REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
OfficialPublicationoftheBrazilianSocietyofAnesthesiologywww.sba.com.br
SCIENTIFIC
ARTICLE
Frequency
of
colonization
and
isolated
bacteria
from
the
tip
of
epidural
catheter
implanted
for
postoperative
analgesia
夽
Débora
Miranda
Diogo
Stabille
a,∗,
Augusto
Diogo
Filho
b,c,d,e,
Beatriz
Lemos
da
Silva
Mandim
f,
Lúcio
Borges
de
Araújo
g,
Priscila
Miranda
Diogo
Mesquita
a,
Miguel
Tanús
Jorge
b,haHealthSciences(HS),UniversidadeFederaldeUberlândia(UFU),Uberlândia,MG,Brazil
bPostgraduateProgram,CiênciasdaSaúde(CS),UniversidadeFederaldeUberlândia(UFU),Uberlândia,MG,Brazil cColégioBrasileirodeCirurgiões,RiodeJaneiro,RJ,Brazil
dColégioBrasileirodeCirurgiaDigestiva,SãoPaulo,SP,Brazil
eDepartmentofSurgery,FaculdadedeMedicina,UniversidadeFederaldeUberlândia(UFU),Uberlândia,MG,Brazil fDepartmentofAnesthesiology,HospitaldeClínicas,UniversidadeFederaldeUberlândia(UFU),Uberlândia,MG,Brazil gFaculdadedeMatemáticadaUniversidadeFederaldeUberlândia(UFU),Uberlândia,MG,Brazil
hDepartmentofClinicalMedicine,FaculdadedeMedicinadaUniversidadeFederaldeUberlândia(UFU),Uberlândia,MG,Brazil
Received20March2014;accepted6May2014
Availableonline30March2015
KEYWORDS
Epiduralanesthesia; Infection;
Bacteria
Abstract
Backgroundandobjective: Theincreaseduseofepiduralanalgesiawithcatheterleadstothe need to demonstrate the safety ofthis method and know the incidenceof catheter colo-nization,insertedpostoperativelyforepiduralanalgesia,andthebacteriaresponsibleforthis colonization.
Methods:From November2011 toApril 2012, patients electivelyoperated and maintained under epidural catheter for postoperative analgesia were evaluated. The catheter tip was collectedforsemiquantitativeandqualitativemicrobiologicalanalysis.
Results:Of68culturedcatheters,sixtips(8.8%)hadpositivecultures.Nopatienthad super-ficialordeepinfection.Themeandurationofcatheterusewas43.45h(18---118)(p=0.0894). Thetypeofsurgery(contaminatedoruncontaminated),physicalstatusofpatients,and sur-gical time showed no relation with the colonization of catheters. Microorganisms isolated fromthecathetertipwereStaphylococcusaureus,PseudomonasaeruginosaandSphingomonas paucimobilis.
夽
StudyconductedatHospitaldeClínicasdaUniversidadeFederaldeUberlândia,Uberlândia,MG,Brazil.
∗Correspondingauthor.
E-mail:deboramdiogo@yahoo.com.br(D.M.D.Stabille). http://dx.doi.org/10.1016/j.bjane.2014.05.015
Conclusion: Postoperativeepiduralcatheteranalgesia,underthesestudyconditions,wasfound tobelowriskforbacterialcolonizationinpatientsatsurgicalwards.
© 2014SociedadeBrasileirade Anestesiologia.Publishedby ElsevierEditoraLtda.Allrights reserved.
PALAVRAS-CHAVE
Anestesiaepidural; Infecc¸ão;
Bactérias
Frequênciadecolonizac¸ãoebactériasisoladasdepontadecateterdeperidural implantadoparaanalgesiapós-operatória
Resumo
Objetivos: Oaumento do uso deanalgesia pela via periduralcom uso de cateteresleva à necessidadedesedemonstraraseguranc¸adométodo.Opresenteestudotevecomoobjetivo conheceraincidênciadecolonizac¸ãodecateteresinseridosparaanalgesiaperiduralno pós-operatórioeasbactériasresponsáveisporestascolonizac¸ões.
