SOCIEDADE BRASILEIRA DE ORTOPEDIA E TRAUMATOLOGIA
w w w . r b o . o r g . b r
Update
Article
Subtrochanteric
fractures
of
the
femur:
update
Paulo
Roberto
Barbosa
de
Toledo
Lourenc¸o
a,
Robinson
Esteves
Santos
Pires
b,c,∗aHospitalQuintaD’Or,RiodeJaneiro,RJ,Brazil
bHospitaldasClínicas,UniversidadeFederaldeMinasGerais,BeloHorizonte,MG,Brazil
cHospitalFelícioRocho,BeloHorizonte,MG,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received23April2015
Accepted23April2015
Availableonline21March2016
Keywords:
Hipfractures/etiology
Hipfractures/diagnosis
Hipfractures/surgery
Hipfractures/classification
a
b
s
t
r
a
c
t
Becauseoftheanatomicalpeculiaritiesofthesubtrochantericregion,treatmentof
frac-turesinthisregionremainschallenging.The undeniableevolutionofimplantshasnot
beenaccompaniedbytheexpecteddecreaseinthecomplicationrate.
The aim of this study was to discuss critical points in detail, such as preoperative
planning,reductiontacticsandthecurrentscientificevidenceconcerning treatmentof
subtrochantericfracturesofthefemur.
©2016SociedadeBrasileiradeOrtopediaeTraumatologia.PublishedbyElsevierEditora
Ltda.ThisisanopenaccessarticleundertheCCBY-NC-NDlicense(http://
creativecommons.org/licenses/by-nc-nd/4.0/).
Fraturas
subtrocantéricas
do
fêmur:
atualizac¸ão
Palavras-chave:
Fraturasdoquadril/etiologia
Fraturasdoquadril/diagnóstico
Fraturasdoquadril/cirurgia
Fraturasdoquadril/classificac¸ão
r
e
s
u
m
o
Devidoàsparticularidadesanatômicasdaregiãosubtrocantérica,otratamentodas
frat-urasnessaregiãopermanecedesafiador.Aincontestávelevoluc¸ãodosimplantesnãofoi
acompanhadapelaesperadadiminuic¸ãonoíndicedecomplicac¸ões.
Oobjetivodopresenteestudoédiscutir,minuciosamente,pontoscríticoscomo
planeja-mentopré-operatório,táticasdereduc¸ãoeevidênciascientíficasatuaisnotratamentodas
fraturassubtrocantéricasdofêmur.
©2016SociedadeBrasileiradeOrtopediaeTraumatologia.PublicadoporElsevierEditora
Ltda.Este ´eumartigoOpenAccesssobumalicenc¸aCCBY-NC-ND(http://
creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
Subtrochantericfracturestakeplaceintheproximalregion
ofthe femur, whose anatomicaldefinition isdifficultand
∗ Correspondingauthor.
E-mail:robinsonestevespires@gmail.com(R.E.S.Pires).
controversial.Fielding1proposedadefinitionthatisstill
fre-quentlyused:thesubtrochantericregioncorrespondstothe
interval betweenthe lessertrochanterand around5–7.5cm
belowit,towardthefemoralisthmus.Thefracturescanextend
http://dx.doi.org/10.1016/j.rboe.2016.03.001
2255-4971/©2016SociedadeBrasileiradeOrtopediaeTraumatologia.PublishedbyElsevierEditoraLtda.Thisisanopenaccessarticle
totheproximalregion(trochantericorfemoralneck)ordistal
region(diaphyseal).1,2
They account for 25% of the proximal fractures of the
femurand theirdistributionisbimodal.Youngmaleadults
involved inhigh-energy traumas present complex fracture
patterns;whereasoldpatients,predominantlyfemales,
gen-erallypresentspiralfractures.1
Duetotheanatomicalpeculiarityand,especially,dueto
thedifficultyinreduction,thetreatmentofsubtrochanteric
fracturesisstillagreatchallengetothetraumatologist,not
onlybecauseofthe osteosynthesisdifficulties, but alsofor
thestillfrequentcomplications.Thenextsectionaddresses
importantaspectsthatwillhelptoexplainthepeculiaritiesof
thetreatmentofthesubtrochantericfractures.
Why
are
their
anatomical
and
biomechanic
characteristics
unique?
