REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
PublicaçãoOficialdaSociedadeBrasileiradeAnestesiologia www.sba.com.brCLINICAL
INFORMATION
Intermittent
left
bundle
branch
block
---
reversal
to
normal
conduction
during
general
anesthesia
Ana
Maria
Oliveira
Correia
da
Silva
∗,
Emília
Alexandra
Gaspar
Lima
da
Silva
CentroHospitalardeEntreoDouroeVouga,Servic¸odeAnestesiologia,SantaMariadaFeira,Portugal
Received3August2016;accepted23November2016 Availableonline8April2017
KEYWORDS Cardiacconduction defects;
Arrhythmia;
Completeleftbundle branchblock; Generalanesthesia
Abstract
Backgroundandobjectives: Transientchangesinintraoperativecardiacconductionare uncom-mon.Rarecasesofthedevelopmentorremissionofcompleteleftbundlebranchblockunder generalandlocoregionalanesthesiaassociatedwithmyocardialischemia,hypertension, tachy-cardia,anddrugshavebeenreported.Completeleftbundlebranchblockisanimportantclinical manifestationinsomechronichypertensivepatients,whichmayalsobeasignofcoronaryartery disease,aorticvalvedisease,orunderlyingcardiomyopathy.Althoughusuallypermanent,itcan occurintermittentlydependingonheartrate(whenheartrateexceedsacertaincriticalvalue).
Casereport: Thisisacaseofcompleteleftbundlebranchblockrecordedinthepreoperative periodofurgentsurgerythatrevertedtonormalintraoperativeconductionundergeneral anes-thesiaafteradecreaseinheartrate.Itresurfaced,intermittentlyandinaheart-rate-dependent manner,intheearlypostoperativeperiod,eventuallyrevertingtonormalconductionina sus-tainedmannerduringsemi-intensiveunitmonitoring.Thetesttoidentifymarkersofcardiac musclenecrosiswasnegative.Painduetotheemergencysurgicalconditionandintheearly postoperativeperiodmayhavebeenthecauseoftheincreaseinheartrateuptothecritical value,causingblockage.
Conclusions:Although the development or remission of this blockade under anesthesia is uncommon,theanesthesiologistshouldbealerttothepossibilityofitsoccurrence.Itmaybe benign;however,thecorrectdiagnosisisveryimportant.Theelectrocardiographic manifesta-tionsmaymaskorbeconfusedwithmyocardialischemia,factorsthatareespeciallyimportant inapatientundergeneralanesthesiaunabletoreportthecharacteristicsymptomsofischemia. ©2016SociedadeBrasileiradeAnestesiologia.PublishedbyElsevierEditoraLtda.Thisisan openaccessarticleundertheCCBY-NC-NDlicense( http://creativecommons.org/licenses/by-nc-nd/4.0/).
∗Correspondingauthor.
E-mail:ana.maria.silva@sapo.pt(A.M.Silva).
http://dx.doi.org/10.1016/j.bjane.2016.11.002
PALAVRAS-CHAVE Defeitosdaconduc¸ão cardíaca;
Arritmia;
Bloqueiocompletode ramoesquerdo; Anestesiageral
Bloqueiointermitentederamoesquerdo---reversãoparaconduc¸ãonormaldurante
anestesiageral
Resumo
Justificativaeobjetivos: Alterac¸õestransitóriasdaconduc¸ãocardíacanointraoperatóriosão poucofrequentes.Foramreportadosraroscasosdedesenvolvimentoouremissãodebloqueio completo deramoesquerdosob anestesia(geral elocorregional),associados aisquemiado miocárdio,hipertensão,taquicardiaefármacos.Obloqueiocompletoderamoesquerdoéuma manifestac¸ãoclínicaimportanteemalgunshipertensoscrônicos,podetambémsignificardoenc¸a arterialcoronária,doenc¸avalvularaórticaoucardiomiopatia subjacentes.Embora habitual-mente permanente,podeocorrernaformaintermitentedependentedafrequênciacardíaca (quandoafrequênciacardíacaexcededeterminadovalorcrítico).
Relatodecaso: Esteéum caso debloqueio completode ramoesquerdo registradono pré-operatório de cirurgia urgente que reverteu para conduc¸ão normal no intraoperatório sob anestesia geralapósdiminuic¸ãodafrequênciacardíaca.Ressurgiu,deformaintermitentee dependenteda frequênciacardíaca,nopós-operatório imediato,acabou porreverter nova-menteàconduc¸ãonormaldeformasustentadadurantevigilânciaemunidadesemi-intensiva. Oestudocommarcadoresdenecrosemuscularcardíacosfoinegativo.Adordoquadrocirúrgico urgenteepós-operatórioimediatopodeterestadonaorigemdasubidadafrequênciacardíaca atéaovalorcríticoecausadobloqueio.
