SOCIEDADE BRASILEIRA DE ORTOPEDIA E TRAUMATOLOGIA
w w w . r b o . o r g . b r
Original
Article
Reconstruction
of
the
medial
patellofemoral
ligament
by
means
of
the
anatomical
double-bundle
technique
using
metal
anchors
夽
David
Sadigursky
a,b,∗,
Matheus
Simões
de
Melo
Laranjeira
b,
Marzo
Nunes
a,
Rogério
Jamil
Fernandes
Caneiro
a,
Paulo
Oliveira
Colavolpe
aaClínicaOrtopédicaTraumatológica,Salvador,BA,Brazil
bFaculdadedeTecnologiaeCiências,Salvador,BA,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory: Received5July2015 Accepted30July2015 Availableonline27April2016
Keywords: Ligamentpatellar Patellardislocation Patella
Knee
Reconstructivesurgicalprocedures
a
b
s
t
r
a
c
t
Objective:Toevaluatedouble-bundlereconstructionofthemedialpatellofemoralligament (MPFL)usingagraftfromthesemitendinosustendonandfixationwithmetalanchorsover themediumterm.
Methods:Thiswasaprospectivecross-sectionalstudy.Afterapprovalfromtheresearch ethicscommittee,31patientswithpatellofemoralinstabilitywhounderwentMPFL recon-structionbymeansoftheanatomicaldouble-bundletechnique,withfixationusingmetal anchors,wereanalyzedbetweenMay2010andJanuary2015.Toevaluatetheeffectiveness oftheMPFLreconstructionsurgery,theKujalascaleandtheTegner–Lysholmscorewere assessedbeforetheprocedureandoneyearafterwards,alongwithclinicaldatasuchas painlevels,rangeofmotionandJsign.ThedataweretabulatedintheExcel®softwareand wereanalyzedusingtheSPSSStatistics®software,version21.Thestatisticalanalysiswas performedusingtheWilcoxonTtestandtheMcNemartest.
Results:ThemeanpreoperativescorefromtheKujalatestwas45.64±1.24andthe post-operativescorewas94.03±0.79(p<0.001).The preoperativeTegner–Lysholm scorewas 40.51±1.61andthepostoperativescorewas91.64±0.79(p<0.001).Thepreoperativerange ofmotionwas125.96±2.11andthepostoperativerangewas138.38±1.49(p<0.05). Conclusion:MPFLreconstructionbymeansoftheanatomicaldouble-bundletechniqueis easilyreproducible,without episodesof recurrence,with satisfactory results regarding restorationofstabilityandfunctionofthepatellofemoraljoint.
©2015SociedadeBrasileiradeOrtopediaeTraumatologia.PublishedbyElsevierEditora Ltda.ThisisanopenaccessarticleundertheCCBY-NC-NDlicense(http:// creativecommons.org/licenses/by-nc-nd/4.0/).
夽
StudyconductedatClínicaOrtopédicaTraumatológica(COT),Salvador,BA,Brazil.
∗ Correspondingauthor.
E-mail:davidsad@gmail.com(D.Sadigursky).
http://dx.doi.org/10.1016/j.rboe.2015.07.011
Reconstruc¸ão
do
ligamento
patelofemoral
medial
pela
técnica
anatômica
do
duplo-feixe
com
âncoras
metálicas
Palavras-chave: Ligamentopatelar Luxac¸ãopatelar Patela
Joelho
Procedimentoscirúrgicos reconstrutivos
r
e
s
u
m
o
Objetivo:Avaliar,emmédioprazo,areconstruc¸ãodoligamentopatelofemoralmedial(LPFM) comduplo-feixecomenxertodotendãosemitendíneoefixac¸ãocomâncorasmetálicas. Métodos: Estudoprospectivodecortetransversal.Demaiode2010ajaneirode2015,após aprovac¸ãodocomitêdeéticaempesquisa,foramanalisados31pacientescominstabilidade patelofemoral,submetidosàcirurgiadereconstruc¸ãodoligamentopatelofemoralmedial (LPFM)comatécnicaanatômicadoduplo-feixecomfixac¸ãocomâncorasmetálicas.Para avaliaraeficáciadacirurgiadereconstruc¸ãodoLPFM,foramutilizadasaescaladeKujala eoescoredeTegner-Lysholm,antesdoprocedimentoeapósumano.Foramavaliadosos dadosclínicoscomooarcodemovimento,presenc¸adoSinaldoJeníveldedor.Osdados foramtabuladosnoprogramaExcel®eanalisadoscomoprogramaSPSSStatistics®versão 21.AanáliseestatísticafoifeitacomotesteTdeWilcoxoneotestedeMcNemar. Resultados: Amédiadosresultadosobtidosnopré-operatóriocomotestedeKujalafoide 45,64±1,24enopós-operatóriode94,03±0,79(p<0,001).Oescoredojoelhode Tegner-Lysholm alcanc¸adofoi de 40,51±1,61no pré-operatório, para91,64±0,79 (p<0,001)no pós-operatório.Oarcodemovimentoobtevemédiade12,596±2,11nopré-operatórioe 13,838±1,49nopós-operatório(p<0,05).
