SOCIEDADE BRASILEIRA DE ORTOPEDIA E TRAUMATOLOGIA
w w w . r b o . o r g . b r
Update
Article
Bone
graft
in
the
treatment
of
nonunion
of
the
scaphoid
with
necrosis
of
the
proximal
pole:
a
literature
review
夽
Antônio
Lourenc¸o
Severo
a,∗,
Marcelo
Barreto
Lemos
a,
Osvandré
Luiz
Canfield
Lech
a,
Danilo
Barreto
Filho
b,∗,
Daniel
Paulo
Strack
c,
Larissa
Knapp
Candido
aaInstitutodeOrtopediaTraumatologiadePassoFundo,HospitaldoTrauma,PassoFundo,RS,Brazil
bHospitalUniversitárioDr.MiguelRietCorreaJr.,RioGrande,RS,Brazil
cCentrodeEspecialidadesdeOrtopediaeTraumatologia,Ijuí,RS,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received5September2016
Accepted10November2016
Availableonline27October2017
Keywords:
Scaphoidbone
Osteonecrosis
Fracturenonunion
Bonetransplantation
a
b
s
t
r
a
c
t
Scaphoidfracturesarethemostcommonfracturesofthecarpalbones,correspondingto
60%.Ofthese,10%progresstononunion;moreover,3%canpresentnecrosisoftheproximal
pole.Therearevariousmethodsoftreatmentusingvascularizedandnon-vascularizedbone
grafts.
Toevaluateandcomparetherateofscaphoidconsolidationwithnecrosisoftheproximal
poleusingdifferentsurgicaltechniques.
Theauthorsconductedareviewoftheliteratureusingthefollowingdatabases:PubMed
andBIREME/LILACS,where13caseserieswereselected(tenwithuseofvascularizedbone
graftsandthreeofnon-vascularizedbonegrafts), accordingtoinclusionandexclusion
criteria.
InmostcasesVBGswereused,especiallythosebasedonthe1,2intercompartmental
supraretinacularartery,duetogreaterreproducibilityinperformingthesurgicaltechnique.
©2017SociedadeBrasileiradeOrtopediaeTraumatologia.PublishedbyElsevierEditora
Ltda.ThisisanopenaccessarticleundertheCCBY-NC-NDlicense(http://
creativecommons.org/licenses/by-nc-nd/4.0/).
Enxerto
ósseo
no
tratamento
da
não
consolidac¸ão
do
escafoide
com
necrose
do
polo
proximal:
revisão
da
literatura
Palavras-chave:
Ossoescafoide
Osteonecrose
Fraturasnãoconsolidadas
Transplanteósseo
r
e
s
u
m
o
Asfraturasdoescafoidesãoasmaiscomunsdosossosdocarpo,correspondema60%.
Dessas,10%evoluemparanãoconsolidac¸ão;alémdisso,3%podemapresentarnecrosedo
poloproximal.Existemváriosmétodosdetratamentocomenxertosósseos,vascularizados
enãovascularizados.
夽
StudyconductedattheInstitutodeOrtopediaeTraumatologia,HospitaldoTraumadePassoFundo,PassoFundo,RS,Brazil.
∗ Correspondingauthors.
E-mails:antoniolsevero@gmail.com(A.L.Severo),drdanilo.cirurgiadamao@gmail.com(D.BarretoFilho).
http://dx.doi.org/10.1016/j.rboe.2016.11.011
2255-4971/©2017SociedadeBrasileiradeOrtopediaeTraumatologia.PublishedbyElsevierEditoraLtda.Thisisanopenaccessarticle
Avaliarecompararastaxasdeconsolidac¸ãodoescafoidecomnecrosedopoloproximal
comdiferentestécnicascirúrgicas.
Fez-seumarevisãonaliteraturanasbasesdedadosPubMedeBireme/Lilacs,dasquais
foramselecionadas13sériesdecasos(dezcomusodeenxertosósseosvascularizadosetrês
enxertosósseosnãovascularizados),deacordocomoscritériosdeinclusãoeexclusão.