Conclusões: Emboraodesenvolvimentoouaremissãodessebloqueiosobanestesiasejam inco-muns,oanestesiologistadeveráestaralertadoparaapossibilidadedasuaocorrência.Podeter caráterbenigno,contudoodiagnósticocorretoémuitoimportante.Asmanifestac¸ões eletro-cardiográficaspodemserconfundidascomouencobririsquemiamiocárdica,fatosdeespecial importâncianumpacientesobanestesiageralincapazdereferirsintomatologiacaracterística deisquemia.
©2016SociedadeBrasileiradeAnestesiologia.PublicadoporElsevierEditoraLtda.Este ´eum artigo OpenAccess sobumalicenc¸aCCBY-NC-ND( http://creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
Acompleteleftbundle-branchblock(LBBB)developmentor remissioninpatientsunderanesthesiaisuncommon.1---4The
heartrate-dependentintermittentblockmaybebenign5,6;
however, the correct diagnosis is very important. The electrocardiographicmanifestationsmaybeconfusedwith or mask a myocardial ischemia,5,7 facts of particular
importance in a patient under general anesthesia unable to describe the characteristic symptoms of myocardial ischemia.
We reportacase ofcomplete preoperative leftbundle branch block that reverted to normal conduction after a decreasein heartrate duringsurgeryundergeneral anes-thesiaandwhichresurgedintermittentlyanddependenton heartrateintheimmediatepostoperativeperiod.
Clinical
case
A73-year-old femalepatientsuspected of iatrogenic per-foration of the sigmoid colon during colonoscopy with polypectomy was referred for urgent exploratory laparo-tomy.Pre-anestheticevaluationrevealedamedicalhistory ofbronchialasthma,hypertension,type2diabetesmellitus, gastritis, hiatal hernia, obesity, and depressive syn-drome. Anesthetichistory included generalanesthesiafor
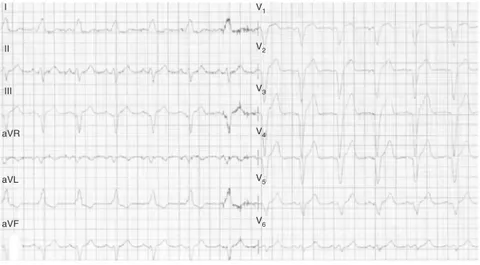
hysterectomyandlocoregionalanesthesiaforvaricosevein surgery,withnoknowncomplications.Physicalexamination revealedonly abdominalpain,withnosignsof peritoneal irritationor significantdysfunctionof other organsor sys-tems.Laboratorytestsshowedleukocytosis(21,100mm−3), withno other distinct changes in blood count, renal and hepaticfunctions, orionogram.ArterialBloodgasanalysis showednochanges.ECGshowedsinusrhythmwith82bpm andapatterncompatiblewithcompleteleftbundlebranch block(LBBB)(Fig.1).The patientremainedwithoutchest pain and with blood pressure and heart rate (HR) values withinnormal range fromhospital admission toarrival in theoperatingroom.
Duetotheurgentnatureofthesurgeryandthe hemody-namicstability,itwasdecidednottopostponethesurgical procedurefor furtherstudy of electrocardiographic alter-ations.
On admission to the operating room, the patient pre-sented with blood pressure of 123/69mmHg, HR 83bpm, peripheral oxygen saturation 96%, and LBBB. Under the American Society of Anesthesiologists monitoring stan-dards,induction ofgeneralanesthesiawithpropofolbolus (2mg·kg−1)andinfusionofremifentanil(0.5g·kg−1forone
minute,followedby0.1g·kg−1·min−1)andneuromuscular
blockwithrocuronium(0.6mg·kg−1),afterwhichthe
II
III
aVR
aVL
aVF
1
V2
V3
V4
V5
V6
Figure1 Preoperative12-leadECGwithaLBBB-compatiblepattern.
