JPediatr(RioJ).2017;93(4):328---342
www.jped.com.br
REVIEW
ARTICLE
Motor
development
of
preterm
infants
assessed
by
the
Alberta
Infant
Motor
Scale:
systematic
review
article
夽
Rubia
do
N.
Fuentefria,
Rita
C.
Silveira,
Renato
S.
Procianoy
∗UniversidadeFederaldoRioGrandedoSul(UFRGS),ProgramadePós-Graduac¸ãoemSaúdedaCrianc¸aedoAdolescente,Porto
Alegre,RS,Brazil
Received17October2016;accepted22March2017 Availableonline12May2017
KEYWORDS
Prematurity; Childdevelopment; Motordevelopment
Abstract
Objective: Prematurenewbornsareconsideredatriskformotordevelopmentdeficits,leading totheneedformonitoringinearlylife.Theaimofthisstudywastosystematicallyreviewthe literatureaboutgrossmotordevelopmentofpreterminfants,assessedbytheAlbertaInfant MotorScale(AIMS)toidentifythemainoutcomesindevelopment.
Datasource: Systematicreviewofstudiespublishedfrom2006to2015,indexedinPubmed, Scielo,Lilacs,andMedlinedatabasesinEnglishandPortuguese.Thesearchstrategyincluded thekeywords:AlbertaInfantMotorScale,prematurity,preterm,motordevelopment,postural control,andfollow-up.
Datasummary: Atotalof101articleswereidentifiedand23wereselected,accordingtothe inclusioncriteria.Theagesofthechildrenassessedinthestudiesvaried,includingthefirst6 monthsupto15or18monthsofcorrectedage.Thepercentagevariationinmotordelaywas identifiedinthemotoroutcomedescriptionsoftenstudies,rangingfrom4%to53%,depending ontheagewhentheinfantwasassessed.Thestudiesshowsignificantdifferencesinthemotor developmentofpretermandfull-terminfants,withadescriptionoflowergrossscoresinthe AIMSresultsofpreterminfants.
Conclusions: Itisessentialthatthefollow-upservicesofat-riskinfantshaveassessment strate-giesandmonitoringofgrossmotordevelopmentofpreterminfants;AIMSisanassessmenttool indicatedtoidentifyatypicalmotordevelopmentinthispopulation.
©2017PublishedbyElsevierEditoraLtda.onbehalfofSociedadeBrasileiradePediatria.Thisis anopenaccessarticleundertheCCBY-NC-NDlicense(http://creativecommons.org/licenses/ by-nc-nd/4.0/).
夽
Pleasecitethisarticleas:FuentefriaRN,SilveiraRC,ProcianoyRS.MotordevelopmentofpreterminfantsassessedbytheAlbertaInfant MotorScale:systematicreviewarticle.JPediatr(RioJ).2017;93:328---42.
∗Correspondingauthor.
E-mail:rprocianoy@gmail.com(R.S.Procianoy). http://dx.doi.org/10.1016/j.jped.2017.03.003
Motordevelopmentofpreterminfants 329
PALAVRAS-CHAVE
Prematuridade; Desenvolvimento infantil;
Desenvolvimento motor
DesenvolvimentomotordeprematurosavaliadospelaAlbertaInfantMotorScale: artigoderevisãosistemática
Resumo
Objetivo: Recém-nascidosprematurossãoconsiderados deriscopara déficitsno desenvolvi-mentomotor,ocasionandoanecessidadedeacompanhamentonosprimeirosanosdevida.O objetivodopresenteestudoérevisardeformasistemáticaaspublicac¸õesqueabordamo desen-volvimentomotoramplodecrianc¸asnascidasprematuras,avaliadaspormeiodaAlbertaInfant MotorScale(AIMS),demodoàapontarosprincipaisdesfechosmotores.
Fontesdosdados: Revisãosistemáticadaspublicac¸õesdoperíodode2006a2015,indexadas nasbasesdedadosPubmed,Scielo,LilacseMedline,nosidiomasinglêseportuguês.A estraté-giadebuscaincluiupalavras-chaves:prematuro,pré-termo,prematuridade,desenvolvimento motor, controle postural, seguimento, Alberta Infant Motor Scale, prematurity, pre-term, motordevelopment,posturalcontrolandfollow-up.
Síntesedosdados: Foramidentificados101 artigoseselecionados23,conforme critériosde inclusão.Asidadesdascrianc¸asavaliadasnosestudosincluíramosprimeiros6mesesatéos 15 ou 18 mesesde idade corrigida.Variado percentual de atraso motor foi identificado na descric¸ãodosdesfechosmotoresde10estudos,indode4a53%,dependendodaidadeemque obebêfoiavaliado.Osestudosapontamdiferenc¸assignificativasnodesenvolvimentomotor deprematurosecrianc¸asnascidasatermo,comdescric¸ãodeescoresbrutosmaisbaixosnos resultadosdaAIMSdecrianc¸asprematuras.
Conclusões: Éfundamentalqueosservic¸osdefollow-updebebêsderiscoapresentem estraté-giasdeavaliac¸ãoeacompanhamentododesenvolvimentomotoramplodeprematuros,sendoa AIMSumaferramentadeavaliac¸ãoindicadaparaidentificarcomportamentosmotoresatípicos nessapopulac¸ão.
©2017PublicadoporElsevierEditoraLtda.emnomedeSociedadeBrasileiradePediatria.Este ´
eumartigoOpenAccesssobumalicenc¸aCCBY-NC-ND(http://creativecommons.org/licenses/ by-nc-nd/4.0/).
Introduction
Advances in clinical management, including the use of pediatricmechanicalventilators,surfactants,andprenatal corticosteroids, are factors that have greatly contributed toimprovesurvivalofpretermandat-riskbabiesinrecent decades.1 Although the mortality rate has dramatically improvedoverthepastdecades,pretermnewbornsremain vulnerable to many complications, including neurological insult and long-term growth and development deficits,2 resultinginthenecessityforamuchstrictermonitoringthan inthepast.3
As birth weight and gestational age decrease, and in cases where thereis an association of adverse biological conditions, such as grade III and IV peri-intraventricular hemorrhage, periventricular leukomalacia, prolonged mechanicalventilation,stageIIIretinopathyofprematurity or bronchopulmonary dysplasia, the risk of neurodevel-opmental abnormalities increases.4 Particularly, infants bornatlessthan32weeksofgestationalageandweighing less than 1500g have a high biological risk condition for development.5
Although transient neurological abnormalities occur in 40---80% of cases, disappearing in the second year of life, severeanddefinitiveneurosensorysequelae,suchasvisual and auditory deficiency and cerebral palsy, are detected in4---20% of extremelylow-weightpreterminfants.5---7 Sig-nificant developmental delays are also evident in 16% of thecases,7demonstratingasignificantcorrelationbetween developmentaldelayandpretermbirth.8
Inthis sense,carryingoutperiodicevaluationsof each child’smotordevelopment(MD)progressisessentialforthe identificationof deficits,thusfacilitating referraltoearly interventionprograms.3,8 Although thereis no homogene-ity amongthe several studies regarding the best method forevaluatingdevelopment,theimportanceofearly iden-tification, i.e., within the child’s first year of life, is a consensus.5,9 Amongtheassessment toolsusedtomonitor alterationsinMDanddifferentiateatypicalmotorbehaviors, theAlbertaInfantMotorScale(AIMS)ishighlightedasavalid and reliable tool for evaluating at-risk infants,10 demon-strating unique characteristics regarding preterm infants’ qualityofmovement at anearly age.11,12 In contrastwith thetraditionalneurologicalexamination,thescale empha-sizesfunctionalcapacitiesandthequalityofmovement,13 offeringup-to-datenormativereferencevalues.14AIMSwas validatedfortheBrazilianpediatricpopulation,resultingin aBrazilian Portuguese version,15 and new standardswere establishedtobestrepresentthis.16 Ithashighsensitivity, specificity,andaccuracytodetectmotordeficits,being indi-catedinthefollow-upofpretermchildren’sMDinthefirst 18monthsoflife.17
330 FuentefriaRNetal.
mainmotoroutcomesinrelationtochildrenbornatterm, aged0---18monthsofcorrectedage(CoA).