Conclusão: Areconstruc¸ãodoLPFMcomduplo-feixeéumatécnicadefácilreproduc¸ão,sem episódiosderecidiva,ecomresultadosadequadosparaarestaurac¸ãodaestabilidade.
©2015SociedadeBrasileiradeOrtopediaeTraumatologia.PublicadoporElsevier EditoraLtda.Este ´eumartigoOpenAccesssobumalicenc¸aCCBY-NC-ND(http:// creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
Patellardislocationisaverycommonconditionin orthope-dics.Itprimarilyaffectsyoungpatientsofbothsexes,witha higherincidenceinfemales,althoughinmales,casestendto bemoresevere.1
Recurrentpatellardislocationisdefinedastwoor more episodesofdislocation, orsymptoms ofpatellarinstability thatlastformorethanthreemonthsafterthefirstdislocation episode.2
Themedialpatellofemoralligament(MPFL)wasdescribed byConlanetal.3asthemajorrestrainttolateraldisplacement ofthepatella,accountingforapproximately53%ofthe resis-tance,andcontrollingitstrajectoryduringtheexecutionof thefullrangeofmotion.3,4Inmostpatients,thisligamentis rupturedduringacutepatellardislocation.5
Camanhoetal.6 demonstratedthatspecificMPFL recon-structionafterthedislocationepisodeleadstomorefavorable results when compared with conservative treatment, with lowerchanceofrecurrence.
Therefore,itisknownthatsurgicaltreatmentisnecessary torestorethepatellarstability.7Anumberofsurgical tech-niquesforMPFLreconstructionhavebeendescribedforthe treatmentofthiscondition.8
Despiteitsbiomechanicalimportance,thevalueofMPFL reconstructionhasonlyrecentlybeenacknowledged,mostly inthelasttwodecades.9Despitethewiderangeoftechniques describedforitsreconstruction,withdifferentgraftsources andfixationmethods,thereisgrowingevidenceofgood clin-icaloutcomes forthis surgery,butthereare stillimportant
unsatisfactoryresults,around12.5%,asinthefindingsof Sing-haletal.10Themaincomplicationafterreconstructionisjoint stiffnessandpainaftertheprocedure.
Onecauseofthiscomplicationisthenon-anatomicalgraft positioninginMPFLreconstruction.Itwasobservedthatsmall errorsofupto5mmfromtheidealpositionorexcessive ten-sioningofthegraft(>2N),causeanincreaseinthepressure forceson themedialaspectofthepatella.Thiscreatesthe needfortechniquesthatcanproperlydistributegrafttension onthepatellaandcloserreproductionoftheanatomy.11–13
Fromthemeanandmaximumflexion,Sandmeieretal.14 and Parkeret al.15 demonstratedthatisolated MPFL recon-struction was not able torestore normal patellar tracking. FailuretorestoreproperMPFLanatomyorisometrymaycause thisresultand,therefore,limitthesuccessforlonger follow-ups.13
Kangetal.16introducedtheconceptoffunctionalbundles oftheMPFL.Theligamenthasathinlayerthatconnectsthe femoralcondyle tothesuperomedial border ofthe patella. Theinferiorfibersactasastaticstabilizer,andthesuperior fibersactinthedynamicstabilizationofthepatella,dueto theircloserelationshipwiththetendonofthevastusmedialis obliquus.
Thekeytoachievingfavorablelong-termresultsis attach-ingthegraftinthemostanatomicalformpossible.However, theidealfixationmethodremainsamatterofdiscussion. Dif-ferentfixationmethodshavebeendescribed,suchasfixation bybonetunnels,internalbuttons,andanchors.17
Ithasbeen postulated thatclinical resultswiththe use of metalanchorsarecomparablewithpublishedpreviousdata regardinganatomicdouble-bundleMPFLreconstructionusing bonetunnelsinthepatella.10,19–23
Thisstudyaimedtoassesstheeffectivenessofanatomic double-bundleMPFLreconstructionusingthesemitendinosus andfixationwithmetalanchorsinthemedialborderofthe patella.