II I
III
aVR
aVL
aVF
V1
V2
V3
V4
V5
V6
Figure2 Intraoperative12-leadECGwithnormalconduction,withoutLBBB.
of bronchospasm followed the administration of intra-venoushydrocortisone(100mg)andsalbutamol(400g)and ipratropium bromide (40g) via expander chamber. For maintenance of anesthesia, oxygen, air, and sevoflurane (FiO235%,end-tidalsevofluraneconcentrationof1.8%)and
remifentanil infusion (0.1---0.2g·kg−1·min−1) were used.
Ventilationwasmechanicallycontrolled.Analgesiawas per-formedwithparacetamol(1g)andtramadol(150mg)and antiemetic prophylaxis with intravenous dexamethasone (4mg at induction) and ondansetron (4mg at the end of surgery).
Intraoperatively,afterabout30minofanesthesia,LBBB revertedtonormalconduction,atwhichpointHRreached 74bpmafteragradualreduction,thusremainingduringthe 2hofsurgery.Meanarterialpressurevariedbetween73and 80mmHgandHRbetween65and74bpmduringthisperiod. At theend of the surgery, but still beforethe anesthesia reversal, a 12-lead ECG wasperformed, which confirmed absenceofLBBB(Fig.2).
Thepatientwasthenawakened,andtheneuromuscular blockreversedwithsugammadex(200mg).
Upon arrival at the post-anesthesia care unit (PACU), themonitoringshowedbloodpressureof125/66mmHg;HR 86bpmandECGwithLBBBpattern,whichwasmaintained
intermittently and dependent on HR≥75bpm over 2h of
surveillance.Duringthisperiod,twobolusesofintravenous morphine(2mg)wereadministeredforpainmanagement. Therewerenochangesinbloodpressureduringtheblockade periods.
After a joint evaluation by the PACU anesthesiologist and the physician responsible for the semi-intensive care unit, the patient was admitted to this unit for clini-cal,laboratory,andelectrocardiographicsurveillance.The patientremainedasymptomaticthroughoutthestayinthis unit, the markers of cardiac muscle necrosis were nega-tive, and serialECGs showed noblockade. An emergency cardiologistevaluatedtheresultsandestablishedthe diag-nosis of intermittent LBBB, with no need for particular care. The patient was taken then tothe general surgery care unit, and the remaining postoperative period was uneventful.
Discussion
and
conclusions
Branchblockmayoccurinseveralsituations.LBBBisan importantclinicalmanifestationinsomechronic hyperten-sive subjects. It may also imply coronary artery disease, aortic valve disease, or underlying cardiomyopathy.9 In
youngadultsitisoftenabenignfinding,6,10butintheelderly
it may represent progressive myocardial degeneration affectingtheconductivesystem.9Delayedintraventricular
conduction may also be caused by extrinsic factors that decreaseconduction,suchashyperkalemiaordrugs (antiar-rhythmics,tricyclicantidepressants,andphenothiazines).
Impaired conduction in the bundle of His (or bundle branches)iselectrocardiographicallytranslatedintoaQRS intervalprolongation(≥120msincompletebranch block);
QRSvectorisdirectedtothemyocardialregionwhere depo-larizationisdelayed.8Leftbundlebranchblockchangesthe
early andlatestages ofventricular depolarization.Septal depolarizationabnormallyoccursfromrighttoleft,andthe main QRS vector is oriented to the left and backwards.8
Thus,aLBBBgeneratescomplex,elongated,and predomi-nantlynegativeQSintherightprecordialleadsandcomplex and fully positive R (absence of physiological Q-waves) in lead V6.8 In addition to these depolarization changes,
the blockade is also characterized by secondary changes in ventricular repolarization. Although depolarization and repolarizationcausedeflectionsofoppositepolarityatthe cellular level, under normal conditions the QRS complex and the T-wave have the same polarity, as depolariza-tion and repolarization waves occur, at least in part, in opposite directions in the heart.7 In LBBB the
depolar-ization and repolarization sequences are altered, so that thetwowaveshave almostparallel directions.7 Moreover,
thedelayedleftbundlebranchconductionassociatedwith changesinthedepolarizationandrepolarizationsequence prevents the occurrenceof therefractory periodof most myocytes simultaneously and allows the occurrence of a delayeddepolarizationoftheleftventriclelateralwalland earlyrepolarizationoftherightventricleatthesametime.7