Method
Sourceofdata
Asystematicreviewofarticlespublishedinthelast10years andavailableinthefollowingdatabases:USNationalLibrary ofMedicineNational Institutes ofHealth(PubMed), Scien-tificElectronicLibraryOnline(SciELO),LatinAmericanand Caribbean Health Sciences (LILACS), and National Library ofMedicine UnitedStates(MEDLINE) wascarriedout.The searchstrategyincluded thecombination of thefollowing keywordsinPortuguese:prematuro,pré-termo, prematuri-dade, desenvolvimento motor amplo, controle postural, seguimento.ItalsoincludedthefollowingwordsinEnglish: preterm, prematurity, gross motor development,postural control,Alberta Infant MotorScale, follow-up. The words werealwayscombinedusingthetermAND.Asimilarsearch wasperformedinalldatabases.Thekeywordswereselected basedonthesearchforDecs/MeSHterms(LILACSand Sci-ELO).
Selectioncriteria
Studieswereincluded when theymetthefollowing crite-ria: (1) Original articlesinvolving the observational study ofMDofpreterm infants,aged0---18monthsof CoA, pub-lishedinthelasttenyears(January01,2006toDecember 31,2015).TheCoArepresentstheadjustmentofthe chrono-logicalageaccordingtothedegreeofprematurity,thatis, theweeksthatwerelackingforthegestationalagetoreach 40weeksaresubtractedfromthepreterminfant’s chrono-logicalage.6(2)Studieswithoneofthefollowingdesigns: cohortstudy(prospectiveorretrospective),cross-sectional study,control---casestudy;(3) studiesthat usedAIMSasa toolforassessingmotordevelopment;(4)studiespublished onlyinPortugueseorEnglish.
Inthepresentstudy,prematuritywasdefinedaccording tothe Shapiro---Mendoza andLackritz classification18: late prematurity(34weekscompleted to36weeksand6 days ofgestationalage),moderateprematurity(32weeksto33 weeksand6daysofgestationalage),andextreme prema-turity(23:31weeksand6daysofgestationalage).
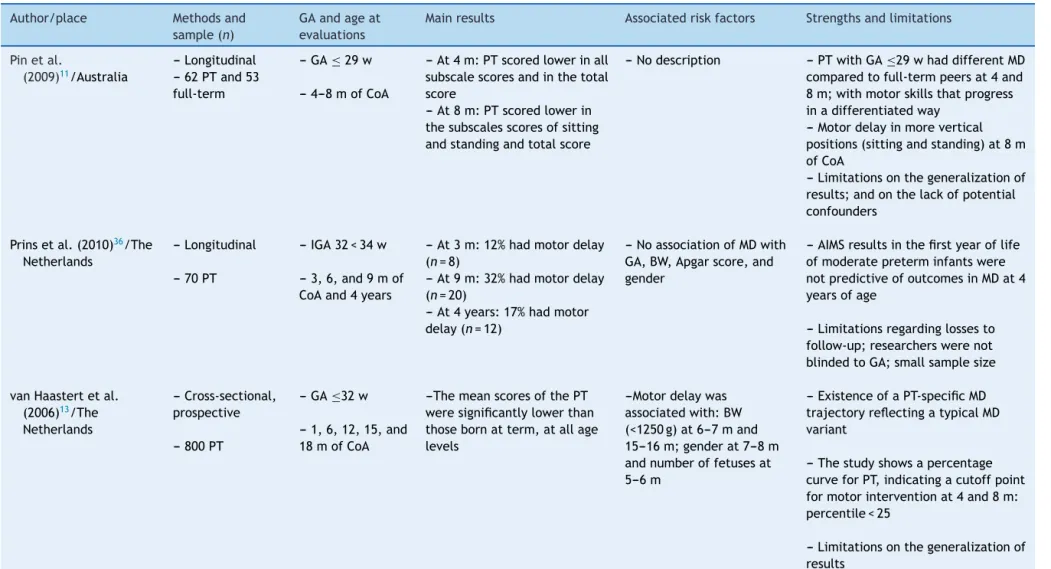
Allstudiesthatmettheinclusioncriteriaweresubmitted todataextractionandcriticalevaluationprocess.Themain characteristics were summarized following a data extrac-tionmodelconsistingof:author/local;method,andsample; gestationalage and age at theevaluations; main results; associatedriskfactors;andstrengthsandlimitations.
Datasynthesis/analysis
Thesearchstrategyresultedinatotalof101listedtitles, ofwhich23wereselectedforthereview.Afterreadingthe titleandtheabstract,78articleswereexcluded,basedon theinclusioncriteria.The23selectedarticleswereincluded inthereviewandtheresultsweredescriptivelyanalyzed.
Results
and
discussion
ThecharacteristicsofthestudiesaredescribedinTable1. Itcanbeobservedthattheperiodof2010---2015hadthe highest numberofpublications onthe subject,exceptfor theyear2014, inwhichnoarticlewaspublishedwiththis approach.Intheanalysisofstudylocations,Brazilwasthe mostprevalent,with12publications.TheNetherlandsand Australiacameinsecondplace,withsevenstudies.
