SOCIEDADE BRASILEIRA DE ORTOPEDIA E TRAUMATOLOGIA
w w w . r b o . o r g . b r
Original
article
A
retrospective
analysis
of
surgically-treated
complex
proximal
femur
fractures
with
proximal
femoral
locking
compression
plate
夽
Syed
Ibrahim
∗,
Jimmy
Joseph
Meleppuram
VinayakaMissionsMedicalCollegeandHospital,DepartmentofOrthopaedics,Karaikal,PondyIndia
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received30August2016 Accepted3October2016 Availableonline7January2017
Keywords:
Femoralfractures Boneplates Fracturefixation Internal
a
b
s
t
r
a
c
t
Objective:Analyzetheoutcomesofproximalfemorallockingcompressionplate(PF-LCP)in thesecomplexfractures.
Methods:Thisstudyretrospectivelyanalyzed21proximalfemoralfracturestreatedwith PF-LCPfromJune2013toFebruary2015.Therewere15females(71%)andsixmales(29%)with anaverageageof61.4years(range:34–80years).Theperitrochantericfracturesconstituted byintertrochantericandsubtrochantericfractureswereclassifiedbytheBoydandGriffin classificationandSeinshemier’sclassification,respectively.Amongthem,16cases(76%) wereofintertrochantericandfivecases(24%)wereofsubtrochantericfracturepattern.The functionaloutcomewasassessedbyHarrisHipScoreandtheParkerPalmermobilityscore oneyearpost-surgery.
Results:Among21patients,19patientsobtainedfractureunionwithoutfurther interven-tion;twopatientsrequiredadditionalbonegrafting.Nocasesofthehipscrewcuttingthe femoralheadwerenoted.Therewasnopost-operativemortalityinthisstudy.Theaverage HarrisHipScorewas84.5(range:83–94).TheassessmentbyParkerandPalmarmobility scorewas7.5(range:4–9).
Conclusion:ThePF-LCPis agood,stablealternativeinthetreatmentofperitrochanteric femoralfractures.Itprovidesgood-to-excellentbonehealingwithreducedcomplications.
©2016SociedadeBrasileiradeOrtopediaeTraumatologia.PublishedbyElsevierEditora Ltda.ThisisanopenaccessarticleundertheCCBY-NC-NDlicense(http:// creativecommons.org/licenses/by-nc-nd/4.0/).
夽
WorkperformedintheVinayakaMissionsMedicalCollegeandHospital,DepartmentofOrthopedics,Karaikal,India.
∗ Correspondingauthor.
E-mails:dr.ibrahim21@rediffmail.com,drsyedibrahima@gmail.com(S.Ibrahim). http://dx.doi.org/10.1016/j.rboe.2016.12.012
Uma
análise
retrospectiva
de
fraturas
complexas
do
fêmur
proximal
tratadas
cirurgicamente
com
placa
de
compressão
bloqueada
do
fêmur
proximal
Palavras-chave:
Fraturasdofêmur Placasósseas Fixac¸ãodefratura Interna
r
e
s
u
m
o
Objetivo: Analisarosresultadosdaplacadecompressãobloqueadadofêmurproximal (PF-LCP)nestasfraturascomplexas.
Métodos: Esteestudoretrospectivamenteanalisou21fraturasproximaisdofêmurtratadas comPF-LCPentrejunhode2013efevereirode2015.Foramincluídas15mulheres(71%)eseis homens(29%)comidademédiade61,4anos(intervalo:34a80anos).Asfraturas peritrocan-téricasconstituídasporfraturasintertrocantéricasesubtrocantéricasforamclassificadas pelaclassificac¸ãodeBoydeGriffinepelaclassificac¸ãodeSeinshemier,respectivamente. Entreelas,16casos(76%)foramclassificadascomopadrãointertrocantéricoecincocasos (24%)comopadrãosubtrocantérico.Oresultadofuncionalfoiavaliadopeloescoredequadril deHarrisepeloescoredemobilidadedeParkerPalmerumanoapósacirurgia.
Resultados:Dentreos21pacientes,19obtiveramuniãodefraturasemintervenc¸ãoadicional edoispacientesnecessitaramenxertoósseoadicional.Nenhumcasodecortedacabec¸a femoralpeloparafusodoquadrilfoiobservado.Nãohouvemortalidadepós-operatórianeste estudo.AmédiadoescoredequadrildeHarrisfoide84,5(intervalo:83a94).Amédiado escoredemobilidadedeParkerPalmerfoide7,5(intervalo:4a9).
