REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
PublicaçãoOficialdaSociedadeBrasileiradeAnestesiologiawww.sba.com.br
SCIENTIFIC
ARTICLE
Axillary
local
anesthetic
spread
after
the
thoracic
interfacial
ultrasound
block
---
a
cadaveric
and
radiological
evaluation
Patricia
Alfaro
de
la
Torre
a,
Jerry
Wayne
Jones
Jr.
b,
Servando
López
Álvarez
c,
Paula
Diéguez
Garcia
c,
Francisco
Javier
Garcia
de
Miguel
d,
Eva
Maria
Monzon
Rubio
e,
Federico
Carol
Boeris
f,
Monir
Kabiri
Sacramento
g,
Osmany
Duany
h,
Mario
Fajardo
Pérez
i,∗,
Borja
de
la
Quintana
Gordon
jaTajoUniversityHospital,Madrid,Spain
bUniversityofTennesseeHealthScienceCenter/RegionalOneHealth,CollegeofMedicine,DepartmentofAnesthesiology,TN,
USA
cHospitalComplexoHospitalariodeACoru˜na,Coru˜na,Spain
dHospitalGeneraldeSegovia,DepartamentodeAnestesia,Segovia,Spain eTajoUniversityHospital,DepartamentodeAnestesia,Madrid,Spain fHospitalUniversitarioParcTauliSabadell,Sabadell,Spain
gHospitalUniversitariodeGuadalajara,Guadalajara,Spain
hPrimaryCareandChronicPainManagementAttending,DepartmentofVeteransAffairs,Muskogee,OK,USA iHospitalUniversitariodeMóstoles,Madrid,Spain
jHospitalUniversitariodeMóstoles,DepartamentodeAnestesia,Madrid,Spain
Received23February2015;accepted14April2015 Availableonline22June2016
KEYWORDS
Anesthesia, conduction; Axilla;
Intercostalmuscles; Brachialplexusblock; Intercostalnerves; Lymphnodeexcision; Ultrasonography
Abstract
Background: Oralopioidanalgesicshavebeenusedformanagementofperi-andpostoperative analgesiainpatientsundergoingaxillarydissection.Theaxillaryregionisadifficultzonetoblock anddoesnothaveaspecificregionalanesthesiatechniquepublishedthatoffersitsadequate blockade.
Methods:After institutional reviewboardapproval, anatomicandradiological studieswere conducted to determinethe deposition andspreadofmethylene blue andlocal anesthetic injected respectivelyinto theaxillaviathethoracicinter-fascialplane.MagneticResonance Imagingstudieswerethenconductedin15of34patientsscheduledforunilateralbreastsurgery thatentailedanyofthefollowing:axillaryclearance,sentinelnodebiopsy,axillarynodebiopsy, orsupernumerarybreasts,toascertainthedepositionandtimecourseofspreadofsolution withinthethoracicinterfascialplaneinvivo.
∗Correspondingauthor.
E-mail:mfajardoperez@yahoo.es(M.F.Pérez).
http://dx.doi.org/10.1016/j.bjane.2015.04.007
Results:Radiologicalandcadavericstudiesshowedthattheinjectionoflocalanestheticand methyleneblueviathethoracicinter-fascialplane,usingultrasoundguidetechnique,results inreliabledepositionintotheaxilla.Inpatients,theinjectionofthelocalanestheticproduced areliableaxillary sensoryblock.Thisfinding wassupportedbyMagneticResonanceImaging studiesthatshowedhyper-intensesignalsintheaxillaryregion.
Conclusions:These findings define the anatomiccharacteristics ofthe thoracic interfascial planenerveblockintheaxillaryregion,andunderlinetheclinicalpotentialofthisnovelnerve block.
©2016SociedadeBrasileiradeAnestesiologia.PublishedbyElsevierEditoraLtda.Thisisan openaccessarticleundertheCCBY-NC-NDlicense(
http://creativecommons.org/licenses/by-nc-nd/4.0/).
