www.jped.com.br
ORIGINAL
ARTICLE
Maple
syrup
urine
disease
in
Brazil:
a
panorama
of
the
last
two
decades
夽
,
夽夽
Silvani
Herber
a,
Ida
Vanessa
D.
Schwartz
b,c,d,e,f,∗,
Tatiéle
Nalin
c,f,
Cristina
Brinkmann
Oliveira
Netto
b,
José
Simon
Camelo
Junior
f,g,
Mara
Lúcia
Santos
f,h,
Erlane
Marques
Ribeiro
f,i,j,
Lavinia
Schüler-Faccini
a,b,c,e,j,
Carolina
Fischinger
Moura
de
Souza
b,faPostgraduatePrograminPediatricsandAdolescentHealth,UniversidadeFederaldoRioGrandedoSul(UFRGS),PortoAlegre,
RS,Brazil
bMedicalGeneticsService,HospitaldeClínicasdePortoAlegre,PortoAlegre,RS,Brazil
cPostgraduatePrograminGeneticsandMolecularBiology,UniversidadeFederaldoRioGrandedoSul(UFRGS),PortoAlegre,RS,
Brazil
dBRAINLaboratory,HospitaldeClínicasdePortoAlegre,PortoAlegre,RS,Brazil
eDepartmentofGeneticsandMolecularBiology,UniversidadeFederaldoRioGrandedoSul(UFRGS),PortoAlegre,RS,Brazil fBrazilianMSUDNetwork,PortoAlegre,RS,Brazil
gDepartmentofPediatrics,SchoolofMedicineofRibeirãoPreto,RibeirãoPreto,SP,Brazil hHospitalPequenoPríncipe,Curitiba,PR,Brazil
iHospitalInfantilAlbertSabin,Fortaleza,CE,Brazil
jInstitutoNacionaldeGenéticaMédicaPopulacional(INAGEMP),PortoAlegre,RS,Brazil
Received2April2014;accepted29August2014 Availableonline12December2014
KEYWORDS
Maplesyrupurine disease;
MSUD;
Inbornerrorsof metabolism; Diagnosis
Abstract
Objective: TocharacterizeasampleofBrazilianpatientswithmaplesyrupurinedisease(MSUD)
diagnosedbetween1992and2011.
Methods: In thisretrospective study,patients were identifiedthrough anational reference
laboratoryforthediagnosisofMSUDandthroughcontactwithothermedicalgeneticsservices
acrossBrazil.Datawerecollectedbymeansofachartreview.
Results: Eighty-threepatientsfrom75familieswereenrolledinthestudy(medianage,3years;
interquartilerange[IQR],0.57---7).Medianageatonsetofsymptomswas10days(IQR5---30),
whereasmedianageatdiagnosiswas60days(IQR29---240,p=0.001).Onlythree(3.6%)patients
werediagnosedbeforetheonsetofclinicalmanifestations.Acomparisonbetweenpatientswith
夽 Pleasecitethisarticleas:HerberS,SchwartzIV,NalinT,NettoCB,JuniorJS,SantosML,etal.MaplesyrupurinediseaseinBrazil:a
panoramaofthelasttwodecades.JPediatr(RioJ).2015;91:292---8.
夽夽
StudyconductedatUniversidadeFederaldoRioGrandedoSul(UFRGS),PortoAlegre,RS,Brazil.
∗Correspondingauthor.
