REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
PublicaçãoOficialdaSociedadeBrasileiradeAnestesiologiawww.sba.com.br
SCIENTIFIC
ARTICLE
Nondepolarizing
muscle
relaxant
improves
direct
laryngoscopy
view
with
no
effect
on
face
mask
ventilation
Marwan
S.
Rizk
a,
Salah
M.
Zeineldine
b,
Mohamad
F.
El-Khatib
a,
Vanda
G.
Yazbeck-Karam
c,
Sophie
D.
Ayoub
a,
Pierre
K.
Bou-Khalil
b,
Elie
Abi-Nader
c,
Marc
M.
Ghabach
d,
Chakib
M.
Ayoub
a,∗aAmericanUniversityofBeirut---MedicalCenter,DepartmentofAnesthesiology&PainManagement,Beirut,Lebanon bAmericanUniversityofBeirut---MedicalCenter,DepartmentofPulmonaryandCriticalCare,Beirut,Lebanon cLebaneseAmericanUniversity,DepartmentofAnesthesiology,Beirut,Lebanon
dAmericanUniversityofBeirut,DepartmentofBiology,Beirut,Lebanon
Received14March2016;accepted28July2016 Availableonline17August2016
KEYWORDS Nondepolarizing musclerelaxants; Laryngoscopyview; Facemaskventilation
Abstract
Background: Difficultorimpossiblefacemaskventilationcomplicatedwithdifficulttracheal intubationduringanesthesiainductionoccursin0.4%ofadultanesthesiacases,possiblyleading tolife-threateningcomplications.Becauseofsuchcatastrophes,musclerelaxantshavebeen recommendedtobeadministeredafterconfirmingadequatefacemaskventilationwithouta solidscientificvalidationofthisprincipal.
Methods:In thisobservationalstudy,theeaseofventilationandthescoresofdirect laryn-goscopyviewsbeforeandafteradministrationofcisatracuriumwereassessedinninetyyoung healthyadults,withoutanestheticrisksandwithoutforeseendifficultintubationandwhowere scheduledforgeneralelectivesurgeries.
Results:Beforemusclerelaxation,43patients(48%)wereCormackGradeI,whiletheremaining 47 patients (52%)were either CormackGrade II(28patients, 31%)orCormackGrade II(19 patients,21%).Followingmusclerelaxationwithcisatracurium,thenumberofpatientswith CormackGradeIsignificantlyincreasedfrom43patients(48%)to65patients(72%)(p=0.0013). Only1patientoutof19patients (5%)improvedhisCormackgradefromGradeIIItoGradeI while16out19patients(84%)improvedtheirCormackgradefromGradeIIItoGradeIIafter theuseofcisatracurium.Thequalityoffacemaskventilationdidnotdifferwithandwithout musclerelaxantsinallpatients.
∗Correspondingauthor.
E-mail:ca04@aub.edu.lb(C.M.Ayoub).
http://dx.doi.org/10.1016/j.bjane.2016.07.005
Conclusion:Theuseofcisatracuriuminhealthyyoungadultsundergoinggeneralelective sur-gerieswithnoanticipateddifficultendotrachealintubationhadnoeffectonthequalityofface maskventilationdespiteresultinginaquantifiableimprovementinthelaryngealview. ©2016PublishedbyElsevierEditoraLtda.onbehalfofSociedadeBrasileiradeAnestesiologia. Thisisanopenaccess articleundertheCCBY-NC-NDlicense(http://creativecommons.org/ licenses/by-nc-nd/4.0/).