PALAVRAS-CHAVE
Anestesiapor conduc¸ão; Axila;
Músculosintercostais; Bloqueiodoplexo braquial;
Nervosintercostais; Excisãodelinfonodo; Ultrassonografia
Dispersãoaxilardeanestésicolocalapósbloqueiointerfascialtorácicoguiado porultrassom-estudoradiológicoeemcadáver
Resumo
Justificativa:Osanalgésicosoraisàbasedeopioidestêmsidousadosparaomanejodaanalgesia nosperíodosperiepós-operatóriodepacientessubmetidosàlinfadenectomiaaxilar.Aregião axilaréumazonadifícildebloquearenãoháregistrodeumatécnicadeanestesiaregional específicaqueoferec¸aoseubloqueioadequado.
Métodos: Apósa aprovac¸ão do Conselho deÉtica institucional, estudos anatômicose radi-ológicosforamrealizadosparadeterminaradeposic¸ãoedisseminac¸ãodeazuldemetilenoe anestésicolocal,respectivamenteinjetadosnaaxilaviaplanointerfascialtorácico.Examesde ressonânciamagnéticaforamentãorealizadosem15de34pacientesprogramadosparacirurgia demamaunilateralenvolvendoqualquerumdosseguintesprocedimentos:esvaziamento axi-lar,biópsiadelinfonodosentinela,biópsiadelinfonodoaxilar,oumamassupranumerárias,para verificaradeposic¸ãoetempodepropagac¸ãodasoluc¸ãodentrodoplanointerfascialtorácico
invivo.
Resultados: Estudosradiológicoseemcadáveresmostraramqueainjec¸ãodeanestésicolocale azuldemetilenoviaplanointerfascialtorácicousandoatécnicaguiadaporultrassomresultaem deposic¸ãoconfiávelnaaxila.Nospacientes,ainjec¸ãodeanestésicolocalproduziuumbloqueio sensitivoaxilarconfiável.Esseachadofoicorroboradoporestudosderessonânciamagnética quemostraramsinaishiperintensosnaregiãoaxilar.
Conclusões:Essesachadosdefinemascaracterísticasanatômicasdobloqueiodaregiãoaxilar edestacamopotencialclínicodessesnovosbloqueios.
©2016SociedadeBrasileiradeAnestesiologia.PublicadoporElsevierEditoraLtda.Este ´eum artigoOpen Accesssobumalicenc¸aCCBY-NC-ND(
http://creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
Patientswhoundergoaxillarysurgerysuffervariable post-operativediscomfortandpain.1Untiltoday,therehasbeen no ultrasound-guided regional anesthesia technique that providesadequate blockade of the axillary compartment. Thoracic paravertebral block (TPVB) is the main regional anesthetictechniqueusedinbreastsurgery,2,3 butit does not provide complete analgesia to the anterior and lat-eralchestwallduetoinnervationsfromthesupraclavicular nerves(C4---C5), thelateralpectoral nerve[LPn](C5---C6), medialpectoral nerve[MPn] (C8---T1) andmedial brachio-cutaneous nerve [MBCn] (C8---T1).4 The chronic pain that occursafteraxillarydissection(AD),oftenresultsfrom inad-equatetreatmentofacutepostoperativepain.5---7
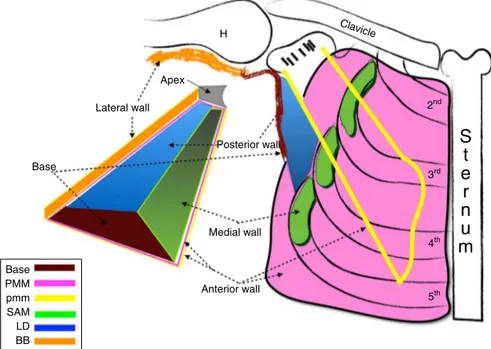
AsdescribedbyMooreandDalley,8theaxillahas4walls, 3ofwhicharemuscularFig.1.Thecutaneoussensory inner-vation of the axilla is supplied by the intercostobrachial nerves(ICBn)andmedialbrachio-cutaneousnerve(MBCn).
