REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
Official Publication of the Brazilian Society of Anesthesiologywww.sba.com.br
SCIENTIFIC
ARTICLE
A
randomized,
double
blind
comparison
of
pethidine
and
ketoprofen
as
adjuvants
for
lignocaine
in
intravenous
regional
anaesthesia
夽
,
夽夽
Sameer
N.
Desai
∗,
M.C.B.
Santhosh
DepartmentofAnaesthesiology,ShriDharmasthalaManjunatheshwaraMedicalCollege,Sattur,Dharwad,India
Received15May2012;accepted20March2013
Availableonline23October2013
KEYWORDS
Intravenousregional anaesthesia; Pethidine; Ketoprofen
Abstract
Backgroundandobjectives: Areviewofalltheadjunctsforintravenousregionalanaesthesia concludedthatthereisgoodevidencetorecommendNonSteroidalAnti-Inflammatoryagents andpethidineinthedoseof30mgdoseasadjunctstointravenousregionalanaesthesia.But there areno studies tocompare pethidine of 30mg dose toany ofthe NonSteroidal Anti-Inflammatoryagents.
Methods:Inaprospective,randomized,doubleblindstudy,45patientsweregivenintravenous regionalanaesthesiawitheitherlignocainealoneorlignocainewithpethidine30mgor ligno-cainewithketprofen100mg.Fentanylwasusedasrescueanalgesicduringsurgery.Forthefirst 6hofpostoperativeperiodanalgesiawasprovidedbyfentanylinjectionandbetween6and24h analgesiawasprovidedbydiclofenactablets.Visualanaloguescoresforpainandconsumption offentanylanddiclofenacwerecompared.
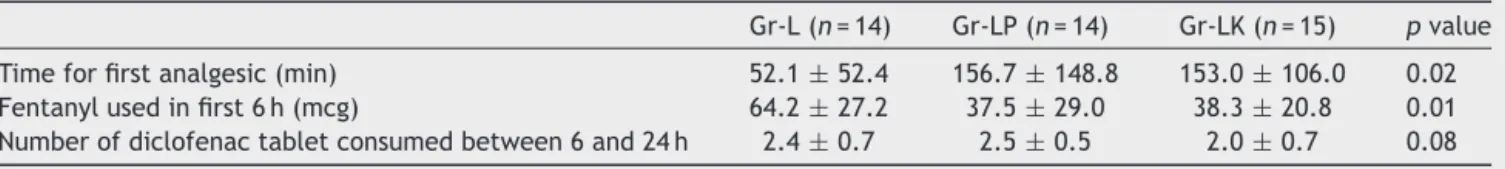
Results:Theblockwasinadequateforonecaseeachinlignocainegroupandpethidinegroup, so generalanaesthesiawas provided. Timefor the first doseoffentanyl required for post-operative analgesiawas significantlymore inpethidineandketoprofengroups compared to lignocainegroup(156.7±148.8and153.0±106.0vs.52.1±52.4minrespectively).Total fen-tanylconsumptioninfirst6hofpostoperativeperiodwaslessinpethidineandketoprofengroups compared to lignocaine group (37.5±29.0mcg, 38.3±20.8mcg vs. 64.2±27.2mcg respec-tively).Consumptionofdiclofenactabletswas2.4±0.7,2.5±0.5and2.0±0.7inthecontrol, pethidineandketoprofengrouprespectively,whichwasstatisticallynotsignificant.Sideeffects werenotsignificantlydifferentbetweenthegroups.
夽 ThisworkwasconductedintheDepartmentofAnesthesiologyandCriticalCare,AllIndiaInstituteofMedicalSciences,NewDelhi, India.
夽夽ThisarticlewaspresentedasposterinInternationalCongressonRegionalAnaesthesiaandPainMedicine,NewDelhi,February20---22, 2004.
∗Correspondingauthor.
E-mail:sameeranaes@gmail.com(S.N.Desai).
0104-0014/$–seefrontmatter©2013SociedadeBrasileiradeAnestesiologia.PublishedbyElsevierEditoraLtda.Allrightsreserved.