Enxertos ósseosvascularizados foramusadosnamaioriados casos,principalmente
naquelesbaseadosnaartériaintercompartimentalsuprarretinacular1e2,devidoàmaior
reprodutibilidadenatécnicacirúrgica.
©2017SociedadeBrasileiradeOrtopediaeTraumatologia.PublicadoporElsevier
EditoraLtda.Este ´eumartigoOpenAccesssobumalicenc¸aCCBY-NC-ND(http://
creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
Scaphoidfracturesaremostcommonfracturesofthecarpal
bones,accountingfor60%ofsuchfractures.Although
con-solidationcanoccurwithouttheneedforsurgicaltreatment,
somecaseseriesindicatenonunionratesofupto10%.1Recent
datasuggestthatthemainriskfactorfornonunionisfragment
dislocation,whichisassociatedwithnonunionratesofupto
55%.2
Avascularnecrosishasanestimatedoccurrenceof3%in
allcasesofscaphoidfractures;itoccurspredominantlyinthe
proximalpole,afactattributedtothepeculiarvascularization
ofthisbone.Studiesonthesubjectdescribethatthearterial
supplyofthe scaphoid flowsthrough threevessels(lateral
volar,dorsalanddistal),classifiedaccordingtotheirspatial
relationwiththescaphoid.3,4Morerecently,somestudieshave
showntheexistenceoftwoarteries:onecompletelydorsal
andthesecondlimitedtothetubercle.5
Forthe diagnosis ofavascularnecrosis,the useof
mag-neticresonanceimaging(MRI)hasbeenrecommended,which
hasanaccuracyofupto68%,increasingto83%when
associ-atedwiththeuseofgadoliniumcontrast.However,thegold
standard is anintraoperative evaluation ofthe absence of
bleedingintheproximalfragment.6Severaltreatment
tech-niqueshavebeendescribed,withbothvascularized(VBG)and
non-vascularized(NVBG)bonegrafts.
Inarecentsystematicreview,Merreletal.7concludedthat
therateofconsolidationofscaphoidfractures thatevolved
tononunionwas88%inVBGvs.47%inNVBG.Inlightofsuch
data,thisstudyaimedtoperformanupdatedliteraturereview
ontheratesofconsolidationusingthedifferenttypesofgrafts
(VBGandNVBG)usedforthetreatmentofnonunionofthe
scaphoidwithnecrosisoftheproximalpole.
Methods
The current medical literature in the PubMed and
BIREME/LILACSdatabaseswassearchedusingthefollowing
keywordcombinations(Table1)8:
1. Bonegraftscaphoid
2. Nonunionscaphoid
3. Vascularizedbonegraftnonunionscaphoid
4. Cancellousbonegraftscaphoid
5. Pseudoartrosisscaphoid
Allarticlesthatdidnotmentiontheuseofbonegraftsfor
thetreatmentofnonunionofthescaphoid,thosethatreferred
theuseofimmatureskeletalgraft,thosethatcitedtheuseof
bonegraftsinothercarpalpathologies,andthosepublished
over20yearswereexcluded.
Thus,thefollowingselectionwasobtained(Table1).
Allthearticlesthatdidnotrefertoavascularnecrosisof
theproximalpolewereexcluded.
Therefore,13articleswereincluded.
Analysis
of
results
Afteraliteraturereview,itwasobservedthatinthelasttwo
decades therehasbeen atendency towardthe useofVBG
incasesofnonunionofthescaphoid,especiallywhenthere
aresignsofavascularnecrosisoftheproximalpole,themain
indicationfortheuseofthesegrafts.
The literaturereview evidenced the use of several VBG
techniques, among them: VBG based on capsular
circula-tion,VBGbasedonthemetaphysealcirculationofthedistal
radius,VBGbasedonthevolarcirculationofthedistalradius,
VBGbased onthe 1,2intercompartmentalsupraretinacular
artery (1,2 ICSRA), and VBG originating from the femoral
condyle and from the iliac crest (the latter made through
microanastomosisontheradialartery).Alltechniquesshow
highconsolidationrates,withameanof89%(Table2).