PALAVRAS-CHAVE Relaxantes
muscularesnão despolarizantes; Visibilidadeem laringoscopia; Ventilac¸ãovia máscarafacial
Relaxantesmuscularesnãodespolarizantesmelhoramavisibilidadeemlaringoscopia
diretasemefeitosobreaventilac¸ãoviamáscarafacial
Resumo
Justificativa:Aventilac¸ãodifícilouimpossívelviamáscarafacialcomplicadapelaintubac¸ão traqueal difícildurante ainduc¸ãoda anestesia ocorreem 0,4%dos casos de anestesia em adultos,possivelmentelevandoacomplicac¸õesfatais.Devidoataiscatástrofes, recomendou-sequeaadministrac¸ãoderelaxantesmuscularessejafeitaapósaconfirmac¸ãodeventilac¸ão adequadaviamáscarafacial,semumavalidac¸ãocientíficasólidadessaconduta.
Métodos: Nesteestudoobservacional,afacilidadedeventilac¸ãoeosescoresdevisibilidade emlaringoscopiadiretaanteseapósaadministrac¸ãodecisatracúrioforamavaliadosem 90 adultosjovensesaudáveis,semriscosanestésicosesemintubac¸ãodifícilprevista,agendados paracirurgiaseletivasgerais.
Resultados: Antesdorelaxamentomuscular,43pacientes(48%)eramCormackGrauI,enquanto os 47 pacientes (52%) restantes eram ouCormack Grau II (28 pacientes, 31%)ou Cormack Grade III(19pacientes, 21%).Apóso relaxamentomuscularcomcisatracúrio,onúmero de pacientescom Cormack GrauI aumentousignificativamente de43 (48%) para 65 pacientes (72%)(p=0,0013).Apenasumpaciente(5%)dos19melhorousuaclassificac¸ãodeCormackdo GrauIIIparaoGrauI,enquanto16dos19pacientes(84%)melhoraramsuasclassificac¸õesde CormackdoGrauIIIparaograuIIapósousodecisatracúrio.Aqualidadedaventilac¸ãovia máscarafacialnãodiferiucomousemrelaxantesmuscularesemtodosospacientes.
Conclusão:Ousodecisatracúrioemadultosjovenssaudáveissubmetidosacirurgiaseletivas geraissemintubac¸ãotraquealdifícilprevistanãoteveefeitosobreaqualidadedaventilac¸ão viamáscarafacial,mesmoresultandoemmelhoraquantificáveldavisibilidadedalaringe. ©2016PublicadoporElsevierEditoraLtda.emnomedeSociedadeBrasileiradeAnestesiologia. Este ´e um artigo Open Access sobuma licenc¸a CC BY-NC-ND(http://creativecommons.org/ licenses/by-nc-nd/4.0/).
Introduction
AdequateFacemaskVentilation(FMV)andtracheal intuba-tionarethemostfundamentalandimportantskillsforsafe airwaymanagement during anesthesia induction. Difficult or impossible FMV combined with difficult tracheal intu-bationduringanesthesiainductionoccursinapproximately 0.4%ofadult anesthesiacases,leadingtolife-threatening complications.1 Because of possible development of such catastrophes,administrationofmusclerelaxantshasbeen recommendedafterconfirmingadequateFMV.2,3
Recently,Ikedaetal.showedthatnondepolarizing mus-clerelaxantsdidnotimpactFMV inanesthetizedpatients with normal upper airway anatomy.4 Furthermore, addi-tionalevidencesuggestthatmusclerelaxantsnotonlydid not influence FMV in anesthetized subjects with normal upper airway anatomy, but nevertheless it improved the intubatingconditions.5,6
The aim ofthis studyis tocompare the easeof venti-lationaswell astogradethe laryngoscopicviewassessed bytheCormack-Lehane7,8scoreinthesamepatientsbefore andafter administrationof nondepolarizingmuscle relax-antsduringgeneralelectivesurgeries.
Materials
and
methods
Table1 Criteriafortheassessmentofthequalityofface maskventilation.
Easy
SpO2>97%
Onehandtechnique Goodchestrise
Difficult
Importantgasflowleakbythefacemask
↑gasflowabove15L/minanduseofO2flushvalve>2
times
Noperceptiblechestmovement 2handedmaskventilationtechnique Changeofoperatorrequired
Impossible
NeedanalternativetoFMVinemergencyconditionto maintainSpO2>90%
bodies in the upper airway were not enrolled in the
study.
