rev bras hematol hemoter. 2015;37(3):207–210
w w w . r b h h . o r g
Revista
Brasileira
de
Hematologia
e
Hemoterapia
Brazilian
Journal
of
Hematology
and
Hemotherapy
Case
Report
Central
retinal
vein
occlusion
as
first
manifestation
of
relapse
in
acute
lymphoblastic
leukemia
Flávia
Kessler
Borges,
Júlia
Biegelmeyer,
Samantha
Thifani
Alrutz
Barcelos
∗,
Raquel
Cristine
Breunig
UniversidadeFederaldeCiênciasdaSaúdedePortoAlegre(UFCSPA),PortoAlegre,RS,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received6November2014 Accepted31December2014 Availableonline14April2015
Introduction
Retinal vein occlusion is the second most common cause ofvisualloss dueto retinalvascular disease afterdiabetic retinopathy.1 Among the risk factors described, it is well knownthatthehypercoagulablestatepresentinneoplasias canculminateinveinocclusion.Itisdescribedthatanyocular structuremay beinvolvedinacuteleukemia2; involvement of the choroid and retina is the most common. However, leukemic cells can infiltrate the conjunctiva and lacrimal glands,producingobviousmasses.Kareshetal.publisheda twoyearprospectivestudy ofnewly diagnosedadultswith acutemyeloidleukemia;64%ofpatientshadretinaloroptic nerve abnormalities where hemorrhages and cotton wool spots(aconsequenceofnervefiberischemia)werethemost frequentfindings.3 Theassociation betweencentral retinal vein occlusion and acute lymphoblastic leukemia (ALL) relapsehasrarelybeendescribedthough.4–6Weherebyreport
∗ Correspondingauthorat:RuaSarmentoLeite,245,Centro,90050-170PortoAlegre,RS,Brazil.
E-mailaddress:samanthatifani@gmail.com(S.T.A.Barcelos).
a case of central retinal vein occlusion as the presenting manifestationofrelapseinALL.
Case
report
A59-year-oldfemalewasdiagnosedwithALLinNovember 2013.Atthattime,shehadthefollowinglaboratoryresults: hemoglobin:8.7g/dL;redbloodcells:2.95×109/L;MCV:89fL; total leukocytes: 18.66×109/L; lymphocytes: 5.374×109/L;
segmented neutrophils: 2.930×109/L; blasts: 9143cells/L; uric acid: 5.2mg/dL; lactic dehydrogenase: 1672U/L; creati-nine: 3.1mg/dL; and urea: 83mg/dL. She received volemic resuscitation for tumor lysis syndrome. Subsequently, she developed pneumonia caused by Cryptococcus neoformans and herpeszoster skin lesions.Treatment was made with meropenem, amphotericin and acyclovir. In January 2014, aftercompletingtreatmentfortheinfections,shewas sub-mitted to chemotherapy induction using the hyperCVAD
http://dx.doi.org/10.1016/j.bjhh.2015.03.008
208
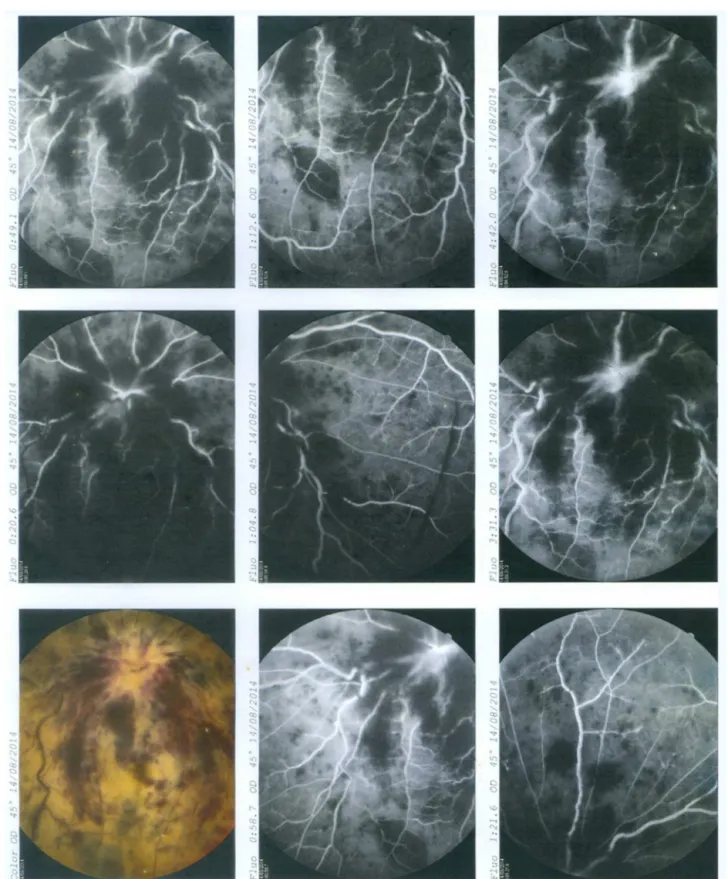
revbrashematolhemoter.2015;37(3):207–210Figure1–Fluoresceinangiographyshowingocclusionofcentralretinalvein.