Conclusão: A PF-LCPé umaalternativa adequada eestável no tratamento de fraturas femoraisperitrocantéricas,propiciandoumaosteossínteseclassificadacomoboaou exce-lente,compoucascomplicac¸ões.
©2016SociedadeBrasileiradeOrtopediaeTraumatologia.PublicadoporElsevier EditoraLtda.Este ´eumartigoOpenAccesssobumalicenc¸aCCBY-NC-ND(http:// creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
Proximalfemoralfracturesarecommoninjuriesthatmainly affectthegeriatricpopulation.1Inyoungandhealthy
individ-uals,theinjuryowesduetohighenergytrauma,roadtraffic accidentswhereasintheelderagegroup,mostofthe frac-turesare osteoporotic,resultingfromatrivialfall.Proximal femurfracturescomprise,fracturesofintertrochantericand subtrochantericregionorbothincombination.
Intertrochantericfractures aremostcommoninfemale ofelderly agegroup due toosteoporosisand 90% ofthese fractures resultfrom asimple fall.1 Asconservative
meth-odsprognosedtohavehigher mortalityratesrangingfrom 4.5to22% theyarenow reservedonlyforvery elderly per-son with high medical risk for anesthesia and surgery.2
Thus, surgery by open reduction and internal fixation is the ideal choice of management. The objective of the surgery is to attain initial stability and early mobilization of the patients in order to avoid complications such as deep vein thrombosis, pulmonary embolism, urinary tract and lung infections and ulcers.2 Dynamic hip screw(DHS)
isthe gold standard treatment for stableintertrochanteric fractures.3
Incase ofunstable intertrochanteric fractures,the inci-denceofmedializationofdistalfracturefragment, implant cutoutsandlimbshorteningarehigh.Inthosecases, prox-imal femur nail (PFN)is the implant of choice.4,5 PFN has
anadditionalanti rotation pinor set pinwhich isused to preventtherotationalstrainatthefracturesite.Due tothe
betterunderstandingofbio-mechanicsofhipfractureandits geometry,thistechniquecouldprovidepromisingresults.6,7
Incertaincases,likegreattrochanterorlateralwall frac-ture variety in proximal femoral fractures, PFN cannot be performed.8,9Inthosecases,DynamicCondylarScrew(DCS)
isthetreatmentofchoice,but,incaseifthereismore com-munitioninthelateralwall,DCSisdifficulttoemploy.10The
lateraltrochantericwallisbelievedtobeanimportantfactorin stabilizingpertrochantericfractures,keepingthelateralwall intactminimizestheratesofmalunionandnonunionaswell ascanpromoteinquickfracturehealing.Thisledwaytothe developmentofnewermethodslikeProximalFemurLocking CompressionPlate(PF-LCP).Itisthefeasiblealternativefor thetreatmentofthesekindsoffractures.11,12
PF-LCPprovidesthesurgeonwiththeeasyaccessibilityto achieveplate toboneappositionaswellasaxialload com-pressionorangularstabilitybecauseofthreescrewfixation patternatthefracturesite.Unlikeconventionalcompression plates,thescrewheadlocksintothePF-LCP,therebycreating anangularstableconstruct.PF-LCPcanprovideastressshield forthelateraltrochantericwallandpreventlateralmigration ofproximalfracturefragments.Thus,PF-LCPdoesnotfailat thescrewboneinterfaceaswellasprovideastronganchor inosteoporoticbone.Themultiplelockingscrewholesofthe PF-LCPprovidevariousoptionstoovercomeanycomplex frac-turepattern.Itfunctionsasaninternalizedexternalfixator andminimizesthepressureontheperiosteumandthereby encouragesquickbiologicalhealing.13
ofunion,functional outcome,post-operativecomplications andfailurerate.
Materials
and
methods
Inourstudy,21adultpatientswithcomplexproximalfemur fractures following the inclusion criteria treated with PF-LCP from June 2013 to February 2015 were retrospectively analyzedfromthe hospitalrecords.Therewere 15females (71%)andsixmales(29%)withanaverageageof61.4years (range: 34–80years). Most ofthe fractures were caused by trivial fall (n=14) followed by road traffic accidents (n=7). Therightsidewasincludedineightcases(38%)andtheleft sidein13cases(62%).Theperitrochantericfractures consti-tutedbyintertrochantericandsubtrochantericfractureswere classifiedbyBoydandGriffinclassificationalongwith Sein-shemier’sclassification,respectively.14Amongthat,16cases
(76%)wereofintertrochantericandfivecases(24%)wereof subtrochantericfracture variety.Allcaseswerefollowedup routinely.
