www.jped.com.br
ORIGINAL
ARTICLE
HIV
testing
in
the
maternity
ward
and
the
start
of
breastfeeding:
a
survival
analysis
夽
,
夽夽
Glaucia
T.
Possolli
a,∗,
Márcia
L.
de
Carvalho
b,
Maria
Inês
C.
de
Oliveira
caDepartmentofNursing,UniversidadeEstadualdoCentro-Oeste(UNICENTRO),Guarapuava,PR,Brazil
bDepartmentofEpidemiologyandQuantitativeMethodsinHealth,EscolaNacionaldeSaúdePública(ENSP),Fundac¸ãoOswaldo
Cruz(FIOCRUZ),RiodeJaneiro,RJ,Brazil
cDepartmentofEpidemiologyandBiostatistics,InstitutodeSaúdedaComunidade,UniversidadeFederalFluminense(UFF),
Niterói,RJ,Brazil
Received28July2014;accepted3November2014 Availableonline16May2015
KEYWORDS Breastfeeding; Hospitalbirth; AIDSserodiagnosis; Survivalanalysis
Abstract
Objective: The purposeofthisstudy was toanalyze thefactorsthatinfluence ofthetime betweenbirthandthebeginningofbreastfeeding,especiallyatthemomentoftherapidHIV testresultsathospitaladmissionfordelivery.
Methods: Cohortstudyof932pregnantwomenwhounderwentrapidHIVtestadmittedinthe hospitalfordeliveryinBaby-FriendlyHospitals.Thesurvivalcurvesoftimefrombirthtothe firstfeedingwereestimatedbytheKaplan---Meiermethodandthejointeffectofindependent variablesbytheCoxmodelwithahierarchicalanalysis.Asthesurvivalcurveswerenot homo-geneousamongthefivehospitals,hinderingtheprincipleofproportionalityofrisks,thedata weredividedintotwogroupsaccordingtothemediantimeofonsetofbreastfeedingatbirth inwomenundergoingrapidHIVtesting.
Results: Hospitalswithmediantimetobreastfeedingonsetatbirthofupto60minwere con-sideredasearlybreastfeedingonsetandthosewithhighermedianswereconsideredaslate breastfeeding onset atbirth. Riskfactorscommontohospitals consideredto bewith early andlatebreastfeeding onsetatbirthwere:cesareansection(RR=1.75[95%CI:1.38---2.22]; RR=3.83[95%CI:3.03---4.85])andrapidtestresultafterbirth(RR=1.45[95%CI:1.12---1.89]; RR=1.65[95%CI:1.35---2.02]),respectively;andhospitalswithlate onset:startingprenatal careinthethirdtrimester(RR=1.86[95%CI:1.16---2.97]).
夽 Pleasecitethisarticleas:PossolliGT,deCarvalhoML,deOliveiraMI.HIVtestinginthematernitywardandthestartofbreastfeeding:
asurvivalanalysis.JPediatr(RioJ).2015;91:397---404.
夽夽
StudyconductedatEscolaNacionaldeSaúdePública(ENSP),Fundac¸ãoOswaldoCruz(FIOCRUZ),RiodeJaneiro,RJ,Brazil.
∗Correspondingauthor.
E-mail:glauciatalita@hotmail.com(G.T.Possolli).
http://dx.doi.org/10.1016/j.jped.2014.11.004
Conclusions: Theonsetofbreastfeedingispostponed,eveninBaby-FriendlyHospitals,when theresultsoftherapidHIVtestrequestedinthematernityarenotavailable atthetimeof delivery.
©2015SociedadeBrasileiradePediatria.PublishedbyElsevierEditoraLtda.Allrightsreserved.
PALAVRAS-CHAVE
Aleitamentomaterno;
Nascimentoem
hospital;
Sorodiagnósticode
AIDS;
Análisedesobrevida
Testagemanti-HIVnamaternidadeeoiníciodoaleitamentomaterno:umaanálisede sobrevida
Resumo
Objetivo: Identificar os fatores associados ao tempo entre o nascimento e o início da amamentac¸ãoemmães,especialmenteomomentodoresultadodotesterápidoanti-HIV,na internac¸ãoparaoparto.
Metodologia: Estudodecoortecom932parturientesquerealizaramtesterápidoanti-HIVna internac¸ãoparaopartoemHospitaisAmigosdaCrianc¸a.Ascurvasdesobrevidadotempodo nascimentoatéa1amamadaforamestimadaspelométodoKaplan---Meier,eoefeitoconjunto
dasvariáveisindependentespelomodelodeCox,comanálisehierarquizada.Comoascurvasde sobrevidanãoforamhomogêneasentreos5hospitais,ferindooprincípiodeproporcionalidade deriscos,osdadosforamdesmembradosemdoisgrupossegundootempomedianodeiníciode aleitamentomaternoaonasceremmulheressubmetidasaotesterápidoanti-HIV.
Resultados: Hospitaiscomtempomedianodeaté60minutosforamconsideradoscomohospitais deinícioprecocedoaleitamentomaternoehospitaiscomtempomedianosuperiorforam con-sideradoscomohospitaisdeiníciotardiodoaleitamentomaternoaonascer.Foramfatoresde riscocomunsaoshospitaiscominícioprecoceetardiodoaleitamentomaternoaonascer:parto cesáreo[RR=1.75(IC95%:1,38---2,22);RR=3,83(IC95%:3,03---4,85)]eresultadodotesterápido apósoparto[RR=1,45(IC95%:1,12---1,89);RR=1,65(IC95%:1,35---2,02)], respectivamente;e noshospitaiscominício tardiodealeitamentomaterno aonascer:iniciaropré-natalno3◦ trimestre[RR=1,86(IC95%:1,16---2,97)].
