nailing
in
displaced
mid-shaft
clavicle
fractures
夽
Rajesh
Govindasamy
∗,
Saravanan
Kasirajan,
Jimmy
Joseph
Meleppuram,
Fawas
Thonikadavath
VinayakaMissionsMedicalCollegeandHospital,DepartmentofOrthopaedics,Pondy,India
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received13June2016 Accepted21July2016
Availableonline30December2016
Keywords:
Clavicle Fracturefixation Intramedullary Bonenails Titanium
a
b
s
t
r
a
c
t
Objective:Theaimofthisstudyistoanalyzethefunctionaloutcomefollowingtitanium elasticstableintra-medullarynailing (ESIN)fordisplaced mid-shaft clavicularfractures (DMCF).
Methods:Aretrospectivestudyof60patientsbetweenMarch2009andMarch2015was con-ducted.Patientswereselectedbasedontheinclusioncriteria.Sixpatientswerelostduring followup.Outoftheremaining54patients,therewere39malesand15females.Themean agewas30.6years.ThefunctionaloutcomewasanalyzedusingtheConstantscore,rateof boneunion,complication,andearliesttimeofreturntowork.
Results:Allfracturesunitedwell,withanaveragetimeof7.5weeks.Follow-upperiodranged between12monthsand18months(average,14months).24outof54patientshadclosed nailing,while30hadminimalopenreduction.TheaveragesizeofESINwas2mm(range, 1.5–3mm).TheaverageConstantscorewas97.8(range,95–99).Therewerenomajor com-plications,butminorcomplicationsoccurred,viz.skinirritationin15patients,temporary paresthesiainfivepatients,andthreepatientswhodevelopedsuperficialinfections.One casehadimplantmigrationandperforationatthelateralcortex,andonecasehaddelayed union.Therewerefewimplant-relatedproblems,astheauthorsusedastandardprotocol toremoveitafterradiologicalunion.Allpatientsreturnedtoworkwithin10weeksofthe post-operativeperiod.
Conclusion:ESINisasafe,minimallyinvasive,engendersrapidhealingwithgoodcosmesis, andprovidesanexcellentfunctionaloutcomeintermsofpatientsatisfaction,withfewer complications.
©2016SociedadeBrasileiradeOrtopediaeTraumatologia.PublishedbyElsevierEditora Ltda.ThisisanopenaccessarticleundertheCCBY-NC-NDlicense(http:// creativecommons.org/licenses/by-nc-nd/4.0/).
夽
WorkperformedintheVinayakaMissionsMedicalCollegeandHospital,DepartmentofOrthopaedics,Pondy,India.
∗ Correspondingauthor.
E-mail:drgrortho@yahoo.com(R.Govindasamy). http://dx.doi.org/10.1016/j.rboe.2016.07.005
Estudo
retrospectivo
de
haste
intramedular
estável
elástica
de
titânio
em
fraturas
deslocadas
do
terc¸o
médio
da
clavícula
Palavras-chave:
Clavícula Fixac¸ãodefratura Intramedular Hastesósseas Titânio
r
e
s
u
m
o
Objetivo: Oobjetivodeste estudo éanalisar odesfechofuncionalapósousode haste intramedularestávelelásticadetitânio(HIEET)emfraturasdeslocadasdoterc¸omédioda clavícula(FDMC).
Métodos: Realizou-seumestudoretrospectivode60pacientesentremarc¸ode2009emarc¸o de2015.Ospacientesforamselecionadoscombasenoscritériosdeinclusão.Houveperdade seguimentodeseispacientes.Dos54pacientesrestantes,39eramhomense15mulheres.A médiadeidadefoide30,6anos.OdesfechofuncionalfoianalisadopelaescaladeConstant, taxadeuniãoóssea,taxadecomplicac¸ãoetempoderetornoaotrabalho.