Steimannetal.9usedthedistalradiusgraftwiththe1,2
ICSRA technique described by Zaindenberg; these authors
achievedaconsolidationrateof100%in44casestreatedwith
thistechnique.Ofthese,eighthadproximalpolenecrosis.Tsai
etal.,10alsousingthe1,2ICRSAtechnique,achieved
consoli-dationratesof80%(fouroutoffivepatients).Liangetal.11used
thesametechniqueasdescribedabove,obtaininga
consoli-dationrateof100%.Uerpairojkitetal.12alsousedthevascular
grafttechniquebasedonthe1,2ICRSAandachieveda
consol-idationrateof100%intentreatedpatients,fivewithnecrosis
oftheproximalpoleofthescaphoid(Table2).
However,thestudydevelopedbyStrawetal.,13 inwhich
a vascularized bone graft was also used based on the 1,2
ICSRA, presentedconsolidationrateswellbelowthose
pre-viouslymentioned.That studyobtainedconsolidationrates
Table1–SearchincurrentmedicalliteraturethroughthePubMedandBIREME/LILACSdatabases.
Termusedinresearch Numberofarticles inPubMed
SelectedPubMed articles
Numberofarticles inBIREME
SelectedBIREME articles
Bonegraftscaphoid 267 22 167 24 Nonunionscaphoid 273 19 182 18 Vascularizedbonegraftnonunion
scaphoid
22 20 34 16
Structuralbonegraftnonunion scaphoid
10 8 6 5
Pseudoartrosisscaphoid 66 10 273 13
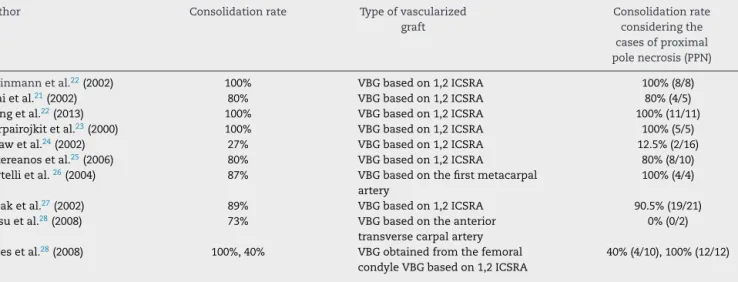
Table2–Consolidationrateaccordingtothetechniqueusedforvascularizedbonegrafting.Vascularizedbonegraft (VBG),1,2intercompartmentalsupraretinacularartery(1,2ICSRA).
Author Consolidationrate Typeofvascularized graft
Consolidationrate consideringthe casesofproximal polenecrosis(PPN)
Steinmannetal.22(2002) 100% VBGbasedon1,2ICSRA 100%(8/8)
Tsaietal.21(2002) 80% VBGbasedon1,2ICSRA 80%(4/5)
Liangetal.22(2013) 100% VBGbasedon1,2ICSRA 100%(11/11)
Uerpairojkitetal.23(2000) 100% VBGbasedon1,2ICSRA 100%(5/5)
Strawetal.24(2002) 27% VBGbasedon1,2ICSRA 12.5%(2/16)
Sotereanosetal.25(2006) 80% VBGbasedon1,2ICSRA 80%(8/10) Bertellietal.26(2004) 87% VBGbasedonthefirstmetacarpal
artery
100%(4/4)
Ribaketal.27(2002) 89% VBGbasedon1,2ICSRA 90.5%(19/21)
Jessuetal.28(2008) 73% VBGbasedontheanterior transversecarpalartery
0%(0/2)
Jonesetal.28(2008) 100%,40% VBGobtainedfromthefemoral condyleVBGbasedon1,2ICSRA
40%(4/10),100%(12/12)
assessingonlycaseswithsignsofproximalpolenecrosis,this
percentagedecreasedto12.5%(Table2).