Conclusões: Oiníciodoaleitamentomaternovemsendopostergado,mesmoemHospitais Ami-gosdaCrianc¸a,quandoosresultadosdotesterápidoanti-HIVsolicitadosnamaternidadenão estãodisponíveisnomomentodoparto.
©2015SociedadeBrasileiradePediatria.PublicadoporElsevierEditoraLtda.Todososdireitos reservados.
Introduction
Breastfeedingatbirthisessentialtoestablishmother---baby bondingandcontributestothecontinuationof breastfeed-ingandthereductionofneonatalmortality.1,2Newbornsare
moreresponsivetothemother’ssmell,touch,andwarmth; whentheskin-to-skincontactis initiatedsoonafterbirth, thenewbornhasthecapacitytoseekoutthenipple---areola regionandlatchonduringthefirsthouroflife.Threetofour hoursafter birth,newborns enterthesleep phase,which complicatestheonsetofbreastfeeding.3
TheBaby-FriendlyHospitalInitiative(BFHI)recommends ‘‘putting babiesin directcontact withthe mother imme-diatelyafterbirthfor at leastan hourand encouragethe mothertoverifywhetherthebabyisreadytobebreastfed andofferhelpifnecessary’’astheStep4ofthe‘‘TenSteps toSuccessfulBreastfeeding’’.4
There are situations, however, when breastfeeding should not be practiced. In Brazil, breastfeeding by human immunodeficiency virus (HIV)-infected mothers is contraindicated due to the risk of vertical transmission throughbreastmilk.5However,theMinistryofHealth(MOH)
recommends thathealth professionalsshould notprohibit
breastfeeding tomotherswho,although submitted tothe anti-HIV test, do not have the result available, as the contraindication should be based on an HIV-reagenttest, stressingthatitistheresponsibilityoftheserviceto estab-lishthelogistics sothattheresultisavailable ina timely manner.6Withthispurpose,theMOHhasregularizedrapid
HIV tests in hospitals for pregnant women not tested for HIV during prenatalcare, in timefor establishing vertical transmissionprophylacticmeasures.7
Additionally, since 2006 the MOH has recommended repeating anti-HIV serology, with the pregnant woman’s consent,nearthe38thweekofpregnancy8whenever
possi-ble.Thus,rapidHIV testsarecurrentlyoftenrequestedin maternity wards, but often without following anycriteria orstandards,evenforwomenwhoalreadyhadadiagnosis at thelasttrimesterofpregnancy. Thisincreaseddemand forrapidtestsandtheprofessionals’workoverloadhas hin-deredhowpromptlyresultsareobtained.9
Methods
This was a cohortstudy, whose initial event wasdelivery
and whose outcome was the onset of breastfeeding. The
database from the research‘‘Gender, Power and
Citizen-ship:isthe womana subjectindecision-making regarding
breastfeedingatbirthwhenHIVstatusisunknowntothe ser-vice?’’10 wasused.Thetargetpopulationofthestudywas
allwomensubmittedtorapidHIVtestathospitaladmission fordeliveryinthefiveBaby-Friendlyhospitalsbelongingto theHigh-RiskPregnancySysteminthecityofRiodeJaneiro betweenSeptember11andDecember11,2006.
The pilotstudy was performed in two hospitals of the High-Risk Pregnancy System in the same city, which had agreedtobecomeBaby-Friendlyhospitals.The study indi-cated a prevalence of non-breastfeeding at birth of 50% amongseronegativewomensubmittedtotherapidHIVtest. Basedonthisparameter,asampleof700motherswas esti-mated,withastatisticalpowerof99%and95%confidence level.
Women included in the study werethose submittedto rapidHIV test atdelivery,whose childrenwereborn alive andremainedinrooming-incare.Thewomenexcludedfrom thestudy werethosewhoseinfants wereborn with5-min Apgar value <7(critically lowstate of vitality), whowere referred to the intensive care unit (ICU; or neonatal ICU [NICU])whenthemotherwasreferredtotheICUorshowed HIVseropositivity.
The interviews were performed by nurses or nursing students trained and supervised weekly by a researcher, after the informed consent had been signed, which con-taineddetailsoftheresearchandensuredconfidentialityof information.The projectwasapprovedbytheHealth Sec-retariatEthicsCommitteeofRiodeJaneiro(Statement82A of31/07/2006).
Adailysurveywascarriedoutinthelaboratoryofeach hospitaltoidentifythepregnantwomensubmittedtorapid HIVtestandthenameofthesewomenwastranscribedtoa datacollectionform.Theformwascompareddailywiththe listofrooming-inadmissions,thechartwaschecked, deliv-erydatawereenteredintoadailyplan,andeligiblemothers wereinterviewed.Theinterviews wereperformed usinga structuredquestionnaire,administeredatleast2hafterthe child’sbirth. Ifduringtheinterview thenewbornhad not been breastfedyet, theinterviewerreturnedtointerview thatmotheragainattheendofthedaytocollectdataon thetimebetweenbirthandthefirstfeeding.