Resultados: Todasasfraturasapresentaramboaunião,emumamédiade7,5semanas.O períododeacompanhamentovariouentre12e18meses(média:14meses).Em24dos54 pacientesusou-sereduc¸ãofechadacomhastesintramedulares;nosoutros30,foiutilizada areduc¸ãoabertacomfixac¸ãomínima.OtamanhomédiodaHIEETfoide2mm(variac¸ão: 1,5-3mm).AmédiadaescaladeConstantfoi97,8(variac¸ão:95-99).Nenhumpaciente apre-sentoucomplicac¸õesdegrandeporte,masalgumascomplicac¸õesdepequenoporteforam observadas,asaber:irritac¸ãoda peleem15 pacientes,parestesiatemporáriaem cinco pacienteseinfecc¸õessuperficiaisemtrêspacientes.Observou-seumcasodemigrac¸ãodo implanteeperfurac¸ãonocórtexlateral;umcasoteveuniãoatrasada.Ataxadeproblemas relacionadosaoimplantefoibaixa,umavezqueosautoresusaramumprotocolopadrão pararemovê-loapósauniãoradiológica.Todosospacientesretornaramaotrabalhoematé dezsemanasapósacirurgia.
Conclusão: AHIEETéummétodoseguro, minimamenteinvasivo,quegeracicatrizac¸ão rápidacomboacosmesiseproporcionaumexcelenteresultadofuncionalemtermosde satisfac¸ãodopaciente,commenoscomplicac¸ões.
©2016SociedadeBrasileiradeOrtopediaeTraumatologia.PublicadoporElsevier EditoraLtda.Este ´eumartigoOpenAccesssobumalicenc¸aCCBY-NC-ND(http:// creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
Theshoulderjointfunctionsasaclosedchainmechanismand constitutesfourjoints.Twoamongthefourjointsarticulates withtheclavicle.Thereforeanyclaviclefractureaffectsthe wholeshouldergirdle.Theclavicleisthefirstbonetoossify anditisoneofthecommonestbonestobefractured(2.6–5% ofallfractures).1Approximately80%offracturesoccurinthe
mid-shaft,asitisatransitionzonebetweentheflattened lat-eralpartandtubulo-triangularmedialpartaswellasitisalso thethinnestsegmentwhichisrelativelyunprotectedasitis notstabilizedbyanyligaments.2
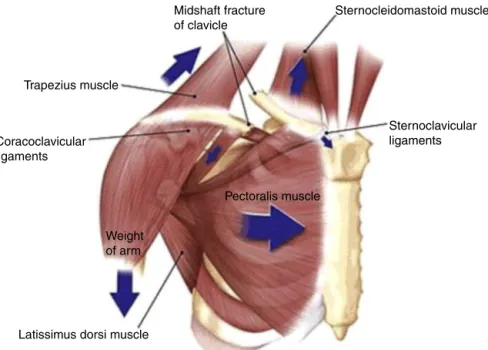
Afallordirectblowtotheshoulderisthemostcommon mechanismofinjuryforanyclaviclefracture.Themid-shaft fractures,tendtoshortenwhendisplaced.Itisduetothe com-binedworkingofthesternocleidomastoidpullingthemedial fragmentsuperiorlyandposteriorly,andthepectoralismajor, thedeltoidandgravitypullingthelateralfragmentinferiorly andanteriorly.Thisresultsinnetdisplacementand shorten-ingofthefracture(Fig.1).Morethan50%ofclaviclefractures aredisplaced.2Theoverallfrequencyofnon-unionin
undis-placedfractures is about 5% and it is higher in displaced fracturesapproximately15.1%.3
Asnaturehasendowedclaviclewithexcellentreparative powers,thesefracturesaretreatedconservativelyingeneral,
buttwo-thirdofDMCFwillendupinsomedegreeofmalunion withshorteningandsymptoms.4
Theclaviclelength playsanimportantrole tomaintain anatomicalrelationshipandfunctionoftheshouldergirdle.4
SoearlysurgicaltreatmentinDMCFimprovesthefunctional outcome by decreasing the rates of nonunion and symp-tomaticmalunion.Sosurgeryhasbeenindicatedforfractures whicharecompletelydisplaced,whichhasskinperforation, havingshorteningofmorethan20mm,neurovascularinjury, bilateralfracturesandfloatingshoulder.5
ThestandardtreatmentofDMCFisplateosteosynthesisas itrestoreslengthandanatomicalalignment,alsotheimplant is mechanically stronger but has its own complications.5