During the preoperative visit, a staff anesthesiologist notedtheage,sex,weight,height,andMallampati
classifi-cation as modified by Samsoon and Young and performed
with the patient in the sitting position with the head in fullextension,tongueoutandwithphonation.9The thyro-mental distance wasmeasured with thepatient in sitting position and head in extension. The mouth opening was measured as the interincisor distance.10 In addition, the anesthesiologist’ssubjectiveassessmentofanticipated Dif-ficultMaskVentilation(DMV)wasalsonoted.Thissubjective assessmentincluded presenceor absenceof macroglossia, recedingmandible,lackofteeth,thepresenceofbeardand ifthepatientisasnorerornot.11
On the day of surgery and upon arrival to the oper-ating room, all patients were placed in the ‘‘sniffing position’’ with their head placed on a pillow, connected to standard monitoring devices and breathed 100% oxy-genuntiltheend-tidaloxygenconcentrationreached 90%. Values of noninvasive arterial blood pressure,heart rate, and oxyhemoglobin saturation were initially obtained as baseline and then measured every 3 minutes throughout inductionofanesthesia.Anesthesiawasinducedwith mida-zolam30mcg/kg−1,1---2mcg/kg−1offentanylintravenously
injected in 60s, followed by 2mg/kg−1 of propofol
intra-venouslyinjectedwithin30sandthelungsweremanually ventilatedthroughafacemaskusing2%sevofluranein oxy-gen. Following induction of anesthesia, FMV was assessed using the mask ventilation scale adapted from Langeron etal.as‘‘Easy’’,‘‘Difficult’’or‘‘Impossible’’(Table1).11 At least on itemof the respective listshould be encoun-teredtoclassifymaskventilationas‘‘Easy’’or‘‘Difficult’’. Afterapproximately4min,anindependentanesthesiologist, notinvolvedinthestudy,performedaninitialdirect laryn-goscopyusingaclassicmetalMacintosh(HeineOptotechnik GmbH & Co. KG, Herrsching, Germany) blade III, with-outattemptsofintubation.Laryngoscopicviewwasscored according tothe Cormack& Lehane (C&L)grading system where Grade I indicates that most of the glottis is seen and Grade 4 indicates that neither epiglottis nor glottis canbeseen.Afterwithdrawaloftheblade,cisatracurium
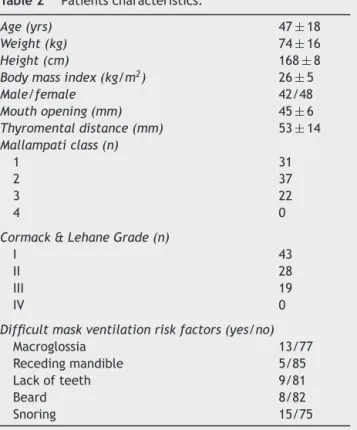
Table2 Patientscharacteristics.
Age(yrs) 47±18
Weight(kg) 74±16
Height(cm) 168±8
Bodymassindex(kg/m2) 26±5
Male/female 42/48
Mouthopening(mm) 45±6
Thyromentaldistance(mm) 53±14
Mallampaticlass(n)
1 31
2 37
3 22
4 0
Cormack&LehaneGrade(n)
I 43
II 28
III 19
IV 0
Difficultmaskventilationriskfactors(yes/no)
Macroglossia 13/77
Recedingmandible 5/85
Lackofteeth 9/81
Beard 8/82
Snoring 15/75
0.15mg/kgwasadministered.Followingconfirmationofan adequate neuromuscular blockade (train-of-four monitor-ing),a second independent anesthesiologist wascalled in toventilate the patientusing the sameface mask for an additional4minafterwhichFMVwasagainassessed.11Then the glottis was visualized and again scored according to C&Lgradingsystem.Finally,theanesthesiamanagingteam assignedtothepatientperformedtheintubationusingthe same metal Macintosh blade used in the previous airway assessments.Allanesthesiologistsinvolvedinthestudywere seniorstaffandwellexperiencedanesthesiologists.