E-mail:ischwartz@hcpa.ufrgs.br(I.V.D.Schwartz). http://dx.doi.org/10.1016/j.jped.2014.08.010
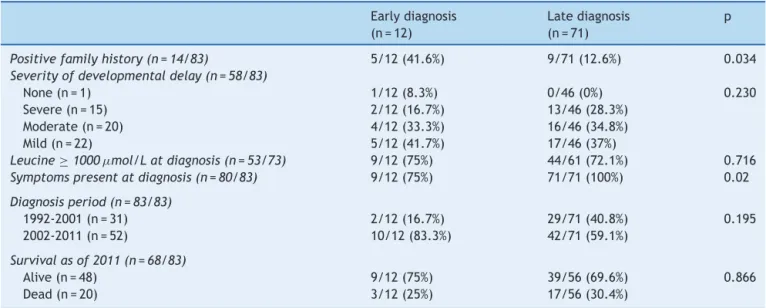
(n=12)andwithout(n=71)anearlydiagnosisshows thatearlydiagnosis isassociatedwith
thepresenceofpositivefamilyhistoryanddecreasedprevalenceofclinicalmanifestationsat
thetimeofdiagnosis,butnotwithabetteroutcome.Overall,98.8%ofpatientshavesome
psychomotororneurodevelopmentaldelay.
Conclusion: InBrazil,patientswithMSUDareusuallydiagnosedlateandexhibitneurological
involvementandpoorsurvivalevenwithearlydiagnosis.Wesuggestthatspecificpublicpolicies
fordiagnosisandtreatmentofMSUDshouldbedevelopedandimplementedinthecountry.
©2014SociedadeBrasileiradePediatria.PublishedbyElsevierEditoraLtda.Allrightsreserved.
PALAVRAS-CHAVE
Doenc¸adaurinade xaropedebordo; DXB;
Errosinatosdo metabolismo; Diagnóstico
Doenc¸adaurinadexaropedebordonoBrasil:umpanoramadasúltimasduasdécadas
Resumo
Objetivo: Caracterizarumaamostradepacientesbrasileiroscomadoenc¸adaurinadexarope
debordo(DXB)diagnosticadosentre1992e2011.
Métodos: Nesteestudoretrospectivo,ospacientesforamidentificadospormeiodeum
labo-ratóriodereferêncianacionalparaodiagnóstico deDXBepormeiodocontatocomoutros
servic¸osdegenéticamédicanoBrasil.Osdadosforamcoletadospormeiodeumarevisãode
prontuários.
Resultados: 83pacientesde75famíliasforamincluídosnoestudo(idademédia:3anos;
inter-valointerquartil(IQR):0,57-7).Aidademédianosurgimentodossintomaserade10dias(IQR:
5-30),aopassoqueaidademédianodiagnósticoerade60dias(IQR:29-240;p=0,001).Somente
três(3,6%)pacientesforamdiagnosticadosantesdosurgimentodemanifestac¸õesclínicas.Uma
comparac¸ãoentrepacientescom(n=12) esem(n=71)um diagnóstico precocemostraque
odiagnósticoprecoceestáassociadoàpresenc¸adehistóricofamiliarpositivoeàreduc¸ãona
prevalênciademanifestac¸õesclínicasnomomentododiagnóstico,porémsemmelhorresultado.
Emgeral,98,8%dospacientestêmalgumatrasonodesenvolvimentopsicomotorouneurológico.
Conclusão: NoBrasil, ospacientescomDXBnormalmenterecebemum diagnóstico tardioe
exibemumenvolvimentoneurológicoebaixasobrevivência,mesmocomumdiagnóstico
pre-coce.SugerimosquepolíticaspúblicasespecíficasparaodiagnósticoetratamentodaDXBsejam
desenvolvidaseimplementadasnopaís.
©2014SociedadeBrasileiradePediatria.PublicadoporElsevierEditoraLtda.Todososdireitos
reservados.