On the ECG, these changes are shown by the QRS com-plexandT-wavediscordance(T-wavetypicallyhasopposite polaritytothatofthelastQRS deflection)andby ST seg-mentelevationordepression.7Thesesecondarychangesin
repolarization caused by the LBBB may be confused with orobscureprimarychangesinrepolarization,suchasacute myocardialinfarction(AMI).5,7
The blockade is usually permanent, but it may occur transiently when reverts to normal conduction----even temporarily----orintermittentlywhenboththeblockadeand normalconductionareobservedonthesameECGtrace.1,3
A large proportion of patients with intermittent block eventually develops a permanent block.5,11 The cause of
this intermittentblock maybe organicor functional. The exact mechanism of an intermittent blockade is unclear, but it appears to result from anatomicalor physiological disruptions in a conductive branch either by ventricular hypertrophy or dilation,3,9 or by functional or neurogenic
depression, with or without conductive tissue underlying lesions.3,9 The intermittent formwasalsoassociatedwith
somedrugs2,4,5andtachycardia.1
TheHR-dependentintermittentbranchblockisthemost commonly reported. It is relatedto a defect in intraven-tricular conduction, which occurs only when HR exceeds a certain critical value usually within the physiological
values.5,12 Increased HR and decreased RR interval may
causedownwardelectricalimpulsestofindoneofthe con-ductivebranchesstillintheirrefractoryperiodandgenerate theblockage.9ItpersistsuntilHRisslowerthanthat
criti-calonethatcausedtheblockage;theRRintervalatwhich the block occursis 80---170ms shorter than that in which conductionreturnstonormal(zoneoflinking).5Atransition
fromnormalconductiontobranchblockissuddenandmay occurevenwithHRvariationsofonly1or2bpm,5,9andthe
criticalvaluedependsonHRvariationvelocity:rapid accel-erationscauseblockagewithlowerHR,rapiddecelerations causereversalwithhigherHR.5,9Electrophysiological
stud-ieshaveshownthatcellsfromtheconductivebranchesof patientswithHR-dependentLBBBhaveprolongedrefractory periods.5WithhigherHR,theirmembranepotentialdoesnot
decreasenormally, andthe hypopolarizationthey present providesadelayedelectricalimpulseconduction.5
Transient changes in cardiac conduction during the intraoperative periodare uncommon.1---4 There have been
rare reports of LBBB development or remission under anesthesia (general and locoregional), which have been associatedwithmyocardialischemia,hypertension, tachy-cardia, HR variations without tachycardia, and drugs (lidocaine,trimethaphan,lithium, andatropine).1,2,4,5,9 In
somecasesitwasnotpossibletoidentifythecauseof inter-mittentblockade.3
Acutepainleadstoatypicalneuroendocrineresponse, proportional to its intensity, mediated by the endocrine and sympathetic nervous systems. Its main cardiovascu-lareffectsaregeneralizedvasoconstrictionwithincreased peripheral vascular resistance and increased cardiac con-tractilityandfrequency.
Inthecasedescribedhere,thepatient,althoughwithout knownhistoryofcoronaryarterydisease,aorticvalvular dis-ease,orcardiomyopathyreferredasoneofherconditionsan arterialhypertensionwithseveralyearsofevolution.Given thesevereacuteabdominalpaincausedbythehollow vis-cera perforation presented by thepatient preoperatively, aswell asan immediatepostoperative pain initially diffi-cult to control, it is likely that the HR values measured, although within normal values, were above the baseline values.Intraoperatively,thesympathetictonereductionby theanalgesicdrugsandanesthetics decreasedtheHR val-ues,which remained between 65 and74bpm,possibly to a value similaror evenlower than the patient’s baseline value. In the semi-intensive care unit, the postoperative painwasalreadycontrolledandtheHRwasprobablyclose tothebaselinevalues.Thus,wehypothesizedthattheHR mayhave been intermittently abovethe patient’s critical HR(75bpm)andcapableoftriggeringaLBBBinaheartwith probablechangescausedbydiabetesandhypertension. Car-diacinvestigationshowednoacutepathologicalcondition.
We therefore consider a case of intermittent rate-dependentLBBBwithablockadepresentinthepreoperative andearlypostoperativeperiodsandintraoperativenormal conduction.