Material
and
methods
TheprospectivestudywasconductedfromMay2010to Jan-uary2015,afterapprovaloftheResearchEthicsCommittee via Plataforma Brasil. The study included 31 patients with patellofemoralinstabilitywhounderwent anatomic double-bundleMPFLreconstructionandfixationwithmetalanchors. All patients had history of more than two episodes of patellar dislocation, and were selected toundergo surgical MPFL reconstruction through the double-bundle technique describedbySongetal.,18usingY-shapedmetalanchorsin thepatella.21
Patientswereattendedinareferralorthopedicshospitalby theinstitutions’kneesurgerygroup.Theywereassessed pre-operativelyand12monthsaftertheprocedure.Thephysical examination was documented through the patellar appre-hension test, J-sign, and range of motion. To evaluatethe effectivenessofthereconstruction,theKujalaet al.24 clini-calandfunctionalquestionnaireswereapplied,aswellasthe Lysholm–Tegnerscores25;theywereappliedpre-and postop-eratively.
TheKujalascale24addressessymptomsrelatedtoanterior kneepain(patellofemoraldisorders).Itevaluatessubjective symptoms,suchaspainandfunctionlimitations,whichare scored from 0 to 100, according to the complaints of the patient; 100 represents the complete absence of pain and limitationsand0,constantpainandseverallimitations.The assessedparametersare:pain,claudication,patellar sublux-ation, walking,stair climbing, and staying seated for long periodswiththekneesbent.
TheLysholm–Tegner score25 consistsof eightquestions withclosedanswers.Eachquestion hasanassigned value, whicharethenadded.Thefinalresultisexpressedboth nom-inallyandordinally:“Excellent,”95–100points;“Good,”84–94 points;“Regular,”65–83points;and“Bad,”forscoresequalto orlessthan64.
Patients with recurrent patellar dislocation (over two episodes),agedlessthan45years(mean29years),andwith magneticresonanceimagingshowingextensiveruptureofthe medialpatellarstabilizerswithoutosteochondrallesionwere included.
Theexclusioncriteria comprisedpatientswith congeni-taldiseases;thosewithosteochondrallesionsofthepatella; those with distance between the anterior tibial tuberosity andtrochleargroove(ATT-TG) greater than20mm, indicat-ingmedializationoftheanteriortibialtuberosity(ATT);those olderthan 45 years;and thosewith inflammatoryor post-traumaticarthritis.
Nopatientunderwent furthertreatmentwithrelease of thelateralretinaculum,trochleoplasty,osteotomy,orcartilage
procedures. All patientswere assessedby medical history-taking,physicalexamination,radiographicassessments,and computedtomographyinthepreoperativeperiod.The patel-larheightwasmeasuredusingtheCaton–Deschampsindex26 andtrochleardysplasia,bytheDejouretal.classification.27
AsemitendinosustendongraftwasusedforMPFL recon-struction.Thefixationwasperformedwithtwo5-mmmetal anchorsinthepatellaandanY-shapedinterferencescrewin thefemur,forcreatingbothligamentbundlesandfixationin independentkneeflexionangles.16
Surgicaltechnique
Thepatientwasplacedinthedorsaldecubitusposition,under spinalanesthesia.Initially,anarthroscopywasperformedin theaffectedkneefortheidentificationofassociatedinjuries orremovalofintra-articulardebris.Lateralretinacularrelease wasnotperformed.
The semitendinosus tendonwas then resected through a 2–3-cm incision over the insertion of the pes anserinus tendons.Thefasciaofthesartoriusmusclewaspushedout throughanobliqueincision,andthetendonwasexposedand resected.Thesemitendinosustendonwasused,asitsgreater lengthandvolumeallowedforabettergraftmanipulation.
The point of graft fixation in the femur was identified withtheaidofprofileradioscopy,accordingtothe parame-tersdescribedbySchöttleetal.28Themedialapproachtothe femurwasperformedaftertheanatomicalpointwas identi-fied.Then,aguide-wire,anterior-andproximal-directed,was inserted,avoidingpenetrationintotheposteriorregionofthe femoralcondyle.
Afterconfirmingtheproperplacementoftheguide-wire,a tunnelwasdrilledwithapowerdrillofthesamediameteras thedoublegraft.Thefoldedsemitendinosustendongraftwas insertedthroughthefemoraltunnel(Fig.1),andfixedwithan interferencescrew(Fig.2).
Alongitudinalthirdincisionwasmadeunderthemedial border ofthepatella.29Thegrooveonthemedialborderof thepatellawascreatedabovethetransitionwiththeposterior chondralfaceofthepatellawiththeaidofacuretteto accom-modatethegraft.Two5-mmmetalanchorswereintroduced and positioned in the two proximal thirds of the patella, 10–15mm of the joint, with a distanceof 15mm between them.Themostdistalbundle,theinferior-straight(IS),was firstestablishedwiththepatellaatapproximately30◦ofknee flexion;then,themostproximalbundle,thesuperior-oblique (SO),atabout60◦offlexion,inaccordancewiththestudiesby Sadigurskyetal.30andStephenetal.13Theremainingmedial retinaculumwassuturedunderthetendon(Fig.3).