In the present report, we will discuss three thoracic interfascial ultrasound-guidedapproaches.9---13 These tech-niques have been recently described, with encouraging effects on blockade of the neural afferents of the chest wall, in spite of the few samples reported.8---11 However, thedetailedanatomiccharacteristicsandthespreadofLA intheseinterfascialultrasound-guidedblockshavenotyet been determined. We hypothesize that LA injection into theinterfascial planeof theantero-lateralchest wallwill produce enough spread into the axillary fascia, due the inter-fascialconnectionofthemuscles thatformthe axil-larywall.Thismayhelpinreducingacutepostoperativepain inpatientsundergoingaxillary dissectionandmaybecome an alternative to other techniques used to provide anal-gesia after breastsurgery. Weconsider theseinter-fascial blockseasytechniques:theyaresuperficialblocksandthe echo-anatomyissimpletounderstand.9---11,13---17
Apex
Lateral wall
Base
Base PMM pmm SAM LD BB
Posterior wall
Medial wall
Anterior wall
2nd H
3rd
4th
5th
S
t
e
r
n
u
m
Clavicle
Figure1 The boundariesoftheaxilla. PMM,Pectoralismajormuscle; pmm,pectoralisminormuscle; SAM,serratusanterior muscle;LD,latissimusdorsi;BB,bicepsbrachiimuscle;H,Humerus.
reconstructive breast cancer surgery or subpectoral prostheses.13
The Serratus-Intercostal Fascial Block (SIFB) anterior approach,15 involvesinjectingtheLAbetweentheSerratus Anterior muscle and the External Intercostalmuscle. The efficacyoftheSIFBtechniquehasbeenreportedbyfindings describedintwoobservationalstudiesinpatientunderno reconstructivebreastsurgery.11,15
We conducted a cadaveric dissection and radiological study, withthe goal of characterizing the SIFB injection, aswellasevaluatingthespreadoflocalanestheticagents injectedviathisinterfascialplane.
Methods
Thirty four consecutive patients, scheduled for axillary surgery, were recruited to take part in the radiological study, 33 females and 1 male. The age range was18---80 yearsofage.Institutionalreviewboardapprovalandwritten consents wereobtained beforeconducting the ultrasound thoracic interfascial blocks and MRI studies in 5 of 34 patients.ThetimeperiodwasSeptember2013throughMay 2014.
Theinclusioncriteriawere:patientsscheduledfor axil-laryclearance,sentinel node biopsy,axillary node biopsy, axillarysupernumerarybreastsormelanomaexcisions.
Exclusioncriteriaincludedpatientsunableorunwillingto cooperateinthisstudy,knownallergytoLAand/orto opi-oids,bleedingdisorders,onanticoagulants,significantliver orrenaldisease,diabetes,historyofdrugoralcoholabuse, painpatientsreceivingchronicanalgesicsorcorticosteroids. Intravenous(IV)accesswasestablished,routine monitor-ing (EKG,non-invasive blood pressure, oxygensaturation) was used. All patients were given midazolam 1---2mg IV before the block. The patients received a preoperative,
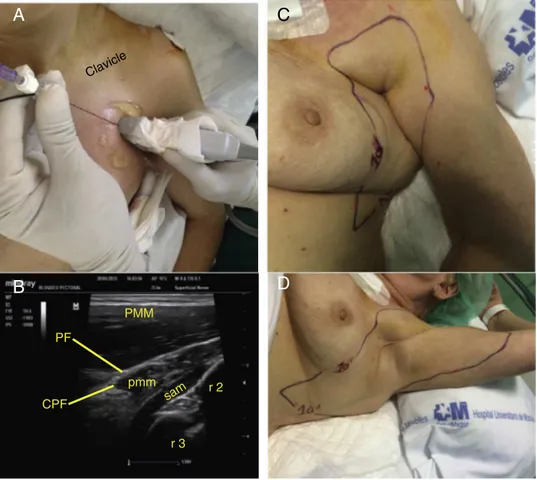
ipsilateralSIFB,anteriorapproachsingle-injectionreferred toasthethoracicinterfascialultrasoundblock(Fig.2).
The ultrasound blocks were performed in the Radiol-ogyDepartment, beforesurgery using a Locoplex (Vygon; Ecouen,France)blockneedle(17degree,25gauge,100mm) anda Mindray M7(Mindray Medical; Madrid,Spain) ultra-soundmachinewithahigh-frequencyprobe(6---13MHz).The totalamount of localanesthetic wasinjectedunder real-timeultrasoundvisualization.
Decreased temperature sensation in the T1---T3 der-matomes was determined as an indication of successful block of the axilla. An unbiased observer evaluated the extentofblockade.Thefineandgrosstouchwereevaluated byusingacottonwoolandpinprick,respectively.