Métodos: Noperíododenovembrode2011aabrilde2012foramavaliadospacientes opera-doseletivamentemantidossobanalgesiaporcateterperiduralnopós-operatório.Apontado cateterfoicoletadaparaanálisemicrobiológicasemi-quantitativaequalitativa.
Resultados: Seis(8,8%) pontasdos 68 cateterescultivadosapresentaram culturaspositivas. Nenhumpacienteapresentouinfecc¸ãosuperficialouprofunda.Otempomédiode permanên-ciadocateterfoide43,45horas(18-118horas)(p=0,0894).Otipodecirurgia(contaminada ounão contaminada),estadofísicodospacientesetempo cirúrgiconão mostraramrelac¸ão com acolonizac¸ão doscateteres. Osmicro-organismos isolados dapontade cateter foram
Staphylococcusaureus,PseudomonasaeruginosaeSphingomonaspaucimobilis.
Conclusão:Conclui-seque,aanalgesiaporcateterperiduralnopós-operatório,nascondic¸ões dopresenteestudo,revelou-seprocedimentocombaixoriscodecolonizac¸ãobacterianaem pacientesdeenfermariascirúrgicas.
©2014SociedadeBrasileira deAnestesiologia.PublicadoporElsevierEditoraLtda.Todosos direitosreservados.
Introduction
Epiduralanesthesiahasbeenusedmainlynotonlyforpain relief,for hoursorafewdaysinsurgical patients,trauma victims,andthoseadmittedinintensivecareunits,butalso for longer periods in patients with chronic pain, such as thoseundergoingcancertreatment.1,2
Evidence shows that association of general and epidu-ralanalgesiafacilitatesearlyrecoveryandimprovespatient outcomebyreducingtheincidenceofthromboembolic, pul-monary,andgastrointestinalevents.1,3---5
Besides the advantages mentioned, the complications associated with epidural catheters include total spinal anesthesia; post-dural puncture headache; spinal cord and nerve root trauma; hematoma; and infections such as epidural abscesses, meningitis, and superficial skin infection.1,6,7 Epidural catheter colonization is defined as
the growth of at least one microorganism in quantita-tive culture regardless of the number of units forming colonywithoutlocalinflammationorinfectioninthespinal space.7
Studies of the use of epidural catheter for analge-sia have shown rates of colonization or infection of 0---28.8%.6,8---10 The incidence of infection associated with
epidural catheter ranges from 0.06% to 5.3% in studies withsurgicalpatientsandtherateofsite-specificinfections
(meningitis,paraspinalandepiduralabscess)rangesfrom0 to0.7%.1,6,10,11
Thereareseveralmechanismsbywhichepiduralcatheter causesinfection.First,infectionmayoccurby contamina-tionofthecatheteremergencesiteoritslumenandspreads alongitsduct.Thesecondmechanismisbyorganismsthat areintroducedduringpunctureorcatheterinsertion. Infec-tionmayoccurviabloodfrombloodstreamorfromadistant focalinfection.Afourthmechanismdescribedis intralumi-nalviaacontaminatedinfuser.1,12
For intravascular catheters, Maki et al. reported that cathetergrowthof morethan 15 coloniescorrelates with increased risk of infection.13 However, the quantitative
valueof theresults of epiduralcathetercultureswasnot determined.1
The vast majority of epidural catheter infections are causedbyStaphylococcusaureus(57---93%ofcases), Strep-tococcus spp. (18%), and a variety of Gram-negative bacilli (13%), but mycobacteria, fungi, and parasites may also be found in the abscesses. The microbiolog-ical spectrum of infection depends on the population studied.12,14---18
Infectionshavealwaysbeenamatterofdebatefor epidu-ralanalgesia,butstudieshavebeenlimitedtocasereports and retrospective reviews. The considerable increase in the use of analgesia delivered through epidural catheter showstheneedtodemonstrate theadvantages andsafety of this method. Although a rare event, the impactof an epidural catheter infection on a healthy patient can be harmful,botheconomicallyandbiologically;therefore,the objective of the study was to perform a prospectively andepidemiologicalanalysisofpatientsadmittedto medi-calwardsundergoingepiduralanalgesiapostoperativelyas well as discover the frequency of colonization and the microorganisms involved in short-term catheters in these patients.