Conclusion:Both pethidine andketoprofenareequally effective inproviding postoperative analgesiaupto6h,withoutsignificantdifferenceinthesideeffectsandnoneoftheadjuncts providesignificantanalgesiaafter6h.
©2013SociedadeBrasileiradeAnestesiologia.PublishedbyElsevier EditoraLtda.Allrights reserved.
PALAVRAS-CHAVE
Anestesiaregional intravenosa; Petidina; Cetoprofeno
Estudocomparativo,randômicoeduplo-cegodepetidinaecetoprofenocomo adjuvantesdelidocaínaemanestesiaregionalintravenosa
Resumo
Justificativaeobjetivos: umarevisão de todosos adjuvantes para anestesiaregional intra-venosaconcluiuque háboasevidências para recomendar osagentes anti-inflamatórios não esteroidesepetidinaemdosede30mgcomoadjuvantesparaanestesiaregionalintravenosa. Porém, não há estudos que comparem petidina (30mg) com quaisquer dos agentes anti-inflamatóriosnãoesteroides.
Métodos: emumestudoprospectivo,randômicoeduplo-cego,45pacientesreceberam aneste-siaregionalintravenosacomapenaslidocaínaoulidocaínacompetidina(30mg)oulidocaína comcetoprofeno(100mg).Fentanilfoiusadocomoanalgésicoderesgateduranteacirurgia. Duranteasseisprimeirashorasdepós-operatório,analgesiafoifornecidaviainjec¸ãode fen-tanile,entreseise24horas,analgesiafoifornecidaviacomprimidosdediclofenaco.Osescores visuaisanalógicosparadoredoconsumodefentanilediclofenacoforamcomparados.
Resultados: o bloqueio foi inadequado para um caso tanto do grupo lidocaína quanto do grupo petidina; portanto, anestesia geral foi administrada. O tempo para a primeira dose necessáriadefentanilpara analgesiapós-operatória foisignificativamentemaiornosgrupos petidinaecetoprofenoemcomparac¸ãocomogrupolidocaína(156,7±148,8e153,0±106,0 vs.52,1±52,4minutos,respectivamente).Oconsumototaldefentanilnasprimeirasseishoras depós-operatóriofoimenornosgrupospetidinaecetoprofenoemcomparac¸ãocomogrupo lidocaína(37,5±29,0mcg,38,3±20,8mcgvs.64,2±27,2mcg,respectivamente).Oconsumo decomprimidosdediclofenacofoide2,4±0,7,2,5±0,5e2,0±0,7nogrupocontrole, petid-ina ecetoprofeno,respectivamente,oque não foiestatisticamentesignificante.Osefeitos colateraisnãoforamsignificativamentediferentesentreosgrupos.
Conclusão:tanto petidina quanto cetoprofeno são igualmenteeficazes para analgesia pós-operatória atéseis horas, sem diferenc¸a significante nos efeitos colaterais, e nenhum dos adjuvantesproporcionouanalgesiasignificativaapósseishoras.
©2013SociedadeBrasileiradeAnestesiologia.PublicadoporElsevierEditoraLtda.Todosos direitosreservados.
Introduction
Intravenousregional anaesthesia(IVRA) is safeand effec-tivewaytoprovideanaesthesiaforthe forearmandhand surgeries lastingup to 90min. Mainlimitations toits use aresignificant tourniquetpain during surgery and lack of postoperativeanalgesia.Toovercometheseproblemsmany ofadjuncts drugshave been used along withlocal anaes-theticagentsinIVRA.Asystemicreviewofalltheadjuncts usedinIVRA,byChoyceandPeng1concludedthatthereis
goodevidencetouseNonSteroidalAnti-Inflammatoryagents (NSAIDs), particularly ketorolac. Among the opioids, the reviewsuggestedthatonlythepethidineinadoseof30mg hassubstantialpostoperativebenefit,butattheexpenseof postdeflationsideeffects.KetoprofenisanNSAIDavailable inintravenousformulation,whichhasaprovenefficacyin providingpostoperativeanalgesiainsurgeriessuchas tonsil-lectomy,thyroidandnasalsurgeries.2---6Dexketoprofenhas
beenshowntoprovidepostoperativeanalgesiawhengiven in IVRA, comparedto givingit intravenously.7 Aimof this
study is to compare ketoprofen with pethidine 30mg as adjuncttolignocaineinIVRA.