Intramedullaryfixationhasemergedasanexcellent alterna-tivesinceitbehavesasaninternalsplintbysharingloadand maintainsalignmentwithoutrigidfixation.5
Intramedullary fixationfor clavicularfractures was first describedbyPeroni6in1950.Thedevicesinclude,Kirschner
wire,Rushpins,Knowlespin,Steinmanpin,Haigepin, Rock-woodpinsandTitaniumelasticnails.5,7–9TitaniumESINcan
block itself in the boneand provide athree point fixation withintheSshapedclavicle.Somestudieshaveshown,there isaspectrumofcomplicationsandtechnicaldifficulties asso-ciatedwiththisprocedure.10
Sternocleidomastoid muscle
Sternoclavicular ligaments Midshaft fracture
of clavicle
Trapezius muscle
Coracoclavicular ligaments
Weight of arm
Pectoralis muscle
Latissimus dorsi muscle
Fig.1–Displacedmidshaftclaviclefracture.
ConstantScore,11(3)earliesttimeforreturntowork,(4)
com-plications.
Materials
and
methods
A retrospective review of a cohort of 60 unilateral DMCF treated at our institution between March 2009 and March 2015,treatedwithtitaniumESINwascarriedout.Sixpatients werelostduringfollowup.Outoftheremaining54patients therewere39males(72%)and15females(28%)inourstudy. Therewere28leftsidedfracturesand26rightsidedfractures. Themeanagewas30.6years(range:23–50years).Commonest modeofinjurywasduetofallontheshouldereitherdueto roadtrafficaccidents(n=35)orfallfromheight(n=19). Our studyincludedallDMCFclassifiedaccordingtoOrthopaedic TraumaAssociation(OTA)Classification.12Wehad26patients
withtypeAfracturesand28patientswithtypeBfractures.
Inclusioncriteria
Skeletally maturepatients with diaphyseal mid-shaft frac-tureswithmorethan20mmofdisplacementofeithertypeA (simplefracturetwosegment)ortypeB(fracturewithbending wedge)ofOTAclassificationswithinsevendaysofinjury.
Exclusioncriteria
(1)Openfractures,(2)floatingshoulder,(3)proximalordistal fractures,(4)neurovascularinjuries,(5)fracturespresenting afteroneweekofinjury,(6) patientswithpre-existing sub-acromialpathology,(7)co-morbiditieswithriskofanaesthesia andsurgery,(8)surgicaltechniquesotherthanESIN,(9)grossly comminutedfractures–typeC(OTA),(10)non-union,and(11) malunion.
Surgicaltechnique
Having got the informed written consentand prophylactic antibiotics,the patientundergeneralanaesthesiawas pos-itionedinasupinebeachchairpositionwithafoldedtowel overthemedialborderoftheaffectedshoulder.Theinjured partwaspreparedanddrapedfromthemidlinetotheupper arm. Care was taken to ensure the sterno-clavicular joint accessibilityfortheentryandwasconfirmedusinganimage intensifier.Thesizeofthenailwasmeasuredusingthe fol-lowingformula−0.4Xcanaldiameterinmm.9
Asmall incisionwas madeoverthe skin1cm lateralto medialendoftheclavicle.Thesubcutaneousfatwasincised alongwithplatysma.Thepectoralfasciawasdividedinline with the skin incision followed bycareful elevationof the underlyingmusculaturefromtheclavicle.Thenforinsertion ofthenailanentrypointwasmadebyAwlintheanterior cor-texoftheboneand3.2mmdrillwasusedforfurtherentry. Titaniumnailwasbenttoabout15degreetofacilitate inser-tion,theT-handlewasusedtopushandrotatethenailintothe medullarycavityunderfluoroscopiccontroluntilitreached thefracturesite(Fig.2A–D).