Thequalityoffacemaskventilationaswellasthe grad-ingofthelaryngoscopicviewwereanalyzedandcompared withthechi-squaredtest.Statistical significancewas con-sideredatp<0.05.Basedonourexperienceandpreviously publisheddata, the percentage of patients withCormack II,III,orIVisabout50%.12ConsideringaTypeIerrorof5%, TypeIIerrorof10%,astatisticalsignificancelevelof5%,and areductioninthepercentageCormackII,III,andIVgrade from50%to35%, apower analysisindicated thatat least 85patientswillbe needed.Ourintentionis toinclude90 patientsinthestudy.
Results
43
21
7
2 1
16
Grade 2 (n=7) Grade 1
(n=43)
Grade 1 (n=65)
Grade 2 (n=28)
Grade 3 (n=19)
Grade 3 (n=2)
Before muscle relaxant After muscle relaxant
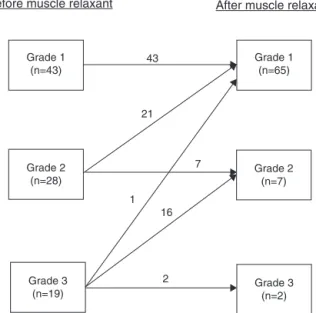
Figure1 ChangesinCormack&Lehanegradesofthe laryn-gealviewaftertheadministrationofnon-depolarizingmuscle relaxant.
GradeIsignificantlyincreasedfrom43patients(48%)to65 patients(72%)(p=0.0013)(Fig.1).Almostallofthisincrease inthenumberof patientswithCormackGradeIafterthe useofcisatracuriumresultedfromimprovingtheCormack gradein21patientsoutof28patients(75%)fromCormack GradeIItoGradeI.Only1outof19patients(5%)improved theCormackgradefromGradeIIItoGradeIaftertheuse ofcisatracurium.Furthermore,16patients(84%)improved their Cormack grade from Grade III to grade II while the remaining 2 patients maintained their Cormack Grade III (Fig.1).
Therewerenosignificantchangesinthequalityofmask ventilationfor patientswithCormackGradeIbefore(93% easy; 7% difficult; 0% impossible) compared toafter (98% easy;2% difficult;0% impossible)theuse ofcisatracurium (p=0.299).Similarly,nostatisticallysignificantdifferences wereobservedinthequalityofmaskventilationforpatients withCormackGradeIIorIIIbefore(68%easy;32%difficult; 0%impossible)comparedtoafter(60%easy; 40%difficult; 0%impossible)theuseofcisatracurium(p=0.605).
Discussion
In the current study, we showed that the use of Nonde-polarizingMuscleRelaxant(NDMR) didnotaffecttheease of face mask ventilation; however, there was a quantifi-able improvement in the laryngeal view. In fact, the use of nondepolarizing muscle relaxant resulted in a 1 grade improvementofthelaryngealviewinasignificantnumber ofpatientswhowereinitiallyscoredasaCormack&Lehane GradeIIandIIIpriortotheuseoftherelaxant.