Sotereanosetal.14describedhighconsolidationrates(80%)
withdistalradiusbonegraftbasedoncapsularcirculation;ten
caseswereevaluated,allofwhichhadproximalpolenecrosis.
Theauthorsemphasizetheabsenceofsmallvesseldissection
asagreatadvantageofthistechnique(Table2).
Removing the bone graft from the base of the thumb
and using a vascularization technique based on the first
metacarpalartery,Bertellietal.15reachedaconsolidationrate
of87%inaseriesof24patients.Fourcaseswithproximalpole
necrosiswereincludedinthatstudy,andradiographic
con-solidationwasachievedinall ofthem.Despitetheneedto
dissectasmallvessel,theauthorsreportasanadvantagethe
presence,inallcases,ofthefirstmetacarpalartery(Table2).
InthestudybyRibaketal.,16aprospectiveevaluationof
46 patients treated with VBG based on the 1,2 ICSRSA vs.
40patientstreatedwithanNVBGextractedfrom thedistal
radius,theauthorsobservedastatisticallysignificantresult
infavoroftheuseofaVBG,witharateof89.1%vs.72.5%
inthosetreatedwithNVBG.Withinthegroupofpatientsin
whomVGBwasused,21hadproximalpolenecrosis;ofthese,
consolidationwasachievedin19(90.5%;Table2).
InthestudybyJessuetal.17withVBGofthevolarportion
ofthe distalradiusbasedonthe anteriortransversecarpal
artery,aconsolidationrateof73%wasobtainedin30cases.
Inthatseries, twocaseshadsigns ofavascularnecrosisof
theproximalpole,andnonepresentedconsolidationwiththe
proposedtreatment(Table2).
Intheirstudy,Jonesetal.18comparedtheratesof
consol-idationintwogroupstreatedwithVBG.Inonegroupof22
patients,thegraftwastakenfromthedistalradiusandits
vas-cularizationwasbasedonthe1,2ICSRA;intheothergroup,
with12patients,afreebonegraftfromthefemoralcondyle
wasused.Astatisticallysuperiorresultwasobtainedwhenthe
graftwasobtainedfromthefemoralcondyle,whichreached
aconsolidationrateof100%,vs.40%inthegroupinwhichthe
graftwasobtainedfromthedistalradius(Table2).
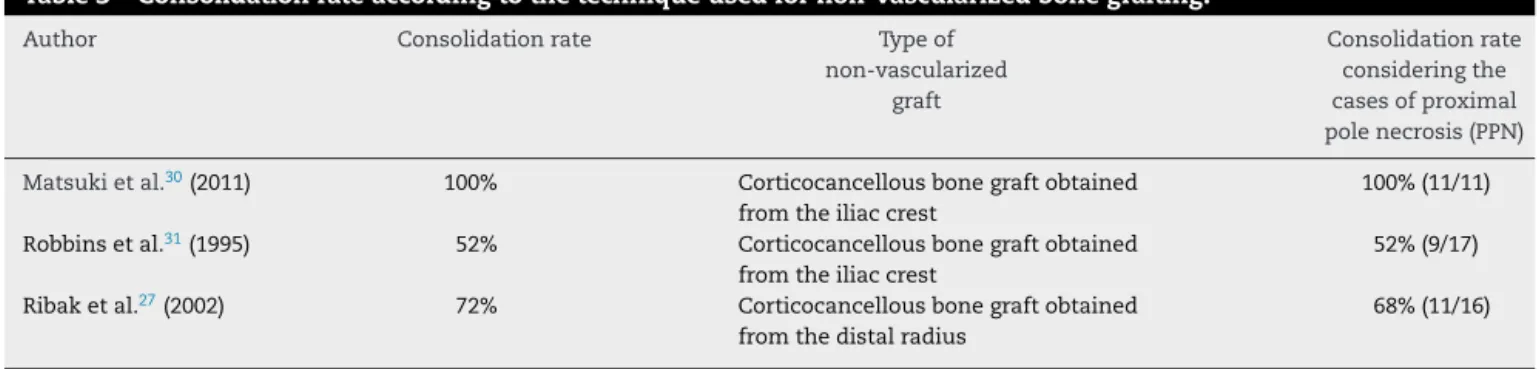
Regarding thetechniquesthatdescribetheuseofNVBG
forthe treatment ofnonunionofthe scaphoid with
proxi-mal polenecrosis, onlythreecase serieswere retrieved in
the presentstudy,whichdidnotpresent definedexclusion
criteria. Matsukietal.19 evaluatedtheconsolidationrateof
proximalscaphoidpolefractures,inwhichNVBGwas
asso-ciatedwiththefixationofaHerbertscrew;11patientswere
evaluatedandconsolidationwasobservedinall(Table3).With
thesametechnique,Robbinsetal.20investigated17patients
withaone-yearfollow-upandobservedaconsolidationrate
of52%(Table3).Ribaketal.16assessedtheconsolidationrate
usingNVBG in40 patients;ofthese,16had necrosisofthe
proximalpoleand11achievedconsolidation(Table3).