Methods
Prospective and epidemiological study carried out from November 2011 to April 2012 at the Hospital de Clínicas da Universidade Federal de Uberlândia. The project was approvedbytheHumanResearchEthicsCommittee,number 280/11,andincludedallpatientsundergoingelective surgi-calprocedures, requiring postoperative epidural catheter analgesiaduringthatperiod.
All patients agreed to participate in the study and gave written informed consent. Data collection was per-formed using the anesthetic records made at the time of anesthesia and during the postoperative period at the surgical and gynecological wards. All patients were sub-jectedtoantisepsiswith70%alcoholforepiduralcatheter insertion.Patientswerefollowed-upforanalgesiaand eval-uation of the inflammatory and/or infectious aspect at the site of epidural catheter insertion, and other symp-toms that may be present during hospitalization (such as fever, paresthesia, postoperative pain). The catheter usedwasSmithsMedicalPortex,16G,withanalgesic solu-tioninfusion by infusion or intermittent pump bolus with syringe.
The data collection instrument included sociodemo-graphic records and information such as hospital stay, comorbidities,surgicalprocedure,antimicrobialsused,date of insertion and dwell time of epidural catheter, inser-tion level (thoracic or lumbar), local anesthetic used, managementcomplications,signsofinflammation(redness, discharge)attheinsertionsite.
After the epidural catheter indwelling period, con-sidered as sufficient by the anesthesiology team, the epidural catheter tip was harvested under strict aseptic and antiseptic techniques (mask, sterile gloves, and 70% alcohol).
Using sterile blades,the distal end of the catheter,at a distance of 3---4cm, was sectioned, placed in a ster-ilecontainer, andtransportedwithin2hfor cultivationin microbiologylaboratory oftheHospitaldeClínicasda Uni-versidade Federal de Uberlândia. Epidural catheter was semi-quantitativelyandqualitativelycultivated.The labo-ratoryculturemethodologyusedwasrecommendedbyMaki etal.,andcolonizationwasconsideredasasemiquantitative culturewithgrowthofmorethan15colonyformingunits, andbacterialidentificationwasperformedby theVITEK2 system.
Thecathetersweregroupedaccordingtopresence(group A) or absence (groupB) of colonization and a dwelltime shorter(group1)andequalorgreater(group2)than48h. GroupsA andBand 1---2were comparedaccording tothe surgery classification, considering uncontaminated (clean andpotentiallycontaminated)andcontaminated (contam-inated,dirtyandinfected);physical conditionofpatients, classifiedasASAI---V,accordingtotheAmericanSociety of Anesthesiologists(ASA),anddurationofthesurgical proce-dure.
Mann---Whitneynonparametrictestwasusedfor compar-ingquantitative variablesbetweengroups, andchi-square test for qualitative variables. The significance level used for thesetests was5%. Calculationswere made usingthe softwareBioEstat5.0.
Results
Seventy-fourpatients were initiallyincluded in thestudy. After excluding eight patients, one by death, two by accidentalexitofcatheter,andfivebyexternalend discon-nection,68patientswereeffectivelyassessed.Allpatients wereadmittedtogeneralsurgery(23),urology (16), proc-tology(14),thoracicsurgery(7),trauma(4),andgynecology (4)wards.
Nopatienthadanysignofinflammationattheinsertion site,epiduralabscess,CNSinfectionorsystemicinfection.