Inclusioncriteria
• Patientswithcomplexproximalfemurfractures • Patientswithlateralwallfracturescomminution • Patientswithfracturesduetosevereosteoporosis.
Exclusioncriteria
• Simpletrochantericfracture • AssociatedFemoralneckfracture • Pathologicalfractures
• ReverseobliqueandNoncommunitedfractures
Surgicaltechnique
As soon as the patient with suspected subtrochanteric or trochantericfracturewasseen,necessaryclinicaland radio-logicalevaluationwascarriedoutand wasadmittedtothe wardafternecessaryresuscitationalongwithsplintageusing skin traction ofadequate weights depending upon his/her nutritionalbuilt.Analgesicsandappropriateantibioticswere givenaccordinglythroughrequiredroutesofadministration. Patientswereassessedforassociatedmedicalproblemsand crossreferencewasobtainedfrom otherconcerned depart-ments, if needed. Associated injuries were evaluated and treatedsimultaneouslywithremedial measuresasearly as possible.Allpatientswereoperatedonplannedelectivebasis. After adequate preoperative planning, under spinal or epiduralanesthesia,patientswerepositionedsupineonthe fracturetable,reductionachieved,maintainedandconfirmed underimageintensifierpayingspecialattentiontothe pos-teriorand medialcorticalcontact.A15cmverticalincision wastakenfromthetipoftrochanterindistaldirectionalong theshaftofinvolvedfemur.Fascialatawassplitinlinewith theincisionand gluteusmediusalong withvastuslateralis muscleswere openedinline withthefibers andtipofthe trochanter,thereby exposingthe proximalfemurwith frac-ture.
Fig.1–Proximalfemurlockingcompressionplatewith
screwsset.
Theultimate platepositionand screwpositiondepends uponthefracturereductionachievedandplacementofguide wiresintothe involvedfemoralheadandneck(Fig.1).The fixed-angleguide wiresare threadedtothe proximalthree holesoftheplate,andtheplateisapproximatedtothe prox-imal femur. Next, aguide wire was advanced through the mostproximal(95-degree)hole.Thecorrectpathofthiswire isapproximately1cminferiortothepiriformisfossaintothe inferiorfemoralheadontheAnteroposterior(AP)view,and centralinthefemoralheadonthelateralview.Aguidewireis inserted intothenextdistal(120-degree)hole,andbecause this isina differentplanethan the firsthole,the surgeon mustvisualizeitspositiononthelateralx-ray.Thethirdguide wire,inthe135-degreehole,isthenplaced,whichisinthe sameplaneasthefirstholeandmayalternativelybeinserted neartheendoftheprocedurewithoutcompromisingthe sta-bility ofthe gained construct.All threeguide wiresshould beinsubchondralboneofthefemurheadbefore inserting the screwswhich is confirmed byimage intensifier in the APandLateralviews.Thescrewlengthsaremeasuredusing anindirectdeviceovertheguidewireswiththewireguides stillattachedandtheappropriate,fullythreaded,cannulated screws(7.3mmforthetwoproximalholesand5.0mmforthe thirdproximalhole)areselected.Thesecannulatedscrewsare insertedovertheguidewiresfollowingafterwhichtheguide wiresareremoved.
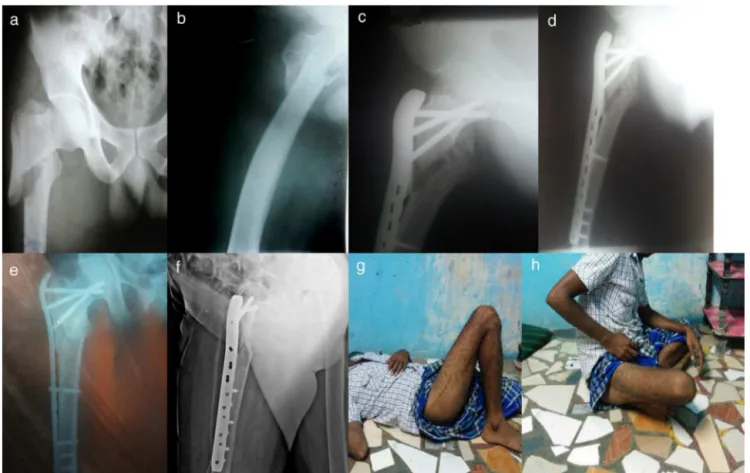
Fig.2–(a,b)Pre-operativeX-raysof60yearsfemalewithleftcomplexproximalfemoralfracture;(c,d)immediatepost-op
X-raysafterPF-LCPfixation;(e,f)X-raysshowingunitedfractureatoneyearfollow-up;(g,h)clinicalpictureshowing
excellentfunctionaloutcomeaswellastheParkerandPalmarmobilityscoreof5.7forthepatient.
screwsdirectly.Afterthecompletionofthefixation,thorough washofthewoundwasgivenwithnormalsalineand anti-septicsolution.Suctiondrainwasinsertedattheentrypoint andwoundclosedinlayerswithadequatesteriledressing.
