w w w . r b o . o r g . b r
Review
Article
Injuries
to
posterolateral
corner
of
the
knee:
a
comprehensive
review
from
anatomy
to
surgical
treatment
夽
Bernardo
Crespo
a,∗,
Evan
W.
James
a,
Leonardo
Metsavaht
b,
Robert
F.
LaPrade
c,daSteadmanPhilipponResearchInstitute,Vail,UnitedStates bInstitutoBrasildeTecnologiasdaSaúde,RiodeJaneiro,RJ,Brazil
cResearchProgram,SteadmanPhilipponResearchInstitute,Vail,UnitedStates dTheSteadmanClinic,Vail,UnitedStates
a
r
t
i
c
l
e
i
n
f
o
Articlehistory: Received24June2014 Accepted18August2014
Availableonline24December2014
Keywords: Kneeinjuries Kneejoint
Reconstructivesurgical procedures/methods Knee/anatomy&histology Biomechanicalphenomena
a
b
s
t
r
a
c
t
Althoughinjuriestotheposterolateralcornerofthekneewerepreviouslyconsideredtobea rarecondition,theyhavebeenshowntobepresentinalmost16%ofallkneeinjuriesandare responsibleforsustainedinstabilityandfailureofconcomitantreconstructionsifnot prop-erlyrecognized.Althoughalsoonceconsideredtobethe“darksideoftheknee”,increased knowledgeoftheposterolateralcorneranatomyandbiomechanicshasledtoimproved diagnosticabilitywithbetterunderstandingofphysicalandimagingexaminations.The managementofposterolateralcornerinjurieshasalsoevolvedandgoodoutcomeshave beenreportedafteroperativetreatmentfollowinganatomicalreconstructionprinciples.
©2014SociedadeBrasileiradeOrtopediaeTraumatologia.PublishedbyElsevierEditora Ltda.Allrightsreserved.
Lesões
do
canto
posterolateral
do
joelho:
uma
revisão
completa
da
anatomia
ao
tratamento
cirúrgico
Palavras-chave: Lesõesdojoelho Articulac¸ãodojoelho Procedimentosdecirurgia reconstrutiva/métodos
Anatomia&histologiadojoelho Fenômenobiomecânico
r
e
s
u
m
o
Emboraaslesõesdocantoposterolateraldojoelhotenhamsidopreviamenteconsideradas comoumacondic¸ãorara,elasestãopresentesemquase16%detodasaslesõesdejoelho esãoresponsáveispelainstabilidadesustentadaefalhadasreconstruc¸õesconcomitantes casonãotenhamsidoadequadamentereconhecidas.Emboratenhasidoconsideradocomo o“ladonegrodojoelho”,omaiorconhecimentodaanatomiaedabiomecânicadocanto posterolateral levouàmelhoriada capacidadediagnósticaeà melhorcompreensãodo examefísicoedeimagem.Omanejodaslesõesdocantoposterolateralevoluiue bons
夽
StudyconductedattheSteadmanPhilipponResearchInstitute,Vail,UnitedStatesandInstitutoBrasildeTecnologiasdaSaúde,Rio deJaneiro,RJ,Brasil.
∗ Correspondingauthor.
E-mail:drbernardocrespo@gmail.com(B.Crespo).
http://dx.doi.org/10.1016/j.rboe.2014.12.008
desfechos têm sido relatados após o tratamento cirúrgico que segue princípios da reconstruc¸ãoanatômica.
©2014SociedadeBrasileiradeOrtopediaeTraumatologia.PublicadoporElsevier EditoraLtda.Todososdireitosreservados.
Introduction
Posterolateralinstabilitymaycausesignificantfunctional lim-itations.Althoughpreviouslyconsideredrare,posterolateral corner(PLC)injurieshavebeenincreasinglyrecognizedand accountforapproximately16%ofallkneeligamentinjuries,1 oftenpresentingwithconcomitantanteriorandposterior cru-ciateligamentinjuries.2–4Failuretodetecttheseinjurieshas beenshowntobeanimportantcauseofrecurrent instabil-ity and failed cruciate ligament reconstructions.5–10 In the past,treatmentoflateralsideinstabilityhasbeen challeng-ingduetolimiteddataontheanatomyandbiomechanicsof thePLCstructuresandunder-reportingofclinicaloutcomes followingnon-operativeand operative treatment. However, morerecently,theanatomyandbiomechanicshavebecome well-defined and good outcomes have been reported after PLCoperativetreatment followinganatomicreconstruction principles.11Thepurposeofthisarticleistoreviewthecurrent stateofknowledgeregardingPLCinjuries.
Anatomy
and
biomechanics
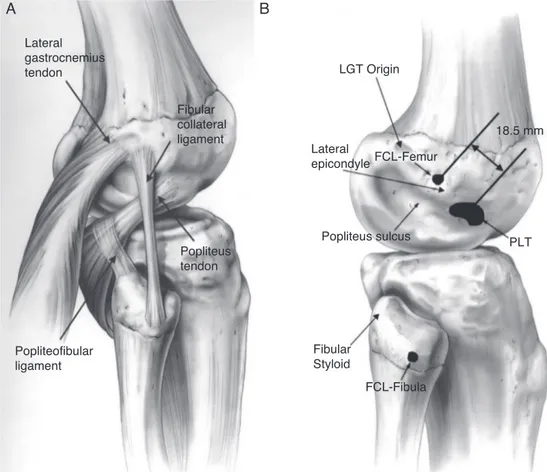
Appreciationofthecomplexanatomyand biomechanicsof thePLCiscriticalforunderstandingthephysicalexam, imag-ing,andtreatmentofPLCinjuries.Themainstructuresthat providestabilitytothelateralaspectofthekneearethefibular collateralligament(FCL),popliteustendon,and popliteofibu-larligament.8,12–15(Fig.1).