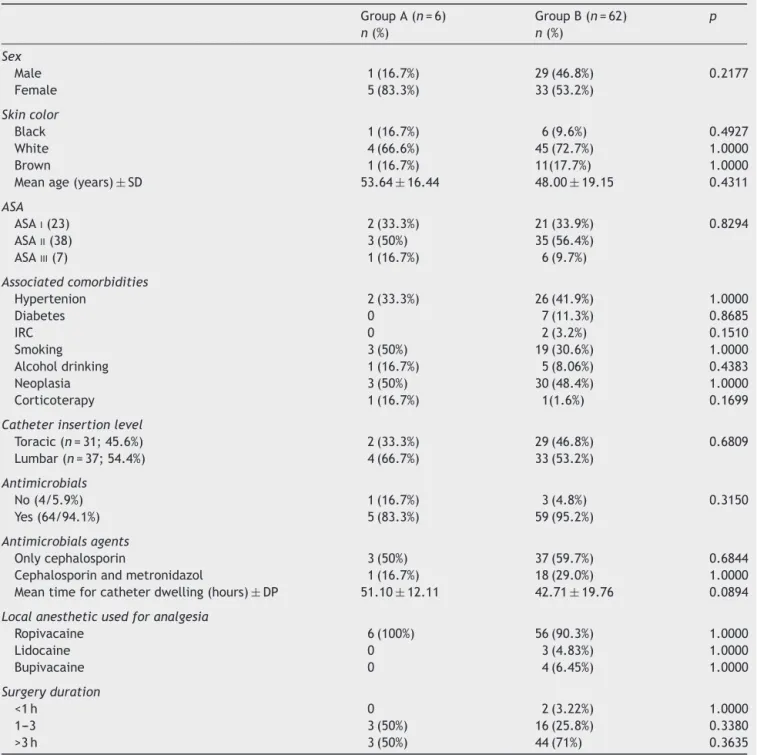
Culturewaspositiveinsixcatheters(8.8%)(groupA)and negativein 62 (91.2%)(group B). Therewasno statistical significanceinthecomparisonbetweenthetwogroups. Pro-phylacticantibioticwasusedinmorethanhalfthepatients inbothgroups.Morethanonetypeoflocalanestheticwas usedinsomepatients.Thevariablesrelatedtoeachgroup areshowninTable1.
There wasSphingomonas paucimobilis isolation of one catheter,S.aureusofanother,andP.aeruginosaofathird catheter. Three others had bacterial growthwithout pre-dominanceofsomekindofcolony,whichledtonoisolation ofanybacteria.
Themeantimeofallcatheterspermanencewas43.45h; in37patients,itwaslessthan48h(group1)andmorethan 48hin31patientsofgroup2.
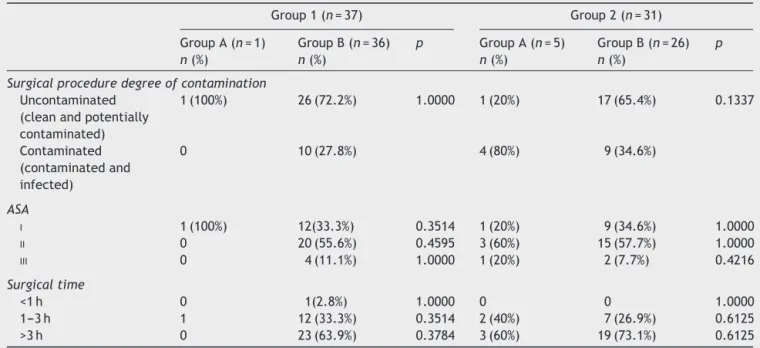
Therewasnostatisticallysignificant differencesin the comparisonofgroup1withgroup2andgroupAwithgroup regarding the degree of surgery contamination, physical conditionofpatients(ASAI,IIorIII),anddurationofsurgical procedure(Table2).