Methods
After taking approval from the ethics committee of the institute and informed consent, 45 ASA grade I and II patients posted for elective forearm and hand surgeries wereselectedforaprospective,randomized,doubleblind study.All thepatients werepreoperatively evaluatedand visual analogue score for pain was explained to them. The patientswerepremeditatedwithintravenous midazo-lam1mg,10minbeforetheprocedure.Routinemonitoring includedECG,NIBP,andSpO2.A20Gcannulawasinserted
Table1 Demographicdata.
Gr-L(n=14) Gr-LP(n=14) Gr-LK(n=15) pvalue Age(yr) 36.8±5.6 33.4±14.1 31.9±16.6 0.68 SexM/Fratio 12/3 11/4 12/3 0.87 Weight(kg) 63.0±8.1 64.7±7.8 63.4±8.5 0.83 Tourniquettime(min) 64.6±17.3 67.8±16.6 76.1±13.5 0.14 Surgicalduration(min) 47.8±15.7 53.0±14.9 56.9±13.9 0.14
Isolation of the limb from systemic circulation was confirmedbyobservingthearmfortheabsenceofdistended veinsandconfirmingabsenceofradialpulse.The Esmarch bandage was removed and 40mL of IVRA solution was injectedthroughthevenouscannulaslowlyoveraperiodof 90s.
The patients were randomly divided intothree groups of 15 each, by closed envelopetechnique. They received either40mLof0.5%lignocaine(Gr-L)or40mLof0.5% lig-nocainealongwithpethidine30mg(Gr-LP)or40mLof0.5% lignocainealongwithketoprofen100mg(Gr-LK).
Pulserate,bloodpressure,andSpO2wererecordedevery
5min. Intra operative tourniquetpain wasassessed every 15minusingvisualanaloguescaleof0---10.Duringintra oper-ativeperiod,fortourniquetpain(VAS>3)25mcgoffentanyl wasgiven intravenously. Afterdeflation of cuff, painwas assessedusingVASscaleat0,15,30,60,120,180,240and 360min.Forearlypostoperativepainupto6h,forVAS>3, bolusdoseoffentanyl25mcgwasgivenintravenously.Time forfirstanalgesicconsumptionandtotalnumberoffentanyl bolusesconsumedwerenoted.
After 6h if the patient had pain, patient was asked to take oral tablet of diclofenac 50mg. The patient was asked to take tablet of diclofenac 50mg every 8th hour, if pain persisted. Total numbers of tablets taken in 24h were noted by telephonic interview. Postopera-tive nausea and vomiting, pruritis, tinnitus and dizziness and respiratory depression (respiratory rate <10/min or SpO2<90%)werenoted.Sedationwasnotedat0,30,60min
after the deflation of tourniquet using a numerical scale (1=completelyawake,2=awakebutdrowsy,3=asleepbut responsivetoverbalcommands,4=asleepbutresponsiveto tactilestimulus,5=asleepandnotresponsivetoany stimu-lus).
Data wereanalyzed using SPSS11.0 statistical analysis software.Ordinal data suchasdemographic data, tourni-quet time, surgical duration, haemodynamic parameters andnumberofdiclofenactabletsconsumedwerecompared usingone-wayANOVA.Ifthedifferencewasstatistically sig-nificant,Schiff’sposthocanalysiswasperformed.Number of patients needing fentanyl during intraoperative period and in the first 6h of postoperative period and the side effects were compared using Chi-square test. Continuous datalikeintraoperative andpostoperativepainscoresand sedation scores within the groups were compared with Friedman rank test. The pain scores and sedation scores between the groups were compared using Kruskal---Wallis test. p value of <0.05 was considered statistically significant.