Afterfixation, thepatellarposition wasverifiedthrough arthroscopicimageandbythemobilityofthepatellaataround one-quarterofitssize.21
Postoperativeperiod
Fig.1–Afterthesemitendinosustendonwaspassed throughthefemoraltunnel,markedat30mmatthedistal end.
loadwasallowedastolerated.Exercisesinclosedkineticchain wereallowedfromthefourthweekaftersurgeryonwards.31
Contactsportsandrotationwereallowedaftersixmonths ofthesurgery.31
Statisticalanalysis
DataweretabulatedinExcel®forMacOSXandanalyzedusing SPSSStatistics®forMacOSX,version21.Categoricaldatawere
Fig.2–Passageofthegraftinthefemoraltunneland fixationwithmetallicinterferencescrew.
Fig.3–Fixationoftheinferior-straight(IS)bundle,followed bythesuperior-oblique(SO)atindependentkneeflexion angles,30◦and60◦,respectively.
presentedasproportionsandquantitativedataasmedians, means,andstandarddeviations.Statisticalanalysiswas per-formedwiththeWilcoxonTtestwithalphaerrorof0.05and McNemartest,alsowithalphaerrorof0.05.
Results
Table1describesthestudysample.Thestudyincluded31 sub-jects,withameanageof29.38andstandarddeviation(SD)of 8.11.Sixteenpatientswerefemale(51.6%),and15weremale (48.4%). Themostaffected knee was the right, in18 cases (58.06%);13subjects(41.9%)hadtheleftkneeaffected.
Thepatellarapprehensiontestwaspositiveinall31(100%) patients preoperatively, and it was negative in 31 (100%) postoperatively.TheJ-sign was positivein24 cases(77.4%) preoperativelyandnegativeinseven(22.6%);positiveinfive cases(16.1%)andnegativein26(83.9%)postoperatively.The Caton–Deschampsindexwaslessthanorequalto1in21cases (67.7%);itremainedbetween1.1and1.2infivecases(16.1%), andwasgreaterthanorequalto1.3infivepatients(16.1%). Eighteencases(58.1%)hadATT-TGbetween12and15mm;13 (41.9%),between15and20mm;andnocasehadATT-TGabove 20mm.Dejour typeAtrochleardysplasiawaspresentin14 subjects(45.2%);typeB,ineight(25.8%);typeC,intwo(6.5%);
Table1–Sociodemographicdescription.
Variable N(%) Mean±SD
Age 31 29.38±8.11
Sex
Male 15(48.4)
Female 16(51.6)
Affectedknee
Right 18(58.06)
Table2–Clinicaldatainthepre-andpostoperative period.
Variable PreoperativeN
(%)
PostoperativeN
(%)
Patellarapprehensiontest
Positive 31(100) 0
Negative 0 31(100)
J-sign
Positive 24(77.4) 5(16.1)
Negative 7(22.6) 26(83.9)
Caton–Deschamps(mean±SD) 1.01±0.17
≤1.0 21(67.7) –
1.1–1.2 5(16.1) –
≥1.3(high) 5(16.1) –
ATT-TG(mean±SD) 15.4±0.19
12–15mm(normal) 18(58.1) –
15–20mm(high) 13(41.9) –
>20 0 –
Trochleardysplasia
A 14(45.2) –
B 8(25.8) –
C 2(6.5) –
Zero 7(22.6) –
andsevenpatientsdidnotpresent anydegreeofdysplasia (22.5%).ThesefindingsarepresentedinTable2.
ThemeanpreoperativeKujalascore24was45.64(SD:1.24; median: 49); the post-operative mean was 94.03 (SD: 0.79; median:96), withstatistical significanceofp=0.001. Inthe categorizedanalysisofthescore,31(100%)subjectspresented apoorpreoperativescore,andallsubjects(100%)presented agood/excellent post-operativescore. Themean preopera-tiveLysholm–Tegner25scorewas40.51(SD:1.61;median:43) thepostoperativemeanwas91.64(SD0.79;median:90),with statisticalsignificanceof0.001.Table3presentsthefindings fromthequestionnaires.Additionally,nopatient(100%) pre-sentedrecurrence.Themeanpostoperativerangeofmotion was138.38±1.49,andthemeanpreoperativerangeofmotion was125.96±2.11,withstatisticalsignificance(p<0.05).
Table4–Pre-andpostoperativepatellarapprehension testscores.
Patellarapprehensiontest
Preoperative Postoperative p
Absent Present
Present 31 0 0.001
Absent 0 31
Table4showstheanalyticalrelationshipbetweenthe pre-andpostoperativepatellarapprehensiontest.Thedifference betweentheseresultswasstatisticallysignificant(p<0.05).