Itcanbeobservedthatchildren’sagesvariedinthe stud-ies.Ofthe23selectedarticles,sixaddressedtheevaluation ofMDinagegroupsinvolvingthefirst6monthsto15or18 months,whereasfourinvolvedthefirst6monthsupto12 or13monthsofCoA.Asinglestudyaddressedtheanalysis after12monthsofCoAupto18months.Onlytwoarticles includedthelong-termstudyofMD,withafollow-upuntil theageof4years,applyinganappropriatescaleforthisage group.Conversely,thelackoffollow-upinchildrenafter12 months of CoA wasobserved in some studies.19---22 One of theminvolvedevaluationsat3monthsofCoA;fourincluded evaluationsupto5or6months,andfiveuntil8or9months ofCoA.11,19---22
Regardingthe gestationalagesinvolved in the studies, itwasobservedthatalmosthalfofthepublications(n=11) comprisedasampleofpreterminfants,bothmoderateand extreme,ofwhicheightwereofextremeprematureinfants only.Conversely,ninestudiesincludedheterogeneous sam-plesregardingtheclassificationofprematurity, sincethey involvedthethreetypesinthesamesample(late, moder-ate,andextreme).21,23---25OnestudydidnotclarifytheGA rangeoftheevaluatedchildren.15
As for the designs, it was observed that most studies hadaprospectivecohort,totaling14articles;followedby thecross-sectionaldesign,witheightpublications.Mostof theanalyzedstudies(n=15)hadasampleconsistingonlyof preterminfants,anddidnotincludeacontrolgroup com-prisinginfantsbornatterm.Forcomparativepurposes,five of thesestudies usedtheAIMSnormative sample to iden-tify differences in the gross motor development between the groups.10,13,23,26,27 The normative data are basedon a populationof2200infantsbornatterm,aged0---18months, from Alberta, Canada.28 Recently, the original AIMS data, collected20yearsago,werecomparedtodatafroma con-temporary sample of 650 Canadian children. The current normativevaluesremainappropriatetointerpretthetotal AIMSscore,andtheoriginalpercentilescontinuetoreflect the contemporaryorderand ageat onsetof infant motor skillsrepresentedintheAIMS.14
Therefore,AIMSnormativedatahavebeen widelyused nationallyandinternationallyasameasureofclinical out-come andresearch,10,12,13,17,21,29 althoughthereis concern thatAIMSCanadianstandardswouldbeinadequatefor chil-drenofdifferentcultures.29,30Inthissense,theauthorsof thenormativevaluereassessmentstudyaffirmedthat,given the stability of the resultsover a 20-year periodand the increase inthe ethnicdiversityof thecontemporary sam-ple, it may not be necessary to investigate international differences.14
Motor
development
of
preterm
infants
331
Table1 Characteristicsofstudiesinvolvingthemotordevelopmentofat-riskpreterminfantsassessedbytheAIMS.
Author/place Methodsand sample(n)
GAandageat evaluations
Mainresults Associatedriskfactors Strengthsandlimitations
Pinetal.
(2009)11/Australia
--- Longitudinal --- 62PTand53 full-term
--- GA≤29w
--- 4---8mofCoA
--- At4m:PTscoredlowerinall subscalescoresandinthetotal score
--- At8m:PTscoredlowerin thesubscalesscoresofsitting andstandingandtotalscore
--- Nodescription --- PTwithGA≤29whaddifferentMD comparedtofull-termpeersat4and 8m;withmotorskillsthatprogress inadifferentiatedway
--- Motordelayinmorevertical positions(sittingandstanding)at8m ofCoA
--- Limitationsonthegeneralizationof results;andonthelackofpotential confounders
Prinsetal.(2010)36/The Netherlands
--- Longitudinal
--- 70PT
--- IGA32<34w
--- 3,6,and9mof CoAand4years
--- At3m:12%hadmotordelay (n=8)
--- At9m:32%hadmotordelay (n=20)
--- At4years:17%hadmotor delay(n=12)
--- NoassociationofMDwith GA,BW,Apgarscore,and gender
--- AIMSresultsinthefirstyearoflife ofmoderatepreterminfantswere notpredictiveofoutcomesinMDat4 yearsofage
--- Limitationsregardinglossesto follow-up;researcherswerenot blindedtoGA;smallsamplesize
vanHaastertetal. (2006)13/The Netherlands
---Cross-sectional, prospective
---800PT
---GA≤32w
---1,6,12,15,and 18mofCoA
---ThemeanscoresofthePT weresignificantlylowerthan thosebornatterm,atallage levels
---Motordelaywas associatedwith:BW (<1250g)at6---7mand 15---16m;genderat7---8m andnumberoffetusesat 5---6m
---ExistenceofaPT-specificMD trajectoryreflectingatypicalMD variant
---Thestudyshowsapercentage curveforPT,indicatingacutoffpoint formotorinterventionat4and8m: percentile<25
332
Fuentefria
RN
et
al.
Table1 (Continued)
Author/place Methodsand sample(n)
GAandageat evaluations
Mainresults Associatedriskfactors Strengthsandlimitations
Pinetal.
(2010)12/Australia
---Longitudinal
---58PTand52 full-term
---GA≤29w
---4,8,12and18 mofCoA
---TotalscoresofPTwerelower inall4agegroups
---Anevidentdifferencewas foundinthesubscalesittingat 8mofCA
---PoorMDwasassociated with:HIV,chroniclung disease,pre-andpostnatal corticoid,andApgarscore (incertainagegroups)
---Childrenborn≤29wGAhada differentmotortrajectoryfromtheir full-termpeersfrom4to18mof CoA;withmotorskillsthatprogress differentlyovertime
---Duetothesmallsamplesizeofthe study,itwasnotpossibletoanalyze allfactorsassociatedwithMD; Limitationsonthegeneralizationof results
FormigaandLinhares (2011)10/Brazil
---Cross-sectional
---308PT
---GA<37wand BW<2500g
---1at12m(12 independent groups)
---TheMDofBrazilianPTswas lowerthanthatoftheAIMS normativesampleinallage groupsevaluated(1---12m)
---Nodescription ---Thestudydemonstratesthatthe MDofPTisdifferentfromtheir full-termpeers
---ItfeaturesanMDcurveforBrazilian PT,accordingtothedistributionof AIMSpercentiles;indicatingthe5th and10thpercentilesasthebest cutoffstoidentifymotordelay
---Limitationsregardingthestudy designandthesample(itwasnot constantduringtheanalyzedm) ManaceroandNunes
(2008)32/Brazil
---Cross-sectional
---44PT
---GA32<34w (samplestratified accordingtoBW)
---40thwof gestationalage,at 4and8mofCoA
---Thepercentilesvariedin bothgroupsbetween10%and 90%;withMDconsidered normalandsimilaracquisition rateinbothgroups
---Meansofthegroup≤1750g:
40thw:43.2%;4thm:42.9%; 8thm43.9%
---Meansofthegroup≥1750g:
40thw:47%;4thm47.8%;8th m:45.7%
---AIMSscoresdidnotshow associationwithBW
---ThePTshowedanormal progressivesequenceofmotorskill onset,withinanappropriatemean percentileintheAIMS(43.2---45.7%), independentlyfromBW
---Limitationsrelatedtogroup stratification,withaBW
Motor
development
of
preterm
infants
333
Table1 (Continued)
Author/place Methodsand sample(n)
GAandageat evaluations
Mainresults Associatedriskfactors Strengthsandlimitations
Wangetal. (2010)23/Taiwan
--- Retrospective
--- 93PTwith BW<1501g
--- GA24<35w
--- 6and12mof CoA
---At6m:30.1%(n=28)had motordelay
---At12m:16.1%(n=15)had motordelay
--- At6and12mofCoAthePT showeddifferencesinthe meanscoreofAIMS,showing poorMDwhencomparedtothe normativedata
---At6m:Correlationof motordelaywithmedical complications,BW, maternallevelofschooling andApgarscoreinthe5th min
---At12m:Correlationwith medicalcomplicationsand maternalage
--- Thestudysubstantiatesand reinforcestheimportanceofearly assessmentatfollow-upinthefirst6 mofCoAofhigh-riskPT
--- Givesevidencethattheinfluence ofsocialandenvironmentalfactors onMDofPTissignificant
--- Thesamplesizewasrelatively small,withonly93casesfornine independentvariables;thestudy designwasretrospectiveandall variableswereextractedfroma conveniencecohortsample RestiffeandGherpelli
(2012)24/Brazil
--- Prospective
--- 101PTand52 full-term
--- GA25<36w
--- 1---18mofCoA (monthly evaluations)
--- Therewasnodifference betweenPTandfull-term newbornsinthemeanAIMS scores,exceptfortheeighth, ninthandtenthm
---Themeanageat
independentgaitacquisitionin PTnewbornswas381.6days, andinfull-term,368.6days
--- Variablesassociatedwith delayedgaitacquisition: BW,birthlength,and durationofneonatal hospitalization
---Thestudypresentsevidencethat prematureinfantsacquire
independentgaitlaterthanfull-term infants,withadelayof
approximatelyonemonth
---Thevariablesbirthweightand lengthanddurationofneonatal hospitalizationwerepredictiveof delayedgaitacquisitioninPT Spittleetal.