15 30
Time
Gr - L Gr - LP Gr - LK
VA
S
5
4
3
2
1
0
45 60
Figure1 IntraoperativeVASscores.
Results
Onepatientinthecontrolgroup(Gr-L)andoneinthe pethi-dinegroup(Gr-LP)hadpatchyblockandweregivengeneral anaesthesia.There werenodifferences amongthe groups indemographicvariable,tourniquettimeandsurgical dura-tion(Table1).Therewasnodifferencebetweengroupsfor haemodynamicsparameters (heart rate, systolic and dia-stolicbloodpressure).
Within each group VAS scores increased progressively from15 to90min (Fig.1).In ordertofindout,whenthe tourniquet pain became significant, Friedman test (rank test)was(Table2)withineachofthesegroups.Tourniquet painincreasedsignificantlybetween30and45mininallthe groups.TheVASscoreswerecomparablebetweenthegroups duringsurgery.Fentanylrequirementfortreatmentofintra operativetourniquetpainwasnotsignificant betweenthe groups.
PostoperativeVASscoreswerecomparablebetweenthe groups. Time for the first dose of fentanyl consumption wassignificantlydelayedingroupsLPandLKcomparedto
Table2 Tourniquetpainwithinthegroup.
Gr-LMeanrank Gr-LPMeanrank Gr-LKMeanrank VAS15 1.6 1.7 1.9
Groups
Gr - L Gr - LP Gr - LK
T
ime (min)
160 140 120 100 80 60 40 20 0
Figure2 Timeforthefirstanalgesicconsumption.
70
60
50
40
30
20
10
0
Gr - L Gr - LP
Groups
Fentanyl (
µ
g)
Gr - LK
Figure3 Fentanyl requirementinfirst 6hofpostoperative period.
groupL(156.7±148.8and153.0±106.0vs.52.1±52.4min respectively)(Fig.2).Totalfentanylconsumptioninfirst6h ofpostoperativeperiod(Fig.3)waslesserinGr-LPand Gr-LKcomparedtoGrL(37.5±29.0mcg,38.3±20.8mcgvs. 64.2±27.2mcgrespectively)(Table3).
Numberofdiclofenactabletsconsumedbetween6and 24h was not significantly different between the groups
(2.4±0.7,2.5±0.5,2.0±0.7inGr-L,Gr-LP,Gr-LK respec-tively).
Onepatientinthecontrolgroup,fourpatientsin pethi-dinegroupandtwopatientsinketoprofenhadtinnitusand dizziness.Onlyonepatientinpethidinehadpostoperative nausea and vomiting and none of patients in control or ketoprofen had PONV. Two patients in ketoprofen group, butnone inpethidine orcontrol grouphadpruritus.None ofthesesideeffectswerestatisticallysignificant between the groups. None of the patients in any group had sig-nificant respiratory depression. Sedation scores were not significantlydifferentbetweenthegroups (meanscores of 1.2±0.1,1.1±0.1,1.4±0.1forgroupsL,LPandLK respec-tively)(Table4).
Discussion
We found that theaddition ofpethidine or ketoprofen as adjunctsinIVRAprovidessignificantlybetterpostoperative analgesiainthefirst6h.Howevertheirefficacy postopera-tiveanalgesiaislimitedbeyond6h.Additionofeitherofthe adjunctsdoes notincreasethetourniquettolerance when comparedtothecontrolgroup.
At the site of surgical trauma there will be release of inflammatory mediators such as histamine, serotonin, bradykinins andmetabolites of cycloxygenase and lipoox-igenase pathways.8 NSAIDs inhibit the production of
prostaglandins from arachidonic acid in the phospholipid membrane.9 Pretreatment of the extremity with NSAIDs
mightbeexpectedtointerferewiththeinitiationofpain. By preventing the synthesis of mediators prior to sur-gical trauma, NSAIDs might minimize the activation of or sensitization of peripheral nociceptors. Although the concept of pre-emptive analgesia is controversial, evi-dence from the animal studies supports the theory that breakingthe linkbetweensurgical traumaandprimaryor secondary hyperalgesia reduce both early and late post-operative pain.10 Ketoprofenis aNSAID agentavailable in
intravenous preparation. It has proven efficacy in provid-ing postoperative analgesia in tonsillectomy, thyroid and
Table3 Timeanddosesofanalgesicsconsumed.