TheFCLisaligamentous structurethatoriginatesfrom adepressionlocated1.4mmproximaland3.1mmposterior to the lateral epicondyle.15 The distal insertion is located 28.4mmdistaltothetipofthefibulahead.15TheFCL aver-ages7cminlengthandcoursesunderneaththesuperficial layeroftheiliotibialband.TheFCLactsastheprimary sta-bilizertovarusstressonthekneeandhelpsstabilizeagainst externalrotationtorqueinlowerdegreesofflexion.16
The popliteus tendon runs obliquely from the postero-medialaspect of the tibia becoming more tendinous as it courseslaterally.Itinsertsonarelativelybroadarea(59mm2)
ontheanteriorfifthofthepopliteussulcus,justposteriorto thelateralfemoralcondylearticularcartilagesurface.15This insertionsiteisconsistentlyanteriortotheFCLinsertionsite byanaveragedistanceof18.5mm,15demonstratingthatan anatomicreconstructionisnotachievablewithaonefemoral tunneltechnique.Thepopliteustendonrunsunderneaththe FCL,throughthefemoralpopliteussulcusandbecomes intra-articularontheposterioraspectofthelateralfemoralcondyle. The popliteofibular ligament is consistently present, originating from popliteusmusculotendinous junction and insertingontheposteromedialaspectofthefibulahead.Both
thepopliteustendonandpopliteofibularligamentcontribute to external rotatory stability. The posterolateral complex and the posterior cruciate ligament (PCL) have a synergis-ticrelationship,withthePCLactingasasecondaryrestraint preventingexternalrotationandthePLChelpinginresisting posteriortibialtranslation,mostlyinlowerdegreesofflexion. Otherstructuresarealsofoundintheposterolateral cor-nerofthe knee.Thelong headofthebicepsattachmentis dividedintoadirectarmthatattachesintheposterolateral aspectofthefibulaheadandananteriorarmthatfansout superficialtotheFCL,formingabursathatmustbeaccessed duringanFCLreconstruction.Theposteriormostaspectofthe posterolateralcorneriscomposedofthelateralheadofthe gastrocnemiusmuscle,whichattachesonthesupracondylar ridge on the lateral femoral condyle. In addition, the gas-trocnemiusisanimportantlandmarkduringaPLCsurgical procedurebecausetheareabetweenthegastrocnemius mus-cle bellyand the posterolateral capsuleand soleus muscle mustbedissecteddowntoallowplacementofretractorsto protecttheneurovascularbundleduringtibialtunneldrilling. Theiliotibialbandisathickfascialstructurethatruns super-ficialtothetensorfasciaelatamuscle,immediatelyunderthe subcutaneoustissue,andcoversallofthePLCfemoral attach-ments.Itoriginatesontheanteriorsuperioriliacspineandthe externallipoftheiliaccrestandinsertsonthelateralaspect oftibiaatGerdy’stubercle.
Thecommonperonealnerveoriginatesfromabifurcation ofthesciaticnerveinthedistalthigh.Thenerverunsdistal, lyingposteriortothelongheadofthebiceps,andcrossing around thelateral aspectofthefibula neckbeforedividing intosuperficialanddeepperonealnerves.Theproximityofthe nervetothePLCstructuresmakesidentificationand neuroly-sisofthenerveimportantaspectsofthesurgicaltechnique.
Thelateralsideofthekneeisinherentlyunstabledueto the lack ofconformity betweenthe convex lateral femoral condyleand the convextibiallateral plateau,coupledwith higher mobility ofthe lateral meniscus.17 Additionally, the normalmechanicalaxisofthemainpopulationcrossesthe kneeslightlymedialtotheneutralaxisofthekneeand,during theadductormoment,thisaxisbecomesevenmoremedial. TheintegrityofthePLCisofparamountimportancetoavoid theopeningofthelateralsideofthejointandoverloadingof themedialcompartment.
Lateral gastrocnemius tendon
Fibular collateral ligament
Popliteus tendon
Popliteofibular ligament
Fibular Styloid
FCL-Fibula Popliteus sulcus Lateral
epicondyleFCL-Femur
LGT Origin
18.5 mm
PLT
A
B
Fig.1–Anatomyoftheposterolateralcornerisrepresented(A)withthethreemainstructuresresponsibleforlateralside stability:popliteustendon,popliteofibularligamentandfibularcollateralligament.Theanatomicalfootprintsofthese structuresarehighlightedin(B)B.(ReprintedwithpermissionfromAmJSportsMed.2003;31:854–860.).
stabilizertovarusstressatalldegreesofflexion.The high-estloadontheFCLoccursat30◦ offlexionwhensecondary stabilizerscontribute less.Novarus gapping occursin PLC injurieswheretheFCLremainsintact.However,aFCLinjury associatedpopliteuscomplexinjurypresentswithincreased varusgappingcomparedtoanisolatedFCLinjury. Tradition-ally,thepopliteuscomplexwasunderstoodtobetheprimary restrainer of the external rotation ofthe knee.18 However, recentstudieshavedescribedthatthe FCLhelpstocontrol externalrotation inthe beginning of knee flexion (0–30◦),5 while the popliteus complex controls external rotation at higherdegreesofknee flexion.ThePCLalsocontributesto externalrotatorystabilityasasecondaryrestrainer whena PLCinjuryispresentmosteffectivelyafter90◦offlexion.