Introduction
Maple syrup urine disease (MSUD) is an autosomal reces-sive genetic disorder caused by deficient activity of the branched-chain alpha-keto acid dehydrogenase complex (BCKDC). Deficiencyofthis enzymecomplexleads tohigh levels of the branched-chain aminoacids (BCAA) leucine, valine, and isoleucine. Leucine and its keto analog 2-oxoisocaproic acid are particularly toxic to the central nervous system (CNS). Although the incidence of MSUD worldwideisusuallyestimatedasbeing1:185,000newborns (NB),1dataretrievedfromnewbornscreeningsuggest this
ratecanbehigher;inGermany,forinstance,theincidence isestimatedat1:133,000NB,2andinsomeMennoniteand
PennsylvaniaDutchcommunitiesintheUnitedStates,itmay beashighas1in200livebirths.3
Neonatal screening by tandem mass spectrometry
(MS/MS), also known as expanded newborn screening,
enablesdiagnosisofMSUDwhile thepatientisstill asymp-tomatic, as well as early treatment onset---two essential factorsinimprovingtheclinical course.3Beforethe
intro-duction of expanded newborn screening, the severe form
(classical MSUD) was believed to account for 75-80% of
cases,4butrecentdatasuggestthemilderformsofMSUDcan
accountforupto50%ofdiagnosedcases.5Intheclassical
form,symptomsfirstoccurbetweenthe4thand7thdayof life,andoftenincluderespiratorychanges,encephalopathy, a characteristic odor, seizures, and coma.6 In the acute
phase,prompt,aggressivetreatmenttoreduceleucine lev-elsisrequired,whichshouldconsistofahigh-rateglucose infusiontostimulateinsulinsecretionandsuppressprotein catabolism.Ifthisfails,invasiveinterventionssuchas per-itonealdialysis, hemodiafiltrationor hemodialysis maybe required.Duringthemaintenancephase,treatmentusually consists of dietary BCAA restriction and supplementation withthiamine and a BCAA-free formula,6---8 although liver
transplantationisagoodalternative.9---11
The Brazilian Public Newborn Screening Program was
implemented in 2001 and does not include screening for
MSUD.TheBCAA-free formula,a high-costproduct,isnot providedbythepublicBrazilianUnifiedHealthSystem
(Sis-tema Único de Saúde, SUS).Furthermore, the laboratory
networkaimingtoimprovelivertransplantationconditions forpatientswithmetabolicdisorders.Finally,thereareno dataontheprevalenceofthisdiseaseinBrazil.
Theobjectiveofthisstudywastooutlinetheprofileof BrazilianpatientswithMSUDfrom1992to2011soasto con-tributeto the consolidationof specific publicpolicies for MSUDinthecountry.
Methods
This retrospective, multicenter, longitudinal study was approvedbythelocalInstitutionalReviewBoard.
PatientswereidentifiedfromtherecordsoftheInborn Errors of Metabolism Laboratory of the Medical Genetics Service,auniversity-basedservicethatservesasa nation-wide referral center for the diagnosis and treatment of inborn errorsof metabolism,and fromtherecordsof the InbornErrorsofMetabolismHotline(Servic¸odeInformac¸ões sobre Erros Inatos do Metabolismo - SIEM) run by the sameMedicalGenetics Service.12 This laboratory probably
accounts for most MSUD diagnoses made in the country;
thenecessaryworkupisprovidedatnocosttothepatient or referring physician,and is usuallycovered by research
funding. Quantitation of BCAAs by high-performance
liq-uidchromatography(HPLC)andurineorganicacidanalysis havebeenavailableatthelaboratorysince1994;automatic aminoacidanalysisandMS/MSarealsocurrentlyavailable, but alloisoleucine detection is no longer performed. The SIEMis a toll-free telephonehotline, establishedin 2001, that providesinformationto physicians and other health-careproviders involved in thediagnosis and treatment of patientswithsuspectedorconfirmedIEMs.
To be included in the study,a patient should present:
1) a significant increase in blood BCAA levels, on more
thanonemeasurement,asdeterminedbyagold-standard
method(HPLC-basedBCAAquantitationorautomaticamino
acidanalyzerorMS/MS);and2)abiochemicallyconfirmed diagnosisofMSUD,establishedbetween1992and2011.
Datacollectionformswerefilledoutforeachpatientby theirattendingphysicianoroneofthestudyinvestigatorsby meansofareviewofavailablepatientrecordsandcharts. Fordeceasedpatients,thedateofthelastavailablerecord wasconsideredthedateofstudyenrollment.