The effect of administration of NDMR on the ease of maskventilationiscontroversial.Fullneuromuscular block-ade might facilitate mask ventilation by increasing chest wallcomplianceorbyreducingupperairwaytone13; alter-natively, itcould make mask ventilation moredifficult by inducing upper airway collapse.14,15 In accordance with
Ikeda et al., our data showed that FMV was not signifi-cantly affectedwiththe use ofNDMR.4 We observed only a minimal and non-significant increase in the percentage of patients with C&L Grade I whowere easy to ventilate before(93%ofpatients)andafter(98%ofpatients) admin-istrationofNDMR.Furthermore,patientswithC&LGradesII andIIIexhibitedastatisticallynon-significanttrendtoward a change inthe qualityofFMV before(68% easy,32% dif-ficult)andafter(60%easy,40%difficult)administrationof NDMR.Thenon-significantincreaseinthepercentageof dif-ficultFMVinpatientswithC&LGradesIIandIIIbefore(32%) andafter(40%)NDMRcouldbeattributedtotherelaxation oftheoropharyngealmusclesandsubsequentobstructionof thesubmandibulartissues,inan alreadygroupofpatients predisposed(i.e.,C&LIIandIII)todifficultFMV.Itisworth mentioningthatimpossibleFMVwasnotencounteredinour patientpopulationbeforeandafteradministrationofNDMR similartopreviousstudies.3,15,16
SimilartopreviousfindingsreportedbyBaillardetal.,our current studyconfirmsthattheuseof NDMRmayimprove theintubationconditionssecondarytotheimprovementin the Cormack & Lehane scoring of the laryngeal view fol-lowing the administrationof NDMR.17 Furthermore, other studies alsoconfirmed improvementin thelaryngeal view and intubation conditions following the administration of NDMR.18---20 However, none of these studies provided nei-ther quantitative changes in the scoring of the laryngeal view, norplausiblemechanismsfor thereported improve-ments.OurstudyclearlyshowsthattheuseofNDMRprior to intubation improved the C&L Grade by 1 grade in 75% of patients with Grade II and 84% of patients with Grade III. Of clinicalinterest, in ourstudy,none of the patients worsened their laryngeal viewfollowing theuse of NDMR (Fig. 1). We postulate that the improvement in the C&L gradeismainlyduetotwoseparatemechanisms.First,the use of NDMR will result in the loss of muscle contraction and a subsequent increase in the complianceof the sub-mandibulartissues.Thesetissueswillbeeasiercompressed intotheavailable submandibularspace,andthelaryngeal exposurewillbecomeadequateandeasytomanipulateby the laryngoscopistwithminimalexerted force andtorque efforts.21,22 Second, withtheuse of NDMR,the relaxation of the masticatory muscles responsible for approximately thefirst25mmofthemouthopeningwillcontributetothe improvementoftheretropalatalandvelopharyngealairway that isconsidered essential part ofthe effective dynamic phaseofdirectlaryngoscopy.21 However,itseemsthatthe effects of NDMR on the laryngeal views arenot dramatic asevidencedbythefactthatinthecurrentstudy,onlyone patient(5%)whowasinitiallyC&LGradeIIIhadgreaterthan 1gradechangeintheC&Lscore(Fig.1).
Few limitations related toour study need to be men-tioned. First, our study was performed on healthy and relativelyyoung patientswithnormalairways andwithno known risk factors for difficult ventilation or intubation undergoing elective surgical procedures. Accordingly, our results may not be generalized toan older population or toapopulationwithknownhistoryofdifficultairwaywhere awakeintubationisindicated.
however we strongly believe that having the patient as his/herowncontrolwillsignificantlyreducepotential con-founding factorsparticularlythe anatomicalfeatures that couldhave influencedthechangesseenor notseen inthe easeofventilationaswellasthescoringofthedirect laryn-goscopy view from before to after administration of the nondepolarizingmusclerelaxant.Assessingtheeaseof ven-tilationandtheCormackandLehanegradebeforeandafter administration of the nondepolarizing muscle relaxant in thesame patientis morehelpful in identifyingand quan-tifyingthe changesseen asaresult ofthe administration ofNDMR.
Conclusion
Inconclusion,ourstudyconfirmsthatNDMRhavenoeffect ontheeaseoffacemaskventilationdespiteaquantifiable improvementinthelaryngealview.Ingeneral, nondepolar-izingmusclerelaxantscanimprovethelaryngealviewby1 gradeaspertheC&Lclassification.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.KheterpalS,HanR,TremperKK,etal.Incidenceand predic-torsofdifficultandimpossiblemaskventilation.Anesthesiology. 2006;105:885---91.