The study endpoint wasobtained throughthequestion ‘‘Howlongafterbirthwasyourbabybreastfedforthefirst time?’’,andinanattempttoimprovethemother’sanswer accuracy,itwassoughttomakeherrecallthetimeofthis eventbasedonthescheduleofhospitalroutines.Theanswer wasgivenin hoursand minutes,and thefirst breastfeed-ingwasconsideredasthemomentofcontactbetweenthe baby’smouthandthemother’snipple---areolaregion,with eithertheoccurrenceofsuctionorlicking.
The variables were organized in a hierarchical model, withsocioeconomicanddemographic(distal),reproductive andprenatalcare(intermediate),andhospital characteris-tics(proximal).The distalvariableswereage,educational level,ethnicity,maritalstatus,maternalemployment,and income.
Theintermediatevariableswere:parity;prenatalcare; trimesterwhenprenatalcare started;numberofprenatal visits; HIV test performed during prenatalcare; trimester whenthe pregnantwomanwastested; andresults of HIV testinginprenatalcare.
Finally, the proximal variables were: hospital; type of delivery;genderofthebaby;motherwantedtobreastfeed; professionalheard whatthe motherhadtosay about her andthe infant; mother knew about performing rapid HIV testatthehospital;motherreceivedexplanationaboutthe test;motherreceivedthetestresult;andmomentwhenthe motherknewthetestresult.
Survivalanalysis11wasused,inwhichtimezerowasbirth
andthefirstfeedingwasthefinalevent.Theanalysis con-sideredthemothersthat startedbreastfeedingwithinthe first24h.Caseswherethefollow-upuntiltheoutcomewas notpossible andthoseinwhichtheoccurrenceof startof breast-feedingtimewasmorethan24hwereomitted.
Survival curves, overall and by stratum, estimated by thenonparametricKaplan---Meiermethod,12wereusedasan
exploratorytoolintheunivariateanalysis.
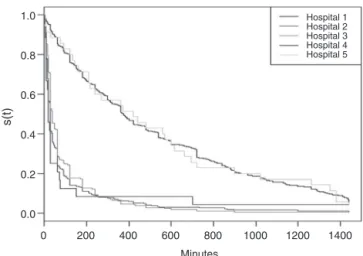
Itwasobservedthatsurvivalcurveswerenothomogenous inthefivehospitals,affectingtheprincipleofrisk propor-tionality.Therefore,itwasdecidedtodividethedatainto twogroups,accordingtothemediantimetoonsetof breast-feedingatbirth:hospitalswithmediantimeofupto60min wereconsideredasearlyonsetofbreastfeedingatbirthand thosewithhighermediantimewereconsideredaslateonset ofbreastfeedingatbirth.
Aftertheinitialanalysis,thevariablesthatshowed statis-ticalsignificanceof10%atthePetotest12orepidemiological
significance test were considered for construction of the hierarchicalmodel.TheWaldtestwasusedtocomparethe differentCox regression models.The R2 of the saturated
modelwasusedtoevaluatethequalityofadjustment,based ontheproportionofexplainedvariance.
In the hierarchical modeling, the block of variables in the distal level was introduced. Variables with statistical significanceat the10% level were kept in themodel and incorporated into the analysis of the intermediate block. The sameprocedure wasrepeatedfor the analysisof the proximal block variables, resulting in a final model with threelevels.13,14
The Schoenfeld and Martingale tests12 wereapplied to
theanalysisof residues. Thedatabase wasbuiltusing Epi Info (Epi InfoTM Centers for Disease Control and
Preven-tion,GA,USA)softwareandthestatisticalmodeling,charts, andresidueanalysiswereperformedusingtheRstatistical package15(RCoreTeam(2012).R:alanguageand
environ-mentforstatisticalcomputing.Vienna,Austria).
Results
Duringthestudyperiodtherewere4895birthsinselected hospitalsand1396(28.5%)womenunderwentrapidHIVtest.
Ofthese,322womenwereexcludedduetothepresenceof
criteriathatcouldimpairorpreventbreastfeedingatbirth. Ofthe1074eligiblewomen,42refusedtoparticipate(3.9%)
andtherewasloss of 77 (7.2%)due toearly discharge or
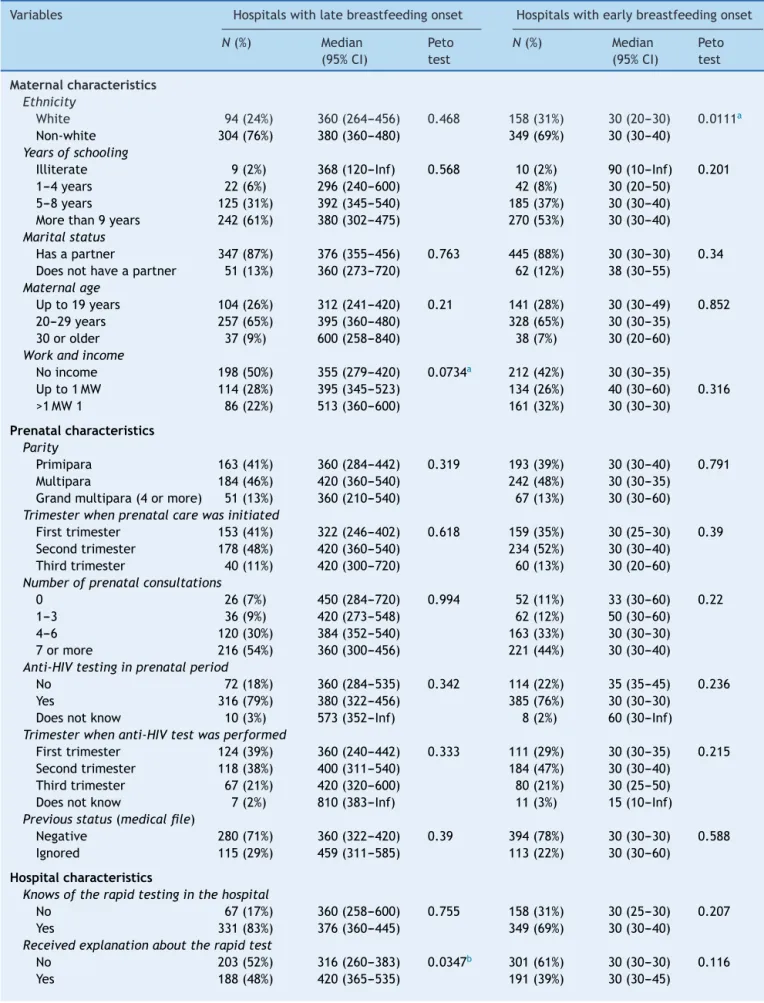
Table1 Mediantimefrombirthtobreastfeedingonset,pertypeofhospitalconduct.RiodeJaneiro,Brazil,2006.