Definitionofstudyvariables
Diagnosiswasconsidered‘‘early’’if thepatienthadbeen diagnosedbeforethe15thdayoflife.Thedurationof dis-easeuntildiagnosiswasdefinedasthetimeelapsedbetween the onset of clinical manifestations and the biochemical diagnosis of MSUD. Presence andseverity of psychomotor andneurodevelopmentaldelaywereassessedonthebasis oftheimpressionsofeachpatient’sattendingneurologistor pediatrician.MSUDwasclassifiedintovariantsaccordingto thecriteriausuallycitedintheliterature.1
Statisticalanalysis
All statistical analyses were carried out in the Statisti-cal Package for the Social Sciences (SPSS®, Statistics for
Windows,Chicago,USA)18.0softwareenvironment. Varia-bleswereonlytakenintoaccountforanalysisifdatawere availableforatleast60%ofthesample.
Fordescriptiveanalysis,datawereexpressedasabsolute andrelativefrequencies.Asymmetricallydistributed contin-uousvariableswereexpressedasmediansandinterquartile ranges. The chi-square test and Fisher’s exact test were usedtodetermine associationsbetweencategorical varia-bles. The Kruskal---Wallis and Mann---WhitneyU tests were usedtocomparethe mediansofdifferentcharacteristics. Thesignificancelevelwassetat5%.
Results
Onehundredandnineteenpatientswithclinicalor labora-tory evidence ofMSUD (‘‘potentialMSUD’’patients) were identified,83ofwhommettheinclusioncriteria.Ofthese, 48werealiveat thetimeofthestudy,20diedbeforethe startofthestudy,and15lackedinformationregarding sur-vival.
The patients enrolled in the study came from all five regionsofBrazil.The medianageat inclusionwas3years (IQR 0.57---7.00 years;range,30 days---23 years).Forty-six (55.4%)weremale,75(90.4%)wereunrelatedand14(18.7%) hadafamilyhistoryofMSUD.Consanguinitywasreportedin 17families(22.7%).
Diagnosis
Themedianageatdiagnosiswas60days(IQR29---240days; range,7days---10years).Themedianleucinelevelat diag-nosis was1,693mol/L (IQR965---2,836mol/L; reference
range,80---200mol/L).
Eighty patients (96.4%) had clinical manifestations of MSUD at the time of diagnosis (median age at symptom onset,10days;IQR5---30days;range,1day---2years).The most common manifestations were seizures (51.2%) and hypoactivity (50%). Other presenting symptoms included poor feeding, poor sucking and changes in respiratory pattern (48.7% each), hypotonia (48.2%), characteristic odor(42.5%),lethargy(41.2%),metabolicacidosis(31.2%), vomiting(30.0%),andencephalopathy(20.0%).The charac-teristicodorofMSUDwasreportedbyhealthcareproviders as a strong, ‘‘soy sauce-like,’’ ‘‘caramel-like,’’ or sweet scent,which wasmost detectablein patientshospitalized due to metabolic decompensation. There was a statisti-callysignificantdifferencebetweenmedianageatsymptom onsetandmedianageatdiagnosis(p=0.001).
Fig. 1 shows the distribution of the number of
diag-noses per year, revealing an upward trend in diagnoses
over the course of the study period. However,
compari-sonofmedianageatdiagnosisbetween1992and2001(90 days;IQR36---270; n=31)and between2002 and2011 (53 days;IQR20---202;n=52)revealednostatisticallysignificant
difference (p=0.053). The median timeelapsed between
symptomonsetanddiagnosiswas60days(IQR28---240)over thefirstdecadeofthestudyand37days(IQR9---180)during theseconddecade(p=0.075).ConsideringallMSUDpatients whowerealiveasof2011(n=48),13hadbeen diagnosed
1992 1 2 3 4 5 6 7 8 9
1997 2001 2002
Year SIEM
Number of diagnosis
2007 2011
Figure1 NumberofMSUDdiagnosesinBrazilandtrendline,1992-2011.
SIEMisatoll-freetelephonehotline,establishedin2001,thatprovidesinformationtophysiciansandotherhealthcareproviders
involvedinthediagnosisandtreatmentofpatientswithsuspectedorconfirmedIEMs.