Thepatientswerethentransferredtotheoperatingroom andgeneral anesthesiawas induced withtarget injection control(TCI) of Propofol and Remifentanyl(depending on thepatient’s age andphysical condition). Laryngeal mask airwaysappropriateforweightwereinserted.
Controlledventilationwasmaintainedaimingatan end-tidal CO2 pressure between 35---40mm/Hg. The patient’s
vitalsignsremainedwithin20%ofbaselinevalues through-outtheoperation.AnesthesiawasmaintainedwithPropofol andRemifentanyl TCIand an oxygen/air mixwitha frac-tion of inspired oxygen (FiO2) of 40%. Bispectral Index
valueswere maintainedbetween40and60. Remifentanyl 5---10mcg/kgbolusdosesweregivenwhenevermeanarterial bloodpressureorheartrateexceeded20%ofpreoperative baselinevalues.AllpatientsweretreatedwithOndansetron 4mgIV,30minbeforetheendoftheprocedure,toprevent PONV.
pmm
sam r 2
r 3 PMM
A
B
PF
CPF
Clavicle
D
C
Figure2 Ultrasound-GuidedAnterior-ApproachSIFPBlockpriortoundergoingtumorectomyintheouterquadrantandsentinel nodebiopsy.(A)Imageshowsprobeplacementandneedleinsertion.(B)Ultrasoundimageoftheanteriorthoracicwallshowsthe pectoralismajormuscle(PMM),pectoralisminormuscle(pmm),serratusanteriormuscle(SAM),clavipectoralfascia(CPF),pectoral fascia(PF)andtheribs(r).(C,D)Showstheareaofsensorylossintheanteriorlateralchestwall10minfollowingtheinjectionof localanestheticbetweentheSAMandexternalintercostalmuscle.
the patients were given IV Acetaminophen 1g and Keto-prophen25mgevery8h.Nausealastingmorethan10minor vomitingwastreatedwith4mgOndansetron.Morphine con-sumption,aswellasadministrationof antiemetic medica-tionandincidenceofadverseeffects(nausea,vomiting, pru-ritus,sedation,headache,andhypotension)wasrecorded.
Postoperativeanalgesiadatawascollectedusingavisual analogscale(VAS),aswellasduringpainfulrestricted move-ment of the shoulder, Fig. 3 classified into three grades (restricted,fair,andfree)every4hstartingfromthearrival ofthepatientatPACU,andlastingthroughoutthe24hstudy period.Initialpain assessment inthe PACUby visual ana-logscale(VAS;0=nopain,10=worstpainimaginable)was zero.Datawascollectedbyanunbiasedobserverwhowas nototherwiseinvolvedinthestudy.Patientsweremonitored throughouttheirhospitalstay forcomplicationsrelatedto SIFB(pneumothorax,externalmammaryarterylesion),and for signs of LA toxicity as well pain in the site of injec-tion.After24hofpost-operativeperiodandfreeofsurgical oranestheticcomplications, thepatientswere discharged home.PatientsweregivenoralAcetaminophen1gplus Keto-prophen25mgevery8h,andTramadol50mgevery4htouse athome.
Afterreceivingapprovalfromthelocalethicscommittee and written consent from the cadavers’ families,as part ofadonationprogramfromthe‘‘UniversidadAutonomade
30
25
20
15
Pacients (n)
10
5
0
2 1
0 3
Recovery 12 hours 24 hours Discharge
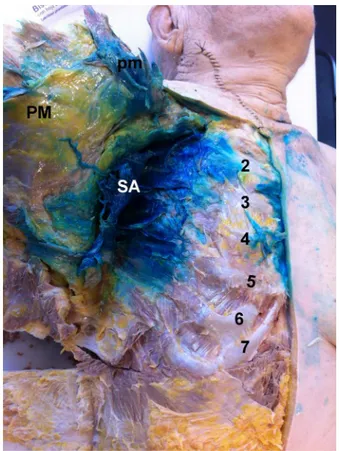
Figure4 Anatomicdissectionoftheanterolateralchestwall. Followinginjectionofmethyleneblue,thedyepenetratedinto theaxilla.(A)Injectionbetweentheserratusanteriormuscle (SA)andexternalintercostalmuscle(anterior-approachSIFP). Pectoralismajor muscle(PM),pectoralis minor muscle(pm), ordinalnumberscorrespondingtheconsecutivesribs.