Variables Hospitalswithlatebreastfeedingonset Hospitalswithearlybreastfeedingonset
N(%) Median
(95%CI)
Peto test
N(%) Median
(95%CI)
Peto test
Maternalcharacteristics Ethnicity
White 94(24%) 360(264---456) 0.468 158(31%) 30(20---30) 0.0111a
Non-white 304(76%) 380(360---480) 349(69%) 30(30---40) Yearsofschooling
Illiterate 9(2%) 368(120---Inf) 0.568 10(2%) 90(10---Inf) 0.201 1---4years 22(6%) 296(240---600) 42(8%) 30(20---50)
5---8years 125(31%) 392(345---540) 185(37%) 30(30---40) Morethan9years 242(61%) 380(302---475) 270(53%) 30(30---40) Maritalstatus
Hasapartner 347(87%) 376(355---456) 0.763 445(88%) 30(30---30) 0.34 Doesnothaveapartner 51(13%) 360(273---720) 62(12%) 38(30---55)
Maternalage
Upto19years 104(26%) 312(241---420) 0.21 141(28%) 30(30---49) 0.852 20---29years 257(65%) 395(360---480) 328(65%) 30(30---35)
30orolder 37(9%) 600(258---840) 38(7%) 30(20---60) Workandincome
Noincome 198(50%) 355(279---420) 0.0734a 212(42%) 30(30---35)
Upto1MW 114(28%) 395(345---523) 134(26%) 40(30---60) 0.316 >1MW1 86(22%) 513(360---600) 161(32%) 30(30---30)
Prenatalcharacteristics Parity
Primipara 163(41%) 360(284---442) 0.319 193(39%) 30(30---40) 0.791 Multipara 184(46%) 420(360---540) 242(48%) 30(30---35)
Grandmultipara(4ormore) 51(13%) 360(210---540) 67(13%) 30(30---60) Trimesterwhenprenatalcarewasinitiated
Firsttrimester 153(41%) 322(246---402) 0.618 159(35%) 30(25---30) 0.39 Secondtrimester 178(48%) 420(360---540) 234(52%) 30(30---40)
Thirdtrimester 40(11%) 420(300---720) 60(13%) 30(20---60) Numberofprenatalconsultations
0 26(7%) 450(284---720) 0.994 52(11%) 33(30---60) 0.22 1---3 36(9%) 420(273---548) 62(12%) 50(30---60)
4---6 120(30%) 384(352---540) 163(33%) 30(30---30) 7ormore 216(54%) 360(300---456) 221(44%) 30(30---40) Anti-HIVtestinginprenatalperiod
No 72(18%) 360(284---535) 0.342 114(22%) 35(35---45) 0.236 Yes 316(79%) 380(322---456) 385(76%) 30(30---30)
Doesnotknow 10(3%) 573(352---Inf) 8(2%) 60(30---Inf) Trimesterwhenanti-HIVtestwasperformed
Firsttrimester 124(39%) 360(240---442) 0.333 111(29%) 30(30---35) 0.215 Secondtrimester 118(38%) 400(311---540) 184(47%) 30(30---40)
Thirdtrimester 67(21%) 420(320---600) 80(21%) 30(25---50) Doesnotknow 7(2%) 810(383---Inf) 11(3%) 15(10---Inf) Previousstatus(medicalfile)
Negative 280(71%) 360(322---420) 0.39 394(78%) 30(30---30) 0.588 Ignored 115(29%) 459(311---585) 113(22%) 30(30---60)
Hospitalcharacteristics
Knowsoftherapidtestinginthehospital
No 67(17%) 360(258---600) 0.755 158(31%) 30(25---30) 0.207 Yes 331(83%) 376(360---445) 349(69%) 30(30---40)
Receivedexplanationabouttherapidtest
No 203(52%) 316(260---383) 0.0347b 301(61%) 30(30---30) 0.116
Table1 (Continued)
Variables Hospitalswithlatebreastfeedingonset Hospitalswithearlybreastfeedingonset
N(%) Median
(95%CI)
Peto test
N(%) Median
(95%CI)
Peto test
Knowstheresultoftherapidtest
Yes 242(62%) 420(360---523) 0.117 181(37%) 35(30---50) 0.104
No 149(38%) 320(255---390) 311(63%) 30(30---30)
Whenmotherlearnedtheresultoftherapidtest
Beforedeliveryanddoesnotknow 229(58%) 302(240---375) 9.2e−05c 373(76%) 30(30---30) 0.000652c
Afterdelivery 167(42%) 486(402---600) 115(24%) 50(30---60) Typeofbirth
Normal 282(71%) 240(198---300) 0c 343(68%) 30(30---30) 1.59e
−05c Cesareansection 116(29%) 924(853---1140) 164(32%) 50(38---60)
Newborngender
Female 208(52%) 336(275---420) 0.072a 237(47%) 30(30---38) 0.904
Male 189(48%) 422(360---560) 266(53%) 30(30---40) Motherwantedtonursethebabyinthedeliveryroom
No 196(50%) 360(300---480) 0.773 187(37%) 35(30---50) 0.000886c
Yesandnotsure 199(50%) 396(360---490) 320(63%) 30(25---30) Professionalslistentothemother
Yes 284(71%) 382(320---480) 0.884 407(80%) 30(30---30) 0.313 Notsureandno 114(29%) 360(300---510) 100(20%) 35(30---60)
CI:confidenceinterval.