Thesubtrochantericregionofthefemurisanareaofgreat
stressconcentrationand,duetoits muscularinsertions, is
subjectedtoseveraldeformingforces.Theclassicdeformities
areflexion(provokedbytheiliopsoas),abduction(bythe
glu-teusmedius),andexternalrotation(bytheexternalrotators)
oftheproximalfragmentofthefemur.Theadductors,inserted
inthedistalregionofthefemur,areresponsibleforthevarus
deformity.2,3
Due to the predominance of cortical bone, the
sub-trochantericregionpresentsamoreprecarious
vasculariza-tion than the transtrochanteric region, which makes the
consolidationofthefracturesdifficult.Complexfractureswith
medialsupportfailurepresentelevatedratesoffixationfailure
andreoperation.2
Is
there
an
ideal
classification
system
for
subtrochanteric
fractures?
Thereareover15describedclassificationsforsubtrochanteric
fractures.1,3–5TheFielding1classificationsubdividesthe
frac-turesaccordingtotheiranatomicallocation:type1fractures
are those at the lesser trochanter level; type 2 fractures
are those located between 2.5 and 5cm below the lesser
trochanter;andtype3fracturesarethoselocatedbetween5
and7.5cmbelowthelessertrochanter.Itsvalueisonly
his-torical,due to its lowreproducibility on account ofethnic
variations.
TheclassificationbyRussell-Taylortakesintoaccountthe
entiretyofthe piriformisfossa (more appropriatelytermed
trochanteric fossa).1 Type I fractures do not extend into
the trochanteric fossa (IA: without extension to the lesser
trochanter;IB:withextensiontothelessertrochanter).TypeII
fracturesextendintothetrochantericfossa(IIA:without
com-minutionofthelessertrochanter;IIB:seriouscomminution
ofthelessertrochanter).Whentheclassificationwascreated,
theauthorssearchedforaguidelineforthemethodof
frac-turefixation with the implants availableatthe time. Type
I fractures, without involvement ofthe trochanteric fossa,
couldbetreatedwithfirst-generationintramedullarimplants
usingthetrochantericfossaasanentrypoint.TypeII
frac-tures,withinvolvementofthetrochantericfossa,shouldbe
treatedwithextramedullaryimplants.Withthedevelopment
and enhancementofintramedullarydevices –second- and
third-generationintramedullary(IM)nails–thisclassification
lostitsprognosticandtherapeuticguidancevalue,sincethe
involvementofthetrochantericfossawasnolongera
coun-terindicationforintramedullarfixation.
TheclassificationbySeinsheimerisperhapsthemostused
andpracticalforsubtrochantericfracturesofthefemur,since
itischaracterizedbythenumberoffracturedfragmentsand
emphasizesnotonlytheinvolvementofthemedialcortex,but
alsoofthelateralcortex.2
Loizouetal.4alsodescribedaclassificationsystembased
onthedegreeofcomminutionofthesubtrochantericfracture.
However,thisclassificationdidnotgainpopularityinthefield.
The AO classification takes into account the bone
(femur=3), the location (diaphysis=2), the energy of the
trauma(A,B,orC),andthemechanism(1,2,or3).Per
con-vention,thesubtrochantericfractureischaracterizedas“1”.
AlthoughitiswidelyusedandrecommendedbytheOTA,
the AOclassificationhasthe disadvantageofincluding the
subtrochanteric fracture in a group of fractures with
dif-ferent mechanical and biological behavior: the diaphyseal
fractures.2
Recently, Guyver et al.5 proposed a classification called
MCG.Thissystemissubdividedintothreetypes:typeI:lesser
and greater trochanter are preserved; type II: the greater
trochanterisinvolved,butthelessertrochanterisintact;type
III:thelessertrochanterisinvolved(mostunstable).
In their original work, these authors also assessed the
intra-andinter-observerreproducibilityoftheMCG,
Russell-Taylor,AO,andSeinsheimerclassifications.Despitethepoor
intra-andinter-observerreproducibilityofallthe
classifica-tions (Kappa0.35), the MCG system presentedthe highest
agreement, followed by the Russell-Taylor, AO, and
Sein-sheimerclassifications.5
Theauthorsbelievethatthereisnotyetanideal
classifi-cationsystemforthesubtrochantericfracturesofthefemur
thatisabletoguidetreatmentandestablishprognosiswith
satisfactory inter-observer reproducibility. In their practice,
the authors have adoptedthe AOclassificationfor easeof
communicationandbecauseitisthereferenceincurrent
pub-lications.
Surgical
vs
.
non-surgical
treatment
Thenon-surgicaltreatmentofsubtrochantericfracturesleads
to deformities caused by shortening and rotational
devia-tion,hinderingthereturntothefunctionalactivitiespriorto
the injury.However,the criticalpointofnon-surgical
treat-ment is related to the morbimortality increase caused by
extended periodsofimmobilization and decubitus.
Atelec-tasis,pneumonia,thromboembolicevents,andbedsoresare
complicationsfrequentlyassociatedwithextendedperiodsof
decubitus.