Gr-L(n=14) Gr-LP(n=14) Gr-LK(n=15) pvalue Timeforfirstanalgesic(min) 52.1±52.4 156.7±148.8 153.0±106.0 0.02 Fentanylusedinfirst6h(mcg) 64.2±27.2 37.5±29.0 38.3±20.8 0.01 Numberofdiclofenactabletconsumedbetween6and24h 2.4±0.7 2.5±0.5 2.0±0.7 0.08
Table4 Sideeffectsprofile.
Gr-L(n=14) Gr-LP(n=14) Gr-LK(n=15) pvalue Tinnitus,dizziness 1 4 2 0.23 Postoperativenauseaandvomiting 0 1 0 0.31
Pruritus 0 0 2 0.15
nasal surgeries.2---6 The NSAIDs have already been shown
to be of definitive advantage when used as adjuncts in IVRA. NSAIDs used in previous studies are ketorolac and tenoxicam.11Lornaxicamwhenusedasadjuncttolignocaine
providedbetteranalgesiacomparedtothecontrol.12
Simi-larlydexketoprofenasadditivetolignocainehasbeenshown toprovide goodpostoperative analgesiacomparedto giv-ingthesamedrugintravenouslyorwhencomparedtothe placebo.7
Peripheralactionofopioidscouldbemediatedbyeither peripheral opioid receptorsor by local anaestheticaction of their own.13 Many opioids (morphine, pethidine,
fen-tanyl,tramadol,sufentanilandalfentanil)havebeenused asadjuncts inIVRA previously. Among theseopioids, only pethidine inthedose above30mghas substantial postop-erativebenefits but at the expenseof post deflation side effects.1
Therearenostudiestocomparepethidineof30mgdose toanyofNSAIDs.Sotheaimofourstudywastocompare pethidineinadoseof30mgwithaNSAID,ketoprofenwith respecttoefficacyandsideeffects.
Previous studies have suggested 30mg as the optimal dose ofpethidineasan adjunctsinIVRA.14 Optimumdose
ofketorolacforuseasadjunctsinIVRAwasdeterminedas twenty milligrams.11 Sincetwenty milligrams of ketorolac
is equipotentto100mgof ketoprofen,we used100mgof ketoprofeninourstudy.
In our study therewas nosignificant difference in the intraoperativefentanylconsumptionandintraoperativeVAS scores for the tourniquetpain between the groups. In all thethreegroupsthetourniquetpainincreasedsignificantly between 30and 45min period.This is in correlation with the other studies that suggest under regionalanaesthesia tourniquetpainusuallyappearsabout45minafterinflation and becomesmore intense withtime.15 Thusboth of the
adjunctsusedinthispresent studydonotdelayorreduce theseverityofintraoperativetourniquetpaincomparedto thecontrol.
The analgesicconsumptionfor treatmentofearly post-operative pain was significantly less in pethidine and ketoprofen group comparedto control. The time for first analgesicrequirementwasalsodelayedwhenpethidineand ketoprofen were usedas adjunctswhen comparedto the control.Thissignifiesthatpethidineandketoprofenprovide significantlybetterpostoperativeanalgesiainthefirst6h. Bothpethidineandketoprofenareequallyefficaciousin pro-viding postoperative analgesia, when used asadjuncts to lignocaineinIVRA.
Analgesic consumption was not significantly different between 6 and 24h period after the surgery. Therefore additionof pethidine or ketoprofen is unlikely toprovide significantanalgesiabeyond6h.