(2015)17/Australia
--- Cohort, prospective
--- 138PT
--- GA<30w
--- 4,8and12mof CoAandat4years
---At4m:22%(n=19)had percentile<10th
---At8m:
26%(n=23)hadpercentile <5th;
---At12m:36%(n=31)had percentile<5th
Cerebralpalsy(4years):7%
(n=6)hadCP
--- Nodescription ---AIMSaccuracywasbetterwhenthe threeassessmentsovertimeshowed delay,ratherthanonlyone.AIMS showedtobelessaccurateat12m andmoreaccurateat4mformotor deficitsfoundat4years,includingCP ---Thestrengthsincludetheuseof standardizedmotorassessmentsfora longtimeandthehighfollow-up rates
334
Fuentefria
RN
et
al.
Table1 (Continued)
Author/place Methodsand sample(n)
GAandageat evaluations
Mainresults Associatedriskfactors Strengthsandlimitations
RestiffeandGherpelli (2006)26/Brazil
---Cohort, observationaland prospective
---43PT
---IG26<36w
---0---13mofCoA (monthly evaluations)
---ThemeangrossMDscoresof thePTweredifferentfrom thoseoftheAIMSstandard, onlywhenusingchronological age.Whencorrectingforage, thescoresweresimilar ---AllPTwereabletowalk withouthelpbefore18mof CoA
---Nodescription ---Theresultssuggestthat,tomore accuratelyidentifychildrenwithreal motordelaybyAIMS,the
chronologicalageshouldbe
correctedaccordingtothedegreeof prematurity,preventingfalse negatives
ValentiniandSaccani (2012)15/Brazil
---Cross-sectional andlongitudinal
---766childrenand 22professionals
---0---18m ---ThePTshoweddifferencesin relationtothefull-term childrenregardingthegross andpercentilescores;PT scoreswerethelowest
---Theresultsofpremature infantswereassociatedwith atypicalMDoratrisksituation (theageusedwasnot corrected)
---Nodescription ---Thefinaltranslationandtheedited scaleresultedinthe
Brazilian---PortugueseversionofAIMS (AIMS-BR);avalidatedandreliable tooltoassesschilddevelopmentand plananinterventionforBrazilian children.
---Limitedpredictivevaliditywas observed,whichmaybeduetothe shorttimeduringwhichthegroups werefollowedlongitudinally FettersandHuang
(2007)19/Boston,USA
---Cohort
---68children(30 PTwithVLBWand withwhitematter lesions;21PTwith VLBWandno whitematter lesions;17 full-terminfants)
---GA24<31wand 6days
---1,5and9mof CoA
---Therewerenodifferencesin thescoresofthesubscales,the totalscoreandtheAIMS percentilebetweenPTwithout lesionsandfull-termbabies,at 1and5m
---At9m,therewasa differenceinthetotalscore andtheAIMSpercentile betweenPTwithandwithout whitematterlesion
---ThegroupofPTwithwhite matterlesionhadthelowest scoresatAIMS
---AIMSscoreswerenot associatedwith:gender, ethnicity,GA,orBW
---Thepronesleeping positionwaspositively associatedwithMD
---At5m,playinginthe pronepositionhadpositive effectsonMD
---Thedatasuggestthatsleepingin thesupinepositiondoesnotappear tohaveanegativeeffectonMD;the pronepositionappearstohavea positiveimpact
---At5m,sleepingandplayinginthe pronepositionweresignificantly associatedwithAIMSscores
Motor
development
of
preterm
infants
335
Table1 (Continued)
Author/place Methodsand sample(n)
GAandageat evaluations
Mainresults Associatedriskfactors Strengthsandlimitations
Formigaetal. (2010)31/Brazil
--- Prospective
--- 10children
--- PTwithLBW (meanGA:32.8w)
--- 4---8mofCoA
---From4to5m:50%with suspectedMD;40%withmotor delay
---From5to6m:30%with suspectedMD;40%withmotor delay
---From7to8m:50%with suspectedMD;30%withmotor delay
--- Themeanscoreinthesitting positionincreasedoverthe threeassessments;thesetting positionshowedahigh correlationwiththeother acquisitions
--- Nodescription --- AIMSalloweddetectingMDdelayin PTchildrenbornwithlowweightup tothe8thmofCoA,mainlyregarding sittingcapacity
--- Therewasagreatercorrelation betweenthesittingandtheprone positionateachageevaluated
--- Limitationsregardingsamplesize andabsenceofcontrolgroup
Cabraletal. (2014)20/Brazil
--- Cross-sectional andcomparative study
---30children(15 PTand15 full-term)
GA:PT<37w
--- 4---6mofCoA
--- 53%(n=8)ofPThad percentileequaltoorlower than5atAIMS
---Therewasnodifferencein AIMStotalscore,thegroups weresimilarintermsofMD
--- Nodescription ---HighMDvariabilityobservedamong thesubjects,sincebothgroupshad childrenwithhighandlowmotor performance
---Thesamplesizelimitedanalysesof correlationbetweenimportantstudy variables
Wangetal. (2013)33/Taiwan
--- Longitudinal
--- 35PTwithPVL; 70PTwithout PVL;76full-term infants
--- GA≤27w
--- 6,12,and18m ofCoA
--- Differenceswerefoundin totalscoresbetweenPT withoutPVLandfull-term infantsonlyat6and12m;and nodifferencewasfoundat18 m
--- At6,12,and18m, differenceswerefoundinthe totalscoresbetween:PTwith PVLvs.PTwithoutPVL; PTwithPVLvs.full-term infants
---At18m,onlyPTwithPVL weredifferentfromPTwithout PVLandoffull-terminfants
---Nodescription ---FirststudythatshowsMDresults throughtheAIMSofVLBWPTwith PVL
---VLBWPTwithcysticPVLareat greaterriskofmotorimpairmentand delaysinthegrossmotormilestones whencomparedtoPTwithoutPVL, withthesupinesubscalebeingthe mostusefultodiscriminatethem,as earlyas6mofCoA
336
Fuentefria
RN
et
al.