Entry point of nail
After insertion
Positioning
Skin incision
Fig.2–Surgicaltechnique.(A)Positioning;(B)skinincision;(C)entrypointofnail;(D)afterinsertion.
afterlittlebentclosedtotheentrypointonthemedialside andburiedunderskintominimizesofttissueirritationaswell asforaneasyextractioninfuture.Thefasciaandskinwere closedinlayers.
Postoperativeprotocol
Postoperativelypatientswerekeptinasling,andtheywere dischargedtheverynextdayafterpostoperativecheckX-rays andencouragedforearlyshouldermobilizationwithpendular exercises.Sutureremovalwasdoneonthetenthday.Active range ofmovement exercises were initiated. The shoulder slingwasdiscardedattheendofthreeweeks,overhead activ-itywasallowedonlyafterfourthweek.Activitiesofdailyliving werestarted thereafter,butthose requiringliftingofheavy weightsweredelayeduntilunionwasachieved.
All patients were reviewed at second, fourth and sixth week, third and sixth month after surgery at the outpa-tientdepartment, ateach visit the patients were accessed clinico-radiologically forprimary and secondary outcomes. Weroutinelyremovedthenailsaftersixmonthswith com-pleteradiologicalunion,whichwasdefinedasvisiblebridging callusorcompleteobliterationoffracturelines.Allpatients werefurtherfollowedupforoneyeartoamaximumfollow upoftwoyears.
As therewere no clavicle trauma scores the functional outcome wasevaluated usingConstant Score.11 Welooked
for any complications in our study. Major complications were:thoserequiringadditionalsurgerytoreviseorremove
thefixationasaresultofnonunion,malunion,deepseated infectionsandbreakageofimplant.Minorcomplicationswere those donotrequireadditionalsurgery, suchassuperficial infections,implantirritation,migration,scarneuromasand neurovascularproblems.13,14
Results
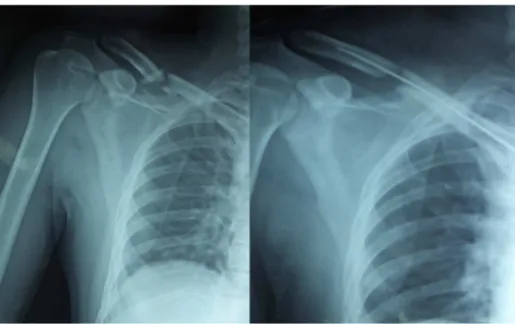
Attheendofthestudywehad54patients,whoreturnedfor clinicalandradiologicalfollowup.Averageclinicalfollowup was14months(range12–18months).Allfracturesunitedwith ameantimeof7.5weeks(7–10weeks).Wehadonecaseof delayedunion(Figs.3–6)andthefractureunitedattheendof 10weekswithimmobilization,withoutneedofanyadditional proceduressuchasbonegrafting.
Out of 54 patients, the average ESIN size was 2mm (1.5–3mm).Inmostcases,weused2mmnails,onlyinfive cases with minimal comminution we used 3mm nails to increasestability.WedidMiniopentechniquein30patients (55%),intherest24patients(45%)weperformedclosed tech-nique.
Fig.3–OTAtypeBfracturefixedwithESINthroughMiniopentechnique.ESIN,elasticstableintramedullarynailing.
Fig.4–FracturewentfordelayedunionwithESINinsitu.ESIN,elasticstableintramedullarynailing.
patients(9.2%)hadtemporaryparaesthesiawhichgotsettled intwoweeks.Inourstudy,wedidnothavemuchimplant relatedproblemsaswehadastandardprotocoltoremoveit afterradiologicalunionatsixmonths.
