w w w . r b o . o r g . b r
Original
Article
Preliminary
results
from
osteosynthesis
using
Ender
nails
by
means
of
a
percutaneous
technique,
in
humeral
diaphysis
fractures
in
adults
夽
Glaydson
Gomes
Godinho
a,b,c,∗,
Flávio
de
Oliveira
Franc¸a
a,c,
José
Márcio
Alves
Freitas
a,b,
Flávio
Márcio
Lago
Santos
c,
Guilherme
de
Almeida
Sellos
Correa
a,b,c,
Lucas
Russo
Maia
a,b,caHospitalOrtopédico(HO),BeloHorizonte,MG,Brazil
bHospitalBeloHorizonte(HBH),BeloHorizonte,MG,Brazil
cHospitalLifecenter(HLC),BeloHorizonte,MG,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received6March2014
Accepted15August2014
Availableonline6July2015
Keywords:
Humeralfractures
Intramedullaryfixationoffractures
Internalfixationoffractures
a
b
s
t
r
a
c
t
Objective:Todemonstratetheclinicalandfunctionalresultsfromtreatment ofhumeral
diaphysisfracturesusingEndernails.
Methods:Eighteenpatientswhounderwentosteosynthesisofhumeraldiaphysisfractures
usingEndernailswereevaluated.Inadditiontotheclinicalandradiographicevaluations,
patientswithaminimumofoneyearoffollow-upwereassessedbymeansoftheConstant,
AmericanShoulderandElbowSurgeons(ASES),MayoClinicandSimpleShoulderValue
(SSV)functionalscores,andinrelationtothedegreeofsatisfactionwiththefinalresult.
Thefixationtechniqueusedwasbymeansofananterogradepercutaneousroute.
Results:Allthepatientsachievedfractureconsolidation,afterameanof2.9months(ranging
from2to4months).ThemeanConstantscorewas85.7(rangingfrom54to100)andthe
meanASESscorewas95.9(rangingfrom76to100).Allthepatientsachievedthemaximum
scoreontheMayoClinicscale.
Conclusion: FixationofhumeraldiaphysisfracturesusingEndernailsbymeansofa
percu-taneoustechniquewasshowntobeamethodwithpromisingpreliminaryresults.
©2014SociedadeBrasileiradeOrtopediaeTraumatologia.PublishedbyElsevierEditora
Ltda.Allrightsreserved.
夽
WorkperformedattheBeloHorizonte,LifecenterandBelvedereHospitals,BeloHorizonte,MG,Brazil.
∗ Correspondingauthor.
E-mail:ggodinho@terra.com.br(G.G.Godinho).
http://dx.doi.org/10.1016/j.rboe.2015.06.006
Resultados
preliminares
da
osteossíntese
com
haste
de
Ender,
por
meio
da
técnica
percutânea
nas
fraturas
diafisárias
do
úmero
nos
adultos
Palavras-chave:
Fraturasdoúmero
Fixac¸ãointramedulardefraturas
Fixac¸ãointernadefraturas
r
e
s
u
m
o
Objetivo:Demonstrarosresultadosclínicosefuncionaisdotratamentodafraturadiafisária
deúmerocomusodashastesdeEnder.
Métodos: Foramavaliados18pacientessubmetidosàosteossíntesedafraturadiafisáriade
úmerocomusodahastedeEnder.Alémdasavaliac¸õesclínicaseradiográficas,ospacientes
comnomínimoumanodeseguimentoforamavaliadospelosescoresfuncionaisde
Con-stant,AmericanShoulderandElbowSurgeons(Ases),MayoClinic,SimpleShoulderValue
(SSV)equantoaograudesatisfac¸ãocomoresultadofinal.Atécnicadefixac¸ãousadafoi
porviaanterógradaepercutânea.