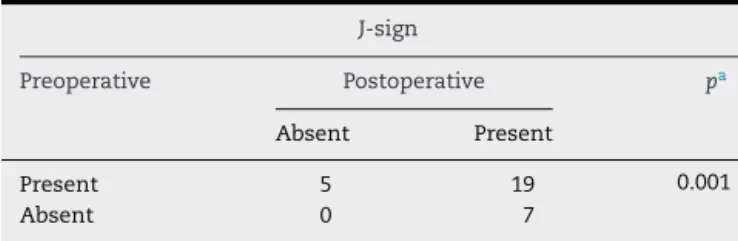
TheMcNemartestwasalsoappliedtotheJ-signratioin both moments (pre- and postoperative), and astatistically significant difference in the periods studied was observed (Table5).
Discussion
Fromthe1990sonwards,MPFLreconstructionhasbecomethe techniqueofchoicebymostauthors.32Exceptincaseswhere ATT-TGisabove20mm,orincasesoftrochleardysplasiawith supratrochlearspurabove5mm,isolatedMPFLreconstruction hasbeenproventobeasuitableandeffectivetechniquefor thecorrectionofpatellarinstability.33Hopperetal.,34when assessing72patients,proposedthatisolatedMPFL reconstruc-tionshouldnotbeperformedinpatientswithseveretrochlear dysplasia.Inoverhalfofpatients,amildtomoderatetrochlear dysplasia wasidentified, but it was foundnottoinfluence theresults.PatientswithDejourtypeDtrochleardysplasia27 wereexcludedfromthisstudy.Oftheselectedpatients,eight (25.8%)hadtypeBdysplasia,butwithoutsupratrochlearspurs above5mm.
Thisfinding is similarto thosebyArendt35 and Steiner etal.,36whoobservedgoodresultsinpatientswithtrochlear dysplasiawhounderwentisolatedMPFLreconstruction.The postoperativerangeofmotionimprovedby15◦inthemedian and12◦inthemean.Thep-valuewasstatisticallysignificant.
Table3–Surgicalandclinicalscores.
Variable PreoperativeN
(%)
PostoperativeN
(%)
pa
Rangeofmotion (median/mean±SD)
125/125.96±2.11 140/138.38±1.49 0.1
Kujalascore
(median/mean±SD)
49/45.64±1.24 96/94.03±0.78 0.001
Poor 31(100) 0
Regular 0 0
Good/excellent 0 31(100)
Lysholmscore 43/40.51±1.61 90/91.64±0.79 0.001
Poor 31(100) 0
Regular 0 0
Good 0 18(58.1)
Excellent 0 13(41.9)
Table5–Pre-andpostoperativeJ-sign.
J-sign
Preoperative Postoperative pa
Absent Present
Present 5 19 0.001
Absent 0 7
a McNemartest,consideredsignificantwhenp<0.05.
In2009, Kang et al.16 described the anatomy and func-tion ofbothMPFL bundles.TheSO bundle,along withthe vastusmedialis obliquus, tracks the kneecapmedially and promotesadynamicconstraint.Inturn,the ISbundleacts asstaticrestrainttobalancetheresultinglateralforces act-ingonthepatella.Thus,thereconstructionofbothbundles couldincreasethestabilityduringthefirstflexionanglesand above30◦ofkneeflexion,whichwouldallowfortension main-tenanceduringthemovementarc,promotedbyeachbundle independently.
Philippotetal.37describedtheroleofthemedial stabiliz-ingligamentsofthepatella,medialpatellotibial(MPTL)and medialpatellomeniscal(MPML),whichpresenttheirhighest performanceatanglesabove45◦ofkneeflexion.The recon-structionofMPTLhasbeengainingpopularityinpatientsboth inthegrowthphase(withopenphysis)andadults.38–40 Dur-ingthemovementarc,fromthetotallength(0◦)to90◦flexion, theMPTLandMPMLcontributewith28%and48%againstthe lateralizationofthepatella,23%and71%againstinclination, and32%and92%againstrotation,respectively.Thisfinding cannotbedisregardedwhenplanningthecorrectionof patel-larinstability.37,38 However,despitethe growing interest in MPTLreconstruction,inordertodecreasethedisplacement ofthepatellaathigheranglesofflexion,possibly eliminat-ingtheinvertedJ-sign,todatethereisnodataprovingthe superiorityoftheclinicalresultsincombineddouble-bundle reconstructionoftheMPTLandMPML.37,39
ThefixationofMPFLbundlesatdifferentangles(theIS bun-dleat0◦ andthe OSat30◦)wassuggestedbyKanget al.41 However,theauthorsbelievethattheOSbundleshouldbe fix-atedat60◦withminimaltension,andtheISbundleataround 30◦,basedonthestudiesbySadigurskyetal.30andHanetal.,20 inordertopreventoverpressureinthemedialaspectofthe patellaand,consequently,anteriorkneepain.Stephenetal.13 demonstratedthattheanatomicalreconstructionpositioned witha2-Ntensionunderthegraft,fixedat30◦or60◦ofknee flexion,restoresnormalcontactpressureinthelateral patel-laraspectaswellasitsappropriateflexion-extensionpath. Songetal.,42inabiomechanicalstudy,demonstratedthatthe lengthoftheMPFLfibersvarieswiththedegreeofkneeflexion. Thesuperiorfibers reachtheirmaximumlengthatsmaller angles;theinferiorfibers,atgreaterflexionangles.