2.Calder I, Yentis SM. Could ‘safe practice’ be compromising safepractice? Shouldanaesthetistshavetodemonstratethat facemaskventilationispossiblebeforegivinganeuromuscular blocker?Anaesthesia.2008;63:113---5.
3.PanditJJ.Checkingtheabilitytomaskventilatebefore admin-isteringlong-actingneuromuscularblockingdrugs.Anaesthesia. 2011;66:520---2.
4.IkedaA,IsonoS,SatoY,etal.Effectsofmusclerelaxantson maskventilation in anesthetized persons withnormal upper airwayanatomy.Anesthesiology.2012;117:487---93.
5.GoodwinMW,PanditJJ,HamesK,PopatM,YentisSM.Theeffect ofneuromuscularblockadeontheefficiencyofmaskventilation ofthelungs.Anaesthesia.2003;58:60---3.
6.CombesX, Andriamifidy L, Dufresne E,et al.Comparison of two induction regimens using or notusing muscle relaxant: impactonpostoperativeupperairwaydiscomfort.BrJAnaesth. 2007;2:276---81.
7.CormackRS,LehaneJ.Difficulttrachealintubationin obstet-rics.Anaesthesia.1984;39:1105---11.
8.Yentis SM, Lee DJ. Evaluation of an improved scoring sys-tem for the grading of direct laryngoscopy. Anaesthesia. 1998;53:1041---4.
9.SamsoonGL,YoungJR.Difficulttracheal intubation:a retro-spectivestudy.Anaesthesia.1987;42:487---90.
10.WilsonME,SpiegelhalterD,RoberstonJA,LesserP.Predicting difficultintubation.BrJAnaesth.1998;61:211---6.
11.LangeronO, MassoE,HurauxC,etal.Prediction ofdifficult maskventilation.Anesthesiology.2000;92:1229---36.
12.GuptaA,SharmaB,KumarA,SoodJ.ImprovementinCormack andLehanegradingwithlaparoscopicassistanceduringtracheal intubation.IndianJAnaesth.2011;55:508---12.
13.AbramsJT,HorrowJC, BennettJA,VanRiperD,StorellaRJ. Upper airway closure. A primary source of difficult ventila-tion with sufentanil induction of anesthesia. Anesth Analg. 1996;83:629---32.
14.OdehM,SchnallR,GavrielyN,OlivenA.Effectofupper air-waymusclecontractiononsupraglotticresistanceandstability. RespirPhysiol.1993;92:139---50.
15.VanLunterenE,StrohlKP.Themusclesoftheupperairways. ClinChestMed.1986;7:171---88.
16.WartersRD,SzaboTA,SpinaleFG,DeSantisSM,RevesJG.The effectofneuromuscularblockadeonmaskventilation. Anaes-thesia.2011;66:163---7.
17.Baillard C, Adnet F, Borron SW, et al. Tracheal intubation inroutinepracticewithandwithoutmuscular relaxation:an observationalstudy.EurJAnaesth.2005;22:672---7.
18.SivarajanM,JoyJV.Effectsofgeneralanesthesiaand paraly-sisonupperairway changesduetoheadpositioninhumans. Anesthesiology.1996;85:787---93.
19.Alexander R, Olufolabi AJ, Booth J, El-Moalem HE, Glass PS. Dosing study of remifentanil and propofol for tracheal intubationwithout theuseofmusclerelaxants.Anaesthesia. 1999;54:1037---40.
20.TraboldF,CasettaM,DuranteauJ,etal.Propofoland remifen-tanilforintubationwithoutmusclerelaxant:theeffectofthe orderofinjection.ActaAnaesthesiolScand.2004;48:35---9.
21.GreenlandKB.Aproposedmodelfordirectlaryngoscopyand trachealintubation.Anaesthesia.2008;63:156---61.