Currently,the non-surgicaltreatmentofsubtrochanteric
fractures of the femur is an exception, and must be
performedonlyinpatientswithextremelyseriousclinical
co-morbidities that counterindicateanesthetic and/or surgical
When
to
operate
a
patient
with
subtrochanteric
fracture
of
the
femur?
Patient victims of high-energy trauma must be assessed
according to the ATLS protocol. Afterclinical stabilization,
thelocalconditions,suchasskinintegrity,neurovascular
sta-tus,andthedegreeofsofttissueinjury,mustbethoroughly
assessed.
In severely polytraumatized cases, in which even after
initialresuscitationmaneuversthepatientremains
hemody-namicallyunstable,immediateexternalfixationisindicated
fordamagecontrol.
Instablepatients,theidealperiodforthedefinitivefixation
ofthefractureiswithinthefirst48h.If,foranyreason,
defini-tivefixationofthefractureisnotpossiblewithinthisperiod,
skeletaltractionor,preferably,externalfixationisindicated
fortemporarystabilization.2
Khanet al.7reviewed52 studies,withatotal of291,413
patients,anddemonstratedthatsurgeryconductedwithinthe
first48hreducescomplicationsandmortality.
Theauthorsoptforearlyfixationofsubtrochanteric
frac-tures ofthe femur(within the first 48h afterthe trauma)
wheneverpossible.
Which
the
best
fixation
method
for
subtrochanteric
fractures?
The
evolution
of
the
implants
Theplates
Although it was developed for the treatment of
transtrochanteric fractures, DHS has also been widely
usedforthefixationofsubtrochantericfractures.However,
duetothecharacteristicbiomechanicsofthesubtrochanteric
fractures,severalauthors reportedunsatisfactoryresultsin
nearly70%ofthecasesinwhichthisimplantwasused.2As
DHS isa dynamicsystem,progressivemedializationofthe
diaphysisandfixationfailurecanoccur.
ThebladeplateandtheDCS,developedbytheAOgroup,are
viableoptionsforthetreatmentofsubtrochantericfractures,
especiallywhentechniquesofindirectreductionandbiological
fix-ationareused.2
Boopalanetal.8 reportedtheresultsof22patients with
23subtrochantericfracturesofthefemurtreatedwithblade
plates using the minimally invasive biological technique.
Nineteen patients did not need additional surgeries. Two
patientswere reoperated duetovarus reductions,and one
patientunderwentsurgicaldebridementduetoinfection.The
functionalresultswereconsideredexcellentintenpatients,
goodinonepatient,andpoorintwopatients.
Duetoits lowcostand thefamiliarityofsurgeonswith
both the DCS and blade plates, these implants persist as
importantandfrequentfixationoptionsforsubtrochanteric
fractures in Brazil.However, it isworth noting that, when
using blade plates or DCS, minimally invasive techniques
should be preferred in order to preserve the biological
integrity of the region. The conventional approach (open)
promotes important local devascularization and increases
the rates of infection, pseudarthrosis, and osteosynthesis
failure.
Recently,someauthorsreportedtheuseofplateswithfixed
anglescrewsinthetreatmentofsubtrochantericfracturesof
thefemur.
Saini et al.,9 using proximal femur-locking compression
plate (PF-LCP – Sharma Surgicals, India) for the treatment
of comminuted subtrochanteric fractures in 35 patients,
achievedconsolidationinall cases.Twopatientspresented
infection,two presented1-cmshortening, andoneevolved
withviciousconsolidationinexternalrotation.Theauthors
concludedthatbiologicalfixationwithPF-LCPincomminuted
subtrochantericfracturespromotesstablefixation,withahigh
rateofconsolidationandlowrateofcomplications.
Recently,Wirtzetal.10 reportedahighrateof
complica-tionswiththeopenreductiontechniqueandinternalfixation
withPF-LCP(Synthes,WestChesterPA,USA).Of19patients
withsubtrochantericfractureswhounderwentfixationwith
PF-LCP, seven presented important complications, such as
infection, cut-out,and varus collapse,requiring new
surgi-calprocedures.Thoseauthorsemphasizedthat,contraryto
intramedullary implants, PF-LCPsdo notallowfor fracture
accommodation,which iscritical forconsolidation in
frac-tureswithlossofposteromedialsupport.
Amit etal.11 described theuse ofthe LessInvasive
Sta-bilization System (LISS – DePuy Synthes) plate, originally
developed fordistal fractures ofthe femur, in the fixation
ofsubtrochantericfractures.Inanon-conventionalmanner,
thoseauthorsperformedosteosynthesiswiththe
contralat-eralreverseplateandemphasizedthepotentialadvantages
ofthedescribedtechnique:theeasinessofaccommodationof
theplateintheproximalregionofthefemur,thefactthatthe
femoralradiuscurvatureisfollowedbytheplatecurvature,
andthepossibilityoffixationofosteoporoticboneswiththe
useofmultiplanarfixed-anglescrews.