Discussion
Evidence supports the hypothesis that the arterial supply
ofthe proximalpoleis poorwhencomparedwiththe
Table3–Consolidationrateaccordingtothetechniqueusedfornon-vascularizedbonegrafting.
Author Consolidationrate Typeof non-vascularized
graft
Consolidationrate consideringthe casesofproximal polenecrosis(PPN)
Matsukietal.30(2011) 100% Corticocancellousbonegraftobtained fromtheiliaccrest
100%(11/11)
Robbinsetal.31(1995) 52% Corticocancellousbonegraftobtained fromtheiliaccrest
52%(9/17)
Ribaketal.27(2002) 72% Corticocancellousbonegraftobtained fromthedistalradius
68%(11/16)
entirelyintra-articular, iscoveredbyhyaline cartilage with
onlyoneligamentinsertion,theradioscapholunateligament.
Therefore,itsvascularizationiscompletelydependentonthe
intraosseouscirculation.Finally,whenthesolutionof
continu-ityislostduetodeviatedfracture,thiscirculationisimpaired,
favoringnonunion.21
TheuseofNVBGbeganwithAdamsandLeonard,22who
usedacorticaltibialgraftembeddedintheproximaland
dis-talfragmentthroughthedorsalaccessroute.In1934,Murray23
describedtheuseofatibialgraftpeggedthroughthescaphoid
tuberosity; in 1928, Barnard and Stubbins24 described the
removalofthisbonepegfromthestyloidprocessoftheradio.
In1936,Matti25developedthetechniqueinwhichthe
prox-imal and distalfragments ofthe scaphoidwere excavated
throughadorsal accessroute,creatingagroovewhichwas
filledwithcancellousbonegraft.Russe26modifiedtheMatti
techniquewhenusingthevolaraccessroutetopreservethe
vascularizationofthescaphoidandtofillthegroovewithen
bloccancellousgraft.
Inturn,Fisk27observedanintenseresorptionofthevolar
portionofthefragmentsandtheensuinginstability,inwhich
thedistalfragmenttendstoflexandtheproximalfragment
tendstoextendalongwiththelunate.Heproposedtheuse
ofa corticocancellous graft to correct this deformity.
Sub-sequently, Segmüller28 followed the precepts described by
Fisk; however, he described the association of the use of
osteosynthesismaterial(tractionscrew).Nonetheless,itwas
Fernandez29whodescribedthistechniqueindetail.
In 1965, Roy-Camille30 published the technique of VBG
obtainedfrom the scaphoid tuberosity. In1986, Kuhlmann
etal.31describedatechniqueinwhichVBGtakenfromthe
medialportionandvolarfromthedistalradiuswereusedto
treatfailuresthatoccurredafterusingtheMatti-Russe
tech-nique.
Zaidenbergetal.32publishedanarticledescribingtheuse
ofVBGremovedfromthedistalportionoftheradiuswith1,2
ICSRAvascularization.