Resultados: Todosospacientesobtiveramconsolidac¸ãodafratura,commédiade2,9meses
(variac¸ãodedoisaquatro).AmédiadoScoredeConstantfoide85,7(variac¸ãode54-100)
eadoASESde95,9(variac¸ãode76-100)etodosobtiverampontuac¸ãomáximapeloescore
MayoClinic.
Conclusão: Afixac¸ãodasfraturasdiafisáriasdoúmerocomousodahastedeEnderpela
técnicapercutâneademonstrouserummétodocomresultadospreliminarespromissores.
©2014SociedadeBrasileiradeOrtopediaeTraumatologia.PublicadoporElsevier
EditoraLtda.Todososdireitosreservados.
Introduction
TheEndernail,which isthin,flexibleand premolded,was
first described by Ender for treating intertrochanteric hip
fractures.1Thefirststudytoevaluatetheresultsfromusing
Endernails fortreating closed humeraldiaphysisfractures
waspublishedin1987.Inthatstudy,osteosynthesiswas
per-formedusinganEndernailafterclosedreductionoffractures
withangulardisplacementsgreaterthan20degrees.2
Themajorityofhumeraldiaphysisfracturescanbetreated
conservativelywith good clinical and functional results.3–5
Surgicaltreatment isreserved for exposed segmental
frac-tures,multipletraumapatients,casesoffloatingshoulderor
elbowandfailureofconservativetreatment.6–8
Currently,thetwotypesofimplantforwhichthereisthe
greatestamountofevidenceregardingsurgicaltreatmentof
humeraldiaphysisfracturesaredynamiccompressionplates
andrigidintramedullarynails.
Anatomicalreductionofthefragments,whichisthe
objec-tive when plates are used, tends to reduce the risks of
poorconsolidation.However,thisrequiresgreater
perioper-ativeexposure,withgreaterdamagetothesofttissuesand
periostealvascularization,whichpossiblycanbecorrelated
witha higher infection rate and pseudarthrosis.6–8 On the
otherhand,rigidintramedullarynails giverise toless
soft-tissueaggression.However,theirusehasbeencorrelatedwith
postoperative shoulder pain and high numbers of second
interventions.7,9–11
Fixationusingflexibleintramedullarynailshasbeen
criti-cizedbecauseofthedeficitofrotationalcontrolandinstability
duringthefixation,7,10alongwiththepossibilitythatthe
rota-torcuffmightbeaffectedincasesofanterogradeentry.2,12
Withmodification tothetechniqueoriginallydescribed for
introducingthenail,goodresultsareexpected.
Theobjectiveofthepresentstudywastodemonstratethe
clinicalandfunctionalresultsfromtreatinghumeral
diaph-ysis fractures usingEnder nails and compare the financial
costsofthisimplantinrelationtothosefromothersurgical
techniques.
Materials
and
methods
Twenty-sixpatientswithclosedhumeraldiaphysisfractures
thathadbeentreatedsurgicallyusingEndernailsasthe
fixa-tion methodwere selected.Theoperations wereperformed
in our institution between July 1998 and August 2011. All
ofthepatientswereretrospectivelyevaluatedregardingthe
neurologicalfunctioningofaffectedlimbbeforethesurgical
procedure,andpossibleassociatedlesionswereinvestigated.
Inaddition,bymeansoforthogonalpreoperativeradiographs
ofthehumerus,inanteroposterior(AP)andlateralviews,the
fractureswereclassifiedinaccordancewiththeAOsystem.
Theinclusioncriteriawerethatthecasesshouldcomprise
closedfracturesthatoccurrednotmorethan7daysbeforethe
surgicalprocedure,inwhichthefracture displacementwas
morethan20 degreesinthesagittalor coronalplane,with
shorteningbetweenthesegmentsgreaterthan2cm,classified
as12A,12B,12C1or12C2fractures.