IMnails
In1964,Zickel12developedanIMnailspecificallyforthe
treat-mentofsubtrochantericfractures.Thissystemisconsidered
theprecursoroftheintramedullaryimplantscurrentlyused
forsubtrochantericfractures.
Wiss and Brien13 revolutionized the treatment of
sub-trochanteric fractures with the use of IM nails on the
contralateralside.Wheninverted,thenailholeforproximal
blockageallowedforthepositioningofascrewdirectedtoward
the femoralneck.Thus,thoseauthors couldtreatfractures
that,accordingtotheRussel-Taylorclassification,were
coun-terindicated forintramedullaryfixation duetotrochanteric
fossainvolvement.
Although initially developed for the treatment of
transtrochanteric fractures, cephalomedullary nails were,
naturally, used in subtrochanteric fractures. They quickly
gainedpopularityand,duetotheirfavorablebiomechanical
properties and minimally invasive application techniques,
presentedsatisfactoryresultswithlowreoperationrates.
Umeretal.14reportedtheresultsofthetreatmentof
sub-trochanteric fractures with IM nails with spiral slides for
cephalicblockage.Intheirstudy,with33patients,theauthors
aftersurgery,withmeansurgicaltimeof2.4handmean
hos-pitalizationofsevendays.
Borens et al.15 treated 90 patients with subtrochanteric
fractureofthe femurusing GammaNail(Stryker)IM nails.
With a mean follow-up of two years, no infections were
reported. One patient presenteda fracture belowthe nail,
which was exchanged for a longer nail. Two patients
pre-sentedosteosynthesisfailureduetovarusreduction.Oneof
themwastreatedwithnailreplacementandbonegraft,while
theotherwastreatedwithremovalofthenail,blade-plating
osteosynthesis,andbonegraft.All87otherpatientspresented
consolidationwithprimarysurgery.Theauthorsemphasized
that, due to the favorable biomechanical properties ofthe
implant(intramedullarytutor),earlyrehabilitationandload
areallowedeveninosteoporoticpatients.
Is
there
an
ideal
entry
point
for
cephalomedullary
nails?
Thedefinitionofthenail’sentrypointdependsontheimplant
chosenforthefixation.Classically,straightnailsutilizethe
piriformisfossa(moreappropriatelycalledtrochantericfossa)
asentrypoint16;nailswith6◦lateralinclinationenterthrough
thetopofthegreatertrochanter;and nailswith10◦ lateral
inclinationenterlaterallytothegreatertrochanter.
However,Streubeletal.,17whenanalyzing50X-raysof
nor-malhips,demonstrated thattheidealentrypointfornails
with6◦lateralinclinationwasslightlymedialtothetopofthe
greatertrochanterin70%ofthestudiedpatientsandlateral
in23%.
Theauthors believethat preoperative surgical planning
isessential topreventadditionaldeformitiescaused byan
unsuitableentrypoint.
Current
evidence
Herscovicietal.18conductedaretrospectivestudyinwhich
theycompared intra- and extra-medullaryimplants inthe
treatment of subtrochanteric fractures of the femur. The
authorsdemonstratedthat,althoughintramedullaryfixation
wasquickerandhadlessbleeding,thefunctionalresultsand
thecomplicationratesweresimilar.Theyemphasizedthatthe
surgeonmustcarefully assessthe fracturepattern to
iden-tifywhenthemostfamiliartechniquewillleadtosatisfactory
functionalresultswithlowcomplicationrates.
Mirbolooketal.19comparedfunctionalresultsandrateof
complicationsinthetreatmentofsubtrochantericfracturesof
thefemurwithtwosurgicaltechniques:openreductionand
internalfixationwith trochantericPF-LCP (DePuySynthes),
andfixationwithcephalomedullarynailsusingthebiological
technique(indirectreduction).Therewasnostatistically
sig-nificantdifferencebetweenbothgroupsregardingfunction,
consolidation,andcomplications.
Kuzyketal.20assessedstudiesthatcomparedintra-and
extra-medullaryfixationsforthetreatmentofsubtrochanteric
fracturesofthefemur.Thesystematicrevisionconsistedof
threestudieswithlevelofevidenceIandninewithlevelIV.
ThoseauthorsreportedalevelofrecommendationBfavorable
tointramedullaryimplantsregardingthesurgerytimeandthe
ratefixationfailure.