Table1 InfluenceofearlydiagnosisonthecourseofMSUDa.
Earlydiagnosis
(n=12)
Latediagnosis
(n=71)
p
Positivefamilyhistory(n=14/83) 5/12(41.6%) 9/71(12.6%) 0.034
Severityofdevelopmentaldelay(n=58/83)
None(n=1) 1/12(8.3%) 0/46(0%) 0.230
Severe(n=15) 2/12(16.7%) 13/46(28.3%)
Moderate(n=20) 4/12(33.3%) 16/46(34.8%)
Mild(n=22) 5/12(41.7%) 17/46(37%)
Leucine≥1000mol/Latdiagnosis(n=53/73) 9/12(75%) 44/61(72.1%) 0.716
Symptomspresentatdiagnosis(n=80/83) 9/12(75%) 71/71(100%) 0.02
Diagnosisperiod(n=83/83)
1992-2001(n=31) 2/12(16.7%) 29/71(40.8%) 0.195
2002-2011(n=52) 10/12(83.3%) 42/71(59.1%)
Survivalasof2011(n=68/83)
Alive(n=48) 9/12(75%) 39/56(69.6%) 0.866
Dead(n=20) 3/12(25%) 17/56(30.4%)
a Earlydiagnosis:diagnosisofMSUDmadebeforethe15thdayoflife.
Only 12patients hadbeen diagnosed early.Inthreeof thesecases,diagnosiswasmadebeforesymptomonsetas a resultof neonatal screening at a private laboratory; at the time of writing, one of these patients is 4 years old andhasnormalneurologicalandpsychomotordevelopment, andtheothertwopatients,aged1yearand6years,have mild and moderate psychomotor and neurodevelopmental delaysrespectively.Table1presentsacomparisonbetween patientswithandwithoutanearlydiagnosisofMSUD.
Clinicalmanifestations
The most common clinical manifestations at the time of patient enrollment were psychomotor and
neurodevelopmental delay (98.8%) and poor nutritional status(74.7%).Twopatientswereoverweight.
Medianageatdiagnosiswasnotsignificantlyassociated withseverityof developmentaldelay (n=58/83;p=0.31), norwereelevatedleucinelevels(n=57/73;p=0.961).
intermediate/intermittentformswerealiveatthetimeof writing.
Treatment
Fifty-eight (69.9%) patients were being managed by neu-rologists,56 (67.5%)bymedicalgeneticists,49(59.0%)by pediatricians,and46(55.4%)bydietitians.Other profession-alsinvolvedinpatientmanagementandfollow-upincluded neonatologists,gastroenterologists,physiciannutrition spe-cialists, speech and language pathologists, and physical therapists.
Thepatientsinoursamplereceivedfollow-upat16 treat-mentcenters,withamedianoffivepatientspercenter(IQR 1.75---6.5).Useofan MSUD-specificmetabolicformulawas reportedin 62of 73 patients(74.7%). Three patientshad undergone liver transplantation; in two cases,the proce-durewasperformedinBrazil.Thirty-sevenpatients(59.7%) received the metabolic formula regularly(median age, 5 years;IQR1-7.5years);thosewhoreportedfailuresin for-mulasupply had a median age of 2 years (IQR0.5-5.00). Mediantimeelapsedbetweendiagnosis andreceiptofthe formula was17.5 days (IQR5.75---30 days).There was no significant association between severity of developmental delayandregularityofformulasupply(n=40/62,p=0.074).
Deaths
Of the patients for whom data were available (n=68), 20----allwithclassicMSUD----diedbeforethestartofthestudy. Medianage at death was225 days (IQR127.5---365 days). There wasno statistically significant correlation between fataloutcomeandleucinelevelsatdiagnosis(p=0.568).