a 0.05<p<0.1.
b p<0.05.
c p<0.001.
fortheanalysis.Ofthese,27caseswereomitted,whohad timeuntilonsetofbreastfeedinglongerthan24h,andthus thenumberofeventswasrestrictedto905.
The median time untilthe onset of breastfeeding was
90min(95%CI:63---120),withaprobabilityof48%to breast-feedwithinthefirsthourafterdelivery.
Themediantimetotheonsetofbreastfeedingforwhite
mothers(60min;95%CI:40---65),with1---4yearsofschooling (60min;95%CI:36---120)andmaternalincome>1minimum wage(60min;IC95%:40---110)waslowerthantheir corre-spondingmatches, withstatistical significancein thePeto Test(p<0.001,p=0.046,p=0.089,respectively).Maternal
age showed no statistical significance when analyzed by
categories in theKaplan---Meier test (p=0.313),but it did whenanalyzedcontinuously(p=0.049),andshowedalinear
association withtime when aspline wasperformed, with
ap-value ofthe linearityofp=0.051, vs.p=0.470 in the non-linearassociation.
Theprenatalvariablesdidnotshowsurvivalcurveswith astatisticallysignificantdifferenceinthePetotest,butin relation to hospital variables, the following factors
post-poned the start of breastfeeding: hospital length of stay
(p<0.001); mother knew about the performance of the
rapidHIV test(120min; 95%CI:90---135);motherreceived
explanation about the test (120min; 95% CI: 105---180);
mother knew the test result (180min; 95% CI: 120---210);
mother knew the test result after delivery (240min; 95%
CI:180---348); motherwassubmittedtoacesareansection (110min;95%CI:120---360);motherdidnotwanttoputthe babyat thebreastat birth(120min;95%CI:95---174);and motherreportedthatthehospitalstaffhadnotlistenedto her(136min;95%CI:110---189).
In the survival curves stratified by hospital, as shown
in Fig. 1, it is seen that the time until the first feeding showeddistinctpatterns.Hospitals2,3,and4hadanearly onsetof breastfeedingatbirthin thecaseof women sub-mittedtotherapidHIVtest,whereashospitals1and5had alateonsetofbreastfeeding,leadingtothedivisionofthe databaseaccording tothe mediantime.The median time wasanalyzedforthesetwogroupsofhospitals(Table1).
Forhospitals withlate onsetof breastfeeding at birth themediantimewas375min.Inhospitalswithearlyonset ofbreastfeedingthemediantimewas30min,representing aperiodmorethan10-foldshorter.
0 200 0.0
0.2 0.4 0.6 0.8 1.0
400 600 800 1000 Minutes
s(t)
1200 1400
Hospital 1 Hospital 2 Hospital 3 Hospital 4 Hospital 5
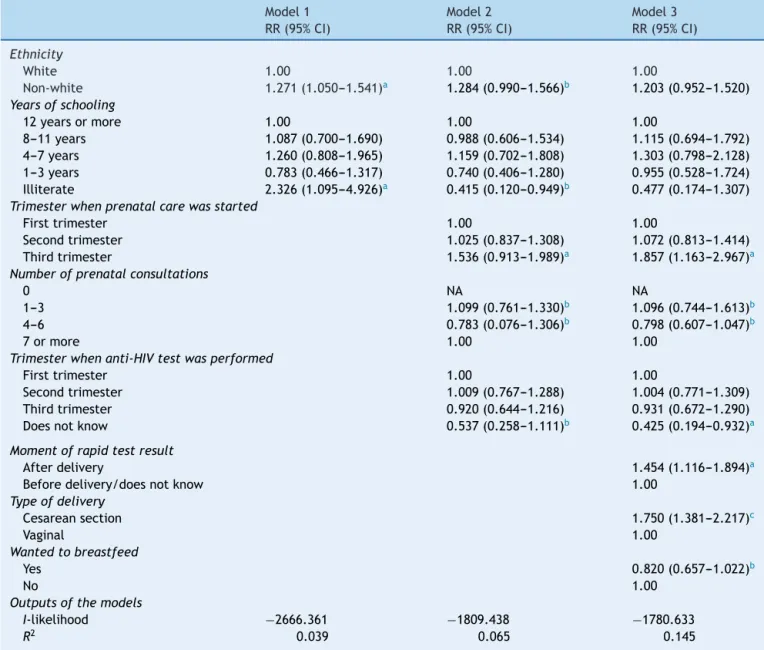
Table2 Hierarchicalmodeloffactorsassociatedwithtimetobreastfeedingonsetinhospitalswithearly-onsetbreastfeeding atbirth.RiodeJaneiro,Brazil,2006.