Post-operatively, adequate analgesics, appropriate intra-venous antibiotics were given for subsequent five days. Prophylactically,inall patients, subcutaneousLow Molecu-larWeightHeparin(LMWH)wasgivenforthreeconsecutive daystoreducetheriskofbedriddencomplicationssuchas deepveinthrombosis,pulmonaryetc.Postoperativecheck X-raywasobtained.Drainwasremovedafter48h.Bedsideknee bendingexerciseswereinitiatedwhenpainreducedonthird or fourthpost-operative day.Patients were reviewedat six weeks,threemonths,sixmonthsandoneyearafteroperation withclinicalandradiographicassessmentfortheprogressof fracturehealingandothercomplications.Thefunctional out-comewasassessedbyHarrisHipScoreandParkerandPalmer mobilityscoreoneyearafterthesurgery.15
Results
Thepatientswerefollowedupforanaverageof13months (12–17months).Theaverageoperatingtimewas60minwith
ameanbloodlossof250ml(includingoperativeandwound drainage).Theaveragelengthofincisionwas9cm(8–16cm). Averageimageintensifiertimewas10min.
Of the proximal femoral fractures, it was found out, subtrochanteric fractures,took longer operativetime, radi-ation exposure and had morebleeding when comparedto intertrochanteric fractures.Amongstthe 21cases, 19cases healedwithnolossofimplantpositionandfracture reduc-tionattheoneyearfollowupcheckup.Thereweretwocases withdelayedunionwhichwasseverelycomminuted,needed additionalbonegrafting.Onecasehadsuperficialinfection duetouncontrolleddiabeteswhichgotsettledlateron.There werenocasesofhipscrewcuttingthefemoralhead.There wasnopostoperativemortalityinourstudy.
TheaverageHarrisHipScorewas84.5(83–94).Theresults were excellentin12cases(57%)(Fig.2), goodinfourcases (19%)(Fig.3)fairinfivecases(24%).Therewerenopoorresults. TheassessmentbyParkerandPalmarmobilityscorewas7.5 (range:4–9).
Discussion
Fig.3–(a,b)Pre-operativeX-raysof36yearmalewithrightcomplexproximalfemoralfracture;(c,d)3monthpost-op
X-raysafterPF-LCPfixationshowingdelayedunionandrequiredadditionalbonegrafting;(e,f)X-raysshowinggood
fractureunionatendofoneyear;(g,h)clinicalpictureshowingfairfunctionaloutcomeandParker–Palmarmobilityscoreof
7.7forthepatient.
ofprolongedbedrestandassociatedcomplications.Theideal treatmentofthesefracturesremainscontroversial.16The
fix-ationmethodrangesfromdynamichipscrew(DHS)instable fractures andintra medullarydevices inunstable fractures whichhassometheoreticaladvantageoverDHSbecausethey don’tdependonthescrewfixationofaplatetothelateral cor-texwhichisaprobleminaveryosteoporoticbone.Thefailure rateinintramedullarydevicesrangesfrom12.7to15%in var-iousstudies.17,18Finsenfoundthattherewasnodifferencein
thetimetakentoreducethefractureorthelengthof oper-atingtimebypreoperativetraction.19ReschandThorngren20
comparedskintractionversusskeletaltraction.50%of skele-tal traction compared with20% of skin traction group. He alsofoundnodifferencebetweenthetwogroupsashestated thatmanypatientsfoundtheapplicationofskeletaltraction painfull,bothFinsenandReschreportedno significant dif-ferenceinthelengthofoperation.Thesewerecomparableas sametoourcaseseries.