Cases were excluded if aminimum ofoneyear of
out-patientfollow-uphadnotbeenconcluded,includingreviews
conducted1week,15daysand1,2,3and6monthsafterthe
operation.Fracturesofthetype12C3werealsoexcluded,as
werepathologicalandexposedfractures.Noneofthepatients
presented a fracture oftype 12B3. Among the 26 patients
selected,eightwerelostfromthefollow-up:oneduetodeath
andsevenbecauseitwasimpossibletocontactthem.Eighteen
patients(12womenand8men)remained,andwereall
meandurationofthepostoperativefollow-upwas3.2years
(range:1–13).
ThemostcommontypeoffracturewasA(66%),followed
byB(27%),andonlyonecasepresentedasegmentalfracture
(typeC2).
Duringthe follow-up,the patientswere evaluatedusing
theConstant,AmericanShoulderandElbowSurgeons(ASES),
Mayo Clinic and Simple Shoulder Value (SSV) functional
scales, including a comparison with the contralateral side
regardingrangeofmotion(ROM)oftheshoulderandelbow.
Neurologicaltestswerealsousedandpossiblecomplications
inherenttothesurgicalprocedure, suchasinfection ofthe
surgicalsiteandsystemiccomplications,were investigated.
TheSSVwasusedtosubjectivelyevaluatetheshoulder,given
thatthisproceduremayindirectlyinfluencethefunctioning
ofthis joint. Subsequently, the patients were asked about
their satisfaction relating tothe treatment ofthe humeral
fractureandwhethertheyweresatisfiedordissatisfiedwith
it.
The postoperative radiographs furnished information
regarding the time taken for the fracture to consolidate
andthealignmentbetweenthesegments,alongwith
infor-mation regarding the positioning and migration of the
nails.
Satisfactoryunionofthe fragmentswasdefined
accord-ingtothefollowingcriteria:viewingofabonebridgebetween
thefragmentsorobliterationofthefracturesite,withunion
ofthecorticalboneinbothviews.Consolidationwas
consid-eredtobedelayedwhen theparameters establishedabove
were absent 4 months after implementation of
osteosyn-thesis and a situation of pseudarthrosis was defined if
consolidation remained absent 9 months after the
opera-tion.
Skewedconsolidationwastakentoberadiographic
con-solidationshowingananglegreaterthan 20degreestothe
anatomicalaxisofthediaphysis.
AllthepatientsusedaVelpeauslingduringtheimmediate
postoperative period. They performed flexion and
exten-sion exercises for the elbow and pendulum exercises for
the ipsilateral shoulder on the day following the
proce-dure.
Surgical
technique
Thesurgerywasperformedwiththepatientinthedeckchair
position,undergeneralanesthesiaorsedation,withregional
blockof the brachial plexus. All the patients were
admin-istered 2g of first-generation cephalosporin intravenously,
30minbeforetheprocedureandthiswasfollowedby1gevery
6hfor24h.
Theentry point was viewed under fluoroscopy,
approx-imately 2cm distallyto the footprint of the supraspinatus
tendon.Atthispoint,alongitudinalincisionofaround2cm
wasmade. Anentry orifice inthe bonewasmade using a
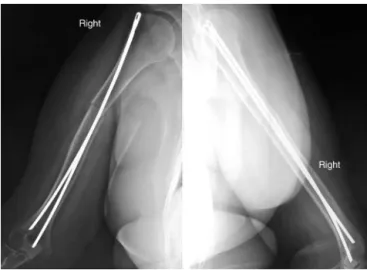
manualstarter(Fig.1).TwoorthreeEndernailswereinserted
(Fig.2)afterreductionofthefracture,performedwhileviewing
usinganimageintensifier(Fig.3),anditwassoughttodiverge
thedistalextremitiesofthenails.Itwasdecidedtoinsertthree
nailswhen instabilitywas observedatthe focusafterarm
Fig.1–Usingthemanualstartertomaketheentryorifice inthebone.