Wecomparedthefinalclavicularlengthsafterfull radio-logicalunionandimplantremoval.InOTAtypeBfractures,in sixcases(21%)wehadclavicularshorteningof1cm.Infour cases(14%)wehad0.5cmshortening.Wedidnothavemuch significantshorteninginOT6AtypeAfractures.
All patients returned to work within 10 weeks of post operative period. The functional outcome was evaluated by using Constant score at each follow up. All patients with one year follow up were included in the study, the average Constant score was 97.8(Max-99, Min-95). Statis-tical data of constant score in our study had standard deviation 2.4, sample variance=5.7, standard error=0.25, skewness=−0.57andthestudywasconsideredassignificant
(p≤0.05).
Discussion
Traditionally,fromHippocraticera,midshaftclaviclefractures were treated conservatively.15 Numerous closed treatment
optionshavebeendescribedtoimmobilizeandalignthe frac-ture.Almostallauthorsthoughtmaintainingthealignment afterclosedreductionofDMCFisawishfullthinking.16The
closed treatmentmethods include,simplesling orafigure of eightbandage.It hasa very high rateof nonunion and malunion.3 Twothirdofthe conservativelymanaged DMCF
willendupinsomedegreeofmalunion.Shorteningofabout 1.4–2cmhasbeenreportedtobecriticaldeficitfor develop-mentofasymptomaticmalunion.Thisresultsinpain,lossof strength,rapidfatiguability,paraesthesiaofthearmandhand, problemswithsleepingonthebackandcosmeticcomplaints.4
Fig.5–Fractureunitedeventuallyandunderwentimplant removal.
Fig.6–Patienthadagoodfunctionaloutcomewitha constantscoreof97.
Themostcommonsymptom isresidual painduring activ-ityor evenatrest andlossofstrength.Thesymptomsare mainly due to shortened lever arm of the shoulder girdle whichchangestheorientationoftheglenoidwithwingingof scapula.Changeinorientationofglenoidincreasesthe shear-ingforceacrosstheshoulderjoint,resultinginprotractionas wellastiltofscapulacanresultinpainduringlyingonthe back.19,20
Theshortenedclaviclehasanegativeeffectonmuscle ten-dontensionresultinginlossofstrengthandendurability.20,21
Italsochangestherestingangleofthesternoclavicularjoint
Fig.7–LateralmigrationofESIN.ESIN,elasticstable intramedullarynailing.
resulting in change of load in both acromioclavicular and sternoclavicularjointwithincreaseincidenceof acromioclav-iculararthritis.17,20Largecallusformationaftermalunioncan
leadtoneurovascularproblemsasaresultofthoracicoutlet syndrome.22
Anatomically aligned united mid shaft clavicle fracture is alwayssuperior overconservatively treatedclavicle.The onlywaytoachievethisisanopenreductionwithinternal fixationorapercutaneousprocedure.Hence,current recom-mendationforthisfracturesisoperativefixation.4,17,21,23Plate
osteosynthesis,23,24 external fixation25 and intramedullary
fixation9,26–28 haveallbeendescribedforsurgicaltreatment
ofclaviclefractures,everymodalityofsurgicalintervention hasitsownprosandcons.