Model1 Model2 Model3
RR(95%CI) RR(95%CI) RR(95%CI)
Ethnicity
White 1.00 1.00 1.00
Non-white 1.271(1.050---1.541)a 1.284(0.990---1.566)b 1.203(0.952---1.520)
Yearsofschooling
12yearsormore 1.00 1.00 1.00
8---11years 1.087(0.700---1.690) 0.988(0.606---1.534) 1.115(0.694---1.792) 4---7years 1.260(0.808---1.965) 1.159(0.702---1.808) 1.303(0.798---2.128) 1---3years 0.783(0.466---1.317) 0.740(0.406---1.280) 0.955(0.528---1.724) Illiterate 2.326(1.095---4.926)a 0.415(0.120---0.949)b 0.477(0.174---1.307)
Trimesterwhenprenatalcarewasstarted
Firsttrimester 1.00 1.00
Secondtrimester 1.025(0.837---1.308) 1.072(0.813---1.414) Thirdtrimester 1.536(0.913---1.989)a 1.857(1.163---2.967)a
Numberofprenatalconsultations
0 NA NA
1---3 1.099(0.761---1.330)b 1.096(0.744---1.613)b
4---6 0.783(0.076---1.306)b 0.798(0.607---1.047)b
7ormore 1.00 1.00
Trimesterwhenanti-HIVtestwasperformed
Firsttrimester 1.00 1.00
Secondtrimester 1.009(0.767---1.288) 1.004(0.771---1.309) Thirdtrimester 0.920(0.644---1.216) 0.931(0.672---1.290) Doesnotknow 0.537(0.258---1.111)b 0.425(0.194---0.932)a
Momentofrapidtestresult
Afterdelivery 1.454(1.116---1.894)a
Beforedelivery/doesnotknow 1.00
Typeofdelivery
Cesareansection 1.750(1.381---2.217)c
Vaginal 1.00
Wantedtobreastfeed
Yes 0.820(0.657---1.022)b
No 1.00
Outputsofthemodels
I-likelihood −2666.361 −1809.438 −1780.633
R2 0.039 0.065 0.145
CI,confidenceinterval;RR,relativerisk.
ap<0.05.
b 0.05<p<0.1.
c p<0.001.
BasedontheunivariateanalysisusingtheKaplan---Meier
methodand epidemiological criteria, variables were
ana-lyzedusingtheproposedhierarchicalmodel.
Model3,afteradjustmentbythehierarchicalmodelof
factorsrelated to thetime of breastfeeding start in hos-pitalswithearlyonsetof breastfeeding,hadacovariance
explanationpowerof14.5%.
Inthissense,factorsthatpostponedthestartof breast-feedingwere: starting prenatalcare in thethird quarter; knowledgeafterdeliveryoftheresultoftherapidHIVtest inthehospital;andcesareandelivery.
In the hierarchical model for hospitals with late
onset of breastfeeding, when the proximal level
varia-bleswereintroduced,thevariablesinthedistallevellost
statisticalsignificanceand,therefore,theireffectappeared tobemediatedbythevariablesinthatlevel(Table2).
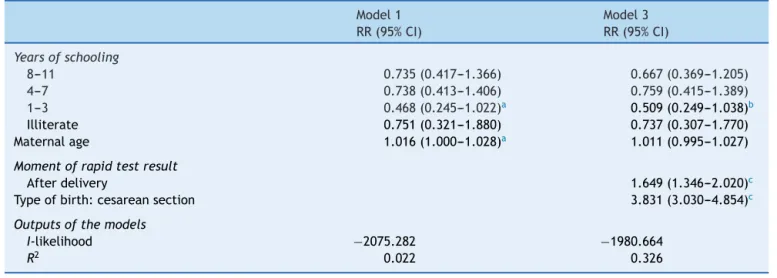
Inthefinalmodelforhospitalswithlateonsetof breast-feedingatbirth,factorsthatnegativelyinterferedwiththe outcomewere:havingreceivedtheresultoftherapidtest performedinthematernityafterbirth;andcesarean deliv-ery.Theinclusionofvariablesintheproximallevelimproved themodelfitby30%(Table3).
Table3 Hierarchicalmodeloffactorsassociatedwithtimetobreastfeedingonsetinhospitalswithlate-onsetbreastfeeding atbirth.RiodeJaneiro,Brazil,2006.
Model1 Model3
RR(95%CI) RR(95%CI)
Yearsofschooling
8---11 0.735(0.417---1.366) 0.667(0.369---1.205)
4---7 0.738(0.413---1.406) 0.759(0.415---1.389)
1---3 0.468(0.245---1.022)a 0.509(0.249---1.038)b
Illiterate 0.751(0.321---1.880) 0.737(0.307---1.770) Maternalage 1.016(1.000---1.028)a 1.011(0.995---1.027)
Momentofrapidtestresult
Afterdelivery 1.649(1.346---2.020)c
Typeofbirth:cesareansection 3.831(3.030---4.854)c
Outputsofthemodels
I-likelihood −2075.282 −1980.664
R2 0.022 0.326
CI:confidenceinterval;RR:relativerisk.
a p<0.05.
b 0.05<p<0.1.
c p<0.001.