Evaluation
Clinicalevaluation
Anaccurate assessmentofPLC injuriesis importantsince thefailuretodiagnoseandtreatPLCinstabilitycanleadto recurrentinstabilityandfailureofconcomitantreconstruction procedures.6,19ThePLCpatientusuallypresentswithahistory ofacutetraumarelatedtomotorvehicleaccidentsandsports injuries.20 Blunt trauma tothe anteromedial aspect ofthe tibiawithaposterolateraldirectedforce,kneehyperextension,
andexternaltibialrotationoverafixedfootarethemost com-moninjurymechanisms.21Inacutecases,painoverthejoint line,ecchymosis,swelling,andinabilitytowalkarethemain complains.Inchroniccases,instabilitywithside-to-site activi-tiesandlimitedabilitytoresumesportsactivitiesarecommon complaints.Usually,PLCinjuriesareassociatedtoACLorPCL tears,withonly28%ofallPLCinjuriesbeenanisolatedtears.22 Regarding the knee physical exam,a detailed examina-tionshouldbeperformedtoassessrangeofmotion,patellar instability,andextensorfunctionandtolookforpossible con-comitantinjuries.Severalspecialtestshavebeendescribedfor assessingposterolateralinstabilityincludingthevarusstress test, posterolateraldrawertest,dialtest,reverse pivot-shift test,andexternalrotationrecurvatumtest.
posterior directed force is applied against the tibia and a positivetestconsistsofincreasedposteriortranslationand externalrotationwhen comparedtothe contralateralside, indicatinginjuryofFCL,popliteustendon,andpopliteofibular ligament.
Withthepatientinthesupineposition,theexternal rota-tionrecurvatumtestisperformedbyliftingthepatient’sleg bythe greattoe whilestabilizing the distalthigh withthe otherhand.Theamountofgenurecurvatumproducedbythe maneuvershouldbecomparedtothe uninjuredside. Mea-surementofthe heal heightsusing a ruler can objectively determinetheamountofrecurvatum.Anegativetestshould beinterpretedwithcautionduetothehighincidenceoffalse negativeresults.
Thereverse pivot-shift testis performed bypositioning the patientinsupineposition withthe kneeflexedto 90◦. A valgusload and externalrotation force isapplied while the knee is slowly extended. If a PLC injury is present, the load will cause posterolateral subluxation ofthe tibial plateauand,whenthe knee reachesaround30◦ offlexion, the iliotibial band willcause totibia toabruptly reduce. A positivereversepivot-shiftmustalwaysbecomparedtothe uninjuredsidebecauseit canbepositivein35%ofnormal knees.
Rotational stabilitycanbe evaluatedusingthe dialtest. Thedialtestisperformedwiththepatientbothintheprone and supinepositions bystabilizing the patient’s thigh and applying an external rotation force at the patient’s ankle. Thetestisperformedbothat30◦ ofkneeflexionandat90◦ of knee flexion. If the patient presents with a PLC injury, aside-to-sidedifference ofmorethan 10◦ ofexternal rota-tionisexpectedat30◦offlexion.BecausethePCLfunctions asa secondary stabilizerofexternalrotation, especially at higherdegreesofflexion,adecreaseintheexternalrotation shouldbeseeninisolatedPLCinjuriesat90◦.Iftheexternal rotationincreasesat90◦,acombinedPLCandPCLinjuryis present.
In addition, gait must be assessed for varus thrust or hyperextensionpatterns,andtheoveralllimbalignmentmust be evaluated because this could change the surgical plan forchronicinjuries.Limbalignmentandweightbearingaxis should be evaluated using long-leg radiographs. A line is extendedonthe radiographfrom thecenterofthefemoral headtothecenteroftheanklemortisejoint.Thelineshould passwithintheregionoftheeminencesonthetibialplateau. IfthepatientisinvarusalignmentandhasachronicPLCtear, anopeningwedgehightibialosteotomywithbonegrafting isrecommendedtocorrectthealignmentdeformitypriorto performingaPLCreconstructionprocedure.
Finally, trauma related to isolated and combined PLC injuries endangers the posterior neurovascular bundle. A poplitealarteryinjurymaybepresentinasmanyas32%of knee dislocations,25 making assessmentofdistal pulsesat thefootandankleanimportantpartoftheinitialevaluation. Theperonealnervemayalsobeinjured,with13%ofallPLC injuries26presentingsymptomsthatmustbeidentifiedand documented. Adetailed physicalexam recording paresthe-siasornumbnessover thedorsumofthe footandthefirst webspace,muscleforcegradingforankledorsiflexion,foot eversion,andgreattoeextensionmustbeperformed.