In the treatment of subtrochanteric fractures, the
authors of the present study prefer fixation with long
cephalomedullarynailsduetotheirbiomechanicalproperties
andtothepossibilityofminimallyinvasivefixation.
However, muchmore important than the choice of the
implantisthequalityoffracturereduction.
Inawell-reducedfracture,theliteraturedemonstratesthat
the resultsofintra- andextra-medullaryfixationusing the
biologicaltechnique(minimallyinvasive)aresimilar.
Traction
table
or
conventional
radiolucent
table?
There areseveralpossiblepositionsforthe fixationof
sub-trochantericfractures.Thechoiceshouldbebasedonthetype
offixation(intra-orextra-medullary)andontheexperience
ofthesurgeonwiththechosentechnique.Themost
impor-tantfactorsarethatappropriateimagescanbeobtainedand
thatthepositioningofthetrunkandlimbsdoesnothinder
thesurgicalprocedure.
Tractiontable
Thepatientcanbepositionedinthe“banana”position,with
thetrunkadducted,thesuperioripsilaterallimbfixedin
shoul-deradduction,andtheinferiorcontralaterallimbininferior
position(“scissors”position).
Thispositioningfacilitatestheplacingoftheimage
inten-sifierbothforcreatingtheentrypointandtheproximaland
distalblockagesoftheIMnail.
Theadductionofthefracturedinferiorlimbtofacilitate
theentrypointshouldbeavoidedduetothevarusdeviation
causedbythispositioning.
Conventionaltable
Fixationispossiblebothinsupinepositionandincomplete
lateraldecubitusorobliquelateraldecubitus.Inlateral
decu-bitus,althoughtheentrypointiseasier,thesurgeonmustbe
carefulthatthefractureisnotinmedialangulation(varus)
duetotheactionofgravityandmusculartraction.
Inthesupineposition,acushioncanbeplacedtofacilitate
thecreationoftheentrypointandtheproximalblockagein
intramedullaryfixation.Thedisadvantageofthesupine
posi-tionistheneedforanassistanttotractionthememberfor
fracturereduction.Asanoptiontomanualtraction,the
sur-geoncanuseanAOdistractor.
Baratz et al.21 assessed radiation exposure, comparing
thelateralandsupinepositioningforthetreatmentof
sub-trochantericfractures,andobservedlowerradiationexposure
inthesupineposition.
Thereisnoconsensusintheliteratureregardingthebest
positioningofthepatientandtheneedforatractiontable.The
surgeonshouldpositionthepatientbasedonthetechnique
withwhichhe/sheismostfamiliar.
Inthispractice,theauthorsprefertousethetractiontable
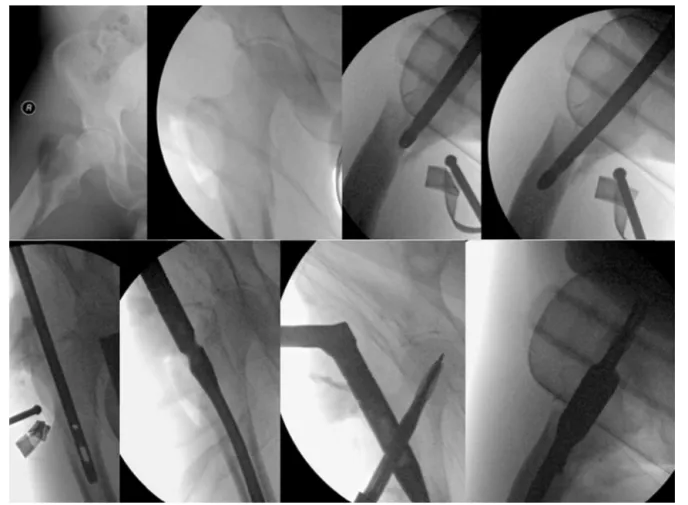
Fig.1–Reductionofthesubtrochantericfracturewithcephalomedullarynail.
inferiorlimbsin“scissors”position). Withthis positioning,
boththeintra-andextra-medullaryfixationsarepossible,and
thesurgeonhasanopensurgicalfieldfortheacquisitionof
perioperativeimages.
How
to
reduce
subtrochanteric
fractures?
Despitetheevolutionofthefixationmethods,allauthors
rec-ognizethatthereductionisthemostimportantisolatedfactor
in the prognosis of subtrochanteric fractures.The authors
emphasizetheneedtoaimforfracturereductionwith
restora-tion of the cervico-diaphyseal angle and of the shaft, in
additiontothecorrectionoftherotationandflexionofthe
proximalfragment,usingmethodsthatdonotcausegreater
biologicaldamage.