Discussion
The variable ‘‘moment of anti-HIV rapid test result after
delivery’’showedsimilarconsistencyandmagnitudeinboth models,regardlessofthehospitalcharacteristicofearlyor
late onset of breastfeeding at birth. This fact shows the
delayinthetestresulthassimilarimpactandsame-intensity
influenceonbreastfeedingpostponementatbirth.
In a study thatdichotomized breastfeeding onset(first
houroflifeandafterthefirsthour),notknowingwhether
the rapidHIV test wasperformed at the hospitaland not
knowingtheresultsalsoshowedtobefactorsthatdelayed breastfeedingatbirth.9
In a recently published systematic review,15 it was
observedthattheonlystudythatinvestigatedtherapidHIV test inrelation tobreastfeedingis the resultofthe same databasethatgaveorigintothisarticle.
Cesarean delivery was negatively associated with the onsetofbreastfeedingand,thus,persistedasabarrierto breastfeedingatbirth.16---18Someauthorsconsidercesarean
sectionariskfactorforthecontinuationofbreastfeedingat oneand3monthsafterbirth.19
The median time to onset of breastfeeding in vaginal birthwas60min,andforcesareansection,themediantime was210min.Accordingtohospitalconduct,themediantime totheonsetofbreastfeedingforavaginaldeliveryin hos-pitalswithearlyonsetis30min,whereasinhospitalswith lateonsetofbreastfeeding thistimeis240min,an 8-fold longerperiod.
Themediantimetothefirstfeedingforcesareandelivery also showed differences by hospital conduct. In hospitals withlate onset,the median was924min andin hospitals withearlyonset,themedianwas50min,analmost18-fold shorterperiod.
The variable ‘‘intention to breastfeed in the delivery room’’wassignificantlyassociatedwiththeoutcomeonly
inhospitalswithearlyonsetofbreastfeedingatbirth, sug-gestingthatthemother’sdecisiontobreastfeedisweakened even in Baby-Friendly Hospitals, where the lack of staff awareness still persists in the autonomy of the woman regardingthehospitalinstitution.
Basedonthefinalmodels,itwasverifiedthatthereare commonfactors,regardlessofthepatternofmedian time untiltheonsetofbreastfeeding,suchasthemomentofthe rapidtestresultandthetypeofdelivery.
Inhospitalswithlateonsetofbreastfeeding,theanalyses suggestthatalmost30%ofthetimevariationispredictable byhospitalvariables.Inhospitalswithearlyonsetof breast-feeding at birth, a small portion of data variability is explainedbythemodel(R2=0.145),buttheproximal
varia-bles still showed greater weight regarding the outcome. Residualanalysisofthefinalmodelsshowedgoodfitofthe models.
In hospitals with early onset of breastfeeding, 74% of women were able tostart breastfeeding withinthe new-born’s first hour of life, whereas in hospitals with late onset,only 15% started breastfeeding within1h of birth. Therefore,thepostponementoftheonsetofbreastfeeding becomes evident as established practice, even in Baby-FriendlyHospitals,andhospitalprotocolsaredescribedin theliteratureasabarriertotheonsetofbreastfeeding.20
Inspite ofthecharacteristics ofthesehospitals,which inessencearebreastfeedingsupporters,thepostponement ofbreastfeedingissupportedbyknowledgenotreportedin theliterature.Thus,althoughtheyareBaby-Friendly Hospi-tals,theycanbeclassifiedashavingearly-orlate-onsetof breastfeedingatbirth.
Thestudyhaslimitations,asitwasnotpossibleto ana-lyzefactorsthat,accordingtoasystematicreview onthe theme,15caninfluencetheonsetofbreastfeeding,suchas:
assessedmothersweresubmittedtotherapidtest, itwas notpossibletoinvestigatetheinfluenceofthetestalone, whichwouldaddmoreinformationtotheanalysis.
Despitetheselimitations,thisstudyisanimportanttool toimproveverticaltransmissionpreventionstrategiesand the Baby-Friendly Hospital Initiative, as well as human-ization strategies in care and the establishment of these policies.
Theonlyprenatalcarevariableassociatedwiththetime toonsetofbreastfeedingwasthebeginningofprenatalcare inthethirdtrimester,inhospitalswithearlyonsetof breast-feedingatbirth.Womenwhostartedalateprenatalappear to constitute a risk clientele for the practice of breast-feeding,eveninhospitalswithpracticesthatpromoteearly onsetofbreastfeeding.Therefore,itcanbeobservedthat greatereffortsareneededtocarryoutgood-quality prena-talcare,withearlyidentificationofpregnantwomenanda morethoroughassessmentforcesareandelivery.
Itiscrucialtodefinestandardsregardingthepracticeof breastfeedingforunknownHIVstatus,counselingpractices andconsent,anddefinitionofresponsibilitiesforproviding resultsinatimelymanner.