Imaging
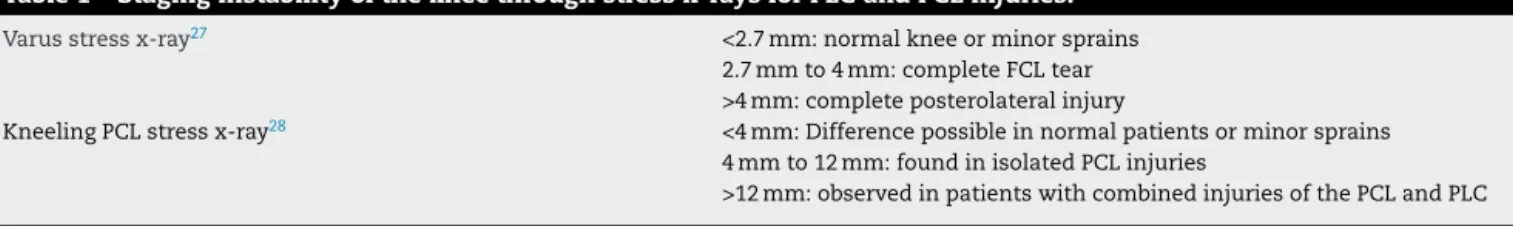
Aroutinex-ray workupwithstandinganteroposterior(AP), lateral, andaxial views should beacquired torule out the presenceoffractures.Astandinglong-legAPviewshouldbe obtainedinchroniccasesbecausethelimbalignmentshould becorrectedusinganosteotomypriortooratthesametime ofthereconstructionprocedure.Additionally,varusandPCL stress X-rayscanbeusedtoobtainobjectivequantification oftheamountoflateralcompartmentvarusgappinganda combinedPLCandPCLinjury,respectively(Table1).
Themagneticresonanceimaging(MRI)isanother impor-tant toolforPLCmanagement that allowsidentificationof concurrentlesionssuchasmeniscustears,cartilagelesions, and occultfractures. It hasbeen shown to have90% sen-sitivity andspecificityforITband,bicepstendon, FCL,and popliteustendoninjury. TheonlyPLCstructurewith lower diagnosticaccuracyvalueswasthepopliteofibularligament, with68.8%sensitivityand66.7%specificity.1,29 However,for theoptimalMRIdiagnosticaccuracyforPLCinjuries,an imag-ing sequence using 2mm slicesin acoronaloblique plane followingtheobliquity ofthe popliteustendon30 shouldbe employed.Finally,bonebruisepatternscanofferadditional cluestothepresentinjury,sincethesearefoundin81%ofall PLCinjuries,usuallyontheanteromedialfemoralcondyle.22 Together,theseimagingtechniquesareexcellenttoolsto aug-mentthediagnosisofPLCinjury.
Classificationandtreatmentrationale
Treatment of PLC injuries depends mostly on the injury grade,chronicity,andpresenceofassociatedinjuries.Despite its subjectivity and a lack of relation to anatomic cutting studies, the Hughston classification31 is still very impor-tantfortreatmentguidance.Adifferentclassificationsystem describingrotationalinstabilitywascreatedbyFanellietal.32
(Table2).
Althoughnon-surgicalmanagementofPLCinjuriesisnot welldocumentedintheliterature,itseemstobeeffectivein gradesIandIIisolatedPLCacuteinjuries.Thelow symptoma-tologyoflowgradePLCinjuriescanmaketheevaluationof thissmallsubgroupdifficult.Goodresultsfornon-operative treatmentofPLCgradesIandIIinjurieswerereported pre-viously using an early mobilization protocol.33,34 Minimal radiographicchangeswerefoundat8yearsfollow-up.By con-trast,gradeIIIPLCinjuriestreatednon-operativelyhadpoor functional outcomes, persistent instability, and increased degenerative arthritic changes.33,34 The rehabilitation pro-tocol used by the authors for PLC conservative treatment consists ofknee bracing witha knee immobilizer orbrace lockedinextensionfor4–6weeks.Weightbearingisusually allowedandprogressesastolerated.Activeandpassiverange ofmotionexercisesinthepronepositionareencouragedto preventstiffness.Comparativestressx-raysafter6weeksare recommendedtoassessforremaininglaxity.Aftertheinitial healingperiod,sports-specifictherapyisinitiatedandreturn tosportisallowedwithin3–4monthsifgoodbalance, muscu-larstrength,andmuscularenduranceareachieved.
Table1–Staginginstabilityofthekneethroughstressx-raysforPLCandPCLinjuries.
Varusstressx-ray27 <2.7mm:normalkneeorminorsprains
2.7mmto4mm:completeFCLtear >4mm:completeposterolateralinjury
KneelingPCLstressx-ray28 <4mm:Differencepossibleinnormalpatientsorminorsprains 4mmto12mm:foundinisolatedPCLinjuries
>12mm:observedinpatientswithcombinedinjuriesofthePCLandPLC
Table2–ClassificationforthePLCinstabilitiesasproposedbyHughston29andFanelli30.