Discussion
Literature shows that conditions leading to immune
impairment (diabetes mellitus, use of corticosteroids or other immunosuppressive therapies, malignancy, alco-holism,chronicrenalfailure),spinalcordinjury (degener-ativediseases,traumainjuries,surgeryorinstrumentation) andsourcesofinfection(respiratory,urinary)areriskfactors forepiduralcathetercolonization.12,19---24
In surgical site infection, studies show that blood glu-cose levels are important in case of diabetes. Levels over 200mgdL−1 in earlypostoperative periodare
Table1 Comparisonofcolonized(groupA)andnotcolonized(groupB)cathetersaccordingtopatientcharacteristics.
GroupA(n=6)
n(%)
GroupB(n=62)
n(%)
p
Sex
Male 1(16.7%) 29(46.8%) 0.2177
Female 5(83.3%) 33(53.2%)
Skincolor
Black 1(16.7%) 6(9.6%) 0.4927
White 4(66.6%) 45(72.7%) 1.0000
Brown 1(16.7%) 11(17.7%) 1.0000
Meanage(years)±SD 53.64±16.44 48.00±19.15 0.4311
ASA
ASAI(23) 2(33.3%) 21(33.9%) 0.8294
ASAII(38) 3(50%) 35(56.4%)
ASAIII(7) 1(16.7%) 6(9.7%)
Associatedcomorbidities
Hypertenion 2(33.3%) 26(41.9%) 1.0000
Diabetes 0 7(11.3%) 0.8685
IRC 0 2(3.2%) 0.1510
Smoking 3(50%) 19(30.6%) 1.0000
Alcoholdrinking 1(16.7%) 5(8.06%) 0.4383
Neoplasia 3(50%) 30(48.4%) 1.0000
Corticoterapy 1(16.7%) 1(1.6%) 0.1699
Catheterinsertionlevel
Toracic(n=31;45.6%) 2(33.3%) 29(46.8%) 0.6809 Lumbar(n=37;54.4%) 4(66.7%) 33(53.2%)
Antimicrobials
No(4/5.9%) 1(16.7%) 3(4.8%) 0.3150
Yes(64/94.1%) 5(83.3%) 59(95.2%)
Antimicrobialsagents
Onlycephalosporin 3(50%) 37(59.7%) 0.6844
Cephalosporinandmetronidazol 1(16.7%) 18(29.0%) 1.0000 Meantimeforcatheterdwelling(hours)±DP 51.10±12.11 42.71±19.76 0.0894
Localanestheticusedforanalgesia
Ropivacaine 6(100%) 56(90.3%) 1.0000
Lidocaine 0 3(4.83%) 1.0000
Bupivacaine 0 4(6.45%) 1.0000
Surgeryduration
<1h 0 2(3.22%) 1.0000
1---3 3(50%) 16(25.8%) 0.3380
>3h 3(50%) 44(71%) 0.3635
ASA,AmericanSocietyofAnaesthesiologists;CRF,chronicrenalfailure;SD,standarddeviation. Theuseofotherantimicrobialwasnotconsideredinthecomparison.
that diabetes is the most important risk factor for the occurrence of epidural abscesses.12 Patients under
corti-costeroidsorotherimmunosuppressivedrugsmaybemore likely to develop surgical site infection25---27 and epidural
abscesses.28
Only patients classified as ASA I---III were enrolled in the study. There was no statistical significance between themregardingcolonization.Regardingsurgical site infec-tion,patientsclassifiedasASAIandIIhavezerorisk,while
patientsASAIII,IV,andVhavefavorablescorestodevelop surgicalsiteinfection.25---27
Theproximityoftheanalregionwiththecaudal epidu-ralcatheterinsertionmayfacilitateinfection.Thus,caudal epiduralanalgesia is currently used less than lumbar due tothehighriskofcontaminationbyenterobacteria.1Inour
Table2 Comparisonofepiduralcathetercolonizationanddwellingtimeregardingsurgicalproceduredegreeofcontamination, physicalstatus,andsurgicaltime.