Madrid’’, the nine cadaverswere embalmed according to classicaltechnique andweremaintainedat room temper-ature for 24h priorto theinjections anddissections. The cadaverswereplacedinthesupineposition,withthearm inabduction,toperformtheSIFBanterior-approach.Twenty mL of methylene blue (0.2% diluted in distillate water) wereinjected,usingablockneedle(17degree, 25gauge, 100mm) and ultrasound machine with a high-frequency probe.Thetotalamountofcontrastdyewasinjectedunder real-time ultrasound visualization. All needle placements weremadebythesameinvestigator,proficientand experi-encedinperformingthethoracicultrasound-guidedregional anesthesia.Assistancewasprovidedforinjectionofthe solu-tion.Theaxillaryspreadofthedye(macroscopicview)was evaluated,anddissectionwasperformedby2investigators, with experiencein cadaveric dissection, between 15 and 30minafterdyeinjection(Fig.4).
Anesthetic
regional
ultrasound-guided
techniques
Serratus-IntercostalFascialUltrasound-Guided Block(SIFB),anteriorapproach
With thepatient in the supine position,a linear probeis positionedbelowtheexternalthirdoftheclavicle(Fig.2)
toidentify, in the surface plane, the pectoralis muscles, thetoracho-achromialarteryandthecephalicveinthatlie between them. In the deepplane, the SAM is identified, restingontheribs.Theneedleisthenintroducedin-plane frommedialto lateral,and itstip is placedbetween the SAM and the External Intercostal muscle at level of sec-ondrib.TwentymLofLevobupivacaine0.25%+Epinephrine 1:200,000wereinjectedunderdirectultrasound visualiza-tioninrealtime,fragmentingthetotalvolume,aspirating every 3mL to reduce the risk of intravascular injection andminimizing the patient discomfortonhydrodissection (Fig.2A).
Study1:determinationofinjectatespreadduring SIFBusingMRI
Theaimofthisstudywastodeterminetheaxillaryspread of the injectate within the SIFB anterior approach. Our image study consisted of a MRI done immediately after LAinjection. Ourradiologist usedMRI sequences toshow T2---weighed,fat-suppressedimages,makingaxialand coro-nalthoracicsectionsfromthesupraclavicularregionstothe inframammarycrease. The same radiologist, proficient in thoracic MRI, analyzed the imagesand issueda report of thespreadof theLAinjectate intheinterfascial thoracic planes(Fig.5AandB).
Study2:ValidationofUltrasound-GuidedSIFBina cadavermodel
The aim of this study was to validate the described ultrasound-guided regional technique, by demonstrating thattheyresulted inthedepositionofdye withinthe lat-eral thoracic interfascial planes reaching the axilla. An ultrasound-guidedSIFBanteriorapproachwasperformedon nineembalmedcadavers(Fig.4).
Results
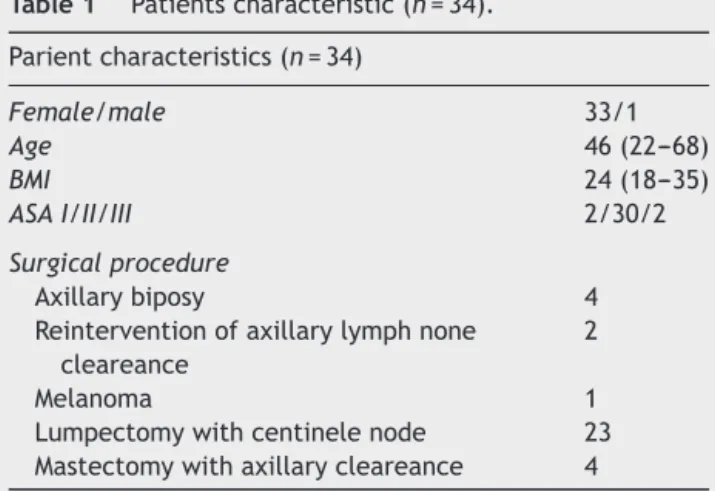
PatientdataandthetypeofsurgeryareshowedinTable1. WedemonstratethatLAreachestheaxillaifinjectedinto theinterfascial planes of the medial axillary wall. In our opinion, the radiological findings support the correlation between MRI images and territories blocked. Thirty two patientsoftheSIFBgroupsreportedaVAS=0atrest.Pain witharm abduction was alsovery low during hospitaliza-tion(Fig.3).Nopatientfromthisgroupsneeded arescue RemifentanylbolusintheintraoperativeperiodorMorphine inPACU.32/34patientsclassifiedtheanesthesiatechnique usedasexcellentand2/34asgood.