HugstonScaleforFCLinstability31(basedonlyinthevarus stressopeningcomparedtotheoppositeside)
GradeI:0–5mm* GradeII:5–10mm* GradeIII:>10mm* FanelliClassificationforPLCinstability32
(locationbased,addressesrotationalinstability)
TypeA:mainlyrotationalinstability(popliteustendonandpopliteofibular ligamenttear)
TypeB:rotationalinstabilitywithamildvarusstressgrapping(popliteus tendon,FCLandpopliteofibularligamentinjury)
4mmto12mm:foundinisolatedPCLinjuries
TypeC:disruptionofthePLCstructureswithacruciateligamentinjury, markedvarusandexternalrotationinstability
∗ Openingdifferencefromthecontralateralside.
injuries,andfailednon-operativetreatment.Acutesurgical treatment(<3weeks)resultsinimprovedoutcomes14,35,36and canavoidthenecessityofanadditionalprocedureforlimb alignmentcorrectionthatmaybenecessaryinchroniccases. Patientstreatedacutelymayundergorepairor reconstruc-tionprocedures.PrimaryrepairsofFCLandpopliteustendons avulsions,without midsubstance injury,may beperformed within2–3weeksaftertheinjury.Afterthatpoint,thetissue becomesretractedandscarsdown,makingitnearly impossi-bletoreattachtheinjuredstructurestotheirnativeanatomic locations.However,midsubstance tears cannotbe repaired regardless the time of the injury. Stannard et al.37 evalu-atedrepairvs.reconstructionoutcomesafterPLCinjuriesand reportedhigherfailureratesintherepairgroup(9%vs.37%). Theresultswere confirmedbyalaterstudybyLevyetal.38 with6%failureforreconstructionsversus40%forrepairs.
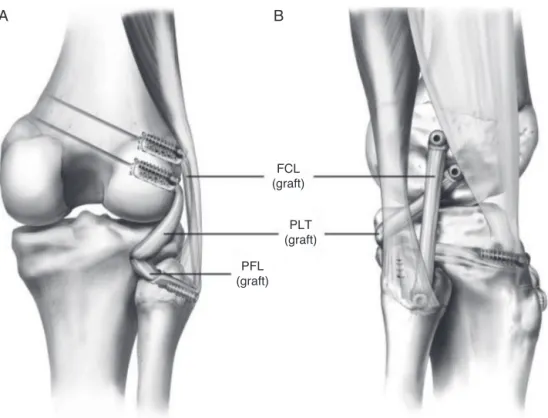
SeveralPLCreconstructionprocedureshavebeendescribed andcanbeclassifiedasanatomicandnon-anatomic accord-ingtotheligamentsreconstructedandthepositioningofthe reconstructiontunnels. TheClancyprocedure39 consistsof abicepstenodesisonthedistallateralfemurtomimicthe FCL.Thetechniquerecommendstheplacement ofa screw andwasheratapointanteriortothelateralepicondyleand re-routingthebicepstendonorastripofthetendonabove thescrew.Thiscreatesan“isometric”constructtoreplacethe FCL andreestablishvarus stability. TheLarsontechnique40 isperformedbyreconstructingtheFCL withaverticalgraft limbfromtheanterioraspectofthefibulaheadtothelateral femoralcondyle,whileaddinganobliquegraftlimbfromthe posterioraspectofthefibulaheadtothefemoralepicondyle. However,therationalewasstillplacingthefemoraltunnelin anisometric,non-anatomicpoint.Modificationsofthe Lar-sontechniqueweredevelopedbyFanelliandArcieroandaim toachieveamoreanatomicalfemoralFCLgraft placement. Fanellietal.32usesawasherlockinthemidpointinbetween FCLandpopliteustendonandcrossesthegraftinafigureof eight.Arciero41drillstwoholesonthefemoralsiteto recre-atethefootprintofpopliteustendonandFCL.However,both
techniquesstilluseonlyonegraftwithtwolimbsto recon-structthreemajorPLCstructuresandfailtoreproducenative anatomy.
TheStannardetal.42 reconstructiontechniqueisa non-anatomic technique that reconstructs the FCL, popliteus tendon, andpopliteofibular ligament.Ananterior or poste-riortibialisallograftwithaminimum24mmlengthisused. Afterperforminganexposureofthelateralknee,atibia tun-nelisdrilledfromanteriortoposterior,exitingatthepopliteus musculotendineousjunctiononthetibia.Asecondtunnelis createdthroughthefibulaheadfromanterolateralto postero-medial,exitingonthefibulastyloid.Athirdfixationpointfor ascrewandwasheriscreatedonthelateralfemoralcondyle, justanteriortowhereFCLandpopliteustendoncrosseach otheratthetheoreticalisometricpointonthefemoralcondyle. Afterallthetunnelsareprepared,thegraftispassedthrough thetibialtunnelfromfronttobackandsecuredwithan inter-ferencescrew,exitingtheposterioraspectofthetibia.Thefree limbofthegraftispassedinthepopliteussulcusandlooped aroundthefemoralscrew,re-routedthroughthefibulartunnel from posteriortoanterior,beforeexitingthrough the ante-rioraspectofthefibularheadandthenbacktothescrewand washer.Althoughthethreemajorstructuresarereconstructed inthistechnique,thereconstructionisnon-anatomicsinceit doesnotplacethereconstructiontunnelsatthelocationof thenativefootprints.
FCL (graft)
PLT (graft)
PFL (graft)
A
B
Fig.2–Anatomicalreconstructionoftheposterolateralcornerwithtwofreegraftsreconstructingthethreemajor
structures,throughtwofemoraltunnels,onetibialtunnelandonefibulartunnel.(ReprintedwithpermissionfromAmJSports Med.2010;38:1674–1680.).
assesstotheposterioraspectoftheknee.Asmall horizon-talincisioniscreatedoverthebicepsbursa,exposingtheFCL distalfibersandfibularattachment.