Group1(n=37) Group2(n=31)
GroupA(n=1)
n(%)
GroupB(n=36)
n(%)
p GroupA(n=5)
n(%)
GroupB(n=26)
n(%)
p
Surgicalproceduredegreeofcontamination
Uncontaminated (cleanandpotentially contaminated)
1(100%) 26(72.2%) 1.0000 1(20%) 17(65.4%) 0.1337
Contaminated (contaminatedand infected)
0 10(27.8%) 4(80%) 9(34.6%)
ASA
I 1(100%) 12(33.3%) 0.3514 1(20%) 9(34.6%) 1.0000
II 0 20(55.6%) 0.4595 3(60%) 15(57.7%) 1.0000
III 0 4(11.1%) 1.0000 1(20%) 2(7.7%) 0.4216
Surgicaltime
<1h 0 1(2.8%) 1.0000 0 0 1.0000
1---3h 1 12(33.3%) 0.3514 2(40%) 7(26.9%) 0.6125 >3h 0 23(63.9%) 0.3784 3(60%) 19(73.1%) 0.6125
ASA,AmericanSocietyofAnaesthesiologists.
upperabdominalsurgeriesremainbedriddenmoretimeand haveahighergrowthofskincommensals,whichcould facil-itatecolonization.2,19,29
In our study, a high percentage of patients (94.1%) receivedadoseof antimicrobialduringinduction of anes-thesia,anditisdifficulttodemonstratewhetheritprovided aprotective effect.It is knownin literature that theuse ofantimicrobials upto1h beforesurgeryor during anes-thesiaminimizestheincidenceofinfectionatthesurgical site.25,30---33Studieswithsurgicalpatientsandepidural
anal-gesia for 2---3 days show thatcatheter colonization is not associatedwithinvasiveinfectionandis notpreventedby theantimicrobialprophylaxisofsurgery.34However,Aldrete
etal.35reportedthatwhenusingprophylacticantibioticsfor
prolongeduseofcatheters,therateofinfectiondecreases. Althoughtherewerepositivecathetertips,therewereno casesofinfection,demonstrating thattheroutineculture of catheters may not be indicated. In our study, the use of antimicrobials may have contributed to the low inci-denceofcathetercolonization,butitwasnotstatistically proven.
Moststudies recommenda limited number of days for epiduralanalgesia.7,21,31 The epiduralcatheterdwell time
isconsidered arisk factor for infectioninsome studies,28
but not in others.34 Catheterizations lasting two days or
lesshavealowincidenceofepiduralinfection,butlonger durationsareassociated withhigherincidence.21 There is
a considerable risk for catheterization with more than 7 days.11 Scott etal.36 andBevacqua etal.37 also found no
associationbetweenthisdwellingtimeandlocalinfection. Itisestimated that1in35cancer patientsandprolonged epiduralanalgesiawillhavedeepepiduralinfectionandthat 1in500willdiefromrelatedcauses.11
Anestheticssuchaslidocaineandbupivacainehave bac-tericidal activity due to the solution acidity, particularly at high concentrations;19,28,35,38 thus, it may be able to
inhibit bacterial growth.This mayexplain the low occur-rence of epidural catheter colonization, as almost all of themreceivedthesedrugs.
The incidence of epidural catheter colonization found in this study is in agreement with findings by other authors.7,19,22,23,37 S.aureus andGram-negativebacilli
iso-latedincathetersarethemostcitedintheliteratura.1,2,6,7,19
The finding of P.aeruginosa emphasizesthe possibility of nosocomial microorganismscontaminate the catheterand reachthespinalspace.7
There areno comparisons between infected and unin-fected catheters and even between colonized and not colonized catheters, as in the present study, regarding catheterdwellingtime,typeand durationofsurgery, and physical statusofpatients intheliterature.However,this knowledge is important to assess the degree of risk to which each patientwill be submitted when a catheter is used. Although in our study none of these factors was found to be predictive of colonization, the number of cases evaluated was small, which led to a low statisti-caltest powertodetectexistingriskfactorsamongthese variables.