Table1 (Continued)
Author/place Methodsand sample(n)
GAandageat evaluations
Mainresults Associatedriskfactors Strengthsandlimitations
Nuysinketal. (2013)27/The Netherlands
---Prospective cohort
---95PT
---GA<30wor BW<1000g
---3,6,and15m ofCoA
---Themeanageofgait acquisitionwas15.7mofCoA (50%ofthesamplewalkedat thisage)
---Childrenbornwithlessthan 30wofGAstartedwalking independentlyapproximately3 maftertheirfull-termpeers, evenwithagecorrection
---Thelevelofgrossmotor maturationat6mofCA, andethnicitywereclearly associatedwithageat independentgait acquisition
---AIMSat3mofCoAcouldnot reliablypredictthegrossMDor walkingskillsat15mofvery prematurebabies
---Aclinicalimplicationisthatthe CoAof3mcanbeconsidered precocioustogivepredictivevalidity ontheoutcomesinthelaterMDof preterminfants
---Limitationsrelatedtosamplesize andthepossibilityofmemoryand selectionbiasinthemeanagesofthe evaluations
Burgeretal.
(2011)25/SouthAfrica
---Descriptiveand prospective
---115children withBW≤1250g
---GA:27<36w
---3and12mof CoA
---22children(19%)hada percentilebelow5at12mof CoA
---Themeanpercentileof evaluationsat12mofCoAwas 35.0±25.1
---Nodescription ---AIMSat12m,wasusedinthe child’sfollow-up,evaluatedusingthe Prechtlmethodat3m,whichshowed highpredictivevalidity,sensitivity andspecificity
---Highspecificityandlowfalse positiveresultsdonotadd
unnecessaryreferralofinfantstothe alreadyoverburdenedand
underdevelopedrehabilitation services
Snideretal.
(2008)22/Netherlands
---Prospective cohort
---100children
---GA≤32wand BW<1500g
---34w;atterm (38---40w)andat3 mofCoA
---37%ofthechildren(n=37) hadabnormaldevelopmentat 3mofCoA(percentile<10)
---Themeanpercentileat3m ofCoAwas17.1(11.7),ranging from2to55
---Nodescription ---AIMSwasusedinthefollow-up evaluationat3mofCoA
---Alowpowerratio(r≤0.25)was foundbetweengeneralmovements assessmentandthetestsusedat3m
Motor
development
of
preterm
infants
337
Table1 (Continued)
Author/place Methodsand sample(n)
GAandageat evaluations
Mainresults Associatedriskfactors Strengthsandlimitations
SouzaandMagalhães (2012)35/Brazil
--- Observational andlongitudinal
--- 60children(30 PTand30 full-terminfants)
--- GA≤34wand BW≤1500g
--- 12,15,and18m ofCoA
--- PTGwalkedat13.8±2.0m ofCoA(415±59days)andthe CG,at12.3±2m(368±62 days)
--- Nodifferenceswerefound betweenthegroupsat12and 15m
--- Therewasadifference betweenthegroupsonlyat18 m
--- Thecorrelationbetween GAandAIMSat12mofCoA wasnotsignificant
--- Althoughnodifferencewasfound inAIMSat12and15m,powerwas 0.95atbothages.Theseresultsraise questionsaboutthediscriminatory powerofAIMStoidentifythegross motordelayinBrazilianchildren after12m
--- Limitations:limitedsamplesize andthenon-inclusionofthe economiclevelasacriterionfor matching;theuseofimportedtests; andtheuseofparents’reportsto allowthecomparisonofthetimeto gaitacquisition
Maiaetal. (2011)34/Brazil
--- Longitudinaland comparative
--- 48children(24 PTand24 full-term)
--- GA32<36.5w
---4and6mofCoA
--- Therewasadifference betweenthegroupsinthe standingpositionat4m;and at6m,intheprone,sitting andstandingpositions
--- Thetotalscoresat6m indicatedadifferencebetween thegroups,withthePT showinglowerscores
--- Nodescription --- Inthetotalscoreandinthe percentile,at4mofCoA,therewas nogreatdifferenceinthefour positions.At6m,thefull-termgroup showedahigherscoreinthefour AIMSpositions
---Limitationsregardingsamplesize andtheinclusionofchildrenfrom otherregionsofBrazil
deCastroetal. (2007)37/Brazil
--- Exploratory
--- 55PT
--- GA<37w
--- Between4and5 mofCoA
--- GAbetween29and34w: 26%(n=8)withpercentile<10
--- GAbetween35and36w: 4%(n=1)withpercentile<10
--- Consideringallthesample (GA<37w):
16.4%(n=9)with percentile<10
--- Thepercentage
ofchildrenwithAIMSscore below
percentile10washigher amongthose
bornatlowerGA(29to34 w)
--- Morepreterminfants(29---34wof GA)hadlowerscoreswhenassessed bytheAIMS,whencomparedtothe PTwith35and36wofGA
--- Theresultsreinforcetheneedfor moredynamictherapeutic
338
Fuentefria
RN
et
al.
Table1 (Continued)
Author/place Methodsand sample(n)
GAandageat evaluations
Mainresults Associatedriskfactors Strengthsandlimitations
Formigaetal. (2015)38/Brazil
---Cross---sectional
---182PMTand LBW
---GA<37w
---2---4m;4---6m; and6---8m(Three independentage groups
---4---6m:
47%ofsamplewithatypicalMD ---6---8m:
36%ofsamplewithatypicalMD
---ThereweredifferencesinMD ofthe3agegroups,when comparingCoAof chronologicalage
---Nodescription ---Thefindingssuggestthatthe correctedageisthebestwayto assesstheactualperformanceof preterminfantsatrisk,especiallyin thefirstyearoflife
---Studylimitationsregardingdesign andlackoffollow-upofchildren olderthan12m
Formigaetal. (2013)21/Brazil
---Cross-sectional
---70PMT (CGof43PMT fromanother study)
---GA<37wand BW<2500g
---Between0and6 mofCoA
---1m:
30%withdelay(percentile<10) ---2m:
20%withdelay(percentile<10) ---3rdm:
40%withdelay(percentile<10) ---4thm:
33%withdelay(percentile<10) ---5thm:
33%withdelay(percentile<1 0)
---6thm:
43%withdelay(percentile<10)
---Therewerenodifferencesin thetotalscoreofthePMT infantsbyAIMSatanyofthe comparedages
---Nodescription ---TheseresultssuggestthatPMT infantsfromdifferentregions, despitebeingsubmittedtodifferent environmentalinfluences,have similarMD
---Itisrelevanttocreatefollow-up programsforat-riskinfantsaccording totheregionormunicipalitywhere theylive
---Althoughthesamplesofinfants studiedwereconsidered
homogeneous,inrelationtoGAand BW,differenceswereobservedin someagegroupsevaluated
Motordevelopmentofpreterminfants 339
differences between Brazilian, Canadian, and Greek chil-dren,found inthatcomparativestudyofthreepopulation samples,prevailed upto15 monthsof age;a representa-tiveportionoftheBraziliansample(34.6%)hadlowermotor performancethantheexpected.Accordingtotheauthors,29 theresultsmayindicateadifferenttrajectoryinMD, pos-sibly influencedbysociocultural factorspertinenttochild care.