As for the PFN, Fogagnolo et al.21 found the
intrao-peartivetechnicalor mechanicalcomplicationrate ashigh as23.4%.Uzunet al.22 reportednon-union5.7%,secondary
varusdisplacement25.7%,screwcut-out5.7%,reverseZeffect 14.3%.Ekström et al.23 reported a lower complicationrate
of 8%. In the current study, we found that the manage-ment of pertrochanteric fractures fixed with PF-LCP could
lowerthecomplicationratethanothertreatmentmodalities described above.In ourstudy,therewere nocasesofinter operativeandtechnicalcomplicationsaspartoother stud-ies compared.24 Other parameters such as operating time,
operativebloodloss, radiationexposuretimeand lengthof incision are bettertothoseinprevious studiesusing other devices.11,12,25
Inourstudy,theunionratewithproximalfemoral frac-tures at the end ofthree months was 88%, at the end of 6monthswas93%and had100%unionatoneyear follow up.Nocaseshadcut-outofthefemoralheadscrewpossibly duetomechanicaladvantageofthreedimensionand angu-larstablefixationbyPF-LCP.Theimplantisbiologicallyand biomechanicallysuitableincomplexfemoralfractures asso-ciatedwithsevere osteoporosis.From previousstudies,the so-calledkickstandscrewplayedanimportantrolein preven-tingvaruscollapseoftheconstruct.26,27ThePF-LCPwiththe
“kickstand”screwwasreportedtohavesimilarbiomechanical propertiesof95-degreeanglebladeplateobserved.Forbetter resultswithPF-LCP,thefracturemustbeadequatelyreduced andallproximalfemorallockingscrews(includingthe ‘kick-stand’screw)shouldbeinsertedtoincreasethemechanical strength ofthe construct.28 PF-LCP locks the fracture in a
purchaseinthe femoralnecksoit isappropriatefor com-plexproximalfemoralfracturefixationeveninosteoporotic bone.
Good preoperative templating with good selection of appropriateimplantalongwithadequatefracturereduction aswellasallthethreeproximalfemorallockingscrews includ-ingthe“kickstand”screwshouldbeinsertedtoincreasethe mechanicalstrength ofthe madeconstruct.Theindication for PF-LCP is narrower and is used only in special situa-tion. The main disadvantage of PF-LCP is open reduction whichcanresultinincreasebloodlossandrequiresskilled technique.12,25
Ourstudyhasseverallimitationsasthesamplesizewas small and we didn’t differentiate trochanteric from sub-trochanteric fracture pattern and lack of comparison with othermodalitiesoftreatmentprotocols.
Conclusion
OurstudyshowsPF-LCPisagoodalternativefortreating com-plexproximalfemoralfractures.Thecomplicationratesare muchlower.Sothetreatmentofcomplexfemoralfracturesis individualizedbasedonpatientassessmentandexperienceof theoperatingorthopaedicianteam.ThePF-LCPprovidesgood toexcellentbonehealingwithalimitednumberof complica-tions.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1. NievesJW,BilezikianJP,LaneJM,EinhornTA,WangY, SteinbuchM,etal.Fragilityfracturesofthehipandfemur: incidenceandpatientcharacteristics.OsteoporosInt. 2010;21(3):399–408.
2. DobbsRE,ParviziJ,LewallenDG.Perioperativemorbidityand 30-daymortalityafterintertrochanterichipfracturestreated byinternalfixationorarthroplasty.JArthroplasty.
2005;20(8):963–6.
3. WolfgangGL,BryantMH,O’NeillJP.Treatmentof
intertrochantericfractureofthefemurusingslidingscrew platefixation.ClinOrthopRelatRes.1982;(163):
148–58.
4. KokoroghiannisC,AktselisI,DeligeorgisA,FragkomichalosE, PapadimasD,PappadasI.Evolvingconceptsofstabilityand intramedullaryfixationofintertrochantericfractures–a review.Injury.2012;43(6):686–93.
5. BoldinC,SeibertFJ,FankhauserF,PeichaG,GrechenigW, SzyszkowitzR.Theproximalfemoralnail(PFN)–aminimal invasivetreatmentofunstableproximalfemoralfractures:a prospectivestudyof55patientswithafollow-upof15 months.ActaOrthopScand.2003;74(1):53–8.
6. SternR.Arethereadvancesinthetreatmentofextracapsular hipfracturesintheelderly?Injury.2007;38Suppl.3:S77–87. Review.Erratumin:Injury2008;39(1):140.
7. HaidukewychGJ.Intertrochantericfractures:tentipsto improveresults.JBoneJointSurgAm.2009;91(3):712–9.
8.GotfriedY.Thelateraltrochantericwall:akeyelementinthe reconstructionofunstablepertrochanterichipfractures.Clin OrthopRelatRes.2004;(425):82–6.