Tsaietal.10 mentionedtwobasicreasonsforthe
prefer-encefortheuseofVBGoverNVBG:theshorterconsolidation
time,whichimpliesfasterfunctionalrecovery,andtheability
todeliverbloodtodevascularizedbone.
SincethepublicationofZaidembergetal.,32whoachieved
a consolidation rate of 100% in cases of nonunion of the
scaphoid,agrowinginterestintheindicationoftheuse of
VBGbased onthedorsalcirculationofthe radiushasbeen
observed,particularlywiththeuseofthe1,2ICSRA.In
sup-portofthesedata, arecentmeta-analysisbyMerrelet al.7
demonstratedaconsolidationrateof88%vs.47%withtheuse
ofVBGandNVBG,respectively. The1,2ICRSAruns
superfi-ciallyovertheextensorretinaculumanddistallytotheradial
metaphyseal bone. Accordingto the studiesthat used this
technique,theeasyidentificationanddissectionoftheartery
isitsmainadvantage.
Steimann etal.,9 Lianget al.,11 and Uerpairojkitet al.12
alsousedthe1,2ICRSAtechnique;allstudiesobserveda
con-solidation rateof100%. Theauthorsofthesethree studies
consideredthisproceduretobetechnicallyeasierwhen
com-pared withother VBG techniques, in additionto its single
incision.Furthermore,thedorsalintercalatedsegment
insta-bility(DISI)causedbythescaphoidcurvature(humpback)was
corrected,afactthathelpstoincreasethearcofmovement
postoperatively.Incontrast,inthestudybyKakaretal.,6the
restorationofcarpalgeometrywasessentialforconsolidation.
However,thebonegraftobtainedfromthedistalradiuswould
betoosmallforcorrectionofhumpback,i.e.,DISI.Thus,to
obtainaVBGthatmetthisrequirement,bonegraftfromthe
medialfemoralcondylewasused.Thedisadvantageofthis
methodwouldbetheneedtouseamicrosurgicaltechnique
forsmallvesselanastomosis;inturn,anexcellentgraftwould
beobtained,offeringgreaterrigiditythangraftsremovedfrom
thedistalradius.Nonetheless,itshouldbepointedoutthat
thetechniquethatusesthefreegraftofthefemoralcondyle
requiresadomainofmicrosurgicaltechniques,specific
train-ing,andalonglearningcurve.18
Jonesetal.18comparedtwogroups:VBGfromthefemoral
condylevs.VBGbasedonthe1,2ICSRA,andobserved
con-solidationratesof100%and40%,respectively.Ribaketal.16
obtainedaconsolidationrateof89%withVBGbasedonthe
1,2ICSRAvs.72%withNVBGobtainedfromthedistalradius.In
turn,Strawetal.,13whenstudyingthe1,2ICSRA-basedVBG,
concludedthattheuse ofthis techniquewas ineffectivein
theirseries,withconsolidationratesof27%,whichreducedto
12.5%whenconsideringonlycasesofproximalpolenecrosis.
Bertellietal.,15usingVBGbasedonthefirst metacarpal
artery,observedconsolidationratesin21ofthe24patients.
ThoseauthorsprefertouseVBGduetoitsgreater
effective-nessinpromotingboneconsolidationwhencomparedwith
NVBG,evenindifficultscenariossuchasavascularnecrosisof
theproximalpole.
TheuseofVBGwithdistalradiuscapsularcirculationwas
describedbySotereanosetal.,14thatobservedaconsolidation
rateof80%.Fortheseauthors,thisisarelativelysimple
tech-niquethateliminatestheneedforsmallvesseldissectionor
Onelimitation ofthistechnique,however, isthat itfailsto
correctthehumpbackdeformityofthescaphoid.
Jessuetal.17 usedVBGbasedon theanteriortransverse
carpal artery, i.e., the vascularized bone graft proposed by
Kuhlmannetal.31Theyobtaineda73%consolidationratein
30patientswithnonunionofthescaphoid;however,thetwo
casesofproximalpolenecrosisdidnotpresentconsolidation.