For the same reason, this study was not intended
to assess the safety of postoperative epidural analge-sia in surgical patients with regard to spinal space infection, as it is a rare occurrence. There are less
than 0.01% of patients when the technique is used
for short-term surgical and obstetrical procedures.7 The
concomitantuseofantimicrobialsmaycontributetothelow incidence.39
Ourstudyhassomelimitations.Epiduralanalgesiahada shortduration,withameanof43h.Althoughtheshort dura-tionmayspeakagainstcolonization,theuseofprophylactic antibiotics,thesmallnumberofcases,andtheclinical fac-torsofthestudypatientsmayhaveinfluencedtheculture results.
Despite uncertainties about the relationship between contaminationand clinical infection,alleffortsshould be directedtominimizethepotentialriskofinfection,asthe impactofapossibleinfectioncausedbyepiduralcatheter could resultin irreversibleconsequences for the patient, suchaspermanentneurologicaldeficits.
The use of postoperative epidural analgesia in surgi-calwardpatients,understrictasepticandantisepticcare provedtobeaprocedurewithlowriskofbacterial coloniza-tion.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.Dawson SJ. Epidural catheter infections. J Hosp Infect. 2001;47:3---8.
2.MishraS,Ishira S,Bhatnagar S,et al.Clinicalimplication of routinebacterialculture fromepiduralcathetertipsin post-operativecancer patients: a prospectivestudy. Anaesthesia. 2006;61:878---82.
3.Yeager MP, Glass DD, Neff RK, et al. Epidural anesthesia and analgesia in high-risk surgical patients. Anesthesiology. 1987;66:729---36.
4.Buggy DJ, Smith G. Epidural anaesthesia and analgesia: better outcome after major surgery? Br Med J. 1999;319: 530---1.
5.Kost-byerlyS,Tobin JR, GreenbergRS,et al. Bacterial colo-nizationandinfectionrateofcontinuousepiduralcathetersin children.AnesthAnalg.1998;86:712---6.
6.Holt HM, Andersen SS, Andersen O, et al. Infections fol-lowing epidural catheterization. J Hosp Infect. 1995;30: 253---60.
7.DarchyB,ForcevilleX,BavouxE,etal.Clinicaland bacterio-logicsurveyofepiduralanalgesiainpatientsintheintensive careunit.Anesthesiology.1996;85:988---98.
8.StraffordMA,WilderRT,BerdeCR.Theriskofinfectionfrom epiduralanalgesiainchildren:areviewof1620cases.Anesth Analg.1995;80:234---8.
9.Burstal R, Wegner F, Hayes C, et al. Epidural analgesia: prospective audit of 1062 patients. Anaesth Intensive Care. 1998;26:165---72.
10.BrooksK,PaseroC,HubbardL,etal.Theriskofinfection asso-ciatedwithepiduralanalgesia.InfectControlHospEpidemiol. 1995;16:725---6.
11.Ruppen W, Derry S, Mcquay HJ,et al. Infection rates asso-ciatedwith epidural indwelling catheters for seven days or longer:systematicreviewandmeta-analysis.BMCPalliatCare. 2007;6:1---8.
12.GrewalS,HockingG,WildsmithJAW.Epiduralabscesses.BrJ Anaesth.2006;96:292---302.
13.Maki DG, Weise CE, Sarafin HW. A semiquantitative culture methodforidentifyingintravenous-catheter-relatedinfection. NEnglJMed.1977;296:1305---9.
14.Baker AS, OJemann RG, Swartz MN, et al. Spinal epidural abscess.NEnglJMed.1975;293:463---8.
15.KhannaRK,MalikGM,RockJP,etal.Spinalepiduralabscess: evaluation of factors influencing outcome. Neurosurgery. 1996;39:958---64.
16.Maslen DR, Jones SR, Crislip MA, et al. Spinal epidural abscess.Optimizingpatientcare.ArchInternMed.1993;153: 1713---21.
17.McGee-Collett M,Johnston IH.Spinal epidural abscess: pre-sentation and treatment. Areport of21cases. MedJ Aust. 1991;155:14---7.