Riehletal.,22inaretrospectivestudyassessingtheresults
ofintramedullaryfixationin35patients,observedthat
unsa-tisfactoryreductions–thosewithover10◦inanyplane–led
toproblemsintheconsolidation.
Miedeletal.,6whenanalyzingtheresultsofintramedullary
fixationinthetreatmentofsubtrochantericfracturesinthe
elderly,observedgoodreductionin50%andacceptable
reduc-tionin50%.Inthegroupwhosereductionwasconsideredby
thesurgeonsasgood,nopatientswerereoperated,whilein
thegroupwithacceptablereduction,23%neededreoperation.
Thoseauthorsemphasizedtheimportanceofasatisfactory
reduction,sincean“acceptable”reductioncanleadtotheneed
foranewsurgeryinone-quarterofthepatients.
Duetothecountlessdeformingforcesthatactinthe
sub-trochantericregion,theindirectreductionofthefracturesis
usuallydifficult.
However,theevolutionofimplantshasbeenaccompanied
bythe evolution inreductioninstruments.Currently,there
are instrumentsthatallowforaneffectivereductionofthe
fracturewithminimallyinvasivetechniques.
Yoon et al.23 reportedthe resultsofthefixationof
sub-trochantericfracturesofthefemurusingWeberclampsfor
the reduction.Infractures withpredominanceofflexionof
theproximalfragment,theauthorsperformeda5cmlateral
incisionforintroducingtheclamps.Infractureswithalong
spiralcomponentinthesagittalplan,theauthorsrecommend
alateralincisionandintroductionofahemostatrestedonthe
anteriorcortexofthefemur,towardthemedialcortex.
Subse-quently,theclampsmustbeliftedtocorrecttheflexionand
theexternalrotationoftheproximalfragmentofthefemur.A
newanteriortransquadricipitalincisionisperformedforthe
introductionoftheWeberclamp.Inastudywithtenpatients
operatedwiththistechnique,themeantimeforreductionwas
12min(betweensixand21min)andallfracturesconsolidated
withonlyapartiallossofreduction.Itisimportanttopoint
outthatthereductionforcepsmustbemaintaineduntilthe
Fig.2–UseofaSchanzscrewtoreducevarus.
Ball-spike pushers, Schanz screws, or Steinmann pins,
placedthroughananteriorpunctiformaccessroute,canbe
usedasajoysticktoreducetheflexionoftheproximal
frag-mentinsubtrochantericfracturesofthefemur.
Inpatientswithgoodbonequalityandintegrityofthe
pos-terior cortex of the femur, the nail itself can be used as an
instrumenttoreducetheflexionoftheproximalfemoral
frag-ment(Fig.1).
Forthecorrectionofvarus,ball-spikepushersorSchanz
screwscanbeused,asillustratedinFig.2.
Someauthorsaddcerclagetomaintainthereductionof
thefracture.24,25 Nonetheless,therearequestionsregarding
thepotentialbonedevascularizationcausedbycerclage.
Tomás et al.24 performed cerclage in 12 patients who
underwent osteosynthesis withcephalomedullary nails for
thefixationofsubtrochantericfractures.Allthefractureswere
consolidatedandtherewerenosuperficialordeepinfections.
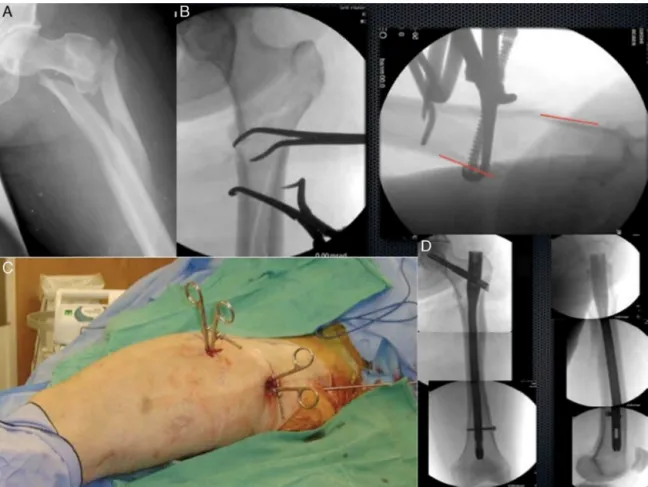
Fig. 3 illustrates the treatment of a complex
sub-trochantericfracturereducedwithpercutaneousclampsand
fixedwithalongcephalomedullarynail.
Seyhanetal.25comparedtheresultsofthetreatmentof
subtrochantericfracturesofthefemurwithIMnailsandthree
reduction techniques: forceps, cerclage, and Poller screws.