Study1:ValidationofUltrasound-GuidedSIFB techniquesusingMRI
Figure5 (A)MRIT2---weighedfat-substractionsequence:axialandsagittalsectionsthroughthechestwallimmediatelyafter injectionoflocalanesthetic. (A,B)Axialandsagittal viewsshowspreadofthelocalanesthetic betweentheanteriorserratus muscleandexternalintercostalmuscleafterananterior-approachSIFP.(C)Diagramshowsdottedlineneedledirectionandlocal anestheticspread(purple).(D)Sagitalviewofthechestwall(T3)showthelocalanestheticbetweenserratusanteriormuscle(SAM) andexternalintercostalmuscle(EIM),subclaviammuscle(SCM),pectoralfascia(PF),thoracicexternalfascia(ETF),pectoralminor muscle(pmm),arteria,veinandintercostalnerve(A,V,N).
Table1 Patientscharacteristic(n=34). Parientcharacteristics(n=34)
Female/male 33/1
Age 46(22---68)
BMI 24(18---35)
ASAI/II/III 2/30/2
Surgicalprocedure
Axillarybiposy 4
Reinterventionofaxillarylymphnone cleareance
2
Melanoma 1
Lumpectomywithcentinelenode 23 Mastectomywithaxillarycleareance 4
Dataarepresentasabsolutenumberormedianswith25thto 75thinterquartilerangeASAindicatesAmericanSocietyof Anes-thesiologist.BMI,bodymassindex.
covering the intercostobrachialnerve territories, and the MedialBrachio-Cutaneousnerve(MBCn)in34/34patients.
InpatientswhoreceivedtheSIFB-anteriorapproach,the LAspread intothe interfascial plane of the lateral chest wallreachingtheaxilla.Thepatientsweremonitoredduring theperformanceofthesebocksandfor24hafterforsigns of local anesthetic toxicity. We used Eco-Doppler images in real time toavoid intravascular injection. There were
norecognizedsymptomsandsignsofthiscomplicationon anypatient.WedidnotobserveLongThoracicnerve(LTn) palsyin anyofthe patients.Brachialplexus motordeficit wasnot seen in any patient. The MBCnand the Intercos-tobrachial nerve territories were blocked in all patients, reaching the upper third of the medial arm. All patients referreddiscomfortafterneedletobonecontactandwhen theLAhydrodissectionstarted.
Study2:ValidationofUltrasound-GuidedSIFB techniquesinacadaver
Anatomic dissection of the 9 embalmed cadavers (as describedabove)showedthespreadofdyeintotheserratus intercostalfascialplane,reachingtheaxilla(Fig.4).
IntheSIFB anteriorapproach, the methylenebluewas found intothe axillain allcadavers. The ICBn,MCBnand theintercostalterritoriesfromT1toT3werestained.We also observed thecontrast reachingthe posterior axillary line.
Discussion
wall. Our findings show that the SIFB anterior approach injections providea potentialspaceinto whichLAcan be deposited to achieve sensory blockade of the IBCn and MBCn.Thesestudiesalsoindicatethatitispossibletoinject LAintotheSIFPinvivousingultrasound-guidedtechniques. Thesefindingsshowthatthemedialchestwalloffersaneasy meanstoreachtheaxillaryregionduethecommunication orpermeabilityofthethoracicinterfascialplanes.