9.PalmH,JacobsenS,Sonne-HolmS,GebuhrP,HipFracture StudyGroup.Integrityofthelateralfemoralwallin intertrochanterichipfractures:animportantpredictorofa reoperation.JBoneJointSurgAm.2007;89(3):470–5. 10.KinastC,BolhofnerBR,MastJW,GanzR.Subtrochanteric
fracturesofthefemur.Resultsoftreatmentwiththe95 degreescondylarblade-plate.ClinOrthopRelatRes. 1989;(238):122–30.
11.ZhaGC,ChenZL,QiXB,SunJY.Treatmentofpertrochanteric fractureswithaproximalfemurlockingcompressionplate. Injury.2011;42(11):1294–9.
12.HasenboehlerEA,AgudeloJF,MorganSJ,SmithWR,HakDJ, StahelPF.Treatmentofcomplexproximalfemoralfractures withtheproximalfemurlockingcompressionplate. Orthopedics.2007;30(8):618–23.
13.EgolKA,KubiakEN,FulkersonE,KummerFJ,KovalKJ. Biomechanicsoflockedplatesandscrews.JOrthopTrauma. 2004;18(8):488–93.
14.JensenJS.Classificationoftrochantericfractures.ActaOrthop Scand.1980;51(5):803–10.
15.NilsdotterA,BremanderA.Measuresofhipfunctionand symptoms:HarrisHipScore(HHS),HipDisabilityand OsteoarthritisOutcomeScore(HOOS),OxfordHipScore (OHS),LequesneIndexofSeverityforOsteoarthritisoftheHip (LISOH),andAmericanAcademyofOrthopedicSurgeons (AAOS)HipandKneeQuestionnaire.ArthritisCareRes (Hoboken).2011;63Suppl.11:S200–7.
16.JensenJS,Sonne-HolmS,TøndevoldE.Unstabletrochanteric fractures.Acomparativeanalysisoffourmethodsofinternal fixation.ActaOrthopScand.1980;51(6):949–62.
17.SaarenpääI,HeikkinenT,RistiniemiJ,HyvönenP,LeppilahtiJ, JalovaaraP.Functionalcomparisonofthedynamichipscrew andtheGammalockingnailintrochanterichipfractures:a matched-pairstudyof268patients.IntOrthop.
2009;33(1):255–60.
18.SehatK,BakerRP,PattisonG,PriceR,HarriesWJ,ChesserTJ. Theuseofthelonggammanailinproximalfemoral fractures.Injury.2005;36(11):1350–4.
19.FinsenV,BørsetM,BuvikGE,HaukeI.Preoperativetractionin patientswithhipfractures.Injury.1992;23(4):242–4.
20.ReschS,ThorngrenKG.Preoperativetractionforhipfracture: arandomizedcomparisonbetweenskinandskeletaltraction in78patients.ActaOrthopScand.1998;69(3):277–9.
21.FogagnoloF,KfuriMJr,PaccolaCA.Intramedullaryfixationof pertrochanterichipfractureswiththeshortAO-ASIF proximalfemoralnail.ArchOrthopTraumaSurg. 2004;124(1):31–7.
22.UzunM,ErtürerE,OztürkI,AkmanS,Sec¸kinF,Ozc¸elikIB. Long-termradiographiccomplicationsfollowingtreatmentof unstableintertrochantericfemoralfractureswiththe proximalfemoralnailandeffectsonfunctionalresults.Acta OrthopTraumatolTurc.2009;43(6):457–63.
23.EkströmW,Karlsson-ThurC,LarssonS,RagnarssonB,Alberts KA.Functionaloutcomeintreatmentofunstabletrochanteric andsubtrochantericfractureswiththeproximalfemoralnail andtheMedoffslidingplate.JOrthopTrauma.
2007;21(1):18–25.
24.SuckelAA,DietzK,WuelkerN,HelwigP.Evaluationof complicationsofthreedifferenttypesofproximal
extra-articularfemurfractures:differencesincomplications, age,sexandsurvivingrates.IntOrthop.2007;31(5):
689–95.
26.GlassnerPJ,TejwaniNC.Failureofproximalfemorallocking compressionplate:acaseseries.JOrthopTrauma.
2011;25(2):76–83.
27.GunadhamU,JampaJ,SuntornsupS,LeewiriyaphunB.The outcomeinearlycasesoftreatmentofsubtrochanteric fractureswithproximalfemurlockingcompressionplate. MalaysOrthopJ.2014;8(2):22–8.