regimen–courseA(cyclophosphamide,vincristine, doxoru-bicinand dexamethasone).Immunophenotypingperformed inFebruary2014showedremissionofthedisease.
In March 2014 she presented febrile neutropenia and typhlitis.Empirictreatmentwithcefepimewasstartedand the hyperCVAD regimen was interrupted. Blood cultures
identifiedEscherichia coliandKlebsiellapnemoniae. Treatment wascompletedonApril20th2014.
revbrashematolhemoter.2015;37(3):207–210
209
tocompletethefourthcycleoftherapyduetohematological toxicity(hemoglobin:9.0g/dL;redbloodcells:2.71×109/L; totalleukocytes:0.870×109/L;neutrophils:0.628×109/L;and
platelets:13×109/L).
In August 2014 she came to our hospital emergency departmentcomplainingofaheadacheoftheright sideof her head, sensitivity to light, nausea, vomiting and visual lossinthe right eyethathad started four dayspreviously. Theneurological exam showed no abnormality, except for the eye fundus examination, which revealed papilledema, intraretinal peripapillary and inframacular hemorrhage in the right eye.The left eye presented a pre-retinal hemor-rhage.
Laboratory exams did not reveal any abnormality. A coagulation panel showed platelets 154×109/L;
prothrom-bin time activity: 100%; international normalization ratio (INR): 1.00; and activated partial thromboplastin time: 36.6s.
Anuclearmagneticresonanceimage(MRI)wasmade,and theonlyabnormalitywasahypointenselesionevidencedin theT2sequenceintherighttemporalposteriorregion,which wasprobablyasequelaeofaprevioushemorrhagicinfarct.
Shewasthensubmittedtoafluoresceinangiographythat revealedocclusionofthecentralretinalvein(Figure1).
Inordertoexcludeanyinfectiousetiology,alumbar punc-turewasmade,withanormalopeningpressure(150cmH2O). Cerebrospinal fluid analysis evidenced low glucose lev-els (28mg/dL and 89mg/dL in blood); high protein levels (89mg/dL); cellularity 2520cells/L; 94% blasts; 5% mono-cytes;and redbloodcells:220cells/L.Culturesforfungus, bacteriaandcytomegalovirusantigenemiaandherpesvirus polymerasechainreaction(PCR)wereallnegative.
Shewasnottakinganydrugthatwouldpotentiallybe capa-bleofinducingretinalveinocclusion.
Inordertocompletetheevaluationofpossible intracere-bralveinthrombosis,thepatientwassubmittedtoavascular MRIthatrevealedthickeningoftherightopticnerveandoptic chiasmprotuberance.
Immunophenotypingoftheliquorhad predominanceof CD10,CD19,DC22,CD34,HLADRcells,suggestingBlineage ALL. Lymphoblasts were identified in the cytopathological examandbonemarrowcytologyconfirmedmedullar infiltra-tion.
Afterconfirming neurologicalrelapse ofALL,intrathecal chemotherapy was given with dexamethasone, cytarabine andmethotrexate.Shehadcompleteremissionofheadache, buthadnoimprovementofhervisualloss.
Amagneticresonanceangiographyofthecentralnervous system(CNS)wascarriedouttoexcludeotherpossible vas-cularthrombosis,butnoalterationwasfoundintheexam, exceptforinfiltrationoftherightopticnerve.
Shewas dischargedfrom hospitalaftertwo sessions of intrathecal chemotherapy, and continues outpatient treat-ment.