Discussion
Tothebestofourknowledge,thisisthefirststudytooutline aprofileofBrazilianpatientswithMSUD.Thecurrent Brazil-ianpopulationisestimatedat190,732,694,with2,944,928 live births occurring per year.13 Therefore, considering a
meanincidence of MSUD of 1:100,000 in the country, we
wouldexpectapproximately300newdiagnosesofthe dis-ease over a 10-year period----a muchlower estimate than thesampleactuallyincludedinthestudy.Thissuggeststhat MSUDisunderdiagnosedinthecountry.
MSUD meetsmost of the Wilsonand Jungner14 criteria
for screening:for instance, thereis a recognizablelatent orearlysymptomaticstageandanacceptedtreatmentfor patientswithrecognizeddisease.IncountrieswhereMSUD isincludedinneonatalscreening,patientsareusually diag-nosedbeforethe10thdayoflife.3,4Conversely,incountries
whereMSUDisnotincludedinpublicneonatalscreening pro-grams,suchasBrazil,diagnosisisusuallydelayed,occurring at agessimilartothose reportedfor our sample.15,16 The
predominanceofclassicMSUDandsymptomaticpatientsin oursamplecouldbealsoduetothenon-inclusionofMSUD inthepublicneonatalscreeningprogram,astheliterature suggeststhatnewbornscreeningenablesearlierdiagnosisof milderformsofthecondition.5
Asexpected,patientswithapositivefamilyhistorywere testedearlierthanpatientswithnofamilyhistoryofMSUD; thiswasprobablyduetogeneticcounselingoffamilieswho hadalreadyhadonechildwiththeconditionandwerethus awareoftheriskofrecurrenceandtheneedforearly inves-tigation.
OurstudyfoundanupwardtrendinthenumberofMSUD diagnosesover thepastdecade, whichcoincidedwiththe establishment oftheSIEMhotlineandtheimplementation ofapublicneonatalscreeningprogrambytheBrazilian Min-istryofHealth.17Thereasonsbehindthistrendareunknown,
butitmayreflectgreaterawareness ofIEMsingeneralby healthcare providers,aswellasgreater awarenessofthe earlyclinicalmanifestationsoftheseconditions. Neverthe-less,theincreasewasnotstatisticallysignificant,andthere wasnosignificantdifferenceinageatdiagnosisbetweenthe twoperiods,whichcorroboratesourbeliefthatasubstantial portionofMSUDpatientscontinue todieundiagnosedand untreatedinBrazil.AsimilarsituationisseeninMalaysia, wherenewbornscreeningdoesnotincludeMSUD:the diag-nosis is oftenlate andMSUDappears tobeless prevalent thanexpected.18
Psychomotor and neurodevelopmental delays were
detectedinpracticallyallpatientsinthesample.Justover halfof patientswhoreceivedtheMSUD-specificmetabolic formulareportedthat theformulawassupplied regularly.
However, most patients exhibited inadequate nutritional
status.ItbearsstressingthatMSUDpatientsshouldalways be followed by nutritional care providers, and only half
of the patients in our sample had the support of a
reg-istered dietitian.19 Most patients who received metabolic
formula,however, weremonitored bydietitians (datanot
shown). Neurologists were the professionals most often
responsibleforpatientfollow-up,whichmaybesecondary
to the high frequency of developmental delay in this
sample.