Although frequently associated withAMI, certain stud-iespointtoa benignnatureof thistypeof blockade,not associatedwithischemiaorchangesinventricularfunction.5
repolarizationgradientbetweennormalandabnormally per-fusedmyocardiumisthebasisforthediagnosisofAMI.7This
isan especially importantfact for patients undergeneral anesthesia, as theyare unableto discribe the character-istic symptoms of myocardial ischemia. The diagnosis of AMIinthiscontext,althoughchallenging,is possible. Cur-rently,themostaccurateandreliableelectrocardiographic signal for thediagnosis ofAMI in the presence of LBBBis ST-segmentelevation,whichrepresentsthesumofthe repo-larizationprimarychangesfrominfarctionandthechanges secondarytotheblockade.7In1996,Sgarbossa13describeda
validatedscoringsystemfortheelectrocardiographic diag-nosisofAMIinpatientswithLBBB.Diagnosis isconsidered positiveifthreepointsarereachedbasedonthefollowing threecriteria:ST-segmentelevation ofat least 1mm ina leadwithQRS complexandT-wave concordant(5 points); ST-segment depression of at least 1mm in lead V1, V2, or V3 (3 points); ST-segment elevation of at least 5mm in a lead with a QRS complex and T-wave discordant (2 points).13 In 2012,Smithetal.14 developedamodification
totheSgarbossacriteriabasedontheST-segmentdeviation ratio with discordant S-wave or R-wave amplitude. Sgar-bossasystemishighlypredictiveofAMIinthepresenceof LBBB.Themodifiedcriteriaappeartobeusefulfor diagno-sis;however,themanualcalculationofST/SorST/Ristime consuming.7
HR-dependent LBBB has also been confused with slow ventriculartachycardiaandinappropriatelytreated.1Thus,
the correct diagnosis of this particular change in car-diacconductionisofparticularimportance.Intraoperative maneuvers were described that, by triggering or inter-rupting the blockadethrough the HRalteration (valsalva, carotid massage, administrationof atropine, neostigmine orpropranolol),aidedthediagnosisofHR-dependentLBBB. However,provocativemaneuversshouldbeusedwith cau-tion in patients with cardiovascular, cerebrovascular, or atrioventricularnodedisease.
Althoughthedevelopmentorremissionofthisblockade underanesthesiaisuncommon,anesthesiologistsshouldbe alertedtothe possibilityofitsoccurrence. In additionto usingtheSgarbossacriteriaand/orthemaneuversdescribed above,itisadvisabletoperformaHoltermonitoringafter surgery.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.Tanus-SantosJE.Transientleftbundlebranchblockduring anes-thesia.RevMexAnest.1998;21:211---3.
2.TaglienteTM,JayagopalS.Transientleftbundlebranchblock followinglidocaine.AnesthAnalg.1989;69:545---7.
3.EdelmanJD,HurlbertBJ.Intermittentleftbundlebranchblock duringanesthesia.AnesthAnalg.1980;59:628---30.
4.AzarI,TurndorfH.Paroxysmalleftbundlebranchblockduring nitrousoxideanesthesiainapatientonlithiumcarbonate: a casereport.AnesthAnalg.1977;56:868---70.
5.DominoKB,LaMantiaKL,GeerRT,etal.Intraoperative diagno-sisofrate-dependentbundlebranchblock.CanAnaesthSocJ. 1984;31:302---6.
6.ChapmanJH.Intermittentleftbundlebranchblockinthe ath-leticheartsyndrome---autonomicinfluenceonintraventricular conduction.Chest.1977;71:776---9.
7.HerwegB,MarcusMB,BaroldSS.Diagnosisofmyocardial infarc-tionand ischemiainthesetting ofbundle branchblockand cardiacpacing.HerzschrElektrophys.2016;27:307---22.
8.BreithardtG,BreithardtO-A.Leftbundlebranchblock,an old-newentity.JCardiovascTransRes.2012;5:107---16.
9.MishraS, NasaP,Goyal GN, etal. Therate dependent bun-dlebranchblock---transitionfromleftbundlebranchblockto intraoperativenormalsinusrhythm---casereport.MiddleEast JAnesthesiol.2009;20:295---8.
10.Grady TA, Chiu AC, Snader CE, et al. Prognostic signifi-cance of exercise-induced left bundle branch block. JAMA. 1998;279:153---6.
11.AbbenR,RosenKM,DenesP.Intermittentleftbundlebranch block:anatomicsubstrateasreflectedintheelectrocardiogram duringnormalconduction.Circulation.1979;59:1040---3.
12.Chakrabarti D, Bhattacharjee A, Bhattacharyya A. Intermit-tentleftbundlebranchblock---adiagnosticdilemma.JIACM. 2013;14:278---9.
13.SgarbossaEB.Recentadvancesintheelectrocardiographic diag-nosisof myocardialinfarction:left bundle branchblockand pacing.PacingClinElectrophysiol.1996;19:1370---9.