Bluntdissectionbetweenthesoleusandthelateralhead ofgastrocnemiusmuscle iscarried out,allowing the iden-tificationofthemusculotendinousjunctionofthepopliteus andthepopliteofibularinsertiononthefibularhead.Aguide pinispassedfromtheFCLfootprintonthelateralsideofthe fibulaheadtotheposteromedial aspectofthefibulaatthe popliteofibularligament’sattachment.Afterproperposition isconfirmed,aretractorisplacedanda7mmdrillisused toreamthetunnel.Dissectionofaflatareajustdistaltothe Gerdy’stubercleisnextperformedtoidentifythetibial recon-structiontunnelentrypoint.Abluntobturatorisplacedinto thefibulatunneltoserveasapalpableguideforthetibia tun-nelplacement.Thetibialtunnelshouldbe1cmmedialand 1cmproximaltofibulartunnelexitpoint.Anaimingdeviceis usedtopassaguidepinfromtheflatspotentrypoint.After checkingthetunnelposition,aretractorisplacedandthe tun-neliscreatedbyoverreamingtheguidepininananteriorto posteriordirectionwitha9mmreamer.
AlongitudinalopeningintheITbandanteriortothelateral epicondyleisnowperformedinordertoexposethefemoral attachmentsfortheFCLandpopliteustendon.OncetheFCL attachmentisidentified,aguidepinisadvancedacrossthe femurintheanteromedialdirection,avoidingthe intercondy-larnotch. Identifyingthe popliteustendon insertionisthe next step. Previous anatomic studies showed the distance betweenthesetwo attachmentstobe 18.5mm.15 Afterthe insertionareaisidentified,asecondguidepinisplacedacross
thefemur.Thedistancebetweenthetwoguidepinsmustbe confirmedtobe18.5mm.Finally,a9mmdrillisusedtoream toadepthof25mmforbothreconstructiontunnels.
Afteralltunnelsarereamed,theintra-articularprocedure isperformedandallconcurrentligament,meniscal,and car-tilagepathologyshouldbeaddressed.Atthesametime,the grafts maybepreparedatthe backtablebyanassistant.A splitAchillesallograftispreferred,withthecalcaneusbone blocksplitinthemiddle.Two9mmofdiameterand25mm longboneplugsarepreparedandthedistalaspectofthegraft istubularizedwithwhipstitchestofacilitategraftpassageand traction.
Graftfixationbeginsatthefemoraltunnels.Thetwobone plugsarefixedwitha7×20mmmetallicinterferencescrew.
Next, the popliteusequivalent graft ispassed through the popliteushiatusexiting intheposterioraspectoftheknee. TheFCLgraftisthenpasseddistallyoverthepopliteusgraft andunderneaththesuperficiallayeroftheITband.Alooped sutureisusedtoguidethepassageofthegraftthroughthe fibularheadinaposteromedialdirection,exitingintheback oftheknee.TheFCLreconstructionistensionedwiththeknee at20◦flexionwhileapplyingavalgusreductionforceinneutral tibialrotation.Thegraftisfixedwithanabsorbable7×23mm
screwinthefibulaheadtunnel.Thetwofreelimbsofthegrafts arepassedthroughthetibiatunnelfromposteriortoanterior. Thegraftsshouldbetensionedonceagainusingan alternat-ingmotiontoremoveanyresidualslackinthegrafts.Finally, fixationisperformedwitha9×23mmabsorbablescrewwith
Post-operative
rehabilitation
Thepostoperativerehabilitationprotocolconsistsof6weeks ofnon-weightbearingwhilewearinganimmobilizerbracein fullextensionatalltimes,exceptduringrangeofmotion exer-ciseswhichareinitiatedonpostoperativedayone.Quadriceps setsandpatellarmobilizationshouldbestartedimmediately. Hamstringssets should beavoidedin thefirst 6weeks, to minimizetheriskofthegraftsstretchingout.Atthe6-week point,thepatientcanstartweightbearingastoleratedand theimmobilizerbracecanbediscontinuedifthepatient is abletoperformastraight legraise withoutalag of exten-sion.Bikingexercisescanbeaddedassoonas100◦ ofknee flexion is achieved. Sports specific training is started at 4 months.Varus stressradiographsare obtainedat6months post-operativelytoassessforstability.Returntosports activ-itiesisdelayeduntilanormalrangeofmotion,strength,and stabilityisachieved(usuallyafter6to9months).
Outcomes
The anatomic reconstruction technique has demonstrated the ability toreduce objective laxityon varus stress x-ray from6.2mmpreoperatively toa0.1mmside-to-side differ-enceatfinalfollow-up.TheCincinnatiandIKDC45subjective outcomesscoresincreasedsignificantlyfrom21.9and 29.1, respectively,to81.4and81.5.36
Forchronic cases,thelimbalignmentmust beassessed priortoareconstructionsurgery.Varusalignmentstressesthe PLCreconstructiongrafts,46,47andneedstobecorrectedprior toanyothersurgicalprocedure.Ahightibialmedialopening wedgeosteotomywasdemonstratedtoreducelaxityinPLC injuredknees.In38%ofpatients,theimprovementinstability wasenoughthatthepatientdidnotneedanadditionalPLC reconstructionsurgery.48,49
Conclusion
Theposterolateralcorner,previouslyknownasthe“darkside oftheknee”,hasbeensubjectofinnumerousstudieslately. ImprovedunderstandingofPLCanatomyandbiomechanics hasledtoimproveddiagnosticsanddevelopmentofsurgical techniquesthatsuccessfullyrestorekneestability.