In Brazil, time between diagnosis and receipt of the metabolicformulaislongandvariable.Whenpatientswere diagnosedintheacutestageofthedisease,duringa hospi-talstayduetometabolicdecompensation,theywerelikely tobestartedonmetabolicformulaonthedateof diagno-sis(iftheformulaisavailableatthehospitalofadmission, of course). Conversely, patients whowere diagnosed at a
non-acute stage of the disease and treated on an
outpa-tient basis were likely to receive the formula only much later; infact, thesepatients usuallysecure access tothe metabolicformulathroughlitigation.Again,itbears stress-ing that use of the BCAA-free formula is essential, as it ensures theamount ofproteinrequiredfor propergrowth anddevelopment.1Recently,studieshavebeen conducted
inratswithnewlyinducedclassicalandintermediateMSUD toassesstheconsequencesofrapidBCAAbuildupandassess potentialtreatmentoptions,suchasnorleucine.20
Leucine levels at diagnosis were high, with a median
value of 1,693mol/L. Leucine levels in excess of
1,000mol/Lareconsideredcritical,astheymayproduce irreversible damage or even death.3,21,22 However, there
Inthisstudy,theadvantageofearlydiagnosisappearsto havebeenlostduetoalackofshort-andlong-termclinical management.AsreportedforFilipinopatients,15noclinical
protocolformanagementofacute-stageMSUDisavailable inBrazil,andpatientsdonotreceivethemetabolicformula reliably.Conversely,inastudyby Mortonetal.4inwhich
patientshadaccesstotheformulaanda clinicalprotocol wasfollowedintheacutestageofthedisease,theoverall
outcomewasbetterandpatientsachievedmoreadequate
development.
In light of the recent adoption of a specific public
policy for diagnosis and management of rare diseases in
Brazil,23,24 wesuggest thefollowing stepsshouldbetaken
to further improve the quality of life of MSUD patients
in the country: a) expand the public newborn screening
program to include MSUD amongthe identified disorders;
b) develop the ability to conduct alloisoleucine testing locally; c)make thespecific metabolicformulas available toallpatients,withouttheneedfor legalintervention;d) establishanationalcenterspecializinginliver transplanta-tionformetabolicdisorders;ande)establishanetworkof multidisciplinary teams comprising physicians, nurses and dietitians specialized in the treatment of inborn errors
of metabolism to develop national protocols for MSUD
management.Thecreationof theBrazilianMSUDNetwork
(http://redexaropedobordo.com.br/), established in 2010
topromoteeducationonthediagnosisandmanagementof
MSUDandsupportedbyaBrazilianresearchagencyandby theMinistry of ScienceandTechnology, isone ofthe first stepstowardthisgoal.
Funding
This study was supported by the Brazilian Coordination for Improvement of Higher Education Personnel (CAPES), Fundo de Incentivo à Pesquisa e Eventos (FIPE-HCPA) and theBrazilian National Councilof Scientificand Technolog-ical Development (CNPq)---grant no. MCT/CNPq/CT-SAÚDE 57/2010.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
Acknowledgments
Theauthorswouldliketothanktheprofessionalsfromthe Brazilian MSUDNetwork whocontributedtothispaper,as wellasthestaffoftheMedicalGeneticsServiceatHospital deClínicasdePortoAlegre,Brazil,especiallythose profes-sionalsinvolvedinthebiochemicalanalysisofpatientswith suspectedmetabolicdisorders.
References
1.ChuangD,ShihV.Disordersofbranched-chainaminoacidand ketoacidmetabolism.In:ScriverC,BeaudetA,SlyW,ValleD, editors.Themetabolicandmolecularbasisofinheriteddisease. 7thed.NewYork:McGraw-Hill;2001.p.1971---95.
2.FingerhutR.RecallrateandpositivepredictivevalueofMSUD screeningis notinfluencedbyhydroxyproline. EurJPediatr. 2009;168:599---604.
3.Simon E, Fingerhut R, Baumkötter J, Konstantopoulou V, RatschmannR,WendelU.Maplesyrupurinedisease:favourable effectofearlydiagnosisbynewbornscreeningontheneonatal courseofthedisease.JInheritMetabDis.2006;29:532---7.
4.MortonDH,StraussKA,RobinsonDL,PuffenbergerEG,Kelley RI.Diagnosisandtreatmentofmaplesyrupdisease:astudyof 36patients.Pediatrics.2002;109:999---1008.
5.Fingerhut R, Simon E, Maier EM, Hennermann JB, Wendel U. Maple syrup urine disease: newborn screening fails to discriminate between classic and variant forms. Clin Chem. 2008;54:1739---41.
6.Saudubray J, Charpentier C. Clinical phenotypes: Diagno-sis/algorithms. In: Scriver CR, Beaudet AL, Sly WS, ValleD, editors.Themetabolicand molecular basesofinherited dis-eases.NewYork:McGraw-Hill;1995.p.327---400.