Discussion
Therearefewcasesreportedintheliteratureshowingocular nerveinfiltrationasanisolatedmanifestationofALLrelapse,
even thoughit is aconsequenceof CNSinvolvementwith severeprognosis.Inthecasereportedherein,thepatienthada headacheassociatedwithvisualloss,whichstronglysuggests CNS damage.Onceher ophthalmologic exam showedonly centralretinalveinocclusion(CRVO),theclinicaldiscussion focusedontheetiology oftheunderlyingprocess:whether it was aconsequenceofa hypercoagulablestateor dueto directinvasionofneoplasticcellssincebothconditionscan culminateinCRVO.
Inordertoelucidatethisquestion,amagneticresonance angiography wasperformed toexcludeother possiblevein occlusionsintheCNS,buttheonlyfindingwasopticnerve infiltration,whichhadnotbeenevidentuntilthismoment. IthasalreadybeendescribedthatMRIisusefulintheearly detectionofocularinvolvement.7
EventhoughCRVOisrelatedwithanhypercoagulablestate, allthecasesdescribedintheliteraturethatassociateCRVO withALLaresecondarytoaninfiltrationofleukemiccells.4–6 Allcasesshowinfiltrationoftheopticdiskprecedingvessel occlusion.
Treatmentdescribedinthesecasesconsistsinintrathecal chemotherapyandradiotherapy.8,9Thereisnobenefitin pre-scribingvascularendothelialgrowthfactor(VEGF)inhibitors inthesecases,asthereiscombineddamageofthevein cir-culationandtheopticnerveconduction;thelattercancause irreversiblevisualloss.10
Conclusion
CNSrelapsecanprecedehematologicalsignsandsymptoms, and regular ophthalmologic exams should be instituted in patients withALL. If ocularsymptomsare presentand the ophthalmologicexamisnormal,aMRIshouldbeconsidered. In cases of ALL and retinal vessel occlusion, always con-sideropticnerveinfiltrationandrapidlyinstitutetreatment withintrathecalchemotherapyandradiotherapytoavoid irre-versibledamage.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1.CugatiS,WangJJ,RochtchinaE,MitchellP.Ten-yearincidence
ofretinalveinocclusioninanolderpopulation:theBlue
MountainsEyeStudy.ArchOphthalmol.2006;124(5):726–32.
2.RosenthalAR.Ocularmanifestationsofleukemia.Areview.
Ophthalmology.1983;90(8):899.
3.KareshJW,GoldmanEJ,ReckK,KelmanSE,LeeEJ,Schiffer
CA.Aprospectiveophthalmicevaluationofpatientswith
acutemyeloidleukemia:correlationofocularand
hematologicfindings.JClinOncol.1989;7(10):1528.
4.SalazarMendezR,FonollaGilM.Unilateralopticdiskedema
withcentralretinalarteryandveinocclusionsasthe
presentingsignsofrelapseinacutelymphoblasticleukemia.
ArchSocEspOftalmol.2014;89(11):
210
revbrashematolhemoter.2015;37(3):207–2105. ChanWM,LiuDT,LamDS.Imagesinhaematology.Combined
centralretinalarteryandveinocclusionsasthepresenting
signsofocularrelapseinacutelymphoblasticleukaemia.BrJ
Haematol.2005;128(2):134.
6. BadelonI,ChaineG,TolubO,CoscasG.Occlusionofthe
centralveinandarteryoftheretinacausedbyinfiltrationof
theopticnerveinlymphoblasticacuteleukemia.BullSoc
OphtalmolFr.1986;86(3):261–4.
7. DeFátimaSoaresM,BragaFT,daRochaAJ,LedermanHM.
Opticnerveinfiltrationbyacutelymphoblasticleukaemia:
MRIcontribution.PediatrRadiol.2005;35(8):799–802.
8.KaikovY.Opticnerveheadinfiltrationinacuteleukemia
inchildren:anindicationforemergencyopticnerve
headradiationtherapy.MedPediatrOncol.1996;26(2):
101–4.
9.MayoGL,CarterJE,McKinnonSJ.Bilateralopticdiskedema
andblindnessasinitialpresentationofacutelymphocytic
leukemia.AmJOphthalmol.2002;134(1):141–2.
10.BraithwaiteT,NanjiAA,GreenbergPB.Anti-vascular
endothelialgrowthfactorformacularedemasecondaryto
centralretinalveinocclusion.CochraneDatabaseSystRev.