Theauthors observedimprovementsin patellar sublux-ation at around 20◦ to 30◦ of knee flexion, demonstrated through negative results in the apprehension test. The invertedJ-signwaspositivein24patients(77.4%) preopera-tivelyandinonlyfive(16.1%)postoperatively.Thefivepatients (16.1%)whoseCaton–Deschampsindexwasgreaterthan1.3, whichcharacterizedhighpatella,showedthepersistenceof
the J-sign, confirming this asafactor ofpoor prognosisin isolated MPFL reconstruction regarding the persistence of residualsubluxationofthepatellainkneeflexionanglesabove 45◦.
Inameta-analysisconductedbySinghaletal.,10a persis-tentpatellarinstabilitywasobserved,fromsubtletofrank,in around4.6%ofcasespostoperatively.Stiffnesswasthemost frequentcomplication(30%).However,theattachmentofthe double-bundlegraftwasmadeinthesameangleandunder thesametension.Inthiscase,theprocedureisperformedby initiallyfixatingthepatella.ThisC-shapedgraftfixation tech-niquecouldleadtoworseoutcomes,withincreasedrestriction ofnormalpatellarmobility.Kangetal.21,41demonstratedthat Y-shapedgraftfixation,whichstartsinthefemur,followedby fixationofeachbundleindependently,canimprovepatellar functionandreducepossiblecomplications.43
Through the Kujala24 and Lysholm–Tegner scores,25 the effectivenessofdouble-bundle MPFL reconstruction canbe demonstrated. The results show a recovery of the biome-chanical function of the patella. The mean Kujala score24 increasedfrom45.64preoperativelyto94.03postoperatively. In theLysholm–Tegner,25 therewas anincreasefrom 40.51 preoperativelyto91.64postoperatively.Ofthe31patients,18 (58.1%)movedto“good”and13patients(41.9%)to“excellent” outcomes.Theseresultsareveryclosetothosefoundinthe meta-analysisbySinghalet al.,10 but withfewer complica-tions.
Based on experimental and anatomical studies, the authorsarguethatMPFLreconstructionshouldbemadeboth isometricallyandanatomically.10,22 Giventheresultsofthis study,aswellasthosebyWangetal.,22MPFLreconstruction shouldbeperformedanatomically,withindependentfixation ofbothbundles.16,21,41
In this study, it was observed that the double-bundle MPFLreconstructionusingsemitendinosustendongraftand fixationwithmetalanchorsinindependentflexionangles pre-sentedfavorableresults,withoutrecurrenceepisodes,pain, oroverloadinthepatellofemoraljoint,andwithsatisfactory rangeofmotionandpossibilityofreturntopreviousactivities. Aweaknessofthestudywasthefactthatitwasconducted atasinglecenter,withoutacomparisongroupusingother correctiontechniquesforpatellarinstability.Nonetheless,the presentsamplewasveryclosetothatofstudieson double-bundleMPFLreconstructionintheliterature.5,7,8,10
Conclusion
Double-bundleMPFLreconstructionusingfixationwithmetal anchorsandindependentbundlefixationwas showntobe effectivebythe resultsobserved inthis study,suchasthe significantimprovementinthe scoreofthe protocols used withoutrelapseepisodesandthereductionofsubluxationat anglesabove45◦ofkneeflexion.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
Acknowledgements
To the members of the knee surgery group ofthe Clínica OrtopédicaTraumatológica(COT).
r
e
f
e
r
e
n
c
e
s
1. BitarAC,DemangeMK,D’EliaCO,CamanhoGL.Traumatic patellardislocation:nonoperativetreatmentcomparedwith MPFLreconstructionusingpatellartendon.AmJSportsMed. 2012;40(1):114–22.
2. NomuraE.Classificationoflesionsofthemedial
patello-femoralligamentinpatellardislocation.IntOrthop. 1999;23(5):260–3.