Conflicts
of
interest
Dr LaPrade is aconsultant forArthrex. The others authors declarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1. LaPradeRF,WentorfFA,FrittsH,GundryC,HightowerCD.A
prospectivemagneticresonanceimagingstudyofthe
incidenceofposterolateralandmultipleligamentinjuriesin
acutekneeinjuriespresentingwithahemarthrosis.
Arthroscopy.2007;23(12):1341–7.
2.CsintalanR,EhsanA.Biomechanicalandanatomicaleffects
ofanexternalrotationaltorqueappliedtothekneea
cadavericstudy.AmJSportsMed.2006;34(10):1623–9.
3.FanelliG,OrcuttD,EdsonC.Themultiple-ligamentinjured
knee:evaluation,treatmentandresults.Arthroscopy.
2005;21(4):471–86.
4.FanelliG,EdsonC.Posteriorcruciateligamentinjuriesin
traumapatients:partII.Arthroscopy.1995;11(5):526–9.
5.LaPradeRF,TsoA,WentorfF.Forcemeasurementsonthe
fibularcollateralligament,popliteofibularligament,and
popliteustendontoappliedloads.AmJSportsMed.
2004;32(7):1695–701.
6.LaPradeRF,MuenchC,WentorfF,LewisJL.Theeffectofinjury
totheposterolateralstructuresofthekneeonforceina
posteriorcruciateligamentgraft:abiomechanicalstudy.AmJ
SportsMed.2002;30(2):233–8.
7.LaPradeRF,ResigS,WentorfF,LewisJL.Theeffectsofgrade
IIIposterolateralkneecomplexinjuriesonanteriorcruciate
ligamentgraftforce.Abiomechanicalanalysis.AmJSports
Med.1999;27(4):469–75.
8.HarnerCDC,MauroCSC,LesniakBP,RomanowskiJR.
Biomechanicalconsequencesofatearoftheposteriorrootof
themedialmeniscus.Surgicaltechnique.JBoneJointSurg
Am.2008;91(2):257–70.
9.HarnerC,HöherJ,VogrinT.Theeffectsofapopliteusmuscle
loadoninsituforcesintheposteriorcruciateligamentand
onkneekinematicsahumancadavericstudy.AmJSports
Med.1998;26(5):669–73.
10.NoyesF,Barber-WestinS.Posteriorcruciateligamentrevision
reconstruction,part1:causesofsurgicalfailurein52
consecutiveoperations.AmJSportsMed.2005;33(5):646–54.
11.LaPradeRF,JohansenS,WentorfFA,EngebretsenL,Esterberg
JL,TsoA.Ananalysisofananatomicalposterolateralknee
reconstruction:aninvitrobiomechanicalstudyand
developmentofasurgicaltechnique.AmJSportsMed.
2004;32(6):1405–14.
12.SeebacherJ,InglisA.Thestructureoftheposterolateral
aspectoftheknee.JBoneJointSurgAm.1982;64(4):536–41.
13.WatanabeY,MoriyaH,TakahashiK.Functionalanatomyof
theposterolateralstructuresoftheknee.Arthroscopy.
1993;9:57–62.
14.VeltriD,DengX,TorzilliP,MaynardM,WarrenR.Theroleof
thepopliteofibularligamentinstabilityofthehumankneea
biomechanicalstudy.AmJSportsMed.1996;24(1):19–27.
15.LaPradeRF,LyTV,WentorfFA,EngebretsenL.The
posterolateralattachmentsoftheknee:aqualitativeand
quantitativemorphologicanalysisofthefibularcollateral
ligament,popliteustendon,popliteofibularligament,and
lateralgastrocnemiustendon.AmJSportsMed.
2003;31(6):854–60.
16.SanchezAR,SugalskiMT,LaPradeRF.Anatomyand
biomechanicsofthelateralsideoftheknee.SportsMed
ArthroscRev.2006;14(1):2–11.
17.LapradeRF,WentorfFA,OlsonEJ,CarlsonCS.Aninvivo
injurymodelofposterolateralkneeinstability.AmJSports
Med.2006;34(8):1313–21.
18.LapradeRF,WozniczkaJK,StellmakerMP,WijdicksCA.
Analysisofthestaticfunctionofthepopliteustendonand
evaluationofananatomicreconstruction:thefifthligament”
oftheknee.AmJSportsMed.2010;38(3):543–9.
19.WentorfFA,LaPradeRF,LewisJL,ResigS.Theinfluenceofthe
integrityofposterolateralstructuresontibiofemoral
orientationwhenananteriorcruciateligamentgraftis
20.CoveyD.Injuriesoftheposterolateralcorneroftheknee.J
BoneJointSurgAm.2001;83(1):106–18.
21.FornalskiS,McGarryM.Biomechanicalandanatomical
assessmentafterkneehyperextensioninjury.AmJSports
Med.2008;36(1):80–4.
22.GeeslinAG,LapradeRF.Locationofbonebruisesandother
osseousinjuriesassociatedwithacutegradeIIIisolatedand
combinedposterolateralkneeinjuries.AmJSportsMed.
2010;38(12):2502–8.
23.GollehonD,TorzilliP,WarrenR.Theroleoftheposterolateral
andcruciateligamentsinthestabilityofthehumanknee.A
biomechanicalstudy.JBoneJointSurgAm.1987;69(2):233–42.
24.GroodE,StowersS,NoyesF.Limitsofmovementinthe
humanknee.JBoneJointSurgAm.1988;70(1):88–97.