7.JouvetP,Jugie M,Rabier D,DesgrèsJ, HubertP,Saudubray JM,etal.Combinednutritionalsupportandcontinuous extra-corporeal removal therapy in the severe acute phase of maple syrup urine disease. Intensive Care Med. 2001;27: 1798---806.
8.StraussKA,WardleyB,RobinsonD,HendricksonC,RiderNL, Puffenberger EG, et al. Classical maple syrupurine disease andbraindevelopment:principlesofmanagementandformula design.MolGenetMetab.2010;99:333---45.
9.FeierFH,MiuraIK,FonsecaEA,PortaG,PuglieseR,PortaA, etal. Successfuldomino livertransplantationinmaplesyrup urinediseaseusingarelatedlivingdonor.BrazJMedBiolRes. 2014;47:522---6.
10.Mazariegos GV, Morton DH, Sindhi R, Soltys K, Nayyar N, BondG,etal.Liver transplantationfor classicalmaplesyrup urinedisease:long-termfollow-upin37patientsand compar-ativeUnitedNetworkforOrganSharingexperience.JPediatr. 2012;160:116---21,e1.
11.Serra JD, Sánchez FA, Visus FS. Enfermidades de orina de jarabearce.In: SanjurjoP,BaldellouA, editors.Diagnóstico ytratamientodelasenfermedadesmetabólicashereditarias. 3aed.Madrid:EdicionesErgon;2010.p.487---98.
12.BrustolinS,SouzaC,PugaAC,RefoscoL,PiresR,PeresR,etal. AssessmentofapioneermetabolicinformationserviceinBrazil. CommunityGenet.2006;9:127---32.
13.Brasil.MinistériodoPlanejamento,Orc¸amentoeGestão.
Insti-tuto Brasileiro de Geografia e Estatística (IBGE). Contagem
Populacional.Brasi´lia:MinistériodoPlanejamento,Orc¸amento
eGestão;2010.
14.WilsonJ,JungnerG. Principlesand practiceofscreeningfor disease.Geneva:WorldHealthOrganization;1968.
15.LeeJY,ChiongMA,EstradaSC,Cutiongco-DelaPazEM,SilaoCL, PadillaCD.Maplesyrupurinedisease(MSUD)–clinicalprofileof 47Filipinopatients.JInheritMetabDis.2008;31:S281---5.
16.PangkanonS,CharoensiriwatanaW,SangtawesinV.Maplesyrup urine disease in Thai infants. J Med Assoc Thai. 2008;91: S41---4.
17.Brasil.MinistériodaSaúde.PortariaGM/MSn◦822/GMde06de
junhode2001.Brasília:MinistériodaSaúde;2001.
18.YunusZM,KamaludinDA,MamatM,ChoyYS,NguL.Clinicaland biochemicalprofilesofmaplesyrupurinediseaseinMalaysian children.JIMDRep.2012;5:99---107.
19.ValadaresEG,GiannettiJG,RefoscoLF,SilvaLC,OliveiraRB, PiresRF. Leucinose: doenc¸a doxaropede bordo.In: Martins AM,FrangipaniBJ,NichelettiC,OliveiraRB,editors.Protocolo brasileirode dietas:errosinatosdo metabolismo.São Paulo: SegmentoFarma;2006.p.53---8.
21.Heldt K, Schwahn B, Marquardt I, Grotzke M, Wendel U. Diagnosis of MSUD by newborn screening allows early inter-ventionwithout extraneousdetoxification.Mol GenetMetab. 2005;84:313---6.
22.HoffmannB,HelblingC,SchadewaldtP,WendelU.Impactof longitudinalplasmaleucinelevelsontheintellectualoutcome inpatientswithclassicMSUD.PediatrRes.2006;59:17---20.
23.Brasil.MinistériodaSaúde.Portarian.◦199,de30dejaneiro
de2014.Brasília:MinistériodaSaúde;2014.