Fig.3–Reductionofthefractureandpassageofthenail, usinganimageintensifier.
rotationtestsduringtheoperation.Thesizeofthenailswas
chosenbymeansofpreoperativeradiographicexaminations
inAPandlateralviews,takingthenormalcontralateralarmas
thestandard.Attheendoftheoperation,thepositionsofthe
nailswerecheckedbymeansofradiographicexaminationsin
APandlateralviews.
Results
ThemeanConstant scorewas85.7 (range:54–100) andthe
meanASESwas95.9(range:76–100).Allthepatientsobtained
100pointsintheevaluationusingtheMayoClinicscale.The
meanscorefromthesubjectiveevaluationusingtheSSVwas
96points.
TwopatientspresentedConstantscoresof54and58,
cor-respondingtoASESscoresof76and79,respectively.
Whenthepatientswereaskedabouttheirdegreeof
satis-faction,allofthemsaidthattheyweresatisfied.
Themigrationrateamongthenailswas33.3%andallthe
migrationswereupwards.
Themeantimetakentoreachfractureconsolidationwas
2.9months(range:2–4)andnoneofthepatientsevolvedwith
delayedconsolidationorpseudarthrosis(Fig.4).
Twopatients (11%)presentedlesionsofthe radialnerve
beforetheoperation,butshowedcomplete recoveryduring
thepostoperativefollow-up(withoutanyinterventionduring
theoperation).
Noneofthepatientsevolvedwithinfection,neuropraxia,
wounddehiscenceoranyothertypeofcomplication.
Postoperativeradiographicevaluations(patientsinvitedto
return)wereperformedon16ofthe18patients.Noneofthem
presentedskewedconsolidationoranyotheralteration.
Fig.4–Radiographdemonstratingtheconsolidation process1monthaftertheoperation.
Discussion
Theimplant options mostusedtodayfortreatinghumeral
diaphysisfracturesareplatesandrigidintramedullarynails.
In ameta-analysis, Ouyang et al.9 sought toobjectively
evaluatethefunctionalandclinicalresultsandthe
compli-cationsfromthesetwotypesofimplant(plates andlocked
intramedullarynails)fortreatinghumeraldiaphysisfractures.
Inthepresentstudy,100%ofthefracturestreatedusing
Ender nails reachedconsolidation, without presenting any
delay.Inthemeta-analysisofOuyangetal.,98.3%ifthe
frac-tures treated using locked intramedullary nails evolved to
pseudarthrosisand 17% todelayedconsolidation.Likewise,
6.75%ofthefracturestreatedusingplatesevolvedto
pseu-darthrosisand5%todelayedconsolidation.
Chiuetal.6showedapseudarthrosisrateof9.4%among
fracturestreatedusingEndernailsandattributedthecause
ofthistoexcessivedislocationatthefocusofthefracture.In
allthecases,thegapbetweenthemainfragmentsduringthe
postoperativeclinicalfollow-upwasgreaterthan0.5cm,even
thoughfragmentimpactionhadbeenperformedduringthe
operationsoastoproduceagapofless than3mmatthat
time.
Amongthepatientsofoursample,allofthemwere
encour-agedtoperformactiveflexionandextensionoftheelbow.Itis
believedthatthismovementhelpstomaintaintheimpaction
ofthefragmentsthroughthestrengthofthebiceps.
Inastudy on86patients whowere treatedusingEnder
nails,HallandPankovich2 onlyobservedonecaseof
pseu-darthrosisandthe meantimetakentoreachconsolidation
was 7.2 weeks.believe that our high fracture consolidation
Table1–AveragecostsofhumeralimplantsonthemetropolitanregionofBeloHorizonte.
Endernaila DCPplateb Lockedplate Lockedplatec
Amounts(reais) 195.62 389.36 1572.00 1520.00
a Twonails(minimumnumberofnailsused).
b Dynamiccompressionplateof4.5mmandeightcorticalscrews. c Lockedplateandlockingscrews.