3. ConlanT,GarthWP,LemonsJE.Evaluationofthemedial soft-tissuerestraintsoftheextensormechanismoftheknee. JBoneJointSurgAm.1993;75(5):682–93.
4. DesioSM,BurksRT,BachusKN.Softtissuerestraintsto lateralpatellartranslationinthehumanknee.AmJSports Med.1998;26(1):59–65.
5. ColvinAC,WestRV.Patellarinstability.JBoneJointSurgAm. 2008;90(12):2751–62.
6. CamanhoGL,ViegasAC,BitarAC,DemangeMK,Hernandez AJ.Conservativeversussurgicaltreatmentforrepairofthe medialpatellofemoralligamentinacutedislocationsofthe patella.Arthroscopy.2009;25(6):620–5.
7. RedziniakDE,DiduchDR,MihalkoWM,FulkersonJP,Novicoff WM,Sheibani-RadS,etal.Patellarinstability.JBoneJoint Surg.2009;91(9):2264–75.
8.ShahJN,HowardJS,FlaniganDC,BrophyRH,CareyJL, LattermannC.Asystematicreviewofcomplicationsand failuresassociatedwithmedialpatellofemoralligament reconstructionforrecurrentpatellardislocation.AmJSports Med.2012;40(8):1916–23.
9.AmisAA,FirerP,MountneyJ,SenavongseW,ThomasNP. Anatomyandbiomechanicsofthemedialpatellofemoral ligament.Knee.2003;10(3):215–20.
10.SinghalR,RogersS,CharalambousCP.Double-bundlemedial patellofemoralligamentreconstructionwithhamstring tendonautograftandmediolateralpatellartunnelfixation:a meta-analysisofoutcomesandcomplications.BoneJointJ. 2013;95(7):900–5.
11.EliasJJ,CosgareaAJ.Technicalerrorsduringmedial patellofemoralligamentreconstructioncouldoverload medialpatellofemoralcartilage:acomputationalanalysis. AmJSportsMed.2006;34(9):1478–85.
12.ServienE,FritschB,LustigS,DemeyG,DebargeR,LapraC, etal.Invivopositioninganalysisofmedialpatellofemoral ligamentreconstruction.AmJSportsMed.2011;39(1): 134–9.
13.StephenJM,KaiderD,LumpaopongP,DeehanDJ,AmisAA. Theeffectoffemoraltunnelpositionandgrafttensionon patellarcontactmechanicsandkinematicsaftermedial patellofemoralligamentreconstruction.AmJSportsMed. 2014;42(2):364–72.
14.SandmeierRH,BurksRT,BachusKN,BillingsA.Theeffectof reconstructionofthemedialpatellofemoralligamenton patellartracking.AmJSportsMed.2000;28(3):345–9.
15.ParkerDA,AlexanderJW,CondittMA,UzodinmaON,Bryan WJ.Comparisonofisometricandanatomicreconstructionof themedialpatellofemoralligament:acadavericstudy. Orthopedics.2008;31(4):339–43.
16.KangHJ,WangF,ChenBC,SuYL,ZhangZC,YanCB. Functionalbundlesofthemedialpatellofemoralligament. KneeSurgSportsTraumatolArthrosc.2010;18(11):1511–6.
17.LenschowS,SchliemannB,GestringJ,HerbortM,SchulzeM, KöstersC.Medialpatellofemoralligamentreconstruction: fixationstrengthof5differenttechniquesforgraftfixationat thepatella.Arthroscopy.2013;29(4):766–73.
18.SongSY,KimIS,ChangHG,ShinJH,KimHJ,SeoYJ.Anatomic medialpatellofemoralligamentreconstructionusingpatellar sutureanchorfixationforrecurrentpatellarinstability.Knee SurgSportsTraumatolArthrosc.2014;22(10):2431–7.
19.SchöttlePB,HenslerD,ImhoffAB.Anatomicaldouble-bundle MPFLreconstructionwithanaperturefixation.KneeSurg SportsTraumatolArthrosc.2010;18(2):147–51.
20.HanH,XiaY,YunX,WuM.Anatomicaltransversepatella doubletunnelreconstructionofmedialpatellofemoral ligamentwithahamstringtendonautograftforrecurrent patellardislocation.ArchOrthopTraumaSurg.
2011;131(3):343–51.
21.KangH,CaoJ,YuD,ZhengZ,WangF.Comparisonof2 differenttechniquesforanatomicreconstructionofthe medialpatellofemoralligament:aprospectiverandomized study.AmJSportsMed.2013;41(5):1013–21.
22.WangC,MaL,ZhouJ,JiG,WangH,WangF,etal.
Double-bundleanatomicalversussingle-bundleisometric medialpatellofemoralligamentreconstructionforpatellar dislocation.IntOrthop.2013;37(4):617–24.