Althoughtheauthorsconsideredtheirconsolidationrateto
bedisappointing, they stillconsidered the techniqueto be
advantageous,mainlybecauseofitsuniquevolarapproach
thatreducesmorbidity,despitethefactthatitrequiresalong
learningcurve.
Allstudiesthatusedthe1,2ICSRAtechniquehighlightthe
easyvisualizationanddissectionofthepedicle,whichmakes
thistechniqueextremelyusefulforthetreatmentofnonunion
ofthe scaphoidwithproximalpolenecrosis.9–13 Studieson
NVBG usedprimarily corticocancellous bonegrafts, simple
techniquesthatpresenttheeasyremovalofthematerialas
anadvantage.However,asignificantvariationin
consolida-tionrateswasobserved.Matsukietal.19 achievedexcellent
results,totaling 100%consolidationinthe11patients with
necrosisoftheproximalpoleofthescaphoid.Inturn,Robbins
etal.20andRibaketal.16achievedmuchlowerrates,72%and
55%,respectively.
Final
considerations
ThereisapreferencefortheuseofVBGinrelationtoNVBG,
despitethefactthatthesurgicaltechniqueismoredetailed
anddemandsspecifictraining,especiallyincaseswhere
vas-cularmicrosurgery is required. Thestudies using the VBG
techniqueobservedabetterreproductionofpositiveresults
whencomparedwithconventionalbonegrafts.Thus,
accord-ing to this literature review, there is no consensus as to
whethertheuse ofthe VBGcanbeeffectiveinallcasesto
consolidatethescaphoidwithproximalpolenecrosis.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1. BuijzeGA,OchtmanL,RingD.Managementofscaphoid nonunion.JHandSurgAm.2012;37(5):1095–100.
2. Al-JabriT,MannanA,GiannoudisP.Theuseofthefree vascularisedbonegraftfornonunionofthescaphoid:a systematicreview.JOrthopSurgRes.2014;9:21.
3. GrettveS.Arterialanatomyofthecarpalbones.ActaAnat (Basel).1955;25(2–4):331–45.
4. TaleisnikJ,KellyPJ.Theextraosseousandintraosseousblood supplyofthescaphoidbone.JBoneJointSurgAm.
1966;48(6):1125–37.
5. GelbermanRH,MenonJ.Thevascularityofthescaphoid bone.JHandSurgAm.1980;5(5):508–13.
6. KakarS,BishopAT,ShinAY.Roleofvascularizedbonegrafts inthetreatmentofscaphoidnonunionsassociatedwith proximalpoleavascularnecrosisandcarpalcollapse.JHand SurgAm.2011;36(4):722–5.
7.MerrellGA,WolfeSW,SladeJF3rd.Treatmentofscaphoid nonunions:quantitativemeta-analysisoftheliterature.J HandSurgAm.2002;27(4):685–91.
8.LefaivreKA,SlobogeanGP.Understandingsystematicreviews andmeta-analysesinorthopaedics.JAmAcadOrthopSurg. 2013;21(4):245–55.
9.SteinmannSP,BishopAT,BergerRA.Useofthe1,2
intercompartmentalsupraretinaculararteryasavascularized pediclebonegraftfordifficultscaphoidnonunion.JHand SurgAm.2002;27(3):391–401.
10.TsaiTT,ChaoEK,TuYK,ChenAC,LeeMS,UengSW.
Managementofscaphoidnonunionwithavascularnecrosis using1,2intercompartmentalsupraretinaculararterialbone grafts.ChangGungMedJ.2002;25(5):321–8.
11.LiangK,KeZ,ChenL,NieM,ChengY,DengZ.Scaphoid nonunionreconstructedwithvascularizedbone-grafting pedicledon1,2intercompartmentalsupraretinacularartery andexternalfixation.EurRevMedPharmacolSci.
2013;17(11):1447–54.
12.UerpairojkitC,LeechavengvongsS,WitoonchartK.Primary vascularizeddistalradiusbonegraftfornonunionofthe scaphoid.JHandSurgBr.2000;25(3):266–70.