The axillary compartmentisa difficultregiontoblock. Despite the thoracic para-vertebral block (TPVB) being the gold standard technique for breast surgery, we have been using these new interfascial thoracic ultrasound-guideblocks.Wedescribedheretoachieveanalgesiaafter breast andaxillary surgery withgood results.9,11,15---17 Pre-incisional LA infiltration reduces pain during the initial hoursafterbreastandaxillaoperations,andthereforethis has become a standard procedure in our unit.5,6 Camp-bell et al. in their study concluded the LA infiltration during breastsurgery hasa marked opioidsparing effect, with significant patient benefits, reducing nursing work-loadand drugcosts.19 Sidiropoulouetal.20 intheir study, evaluated the analgesic efficacy and morphine consump-tion of the twotechniques after mastectomy, concluding thatthecontinuouswound infiltrationoflocalanesthetics isaneffectivealternative toparavertebralanalgesiaafter mastectomy with axillary dissection. These new thoracic ultrasound guide interfascial blocks may have some simi-lar aspects to local wound infiltration, but they use less LA,and acathetercan alsobeplaced beforethe surgery without causing interference with the surgical field and thusreducingpostoperativepainforanextendedperiodof time.16
Oral opioid analgesics have traditionally been used to provide peri-and postoperativeanalgesia inpatients who undergoaxillary dissection.Previousstudiesevaluatedthe effects of peri- and postoperative administration of LA. TheresultsobtainedbyRawlani21 inhisdouble-blind, ran-domized, prospective study, supports the efficacy of a postoperativelocalanestheticpainpumpinreducingpain, narcotic use, and postoperative nausea and vomiting in womenundergoingbreastreduction.Scott22comparedthe efficacy of continuous axillary administration of bupiva-caine versus standard surgical treatment or placebo in patients undergoing axillary lymph node dissection. The patientstreatedwithacontinuousinfusionof bupivacaine experiencedsignificantlylowerpainscores.The postopera-tive opioid analgesic requirements also were significantly decreased in the bupivacaine group. The use of continu-ousadministrationofbupivicaineafteraxillarylymphnode dissectionsignificantlydecreasespainandopioidanalgesic requirements, withconcomitant decreases in nausea and sedation.This studyprovidesencouragingevidenceof the therapeutic benefits of continuous infusion of local anes-thesia and may represent a valuable adjunct for surgical patientswhorequireaxillarylymphnodedissection(ALND), includingthosewithbreastcancerandmelanoma.Strazisar5 observed that wound infusion in the LA group (vs. the standardopioid-basedanalgesiagroup)resultedinagreater reduction of acutepain and enabled reducedopioid con-sumption; they also noted a trend toward reduction of chronic pain in the LA group. Fajardo et al.16 published theinterpectoralfasciainfusionofLevobupivacaine0.125%
(5mL.h−1) in patients undergoing mastectomy and
axil-lary clearance and found good analgesia and less opioid consumption. Diéguez et al.11 in January 2013, published (article in Spanish) the LA infiltration onthe mid-axillary lineina patientfor breastsurgery.Diéguez11 inherstudy demonstrated the effectiveness of the ultrasound-guided injectionofLAbetweenserratusanteriormuscle(SAM)and externalintercostalmuscle (EIM) namedBRILMA (in Span-ish:intercostalbranchnervesinthemidaxillarylineblock) inanobservationalstudyin30patientsscheduledfor non-reconstructivebreastandaxilladissection.Diéguez11found thatinjecting 15mLLevobupivacaine 0.25% (3mL in each intercostal space) provides adequate intraoperative and postoperatoryanalgesia.Blancoetal.,in201323performed theSerratusblockat2differentlevelsinfourhealthy volun-teers’.ThefirstwassuperficialtotheSAM,similartoPec’s blockII,11 techniquepublishedin2012.Thisapproachaims toblockatleastthepectoralnerves,theintercostobrachial andtheintercostalsbranches.
On September 2012, Fajardo published a descriptive, observational study in 44 women scheduled for breast surgery,15 onwhich hecombined the block of the lateral andanteriorcutaneousbranchesoftheintercostalnerves. The objective of this study was to evaluate extension of LA through MRI, after the ultrasound-guided injection of LA between SAM and EIM. It was observed that, in most patients,theLAspreadtotheaxilaandunderthelateraland posteriorchestwall,betweenT2andT7dermatomes,result comparablewithBlancoetal.23WebelievethatLAinjection betweentheSAMandEIMismoreadvantageousthan injec-tionssuperficialtotheSAMbecauseitmayavoidtransitory palsyoftheLTNandlikelyachievemoredistaldermatomal spread.TheLAinjectionbetweenthePectoralMinorMuscle (pmm)andSAM(Pec’sblockII) hasagoodspreadtoo,but thespreadbeyondT3is erraticbecausetheaxillary fatty tissuemaylimittheLAspread.Inourclinicalpractice,we abandonedthisblockinbreastsurgerybecausethepatients referredpainallevelofthenipple-aereolacomplex.