23.ZanonG,MarulloM,BenazzoF.Double-bundlemedial patellofemoralligamentreconstructionwithasinglepatellar tunnel.ArthroscTech.2013;2(4):e401–4.
24.KujalaUM,OstermanK,KormanoM,NelimarkkaO,Hurme M,TaimelaS.Patellofemoralrelationshipsinrecurrent patellardislocation.JBoneJointSurgBr.1989;71(5):788–92.
26.PhillipsCL,SilverDT,SchranzPJ,MandaliaV.The
measurementofpatellarheight:areviewofthemethodsof imaging.JBoneJointSurgBr.2010;92(8):1045–53.
27.DejourH,WalchG,Nove-JosserandL,GuierC.Factorsof patellarinstability:ananatomicradiographicstudy.Knee SurgSportsTraumatolArthrosc.1994;2(1):19–26.
28.SchöttlePB,SchmelingA,RosenstielN,WeilerA. Radiographiclandmarksforfemoraltunnelplacementin medialpatellofemoralligamentreconstruction.AmJSports Med.2007;35(5):801–4.
29.MochizukiT,NimuraA,TateishiT,YamaguchiK,MunetaT, AkitaK.Anatomicstudyoftheattachmentofthemedial patellofemoralligamentanditscharacteristicrelationships tothevastusintermedius.KneeSurgSportsTraumatol Arthrosc.2013;21(2):305–10.
30.SadigurskyD,GobbiRG,PereiraCAM,PécoraJR,CamanhoGL. Métododeensaiobiomecânicoparaanáliseda
isometricidadenareconstruc¸ãodoligamentopatelofemoral medial.RevBrasOrtop.2012;47(5):598–605.
31.FisherB,NylandJ,BrandE,CurtinB.Medialpatellofemoral ligamentreconstructionforrecurrentpatellardislocation:a systematicreviewincludingrehabilitationand
return-to-sportsefficacy.Arthroscopy.2010;26(10):1384–94.
32.MulfordJS,WakeleyCJ,EldridgeJD.Assessmentand managementofchronicpatellofemoralinstability.JBone JointSurgBr.2007;89(6):709–16.
33.SchöttleP,SchmelingA,RomeroJ,WeilerA.Anatomical reconstructionofthemedialpatellofemoralligamentusinga freegracilisautograft.ArchOrthopTraumaSurg.
2009;129(3):305–9.
34.HopperGP,LeachWJ,RooneyBP,WalkerCR,BlythMJ.Does degreeoftrochleardysplasiaandpositionoffemoraltunnel influenceoutcomeaftermedialpatellofemoralligament reconstruction?AmJSportsMed.2014;42(3):716–22.
35.ArendtEA,DejourD.Patellainstability:buildingbridges acrosstheoceanahistoricreview.KneeSurgSports TraumatolArthrosc.2013;21(2):279–93.
36.SteinerTM,Torga-SpakR,TeitgeRA.Medialpatellofemoral ligamentreconstructioninpatientswithlateralpatellar instabilityandtrochleardysplasia.AmJSportsMed. 2006;34(8):1254–61.
37.PhilippotR,BoyerB,TestaR,FarizonF,MoyenB.Theroleof themedialligamentousstructuresonpatellartrackingduring kneeflexion.KneeSurgSportsTraumatolArthrosc.
2012;20(2):331–6.
38.SobhyMH,MahranMA,KamelEM.Midtermresultsof combinedpatellofemoralandpatellotibialligaments reconstructioninrecurrentpatellardislocation.EurJOrthop SurgTraumatol.2013;23(4):465–70.
39.ZaffagniniS,GrassiA,MarcheggianiMuccioliGM,Luetzow WF,VaccariV,BenziA,etal.Medialpatellotibialligament (MPTL)reconstructionforpatellarinstability.KneeSurg SportsTraumatolArthrosc.2014;22(10):2491–8.
40.GiordanoM,FalcigliaF,AulisaAG,GuzzantiV.Patellar dislocationinskeletallyimmaturepatients:semitendinosous andgracilisaugmentationforcombinedmedial
patellofemoralandmedialpatellotibialligament reconstruction.KneeSurgSportsTraumatolArthrosc. 2012;20(8):1594–8.
41.KangHJ,CaoJH,PanS,WangXJ,YuDH,ZhengZM.The horizontalY-shapedgraftwithrespectivegrafttensionangles inanatomicaltwo-bundlemedialpatellofemoralligament reconstruction.KneeSurgSportsTraumatolArthrosc. 2014;22(10):2445–51.
42.SongSY,PangCH,KimCH,KimJ,ChoiML,SeoYJ.Length changebehaviorofvirtualmedialpatellofemoralligament fibersduringinvivokneeflexion.AmJSportsMed. 2015;43(5):1165–71.