RegardingthemainresultsrelatedtoMDwhenassessed byAIMS,thereisacertainheterogeneityinthedescription ofmotoroutcomes.Onlytwostudies11,12discussedthe dif-ferencesobserved in motor acquisitionson each subscale (prone,supine,sitting,andstanding),showingthe percent-ageof pretermchildrenversuschildrenborn atterm that scoredthe assessedacquisition.Pinetal.11 described this dataintheirstudyofMDofpreterminfantsbornata gesta-tional age ≤29 weeks and infants born at term, assessed at 4 and 8 months of CoA. At the age of 4 months, all full-terminfantswereabletoplaywiththeirhandsonthe midline, in comparisonwith 81% of preterm infants; at 8 monthsof CoA, preterm infantsdid notprogress asmuch asexpected,sincemanywerenotabletositindependently (25%vs.90%).
Pin et al.12 followed-upthis cohort until 18 monthsof CoA,anddiscussedthedifferencesofeachevaluated acqui-sition. At 12 months of CoA, more full-term infants than preterminfantsreached thetotalscorein thesitting sub-scale(94%vs.68%);moreover,alargernumberofchildren inthecontrolgroupwereabletoperformlateralgaitalong apieceoffurnitureinthestandingsubscale(90%vs.70%). At18monthsofCoA,almostallfull-termchildrenreached thetotalAIMSscore;however,17prematurechildrenwere unabletodoso(37%vs.2%).
Several studies have compared the MD of preterm and full-term children in the first 2 years of life and demonstrated that the former had an inferior motor performance.10---13,23,31 Of the 23 selected articles, 14 observed significant differences in motor performance between preterm andfull-term infants; however, theage whenthedifferencesareidentifiedvaried.
Conversely, two studies20,26 failed to observea signifi-cant difference in the MD of preterm infants versus that offull-terminfantswhenCoAwasconsidered.Restiffeand Gherpelli26demonstratedthatthemeansofthegrossscores of43low-riskpretermnewbornsweresimilar,afterage cor-rection,totheAIMSstandardsinthe differentagegroups overthe13-monthofCoAperiod.Cabraletal.20alsostated that, when comparing a group of preterm (n=15) with a groupoffull-terminfants(n=15)at4and6months,there wasnosignificantdifferenceinAIMStotalscore,aswellas intheproneandsittingsubscalescores.Inthesetwo stud-ies,the methodologicalcharacteristics, such asthe small samplesize20andtheinclusionofpreterminfantswithlow riskforneurologicallesionandneuromotordisorders,26may haveinfluencedthedescribedfindings.
Corroborating these findings, Manacero and Nunes32 statedthatthemotorperformanceofpreterminfants with-outneurologicaldisorders, evaluatedat the40th weekof gestationalage,inthefourthandeighthmonthsofCoA,was normalbytheAIMSscale.Thepreterminfantsshoweda nor-malprogressivesequenceofmotorskillonsetinallassessed postures(prone,supine,sitting,andstanding),expressedby
themeanpercentileof43.2---45.7%,consideredadequatein theAIMS.32
Among the studies that highlighted significant differ-encesinmotorperformancebetweenpretermandfull-term infants,acriticalanalysiswasperformedbasedontheageat theassessments.At4monthsofCoA,threestudiesshowed differences.10---12 However, only two of these established thiscomparativeanalysisinvolvingextremepreterminfants, withacontrolgroupoffull-terminfants.
Pinet al.11 described lowerscores in all subscalesand inthe total scale score,noting that preterm infants with gestationalage≤29weekshavemotorskills thatprogress differentlyfromtheir full-termpeersin thefourpostures assessed at 4 months of CoA. Pin et al.12 also reported lower total AIMS scores for preterm infants in this age groupwhencomparedwiththecontrolgroup, demonstrat-inglowerscoresinthesupine,prone,andsittingsubscales. Differencesin theMDof preterm andfull-term infants werealsodescribedat6monthsofCoA.Fivestudiesshowed that preterm infants had lower total AIMS scores in this agegroupwhencomparedtothosebornatterm.10,13,23,33,34 Inthe studyby Wangetal.,33 preterm infantsscored sig-nificantly lower than the control group in all subscales. However,although theyshowedlower scores at 6months ofCoA,theyreachedtheMDoftheir full-termpeersover the18 months of CoA. Maia et al.34 alsodescribed lower scoresinthegroupofpreterminfantsinthefourpositions assessedbytheAIMS.
The differences found between preterm and full-term infantsat4and6monthsofCoAsupportandreinforcethe importanceofearlyassessmentinthefollow-upasearlyas inthefirst6monthsofCoA,especiallyinhigh-riskpreterm infants.23 At 8 months of CoA, four studies found differ-encesintheAIMStotalscorebetweenpreterminfantsand theirfull-term peers.10---12,24 Ofthese, twostudies, by Pin etal.11,12involvedtheevaluationofthemotorperformance ofextremepreterminfants(thosewithgestationalage≤29 weeks).Theauthors11,12 describedsignificantlylowertotal scoresthanthoseobservedforthecontrols,aswellaslower scores in the sitting and standing subscales, demonstrat-ing a motor delay in more vertical postures in this age group.
FivestudiesfounddifferencesinMDat12monthsofCoA, indicatinglowertotalscoresinpretermchildren.10,12,13,23,33 In three of these studies, extreme prematurity was the assessed group, indicating there is a specific trajectory of MD that reflects a variant of the typical MD in this population.12,13,33 Pin et al.12 found lower scores in the prone,sitting, and standing subscales. Wang etal.33 also stated that preterm infants differed fromtheir full-term peersinthestandingsubscaleinthisagegroup.
340 FuentefriaRNetal.
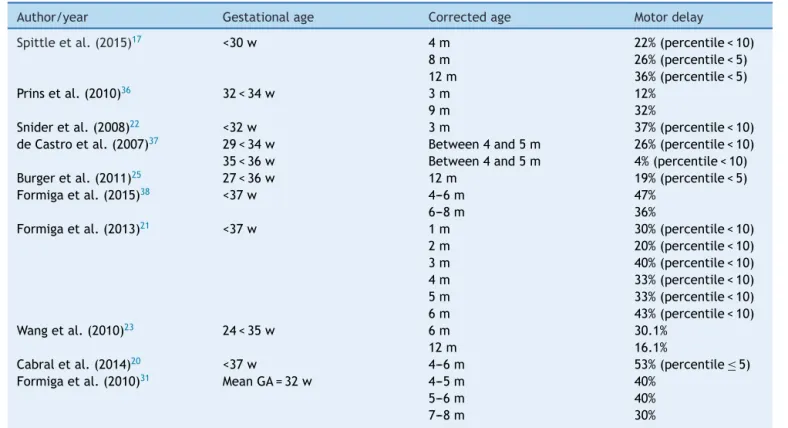
Table2 MotordelaypercentageinpretermchildrenassessedbyAIMS.
Author/year Gestationalage Correctedage Motordelay
Spittleetal.(2015)17 <30w 4m 8m 12m
22%(percentile<10) 26%(percentile<5) 36%(percentile<5)
Prinsetal.(2010)36 32<34w 3m
9m
12% 32%
Snideretal.(2008)22 <32w 3m 37%(percentile<10)
deCastroetal.(2007)37 29<34w 35<36w
Between4and5m Between4and5m
26%(percentile<10) 4%(percentile<10)
Burgeretal.(2011)25 27<36w 12m 19%(percentile<5)
Formigaetal.(2015)38 <37w 4---6m
6---8m
47% 36%
Formigaetal.(2013)21 <37w 1m
2m 3m 4m 5m 6m
30%(percentile<10) 20%(percentile<10) 40%(percentile<10) 33%(percentile<10) 33%(percentile<10) 43%(percentile<10)
Wangetal.(2010)23 24<35w 6m
12m
30.1% 16.1%
Cabraletal.(2014)20 <37w 4---6m 53%(percentile≤5)
Formigaetal.(2010)31 MeanGA=32w 4---5m
5---6m 7---8m
40% 40% 30%
AIMS,AlbertaInfantMotorScale;w,weeks;m,months;GA,gestationalage.