25.GreenN,AllenB.Vascularinjuriesassociatedwithdislocation
oftheknee.JBoneJointSurgAm.1977;59(2):236–9.
26.LaPradeRF,TerryG.Injuriestotheposterolateralaspectof
theknee.AmJSportsMed.1997;25(4):434–8.
27.LaPradeR,HeikesC.Thereproducibilityandrepeatabilityof
varusstressradiographsintheassessmentofisolatedfibular
collateralligamentandgrade-IIIposterolateralknee.JBone
JointSurgAm.2008;90(10):2069–76.
28.JackmanT,LapradeRF,PontinenT,LenderPA.Intraobserver
andinterobserverreliabilityofthekneelingtechniqueof
stressradiographyfortheevaluationofposteriorkneelaxity.
AmJSportsMed.2008;36(8):1571–6.
29.LaPradeRF,BollomTS,WentorfFA,WillsNJ,MeisterK.
Mechanicalpropertiesoftheposterolateralstructuresofthe
knee.AmJKneeSurg.2005;33(9):1386–91.
30.LaPradeR,WentorfF.Diagnosisandtreatmentof
posterolateralkneeinjuries.ClinOrthopRelatRes.
2002;(402):110–21.
31.HughstonJC,AndrewsJR,CrossMJ,MoschiA.Classification
ofkneeligamentinstabilitiesPartII.Thelateral
compartment.JBoneJointSurgAm.1976;58(2):173–9.
32.FanelliG,StannardJP,StuartMJ,MacDonaldPB,MarxRG,
WhelanDB,etal.Managementofcomplexkneeligament
injuries.JBoneJointSurgAm.2010;60(12):2234–46.
33.KannusP.NonoperativetreatmentofgradeIIandIIIsprains
ofthelateralligamentcompartmentoftheknee.AmJSports
Med.1989;17(1):83–8.
34.KrukhaugY,MølsterA,RodtA,StrandT.Lateralligament
injuriesoftheknee.KneeSurgSportsTraumatolArthrosc.
1998;6(1):21–5.
35.ClancyWJr,SutherlandT.Combinedposteriorcruciate
ligamentinjuries.ClinSportsMed.1994;13(3):629–47.
36.GeeslinAG,LaPradeRF.Outcomesoftreatmentofacute
grade-IIIisolatedandcombinedposterolateralkneeinjuries.J
BoneJointSurgAm.2011;93(18):1672–83.
37.StannardJP,BrownSL,FarrisRC,McGwinG,VolgasDA.The
posterolateralcorneroftheknee:repairversus
reconstruction.AmJSportsMed.2005;33(6):881–8.
38.LevyBA,DajaniKA,MorganJA,ShahJP,DahmDL,StuartMJ.
Repairversusreconstructionofthefibularcollateralligament
andposterolateralcornerinthemultiligament-injuredknee.
AmJKneeSurg.2010;38(4):804–9.
39.ClancyW,ChapmanM.Repairandreconstructionofthe
posteriorcruciateligament.OperOrthop.1988;3:1651–65.
40.LarsonR.Isometryofthelateralcollateralandpopliteofibular
ligamentsandtechniquesforreconstructionusingafree
semitendinosustendongraft.OperTechnSportsMed.
2001;9(2):84–90.
41.ArcieroRR.Anatomicposterolateralcornerknee
reconstruction.Arthroscopy.2005;21(9):1147.
42.StannardJP,BrownSL,RobinsonJTGMJr,VolgasDA.
Reconstructionoftheposterolateralcorneroftheknee.
Arthroscopy.2005;21(9):1051–9.
43.McCarthyM,CamardaL,WijdicksCA,JohansenS,
EngebretsenL,LapradeRF.Anatomicposterolateralknee
reconstructionsrequireapopliteofibularligament
reconstructionthroughatibialtunnel.AmJSportsMed.
2010;38(8):1674–81.
44.LaPradeRF,JohansenS,EngebretsenL.Outcomesofan
anatomicposterolateralkneereconstruction.JBoneJoint
SurgAm.2011;93Suppl1:10–20.
45.MetsavahtL,LeporaceG,RibertoM,deMelloSpositoMM,
BatistaLA.Translationandcross-culturaladaptationofthe
BrazilianversionoftheInternationalKneeDocumentation
CommitteeSubjectiveKneeForm:validityand
reproducibility.AmJSportsMed.2010;38(9):1894–9.
46.NoyesF.Hightibialosteotomyandligamentreconstruction
forvarusangulatedanteriorcruciateligament-deficient
knees.AmJSportsMed.2000;28(3):282–96.
47.LaPradeR,HamiltonC,EngebretsenL.Treatmentoracute
andchroniccombinedanteriorcruciateligamentand
posterolateralkneeligamentinjuries.SportsMedArthrosc
Rev.1997;5(2):91–9.
48.ArthurA,LaPradeRF,AgelJ.Proximaltibialopeningwedge
osteotomyastheinitialtreatmentforchronicposterolateral
cornerdeficiencyinthevarusknee:aprospectiveclinical
study.AmJSportsMed.2007;35(11):1844–50.
49.LapradeRF,EngebretsenL,JohansenS,WentorfFA,
KurtenbachC.Theeffectofaproximaltibialmedialopening
wedgeosteotomyonposterolateralkneeinstability:a
biomechanicalstudy.AmJSportsMed.2008;36(5):