18.McLaurin RL. Spinal suppuration. Clin Neurosurg. 1966;14: 314---36.
19.SimpsonRS,MacyntirePE,ShawD,etal.Epiduralcathetertip cultures:resultsofa4-yearauditandimplicationsforclinical practice.RegAnesthPainMed.2000;25:360---7.
20.BirnbachDJ,MeadowsW,SteinDJ,etal.Comparisonof povi-done iodine and duraprep, an iodophor-in-isopropyl alcohol solution,forskindisinfectionpriortoepiduralcatheter inser-tioninparturients.Anesthesiology.2003;98:164---9.
21.MorinAM,KerwatKM,KlotzM,etal.Riskfactorsforbacterial cathetercolonizationinregionalanaesthesia.BMCAnesthesiol. 2005;5:1---9.
22.SteffenP,SeelingW,EssigA,etal.Bacterialcontaminationof epiduralcatheters:microbiologicalexaminationof502 epidu-ralcathetersusedforpostoperativeanalgesia.JClinAnesth. 2004;16:92---7.
23.DarouicheRO,HamillRJ,GreenbergSB,etal.Bacterialspinal epidural abscess. Review of 43cases and literature survey. Medicine(Baltimore).1992;71:369---85.
24.Reihsaus E, Waldbaur H, Seeling W. Spinal epidural abscess: a meta-analysis of 915 patients. Neurosurg Rev. 2000;23: 175---204.
25.MangramAJ,HoranTC,PearsonML,etal.Guidelinefor pre-ventionofsurgicalsite infection,1999. AmJInfectControl. 1999;27:97---134.
26.GiacomettiA,CirioniO,SchimizziAM,etal.Epidemiologyand microbiology of surgical wound infections. J Clin Microbial. 2000;38:918---22.
27.WeigeltJA,LipskyBA,TabakYP,etal.Surgicalsiteinfections causativepathogensandassociatedoutcomes.AmJInfect Con-trol.2010;38:112---20.
28.Du Pen SL, Peterson DG, Williams A, et al. Infection dur-ingchronicepiduralcatheterization:diagnosisandtreatment. Anesthesiology.1990;73:905---9.
29.McneelyJK,Trentadue NC,RusyLM,etal.Cultureof bacte-ria from lumbar and caudal epidural catheters used for postoperative analgesia in children. Reg Anaesth. 1997;22: 428---31.
30.KasudaH,FukudaH,TogashiH,etal.Skindisinfectionbefore epidural catheterization: comparative study of povidone-iodine versus chlorhexidine ethanol. Dermatology. 2002;204: 42---6.
31.Sethna NF, Clendenin D, UmeshkumarA, et al. Incidence of EpiduralCatheter-associatedInfectionsaftercontinuous epidu-ralanalgesiainchildren.Anesthesiology.2010;113:324---32. 32.RaedlerC,Lass-florlC,PuhringerF,etal.Bacterial
contamina-tionofneedlesusedforespinalandepiduralanaesthesia.BrJ Anaesth.1999;83:657---8.
33.Dipiro JT, Cheung RPF, Bowden TA, et al. Single Dose sys-temicantibioticprophylaxisofsurgicalwoundinfections.Surg PharmacolAmJSurg.1986;152:552---9.
34.KostopanagiotouG,KyroudiS,PanidisD,etal.Epiduralcatheter colonization is not associated with infection. Surg Infect. 2002;3:359---65.
36.ScottDA, BeilbyDSN, McClymontC. Postoperative analgesia usingepiduralinfusionsoffentanylwithbupivacaine.A prospec-tiveanalysisof1,014patients.Anesthesiology.1995;83:727---37. 37.BevacquaBK,SluckyAV,ClearyWF.Ispostoperativeintrathecal catheteruseassociatedwithcentralnervoussysteminfection? Anesthesiology.1994;80:1234---40.
38.Feldman JM, Chapin-Robertson K, Turner J. Do agents for epiduralanalgesiahaveantimicrobialproperties?RegAnaesth. 1994;19:43---7.