Thegroupinwhichthereductionforcepswereusedhadthe
longestintervaluntiltotalload(p=0.032)andlowestHarriship
scoreafteroneyear(p=0.02).Conversely,thePollergroup
pre-sentedlongestsurgicaltime.Therewasnodifferenceamong
thegroupsregardingthequalityofthereduction,
consolida-tiontime,complications,andtherateofreoperations.
Complications
Even with modern implants,the complication ratesin the
treatment of the subtrochanteric fractures remain high
Fig.3–ImageskindlysharedbyProfessorGeraldLang,fromtheUniversityofWisconsin.(A)Complexsubtrochanteric fracture;(B)X-raysoftheproximalfemurinanteroposteriorandprofileshowingthereductionwithforceps;(C)Imagesof thethighofthepatientshowingpercutaneousintroductionoftheforceps,anteriorandlaterally;(D)Imagesofthe
(around 21%). Infection, pseudarthrosis, vicious
consolida-tion, and loss of the reduction are the most frequent
complications.2
Regardlessofthefixationmethod,thequalityofthe
reduc-tion lowers the stress on the implant, increases the bone
contact,andmakestheconsolidationeasier.
Earlyfixationfailuregenerallyresultsfromtechnical
prob-lemsrelatedwiththesurgicalprocedure.Latefailuresoccur
asaconsequenceofunsatisfactoryreduction,lowbonestock,
inadequate choice of implant, complex fracture patterns,
smoking,andpoorlocalvascularization.2
Z-effectandreverse Z-effectarecomplicationsresulting
fromthetreatmentofproximalfracturesofthefemurwith
cephalomedullaryimplantsthathavetwocephalicblockage
screws.Thesecomplicationshavebeendescribedas
migra-tions of the cephalic screws inopposite directions due to
factorssuchaslowbonestock,excessivelylateralentrypoint,
varusreductions,andseveremedialcomminution.26
Anotherdescribedcomplicationistheimpingementofthe
nailintheanteriorcortexinthedistalthirdofthefemur.
Stud-ieshavedemonstrated thatpatientsoflowstature (<1.6m,
especiallywomenandAsians)haveincreasedradiusof
cur-vatureofthefemur,whichmightpredisposethemtodistal
femoralfracturesduetotheimpingementofthenailinthe
anterior cortexinthe distal thirdofthe femur. Nails with
unsuitableradialcurvature,aswellasincorrectentrypoint,
arealsoriskfactorsforthiscomplication.27,28
Final
considerations
Due to the unfavorable anatomical peculiarities, despite
the development of new implants, the treatment of
sub-trochantericfracturesofthefemurstillpresentsanelevated
rateofcomplicationsandremainschallenging.
Regardlessofthestabilityprincipleandofthemethod
cho-senfortreatmentofthesubtrochantericfracture,thekeypoint
toreducetheriskofcomplicationsisthequalityofthe
reduc-tion.
Wheneverpossible,indirectreductionwithpreservationof
thesoft-tissueenvelopemustbeattempted.Ifnotpossible,
reductiontechniqueswithpercutaneousclampsorcerclage
canbeused.
Even though blade plates, DCS, or blocked trochanteric
plates remain as viable options for the treatment of
sub-trochantericfractures,theIMnails,duetotheirbiomechanical
propertiesandminimallyinvasivefixationtechnique,present
advantagessuchaslowersurgerytimeandlowerrateof
reop-erations.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1. FieldingJW.Subtrochantericfractures.ClinOrthopRelatRes. 1973;(92):86–99.
2.JoglekarSB,LindvallEM,MartirosianA.Contemporary managementofsubtrochantericfractures.OrthopClinNorth Am.2015;46(1):21–35.
3.RochaLR.Fraturasubtrocantérica.Fixac¸ãocomhaste intramedular.OrtoTrauma:SBOT;2013:19–22.
4.LoizouCL,McNamaraI,AhmedK,PryorGA,ParkerMJ. Classificationofsubtrochantericfemoralfractures.Injury. 2010;41(7):739–45.
5.GuyverPM,McCarthyMJ,JainNP,PoulterRJ,McAllenCJ, KeenanJ.Isthereanypurposeinclassifyingsubtrochanteric fractures?Thereproducibilityoffourclassificationsystems. EurJOrthopSurgTraumatol.2014;24(4):513–8.
6.MiedelR,TörnkvistH,PonzerS,SöderqvistA,TidermarkJ. Musculoskeletalfunctionandqualityoflifeinelderly patientsafterasubtrochantericfemoralfracturetreatedwith acephalomedullarynail.JOrthopTrauma.2011;25(4): 208–13.
7.KhanSK,KalraS,KhannaA,ThiruvengadaMM,ParkerMJ. Timingofsurgeryforhipfractures:asystematicreviewof52 publishedstudiesinvolving291,413patients.Injury. 2009;40(7):692–7.