Fig.5–Radiographsinanteroposteriorandlateralviewof therightarmafterremovalofthenail,withthefracture consolidated.
principleofbiologicalinternalfixation,asdescribedby
Ger-beret al.,13 who emphasized maintenanceof the integrity
ofthesofttissuessurroundingthefracture,throughindirect
reductionofthefocus.Anothertechniquethathasproduced
goodresultsusingthisprinciplewasdescribedbyLivaniand
Belangero14 andconsistedofusingabridgeplate.Nocases
ofpostoperativeinfection(superficialordeep)wereobserved
duringthefollow-upamongourpatients.Webelievethatthis
lackofinfectionwasduetotheminimallyinvasiveapproach.
ThisargumentisvalidatedbythefindingsofOuyangetal.,9
whoobservedinfectionin2%ofthecasesdealt withusing
nailsand in6.3%oftheprocedures withplates.Two cases
ofneurologicallesionsduetopreoperative paralysisofthe
radialnervewereidentified,bothcausedbytrauma,with
com-pleterecoveryduringthepostoperativefollow-upwithoutany
interventionduringtheoperation.Nocasesofpostoperative
neurologicalwereobserved.ThedataofOuyangetal.9showed
that among the patients treated with rigid intramedullary
nails,theradialparalysisratewas2.5%,whileamongthose
treatedwithplates,itwas4.8%.HallandPankovich2reported
twocasesofparalysisoftheradialnerveafterfixationofthe
humeralfractureusingaretrogradeEndernailandachieved
spontaneousimprovementwithoutexplorationofthenerve
affected.
Amongthe18casestreatedwithEndernails,thenailwas
removedin6casesbecauseupwardmigrationwasobserved
afterconsolidation(Fig.5).Thisrepresentsareworkingrate
of33%,but it should benoted that inhalf ofthesecases,
thenailwasremovedasanoutpatientprocedure,usinglocal
anesthetic,afterobtainingradiographicconfirmationof
con-solidation,withoutsubsequentcomplication.Theauthorsof
thepresentstudybelievethatthismigrationisdueto
insuffi-cientimpactionofthenailsinthemedullarycanal.Burialof
thenailsisavoidedasawayoffacilitatingtheirremovalifthis
becomesnecessary.Inasampleof21patientswhounderwent
intramedullaryfixationusingrigidnails,McCormacketal.11
presentedtwocasesinwhichremovalofthenailwas
neces-sarybecauseofthesevereimpactthatthenailhad had.In
themeta-analysisstudybyOuyangetal.,9areoperationrate
of16.1%amongcasesusinglockedintramedullarynailsand
8.5%amongcaseswithplates.
WedidnotobserveanylimitationregardingpassiveROM
(i.e. this was symmetrical to the contralateral side). Two
patients presentedlimitation regarding activeanterior
ele-vation andthesepatients hadthe lowestfunctional scores
(onepatientaged67yearsandtheother,71years).Thesetwo
patientspresentedsignificantdeficitsofrotatorcuffstrength.
Sincethesepatientswereoligosymptomatic,webelievethat
theirdeficitwasduetoapreviouspathologicalconditionof
therotatorcuffthathadnotbeencausedbyintroductionof
thenails,giventhatthesewereinsertedbelowtheinsertionof
thesupraspinatustendon.However,itshouldbeemphasized
thatbothofthesepatientssaidthattheyweresatisfiedwith
theresultfromthesurgery.
SurgerytoimplantEndernails fortreatinghumeral
dia-physisfracturesisarapidminimallyinvasiveprocedurewith
lower costs than those of other implants. In a
random-izedstudyon91fracturesthatweretreatedsurgicallyusing
dynamic compression plates and Ender nails, Chiu et al.6
showedthatthebloodlosswassmallerandthedurationof
theoperationwasshorterintheprocedurewithEndernails,
whichcorroboratesthefindingsofthepresentstudy.These
dataclearlypresentreductionsincostsandmorbidityforthe
patientandforthehealthcaresystem.