Plating is the gold standard operative procedure for DMCF,asitrestoreslengthandalignmentanatomicallyand mechanicallyevenincomminutedfracturesbybecomingthe strongestimplant.23,24 Studieshaveshowncomminutionin
claviclefracturesisanegativeprognosticindicator.29Plating
isthemostdiscussedanditslongtermexperienceinliterature ismentioned.Itisalessdemandingprocedurethatprovides rigidfixationandcompressionforearlyrehabilitation. How-everthistechniquemayrequirelargerincisionandextensive exposurewhichcouldcausecomplicationssuchasinfections, implantfailure,refractureafterimplantremoval, neurovascu-larinjury,nonunion,dysesthesiaandkeloidscar.30,31Arecent
report ofaprospectiverandomizedtrial described an inci-dencewithadverseeventsof37%,howevertheproportionof complicationsinnon-operativegroupwas63%.23
The neurovascular damage with screw placement in plating can be reduced by placing it anteroinferiorly, but anterosuperior plating offersa moresecure fixation.32 The
implantrelatedproblemsinplatinghasnowbeenaddressed with specificallydesigned plates with angularstability.24,33
andimprovementofplatefixation,itisnotfreeof complica-tions.Externalfixationisrarelyusedinclavicularfixation.Its absoluteindicationisonlyinopenclaviclefractures.25
So, another emerging mode of fixation ispercutaneous intramedullaryfixationwithESIN.9,34,35 Itisalsominimally
invasive,conservesfracturehaematomaandperiosteumthat encouragescopiouscallousformationandimprovecosmesis. Studieshaveshowntheaveragetimeofunionissignificantly fasterasitprovidesrelativestability.Itcanbedoneby antero-gradeorretrogradetechnique.Intramedullary fixationwith nailsorpinshasminimallyinvasivecharacteristics,including smallerskinincisions,reducedsofttissuestripping,lessblood loss, shorter operative time, shorter hospital stay, shorter timeforunionandfewmajorcomplications.36Intramedullary
fixation istechnically more demandingand operative out-comemay beinfluenced bylearning curve ofthe involved surgeon.36,37Italsodependsuponthedegreehowmuchthe
implanthastobeflexibleandsmallenoughtobeabletopass throughthenarrowmedullarycanalandofferarigid stabil-ityneededfortheclavicle.Inapproximately50%ofcases,an extraincision isneededtofacilitatefracturereductionand guidethepinthroughthefracturesite.13Thismaynegatively
affecttheoutcomeduetoanincreaseinincisionlengthand fracturehealingduetodisruptionofperiosteumandfracture haematoma.
ThemaincomplicationsofESINaremigrationand perfo-rationofdevice. Althoughtheyareminor complicationsin literature,theyarereportedtobeinrangeof5.2–38.8%.34,36,38
Itisprimarilyduetoinadequatelycutmedialendofthenail duringsurgeryandsecondarilyduetoclavicularshortening. Thesecomplicationscanbereducedbyadequatelycuttingthe nail,useofmedialendcaps,goodanatomicalreductionand intra-operativecompressionandbyavoidingshoulder abduc-tionbeyond90degreesinfirsttwoweekspostoperatively.
Inourstudy,wehadanexcellentunionratesinallcases. Inonecasewehad delayedunion,inOTAtypeBfracture, wherewedid amini open technique. Wedid open reduc-tionin55%ofcaseswhichwascomparabletootherstudies.13
Incidenceofopenreductiondependsonthelearningcurveof thesurgeon.36,37Inourstudy,thetechniquewasdonebytwo
well-trainedsurgeons.Themaincomplicationsinourstudy wasmedialskinirritation(27%),soweroutinelyremovedthe nailafterfractureunion.Inonecase,patienthadafalland hadanimplantmigrationatthemedialendandperforation atthelateralendandthenailwasremovedthrougha sepa-rateincisionatthelateralendafterfractureunion.Allother minorcomplicationssuchassuperficialinfections,temporary paraesthesiagotsettledand ourfinal clavicularshortening was1cminOTAtypeBfractures,sotherewasnosymptomatic malunion.Inourseries,theresultofshoulderfunctionwas assessedbyconstantscoresandwasbetterincomparisonto conservativelymanagedDMCFandinparwithotherstudies withESIN.26,27
Ourstudyalsohaslimitations,itisarelativelysmall retro-spectiveseriesofpatientswithameanfollowupoffourteen months,wedid notcompare study withother methodsof fixation,ourcomplicationswereless aswedidroutinenail removal,we cannotcomment regardingsymptomatic mal-unionaswedidnothavelong-termfollowupandweexcluded OTAtypeCfractures,whereESINproducesmoreshortening,
soplatefixationremainstheoperativeprocedureofchoiceas itoffersbetterclavicularlengthmaintenance.5
Conclusion
ESINisasafe,minimallyinvasivetechniqueinindicatedcases. Wehadfavourableresultswiththistechniquebutneedsalot ofexpertise.Wedonotrecommendthistechniqueinseverely comminutedDMCF.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1.PostacchiniF,GuminaS,SantisP,AlboF.Epidemiologyof claviclefractures.JShoulderElbowSurg.2002;11(5):452–6. 2.NordqvistA,PetersonC.Theincidenceoffracturesofthe
clavicle.ClinOrthopRelatRes.1994;(300):127–32.