8.BoopalanPR,JepegnanamTS,NithyananthM,VenkateshK, CherianVM.Functionaloutcomeofbiologicalcondylarblade platingofsubtrochantericfractures.JOrthopSci.
2012;17(5):567–73.
9.SainiP,KumarR,ShekhawatV,JoshiN,BansalM,KumarS. Biologicalfixationofcomminutedsubtrochantericfractures withproximalfemurlockingcompressionplate.Injury. 2013;44(2):226–31.
10.WirtzC,AbbassiF,EvangelopoulosDS,KohlS,SiebenrockKA, KrügerA.Highfailurerateoftrochantericfracture
osteosynthesiswithproximalfemorallockingcompression plate.Injury.2013;44(6):751–6.
11.AmitS,ShehkarA,VivekM,ShekharS,BirenN.Fixationof subtrochantericfracturesintwopatientswithosteopetrosis usingadistalfemorallockingcompressionplateofthe contralateralside.EurJTraumaEmergSurg.2010;36:263–9.
12.ZickelRE.Anewfixationdeviceforsubtrochantericfractures ofthefemur:apreliminaryreport.ClinOrthopRelatRes. 1967;(54):115–23.
13.WissDA,BrienWW.Subtrochantericfracturesofthefemur. Resultsoftreatmentbyinterlockingnailing.ClinOrthopRelat Res.1992;(283):231–6.
14.UmerM,RashidH,ShahI,QadirI.Useoffemoralnailwith spiralbladeinsubtrochantericfractures.ActaOrthop TraumatolTurc.2014;48(1):32–6.
15.BorensO,WettsteinM,KombotC,ChevalleyF,MouhsineE, GarofaloR.Longgammanailinthetreatmentof
subtrochantericfractures.ArchOrthopTraumaSurg. 2004;124(7):443–7.
16.AnsariMoeinCM,GerritsPD,tenDuisHJ.Trochantericfossa orpiriformfossaofthefemur:timeforstandardised terminology?Injury.2013;44(6):722–5.
17.StreubelPN,WongAH,RicciWM,GardnerMJ.Istherea standardtrochantericentrysitefornailingofsubtrochanteric femurfractures?JOrthopTrauma.2011;25(4):202–7.
18.HerscoviciDJr,PistelWL,SandersRW.Evaluationand treatmentofhighsubtrochantericfemurfractures.AmJ Orthop(BelleMeadNJ).2000;299Suppl.:27–33.
19.MirbolookA,SiavashiB,JafarinezhadAE,JahromiSK, FarahmandM,RadMR,etal.Subtrochantericfractures: comparisonofproximalfemurlockingplateand
intramedullarylockingnailfixationoutcome.IndianJSurg. 2013:1–5.
20.KuzykPR,BhandariM,McKeeMD,RussellTA,SchemitschEH. Intramedullaryversusextramedullaryfixationfor
21.BaratzMD,HuYY,ZurakowskiD,AppletonP,RodriguezEK. Theprimarydeterminantsofradiationuseduringfixationof proximalfemurfractures.Injury.2014;45(10):1614–9.
22.RiehlJT,KovalKJ,LangfordJR,MunroMW,KupiszewskiSJ, HaidukewychGJ.Intramedullarynailingofsubtrochanteric fractures–doesmalreductionmatter?BullHospJtDis(2013). 2014;72(2):159–63.
23.YoonYC,JhaA,OhCW,DuraiSK,KimYW,KimJH,etal.The pointedclampreductiontechniqueforspiralsubtrochanteric fractures:atechnicalnote.Injury.2014;45(6):1000–5.
24.TomásJ,TeixidorJ,BatallaL,PachaD,CortinaJ.
Subtrochantericfractures:treatmentwithcerclagewireand longintramedullarynail.JOrthopTrauma.2013;27(7):e157–60.
25.SeyhanM,UnayK,SenerN.Comparisonofreduction methodsinintramedullarynailingofsubtrochantericfemoral fractures.ActaOrthopTraumatolTurc.2012;46(2):113–9.
26.PiresRE,SantanaEOJr,SantosLE,GiordanoV,Balbachevsky D,DosReisFB.Failureoffixationoftrochantericfemur fractures:clinicalrecommendationsforavoidingZ-effectand reverseZ-effecttypecomplications.PatientSafSurg. 2011;5:17.
27.TyagiV,YangJH,OhKJ.Acomputedtomography-based analysisofproximalfemoralgeometryforlateral impingementwithtwotypesofproximalfemoralnail anterotationinsubtrochantericfractures.Injury. 2010;41(8):857–61.