Regardingindependentgait,threestudiespresented evi-dence that preterm infants acquire this ability at a later agethanthosefull-term.24,27,35RestiffeandGherpelli24and Souza and Magalhães35 reported that there is a delay of approximatelyonemonth, witha meanof13.8monthsof CoA for preterm infants and 12.3 months for the control group.Inturn,Nuysinketal.27 reportedthatchildrenborn atlessthan30weeksofgestationalagestartwalking inde-pendentlyapproximatelythreemonthsaftertheirfull-term peers,evenwithagecorrection.Inthisstudy,27 themean ageofindependentgaitacquisitionforpreterminfantswas 15.7monthsofCoA.
For Pin et al.,11,12 the significant differences in motor performance between preterm and full-term infants over the 18 months of CoA appearto be related to the delay inmotor skilldevelopmentinthe moreverticalpositions, suchassittingandstanding,positionsthatrequiregreater muscle strength and antigravity motor control. Signs of trunk dystonia or imbalance between flexorand extensor forceswerefound morefrequentlyinpreterminfantsand overtime,possiblybecausethe demandfor postural con-trolmadetheinadequateflexorcontrolinthetrunkmore apparent, leading to a delay in the capacity tomaintain sittingandstandingpostures,affectingtheabilitytowalk independently.
Although it is important to identify differences in the motor performance of preterm infants in different age groups, it is also important to identify the motor delay percentage in this population. Therefore, some studies17,20---23,25,31,36---38presentedthemotoroutcomesbased ontheAIMSpercentile,describingthepercentageofdelay foundinpreterminfants(Table2).
Tenstudiesthatusedthisapproachwereretrieved, show-ingavariedpercentageofevaluatedmotor delay,ranging from 4% to 53%, depending at what age the baby was evaluatedinthe firstyearof life.It isobserved thatfour studiesdefinedthegestationalageofthesampletoinclude onlymoderate and/orextreme prematureinfants17,22,36,37; the others involved the outcome analysis, considering a broaderrangeofgestationalage.Extremepreterminfants hada22---37%delayatthecorrectedagesof3---4months,17,22 and 26---36% at the ages of 8 and 12 months.17 Moder-atelypreterminfantsappeartohavebetteroutcomesat3 months,witha12%motordelay;however,thisfactdoesnot seemtobeconfirmedwhentheageof9monthsisassessed (32%).36
Among the variables associated with motor delay, it wasobservedthatlowerbirth weightwasassociatedwith lowergrossAIMSscoreinthreestudies.13,23,24Inturn,some studies didnotfindthis association.19,32,36 Other variables associated with poor motor outcome refer to PIVH (peri-intraventricularhemorrhage),chroniclungdisease,pre-and post-natalcorticosteroids,andlowerApgarscore.12 Ethnic-ity, low maternal schooling, and young maternal age are socialandenvironmentalfactorsthatalsohaveasignificant influenceonpretermMD.23,27
Motordevelopmentofpreterminfants 341
assessmentoftheincludedstudieswasalsoalimitationof thepresentreview.Forfuturestudies,asystematicreview of publications involving standardized assessments of the motorperformanceofpreterminfantsinthepre-schooland schoolyearsissuggested,asthereisaconcernthat prema-tureinfantsmaybemorevulnerablewhenenteringschool age.
Motordelay,aswellasthedifferencesinMDinpreterm infants,areassociatedwiththebiologicalfactorsinvolved, suchasgestationalage,birthweight,cerebralwhitematter lesion,39andassociatedmorbidities.40Additionally,adverse socioculturalconditionscanaggravatethechildren’srisk,29 withapoorprognosisfortheirdevelopment.Pretermbirth challengesmotor controldevelopment,asthechild starts the extrauterine life with immature and more vulnerable centralandsensory-motorsystems.Asaresult,oneofthe most frequent sequelae is the lack of adequate postural controlduringmotor activities.41 Thus,healthcare profes-sionalsmustbeattentivetothedifferentriskfactorsandthe MDofthepreterminfant,inordertodetectdeficitsearly, referringthechildandthefamilyforearlyintervention.
Conclusion
Mostoftheanalyzedstudiessoughttoidentifydifferencesin grossmotordevelopmentthroughtheAIMSbetweenpreterm and full-term infants at differentagesof evaluation. The studiesindicateaninferiormotorperformanceofpreterm infants in the first 18 months of CoA, either through the comparativeanalysiswiththeCanadianAIMSdataor with thedataobtainedfromacontrolgroup,consistingof chil-drenbornatterm.Dependingontheageoftheassessment and the sample characteristics, a variable percentage of motordelaywasidentifiedinpreterminfants.Lowmaternal schoolingandyoungmaternalage,aswellasfactorsrelated toprematurity,suchaslowerbirthweight,PIVH,andchronic lungdisease,wereassociatedwithatypicalmotoroutcome intheAIMS.
Thus,childrenbornprematurelyandinunfavorable envi-ronmentalandsocialconditionsmaybemorevulnerableto motorproblemsataveryearlyage.Therefore,itiscrucial that the follow-up services of at-riskinfants have strate-gies for the evaluation and follow-up of the gross motor developmentof preterminfants, fromthedischarge from theneonatalICUtothefirst2yearsofthechild’slife;AIMS is atool indicated toidentifyatypical motorbehaviorsin thispopulation.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.Shapiro-Mendoza CK, Lackritz EM. Epidemiology of late and moderate pre-term birth. Semin Fetal Neonatal Med. 2012;17:120---5.
2.BehrmanRE,ButlerAS.Pretermbirth:causes,consequences, and prevention. In: Committee on understanding prema-ture birth and assuring healthy outcomes. Washington, DC:
Institute of Medicine of the National Academies, National AcademiesPress;2007.
3.AmericanAcademyofPediatricsCommitteeonFetusand New-born.Hospitaldischargeofthehigh-riskneonate.Pediatrics. 2008;122:1119---26.
4.StoinskaB,GadzinowskiJ.Neurologicalanddevelopmental dis-abilities inELBW and VLBW: follow up at 2 years ofage. J Perinatol.2011;31:137---42.
5.RebageV,Ruiz-EscusolS,Fernández-VallejoM,Montejo-Ga˜nán I,García-I˜niguezJP,Galve-PradelZ,etal.Neurologicalnewborn inourcenterandfollow-up.RevNeurol.2008;47:S1---13. 6.RugoloLM.Crescimentoedesenvolvimento alongoprazodo
prematuroextremo.JPediatr(RioJ).2005;81:S101---10. 7.HighRiskFollow-upWorkingGroup(KowloonRegion).
Neurode-velopmental outcomes of extreme-low-birth-weight infants born between 2001 and 2002. Hong Kong Med J. 2008;14: 21---8.