3.RobinsonCM,Court-BrownCm,McQueenMM,WakefieldAE. Estimatingtheriskofnonunionfollowingnonoperative treatmentofaclavicularfractures.JBoneJointSurgAm. 2004;86(7):1359–65.
4.LazaridesS,ZafiropoulosG.Conservativetreatmentof fracturesatthemiddlethirdoftheclavicle.Therelevanceof shorteningandclinicaloutcome.JShoulderElbowSurg. 2006;15(2):191–4.
5.SmekalV,OberladstaetterJ,StruveP,KrappingerD.Shaft fracturesoftheclavicle:currentconcepts.ArchOrthop TraumaSurg.2009;129(6):807–15.
6.PeroniL.Medullaryosteosynthesisinthetreatmentof claviclefractures.ArchOrtop.1950;63(4):398–405. 7.LeeYS,LinCC,HuangCR,ChenCN,LiaoWY.Operative
treatmentofmidclavicularfracturesin62elderlypatients: knowlespinversusplate.Orthopedics.2007;30(11):959–64. 8.MuddCD,QuigleyKJ,GrossLB.Excessivecomplicationsof openintramedullarynailingofmidshaftclaviclefractures withtheRockwoodClaviclePin.ClinOrthopRelatRes. 2011;469(12):3364–70.
9.MuellerM,RanggerC,StriepensN,BurgerC.Minimally invasiveintramedullarynailingofmidshaftclavicular fracturesusingtitaniumelasticnails.JTrauma. 2008;64(6):1528–34.
10.MillettPJ,HurstJM,HoranMP,HawkinsRJ.Complicationsof claviclefracturestreatedwithintramedullaryfixation.J ShoulderElbowSurg.2011;20(1):86–91.
11.SmithMV,CalfeeRP,BaumgartenKM,BrophyRH,WrightRW. Upperextremity-specificmeasuresofdisabilityand
outcomesinorthopaedicsurgery.JBoneJointSurgAm. 2012;94(3):277–85.
12.O’NeillBJ,HirparaKM,O’BriainD,McGarrC,KaarTK.Clavicle fractures:acomparisonoffiveclassificationsystemsand theirrelationshiptotreatmentoutcomes.IntOrthop. 2011;35(6):909–14.
13.FerranNA,HodgsonP,VannetN,WilliamsR,EvansRO. Lockedintramedullaryfixationvsplatingfordisplacedand shortenedmid-shaftclaviclefractures:arandomizedclinical trial.JShoulderElbowSurg.2010;19(6):783–9.
15.NeerCS.Fracturesoftheclavicle.In:RockwoodCA,GreenDP, editors.Fracturesinadults.Philadelphia:JBLippincott;1984. p.707–13.
16.RoweCR.Anatlasofanatomyandtreatmentofmidclavicular fractures.ClinOrthopRelatRes.1968;58:29–42.
17.HillJM,McGuireMH,CrosbyLA.Closedtreatmentof displacedmiddle-thirdfracturesoftheclaviclegivespoor results.JBoneJointSurgBr.1997;79(4):537–9.
18.NowakJ,HolgerssonM,LarssonS.Sequelaefromclavicular fracturesarecommon:aprospectivestudyof222patients. ActaOrthop.2005;76(4):496–502.
19.AndermahrJ,JubelA,ElsnerA,ProkopA,TsikarasP,JupiterJ, etal.Malunionoftheclaviclecausessignificantglenoid malposition:aquantitativeanatomicinvestigation.Surg RadiolAnat.2006;28(5):447–56.