13.StrawRG,DavisTR,DiasJJ.Scaphoidnonunion:treatment withapedicledvascularizedbonegraftbasedonthe1,2 intercompartmentalsupraretinacularbranchoftheradial artery.JHandSurgBr.2002;27(5):413.
14.SotereanosDG,DarlisNA,DailianaZH,SarrisIK,MalizosKN. Acapsular-basedvascularizeddistalradiusgraftforproximal polescaphoidpseudarthrosis.JHandSurgAm.
2006;31(4):580–7.
15.BertelliJA,TaccaCP,RostJR.Thumbmetacarpalvascularized bonegraftinlong-standingscaphoidnonunion-ausefulgraft viadorsalorpalmarapproach:acohortstudyof24patients.J HandSurgAm.2004;29(6):1089–97.
16.RibakS,MedinaCE,MattarRJr,UlsonHJ,UlsonHJ, EtchebehereM.Treatmentofscaphoidnonunionwith vascularisedandnonvasculariseddorsalbonegraftingfrom thedistalradius.IntOrthop.2010;34(5):683–8.
17.JessuM,WavreilleG,StroukG,FontaineC,ChantelotC. ScaphoidnonunionstreatedbyKuhlmann’svascularized bonegraft:radiographicoutcomesandcomplications.Chir Main.2008;27(2–3):87–96.
18.JonesDBJr,BürgerH,BishopAT,ShinAY.Treatmentof scaphoidwaistnonunionswithanavascularproximal poleandcarpalcollapse.Acomparisonoftwovascularized bonegrafts.JBoneJointSurgAm.2008;90(12):
2616–25.
19.MatsukiH,IshikawaJ,IwasakiN,UchiyamaS,MinamiA,Kato H.Non-vascularizedbonegraftwithHerbert-typescrew fixationforproximalpolescaphoidnonunion.JOrthopSci. 2011;16(6):749–55.
20.RobbinsRR,RidgeO,CarterPR.Iliaccrestbonegraftingand Herbertscrewfixationofnonunionsofthescaphoidwith avascularproximalpoles.JHandSurgAm.1995;20(5):818–31.
21.GeisslerWB,SladeJF.Fracturesofcarpalbones.In:WolfeSW, HotchkissRN,PedersonWC,KozinSH,editors.Green’s operativehandsurgery.6thed.Philadelphia:Churchill Livingstone;2010.p.639–707.
22.AdamsJD,LeonardRD.Fractureofthecarpalscaphoid.Anew methodoftreatmentwithareportofonecase.NEnglJMed. 1928;198(8):401–4.
23.MurrayJ.Bonegraftfornonunionofthecarpalscaphoid.BrJ Surg.1934;22:63–8.
24.BarnardL,StubbinsSG.Styloidectomyoftheradiusinthe surgicaltreatmentofnonunionofthecarpalnavicular;a preliminaryreport.JBoneJointSurgAm.1948;30(1):98–102.
25.MattiH.Technikundresultatemeiner
26.RusseO.Fractureofthecarpalnavicular.Diagnosis, non-operativetreatment,andoperativetreatment.JBone JointSurgAm.1960;42:759–68.
27.FiskGR.Carpalinstabilityandthefracturedscaphoid.AnnR CollSurgEngl.1970;46(2):63–76.
28.SegmüllerG.Navikularepseudarthrose.In:SegmüllerG, editor.Operativestabilisierungamhandskelet.Berlin:Verlag HansHuber;1973.p.99–104.
29.FernandezDL.Atechniqueforanteriorwedge-shapedgrafts forscaphoidnonunionswithcarpalinstability.JHandSurg Am.1984;9(5):733–7.
30.Roy-CamilleR.Fracturesetpseudarthrosesduscaphoid moyenutilisationd’umgrefforpedicule.ActualChirOrthop. 1965;4:197–214.
31.KuhlmannJN,MimounM,BoabighiA,BauxS.Vascularized bonegraftpedicledonthevolarcarpalarteryfornon-union ofthescaphoid.JHandSurgBr.1987;12(2):203–10.