Inourstudytherewasnosignificantdifferenceinthe inci-denceofsideeffectsbetweenthethreegroups.Theresults arein contrastto high incidenceof side effectsin pethi-dinegroupinScott Reuben’sstudy.14 Twoofthe forty-five
patients had successful block in our study. Thus the suc-cessratewas95.56%.Thisiscloseto96---100%successrate describedbyotherstudies.16---18
Thus we conclude that addition of pethidine or keto-profen as adjuncts in IVRA provides significantly better
postoperative analgesia in the first 6h. However their efficacy postoperative analgesia is limited beyond 6h. Addition of either of the adjuncts does not increase the tourniquet tolerance when compared to the con-trol group. Neither of these adjuncts increases the incidence of side effects compared to the control group.
Werecommendtheuseofpethidine30mgorketoprofen 100mgassafeandeffectiveadjunctsinIVRA.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.ChoyceA,PengP.Asystemicreviewofadjunctsforintravenous regional anaesthesiafor surgical procedures.CanJAnaesth. 2002;49:32---45.
2.BastoER,WaintropC,MoureyFD,LandruJP,EurinBJ,Jacob LP.Intravenousketoprofeninthyroidandparathyroidsurgery. AnesthAnalg.2001;92:1052---7.
3.TuomilehtoH,KokkiH,TuovinenK.Comparisonofintravenous and oralketoprofenfor postoperativepainafter adenoidec-tomyinchildren.BrJAnaesth.2000;85:224---7.
4.ElhakimM.Comparisonofintravenousketoprofenwith pethi-dineforpostoperativepainrelieffollowingnasalsurgery.Acta AnaesthesiolScand.1991;35:279---82.
5.Subramaniam R, Ghai B, Khetarpal M, Subramanyam MS. A comparison of intravenous ketoprofen versus pethidine on peri-operative analgesia and post-operative nausea and vomiting in paediatricvitreoretinal surgery.J PostgradMed. 2003;49:123---6.
6.Priya V,Divatia JV, Sareen R, Upadhye S. Efficacy of intra-venousketoprofenforpre-emptiveanalgesia.JPostgradMed. 2002;48:109---12.
7.YurtluS,HanciV,KargiE,ErdoganG,KosalBG,GulS,etal. The analgesic effect of dexketoprofen when added to lig-nocainefor intravenous regional anaesthesia: a prospective, randomizedplacebocontrolledstudy.JIntMedRes.2011;39: 1923---31.
8.WoolfCJ.Recentadvancesinpathophysiologyofacutepain.Br JAnaesth.1989;63:139---46.
9.FoedtWeserJ.Nonsteroidalanti-inflammatorydrugs.NewEng JMed.1980;302:1179---85.
10.Woolf CJ, Chang MS. Preemptive analgesia --- treating post-operative pain by preventing the establishment of central sensitization.AnesthAnalg.1993;77:362---79.
11.Steinberg RB, Reuben SS, Gardener G. The dose---response relationship of ketorolac as a component of intravenous regional anesthesia with lignocaine. Anesth Analg. 1998;86: 791---3.
12.Sen1 S, Ugur B, Aydın ON, Ogurlu M, Gezer E, Savk O. The analgesic effect of lornoxicam when added to lido-caine for intravenous regional anaesthesia. Br J Anaesth. 2006;97:408---13.
13.Stein C, Yassouridis A. Peripheral morphine analgesia. Pain. 1997;71:119---21[editorial].
15.Terse T, Horlocker, Wedel DJ. Anaesthesia for orthopaedic surgery.In:BarashPG,CullenBF,StoeltingRK,editors. Clini-calanaesthesia.Philadelphia:LippincottWilliamsandWilkins; 2001.p.1114.
16.Brill S, Middleton W, Brill G, Fisher A. Bier’s block; 100 years old and still going strong! Acta Anaesthesiol Scand. 2004;48:117---22.
17.Brown EM, McGriff JT, Malinowski RW. Intravenous regional anaesthesia(Bier’sblock):reviewof20yearsexperience.Can JAnaesth.1989;36:307---10.