20.LedgerM,LeeksN,AcklandT,WangA.Shortmalunionsof theclavicle:ananatomicandfunctionalstudy.JShoulder ElbowSurg.2005;14(4):349–54.
21.McKeeMD,WildLM,SchemitschEH.Midshaftmalunionsof theclavicle.JBoneJointSurgAm.2003;85(5):790–7.
22.OnstenkR,MalessyMJ,NelissenRG.Brachialplexusinjury duetounhealedorwronglyhealedclavicularfracture.Ned TijdschrGeneeskd.2001;145(50):2440–3.
23.CanadianOrthopaedicTraumaS.Nonoperativetreatment comparedwithplatefixationofdisplacedmidshaftclavicular fractures.Amulticenter,randomizedclinicaltrial.JBone JointSurgAm.2007;89(1):1–10.
24.MullajiAB,JupiterJB.Low-contactdynamiccompression platingoftheclavicle.Injury.1994;25(1):41–5.
25.SchuindF,Pay-PayE,AndrianneY,DonkerwolckeM,Rasquin C,BurnyF.Externalfixationoftheclavicleforfractureor non-unioninadults.JBoneJointSurgAm.1988;70(5): 692–5.
26.KhalilA.Intramedullaryscrewfixationformidshaftfractures oftheclavicle.IntOrthop.2009;33(5):1421–4.
27.KlewenoCP,JawaA,WellsJH,O’BrienTG,HigginsLD,Harris MB,etal.Midshaftclavicularfractures:comparisonof intramedullarypinandplatefixation.JShoulderElbowSurg. 2011;20(7):1114–7.
28.LiuHH,ChangCH,ChiaWT,ChenCH,TarngYW,WongCY. Comparisonofplatesversusintramedullarynailsforfixation ofdisplacedmidshaftclavicularfractures.JTrauma. 2010;69(6):E82–7.
29.NowakJ,HolgerssonM,LarssonS.Canwepredictlong-term sequelaeafterfracturesoftheclaviclebasedoninitial findings?Aprospectivestudywithninetotenyearsof follow-up.JShoulderElbowSurg.2004;13(5):479–86. 30.BöstmanO,ManninenM,PihlajamäkiH.Complicationsof
platefixationinfreshdisplacedmidclavicularfractures.J Trauma.1997;43(5):778–83.
31.PoigenfürstJ,RappoldG,FischerW.Platingoffreshclavicular fractures:resultsof122operations.Injury.1992;23(4):237–41. 32.KloenP,WernerCM,StufkensSA,HelfetDL.Anteroinferior
platingofmidshaftclaviclenonunionsandfractures.Oper OrthopTraumatol.2009;21(2):170–9.
33.KabakS,HaliciM,TuncelM,AvsarogullariL,KaraogluS. Treatmentofmidclavicularnonunion:comparisonof dynamiccompressionplatingandlow-contactdynamic compressionplatingtechniques.JShoulderElbowSurg. 2004;13(4):396–403.
34.SmekalV,IrenbergerA,StruveP,WambacherM,KralingerFS. Elasticstableintramedullarynailingversusnonoperative treatmentofdisplacedmidshaftclavicularfractures–a randomized,controlled,clinicaltrial.JOrthopTrauma. 2009;23(2):106–12.
35.JubelA,AndemahrJ,BergmannH,ProkopA,RehmKE.Elastic stableintramedullarynailingofmidclavicularfracturesin athletes.BrJSportsMed.2003;37(6):480–3.
36.FriggA,RillmannP,PerrenT,GerberM,RyfC.Intramedullary nailingofclavicularmidshaftfractureswiththetitanium elasticnail:problemsandcomplications.AmJSportsMed. 2009;37(2):352–9.
37.WitzelK.Intramedullaryosteosynthesisinfracturesofthe mid-thirdoftheclavicleinsportstraumatology.ZOrthop Unfall.2007;145(5):639–42.