8.SoleimaniF,VameghiR,HemmatiS,HemmatiS,Salman-Roghani R.Perinatalandneonatalriskfactorsforneurodevelopmental outcomeininfantsinKaraj.ArchIranMed.2009;12:135---9. 9.AmorimRC,LaurentinoGE,BarrosKM,FerreiraAL,MouraFilho
AG,RaposoMC.Programadesaúdedafamília:propostapara identificac¸ãodefatoresderiscoparaodesenvolvimento neu-ropsicomotor.RevBrasFisioter(SãoCarlos).2009;13:506---13. 10.Formiga CK, Linhares MB. Motor development curve from
0 to 12 months in infants born preterm. Acta Paediatr. 2011;100:379---84.
11.PinTW,DarrerT,EldridgeB,GaleaMP.Motordevelopmentfrom 4to8monthscorrectedageininfantsbornatorlessthan29 weeks’gestation.DevMedChildNeurol.2009;51:739---45. 12.PinTW,EldridgeB,GaleaMP.Motortrajectoriesfrom4to18
monthscorrectedageininfantsbornatlessthan30weeksof gestation.EarlyHumDev.2010;86:573---80.
13.vanHaastertIC,deVriesLS,HeldersPJ,JongmansMJ.Early grossmotordevelopmentofpreterminfantsaccordingtothe AlbertaInfantMotorScale.JPediatr.2006;149:617---22. 14.DarrahJ,BartlettD,MaguireTO,AvisonWR,Lacaze-Masmonteil
T.Haveinfantgrossmotorabilitieschangedin20years?A re-evaluationoftheAlbertaInfantMotorScalenormativevalues. DevMedChildNeurol.2014;56:877---81.
15.Valentini NC, Saccani R. Brazilian validation of the Alberta InfantMotorScale.PhysTher.2012;92:440---7.
16.Saccani R, Valentini NC. Reference curves for the Brazilian AlbertaInfantMotorScale:percentilesforclinicaldescription andfollow-upovertime.JPediatr(RioJ).2012;88:40---7. 17.SpittleAJ,LeeKJ,Spencer-SmithM,LoreficeLE,AndersonPJ,
DoyleLW.Accuracyoftwomotorassessmentsduringthefirst yearoflifeinpreterminfantsforpredictingmotoroutcomeat preschoolage.PLoSOne.2015;10:e0125854.
18.Shapiro-Mendoza CK, Lackritz EM. Epidemiology of late and moderate preterm birth. Semin Fetal Neonatal Med. 2012;17:120---5.
19.Fetters L, Huang HH. Motor development and sleep, play, and feeding positions in very-low-birth weight infants with and without white matter disease. Dev Med Child Neurol. 2007;49:807---13.
20.Cabral TI, Pereira da Silva LG, Tudella E, Simões Martinez CM. Motordevelopment and sensory processing: a compara-tivestudybetweenpretermandterminfants.ResDevDisabil. 2014;36C:102---7.
21.FormigaCK,NonatoJC,AmaralLE,FagundesRR,LinharesMB. Comparac¸ãododesenvolvimentomotordelactentespré-termo de duas amostras regionais brasileiras. J Hum Growth Dev. 2013;23:352---7.
342 FuentefriaRNetal.
23.WangTN,HoweTH,HinojosaJ,HsuYW.Posturalcontrolof pre-terminfantsat6and12monthscorrectedage.EarlyHumDev. 2010;86:433---7.
24.RestiffeAP,GherpelliJL.Differencesinwalkingattainmentages between low-riskpretermand healthy full-terminfants. Arq Neuropsiquiatr.2012;70:593---8.
25.BurgerM,FriegA,LouwQA.Generalmovementsasapredictive tooloftheneurologicaloutcomeinverylowandextremelylow birthweightinfants---aSouthAfricanperspective.EarlyHum Dev.2011;87:303---8.
26.Restiffe AP, Gherpelli JL. Comparison of chronological and corrected ages in the gross motor assessment of low-risk preterminfantsduringthefirstyearoflife.ArqNeuropsiquiatr. 2006;64:418---25.
27.NuysinkJ,vanHaastertIC,EijsermansMJ,Koopman-Esseboom C,HeldersPJ,deVriesLS,etal.Predictionofgrossmotor devel-opmentandindependentwalkingininfantsbornverypreterm using the Testof Infant MotorPerformance and the Alberta InfantMotorScale.EarlyHumDev.2013;89:693---7.
28.PiperMC,PinnellLE,DarrahJ,MaguireT,ByrnePJ.Construction andvalidationoftheAlbertaInfantMotorScale(AIMS).CanJ PublicHealth.1992;83:S46---50.
29.Saccani R,Valentini NC.Cross-cultural analysisofthemotor developmentofBrazilian,GreekandCanadianinfantsassessed with the Alberta Infant Motor Scale. Rev Paul Pediatr. 2013;31:350---8.
30.Valentini NC, Saccani R. Escala Motora Infantil de Alberta: validac¸ão para uma populac¸ão gaúcha. Rev Paul Pediatr. 2011;29:231---8.
31.Formiga CK, Cezar ME, Linhares MB. Avaliac¸ão longitudinal do desenvolvimento motor e da habilidade de sentar em crianc¸as nascidas prematuras. Fisioter Pesqui (São Paulo). 2010;17:102---7.
32.Manacero S, Nunes ML. Evaluation of motor performance of preterm newborns during the first months of life using the Alberta Infant Motor Scale (AIMS). J Pediatr (Rio J). 2008;84:53---9.
33.WangLY,WangYL,WangST,HuangCC.UsingtheAlbertaInfant Motor Scale to early identify very low-birth-weight infants withcysticperiventricular leukomalacia.BrainDev.2013;35: 32---7.
34.MaiaPC,SilvaLP,OliveiraMM,CardosoMV.Motordevelopment ofpretermand terminfants---usingtheAlbertaInfantMotor Scale.ActaPaulEnferm.2011;24:670---5.
35.SouzaES,MagalhãesLC.Desenvolvimentomotorefuncionalem crianc¸as nascidaspré-termoeatermo:influência defatores de risco biológico e ambiental. Rev Paul Pediatr. 2012;30: 462---70.
36.PrinsSA,vonLindernJS,vanDijkS,VersteeghFG.Motor devel-opmentofprematureinfantsbornbetween32and34weeks. IntJPediatr.2010,2010.pii:462048.
37.deCastroAG,LimaMdeC,deAquinoRR,EickmannSH.Sensory oralmotorandglobalmotordevelopmentofpreterminfants. ProFono.2007;19:29---38.
38.Formiga KM, Vieira ME, Linhares MB. Avaliac¸ão do desen-volvimentodebebêsnascidospré-termo:acomparac¸ãoentre idadecronológica e corrigida. J Hum Growth Dev. 2015;25: 230---6.
39.WestrupB. Newborn Individualized Developmental Careand AssessmentProgram(NIDCAP)---family-centered developmen-tallysupportivecare.EarlyHumDev.2007;83:443---9.
40.StoinskaB,GadzinowskiJ.Neurologicalanddevelopmental dis-abilitiesin ELBW and VLBW: follow-up at 2 years of age. J Perinatol.2011;31:137---42.