Asurveyofcostsconductedinthepurchasingdepartment
oftheLifecenterHospital,relatingtothepriceschargedbythe
largesthealthcareplanproviderintheMetropolitanRegionof
MinasGerais,showedthevaluesdisplayedinTable1.
Thepresentstudyhadthefollowinglimitations:(1)itwasa
retrospectivestudy;(2)itwasacaseseriesstudywithalimited
sample,whichmadestatisticalanalysisimpossible.
Conclusion
Fixation of the humeral diaphysis fractures using Ender
intramedullarynailswasshowntobeasafeprocedure,with
promising preliminary clinical and functional results. New
studieswithhigherlevelsofevidenceneedtobeconducted
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1. EnderHG.Treatmentofpertrochantericandsubtrochanteric
fracturesofthefemurwithenderpins.In:.In:TheHip:
ProceedingoftheSixthOpenScientificMeetingoftheHip
Society.1978.p.187–206.
2. HallRFJr,PankovichAM.Endernailingofacutefracturesof
thehumerus.Astudyofclosedfixationbyintramedullary
nailswithoutreaming.JBoneJointSurgAm.
1987;69(4):558–67.
3. SarmientoA,ZagorskiJB,ZychGA,LattaLL,CappsCA.
Functionalbracingforthetreatmentoffracturesofthe
humeraldiaphysis.JBoneJointSurgAm.2000;82(4):478–86.
4. KlenermanL.Fracturesoftheshaftofthehumerus.JBone
JointSurgBr.1966;48(1):105–11.
5. SarmientoA,KinmanPB,GalvinEG,SchmittRH,PhillipsJG.
Functionalbracingoffracturesoftheshaftofthehumerus.J
BoneJointSurgAm.1977;59(5):596–601.
6. ChiuFY,ChenCM,LinCF,LoWH,HuangYL,ChenTH.Closed
humeralshaftfractures:aprospectiveevaluationofsurgical
treatment.JTrauma.1997;43(6):947–51.
7.CarrollEA,SchweppeM,LangfittM,MillerAN,HalvorsonJJ.
Managementofhumeralshaftfractures.JAmAcadOrthop
Surg.2012;20(7):423–33.
8.BrumbackRJ,BosseMJ,PokaA,BurgessAR.Intramedullary
stabilizationofhumeralshaftfracturesinpatientswith
multipletrauma.JBoneJointSurgAm.1986;68(7):960–70.
9.OuyangH,XiongJ,XiangP,CuiZ,ChenL,YuB.Plateversus
intramedullarynailfixationinthetreatmentofhumeral
shaftfractures:anupdatedmeta-analysis.JShoulderElbow
Surg.2013;22(3):387–95.
10.WalkerM,PalumboB,BadmanB,BrooksJ,GelderenJV,
MighellM.Humeralshaftfractures:areview.JShoulder
ElbowSurg.2011;20(5):833–44.
11.McCormackRG,BrienD,BuckleyRE,McKeeMD,PowellJ,
SchemitschEH.Fixationoffracturesoftheshaftofthe
humerusbydynamiccompressionplateorintramedullary
nail:aprospective,randomizedtrial.JBoneJointSurgBr.
2000;82(3):336–9.
12.LiebergallM,JaberS,LasterM,Abu-SnienehK,MattanY,
SegalD.Endernailingofacutehumeralshaftfracturesin
multipleinjuries.Injury.1997;28(9–10):577–80.
13.GerberC,MastJW,GanzR.Biologicalinternalfixationof
fractures.ArchOrthopTraumaSurg.1990;109(6):
295–303.
14.LivaniB,BelangeroWD.Osteossíntesedefraturadiafisáriado
úmerocomplacaemponte:apresentac¸ãoedescric¸ãoda