A morerecent study conducted in 15 maternity hospi-talsin RiodeJaneiro in 2009showed thatthe proportion ofmothers submittedtothe rapid test whenadmitted at thehospitalfordeliverywasstillhigh,andthatnotknowing theresultsoftheHIVtesting beforedeliveryincreasedby morethan2-foldthechanceoflateonsetofbreastfeeding,21
showingthatthisscenariohasnotshownapositiveevolution withtime.
Aftertheimplementationof theBaby-FriendlyHospital Initiative,thereweresignificantadvancesinbreastfeeding practices.Thus,theproposedchallengeistheestablishment ofguaranteestoevaluateinterventionsthatmayberelated tothepostponementofbreastfeeding,suchasinadequate operationalizationoftherapidHIVtest.
Funding
GlauciaTalitaPossollireceivedaMaster’sDegreegrantfrom CAPES.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.WorldHealthOrganization.Evidenceforthetenstepsto suc-cessfulbreastfeeding.Divisionofchildhealthanddevelopment. Geneva:WorldHealthOrganization;1988.
2.Boccolini CS, Carvalho ML, Oliveira MI, Pérez-Escamilla R. Breastfeedingduringthefirsthouroflifeand neonatal mor-tality.JPediatr(RioJ).2013;89:131---6.
3.MooreE,AndersonGC.Randomizedcontrolledtrialofberyearly mother---infantskin-to-skincontactandbreastfeedingstatus.J MidwiferyWomensHealth.2007;52:116---25.
4.WHO---WorldHealthOrganization. Baby-friendlyhospital ini-tiative: revised,updated and expanded for integrated care. Section2.Strengtheningandsustainingthebaby-friendly hos-pitalinitiative:acourse fordecision-makers.Geneva: World HealthOrganization;2009.
5.Ministérioda Saúde.Recomendac¸ãopara profilaxiada trans-missãoverticaldoHIVeterapiaanti-retroviralemgestantes. Brasília:MinistériodaSaúde;2004.
6.MinistériodaSaúde,SecretariadeVigilânciaemSaúde, Secre-tariadeAtenc¸ãoàSaúde.Manualnormativoparaprofissionais de saúde de maternidades da Iniciativa Hospital Amigo da Crianc¸a --- referência para mulheres HIV positivas e outras que não podem amamentar. Brasília: Ministério da Saúde; 2004.
7.Brasil.MinistériodaSaúdeInstitui,noâmbitodoSistemaÚnico
deSaúde,oProjetoNascer-Maternidades.Portarian◦2104,19
novembrode2002.
8.Ministério da Saúde. Manual técnico pré-natal e puerpério: atenc¸ãoqualificadaehumanizada.Brasília:MinistériodaSaúde; 2006.
9.OliveiraMI,SilvaKS,GomesJuniorSC,FonsecaVM.Resultadodo testerápidoanti-HIVapósoparto:umaameac¸aàamamentac¸ão aonascimento.RevSaudePublica.2010;44:60---9.
10.UniversidadeFederalFluminense.Gênero,PodereCidadania:
amulherésujeitonoprocessodecisóriodaamamentac¸ãoao
nascimentoquando o statusde HIVéignorado pelo servic¸o?
EditalMCT/CNPq/PR-SMPno.045/2005---Relac¸õesdeGênero,
MulhereseFeminismos.Processono.403015/2005-7.
11.Bustamante-TeixeiraMT1,FaersteinE,LatorreMdoR.Técnicas deanálisedesobrevida.CadSaudePublica.2002;18:579---94.
12.CarvalhoMS,AndreozziVL,Codec¸oCT,BarbosaMTS,Shimakura SE.Análisedesobrevida:teoriaeaplicac¸õesemsaúde.1sted. RiodeJaneiro:EditoraFiocruz;2005.
13.VictoraCG,HuttlySR,FuchsSC, OlintoMT.Therole of con-ceptualframeworksinepidemiologicalanalysis:ahierarchical approach.IntJEpidemiol.1997;26:224---6.
14.Carvalho ML, Valente JG, Assis SG, Vasconcelos AG. Modelo preditivodo usodecocaína emprisões doEstado doRio de Janeiro.RevSaudePublica.2005;39:824---31.
15.Esteves TM, Daumas RP, Oliveira MI, Andrade CA, Leite IC. Fatoresassociadosàamamentac¸ãonaprimeira horadevida: revisãosistemática.RevSaudePublica.2014;48:697---703.
16.TheofilogiannakouM,SkouroliakouM,GounarisA,Panagiotakos D,MarkantonisSL.Breast-feeding inAthens,Greece:factors associatedwithitsinitiationandduration.JPediatr Gastroen-terolNutr.2006;43:379---84.
17.Cakmak H, Kuguoglu S. Comparison of the breastfeeding patterns of mothers who delivered their babies per vagina and via cesarean section: an observational study using the LATCH breastfeeding charting system. Int J Nurs Stud. 2007;44:1128---37.
18.NakaoY,MojiK,HondaS,OishiK.Initiationofbreastfeeding within120minutesafterbirthisassociatedwithbreastfeeding atfour monthsamongJapanese women:a self-administered questionnairesurvey.IntBreastfeedJ.2008;3:1.
19.BoccoliniCS,CarvalhoML,OliveiraMI,LealMC,CarvalhoMS. Fatores que interferem no tempo entre o nascimento e a primeiramamada.CadSaudePublica.2008;24:2681---9.
20.MooreER,AndersonGC,BergmanN.Earlyskin-to-skincontact for mothers and their healthy newborn infants. Cochane DatabaseSystRev.2012:5.