ThePec’sIIblock12 achievessuitableaxillary dissemina-tion.Nevertheless,wedidnotevaluatethistechniquedue toitbeingamorecomplextechniquetoperformthanSIFB despiteagreateraxillaryspread.Thefascialspacebetween the pectoralisminor and serratus anteriormuscles is not alwayseasytofind,especiallyintheelderlypatients. Con-trarytothePec’sblockII,weintentionallyinjectedtheLA belowtheSAMfortworeasons:toachievegreaterspread withintheserratus-intercostalplaneandthus blockingthe secondand thirdintercostal nerves(ICBn),while avoiding thepossibilityof transitorypalsyofthe LTN,leadingtoa wingedscapulathancanbemistakenwithasurgicallesion ofthisnerve.
The serratusinterfascial plane(SIFP)is a small,poorly distensibleneurovascularspacebetween theSAMand EIM containing the perforating lateral intercostal cutaneous branchesoftheintercostalnerves.
TheSIFP’spoordistensibility,alongwiththerespiratory movements,allowstheLAtobeextensivelydispersedwithin thisplane.
SAMhasseveralanatomicalrelationship inthechestwall, thesamewaythetransversusabdominismuscleinthe lat-eralabdominalwall,keepsananatomicalrelationshipwith theinternalobliquemuscle.TheSAM,inthelateralchest wall, attaches to the ribs and gets in contact with the EIM,beingcoveredbythePMM,pmmandlatissimusdorsi, and later gets enmeshed with the external oblique mus-cleintheantero-inferiorthoracicwall.Thereforethename ‘‘serratusanteriorplane’’wouldbeincorrect,sinceitdoes notdescribethespecificinterfascialplanewherethelocal anestheticgetsdeposited.
Wahba25 evaluated the thoracic paravertebral block (TPVB)versus pectoral nerveblock in regardtomorphine consumption andanalgesic efficacy after modified radical mastectomy.
Itwasconcludedthat24hmorphineconsumptionwas sig-nificantlylowerinPec’sblockgroup,andlowerpainscores inthefirst12hincomparisonwithTPVBaftermastectomy. Thisresultarecontradictory,notcorrespondingwithother publishedresults.2,18,26Basedonthecurrentevidence nowa-days,the TPVB is the gold standard technique for breast surgery,despitetheencouragingresultsofthesenew inter-fascialthoracicblock.2,18Basedonourexperience,thePec’s IIblockdoesnotprovideadequateanalgesiaformastectomy andtheLAhardlyreachesbeyondthelevel ofT3---T4.We believethatPec’s IIblock isa goodtechniquefor axillary surgery,notformastectomy.
The SIPB lateral approachwasrecently evaluatedasa method to achieve analgesia after breast surgery, breast brachitherapy, chest drain tube.9,11,15,17,24 To improvethis techniqueweusealong needletoadvanceit throughthe SIFPwiththelateralapproachandutilizehydrodissection, toplacetheLAasdistalaspossible.Theribsareimportant ultrasoundlandmarkstoavoidpleuralorlungpuncture.The useofsedationanalgesiarelievespatientdiscomfortduethe SAMpuncture,ribsperiosteumcontactandhydrodissection oftheinterfascialplane.ToperformSIFB-lateralapproach, wepreferplacingthepatientinthelateraldecubitus posi-tionorplaceapillowunderthechestbecausethesofttissue willdropdownandthedistancebetweentheskin andthe ribsisshortened.Also,restingthehandholdingtheprobeon thelateralchestwallwillmakethetechniquemorestable. To improve these blocks, now we use fine and sharp needlesfor‘‘singleshots’’andTuohyneedlestoplace con-tinuouscatheters.
This thoracic interfascial ultrasound block is a simple technique and relatively quick toperform since they are superficialandsonographicallyeasytounderstand,andthey have a reproducible sonoanatomy in the vast majority of patients,andmaybeperformedinpatients undergeneral anesthesia.Althoughthesenovelblocksaretechniques per-formedusuallybyanesthesiologists,nurseanesthetistswith traininginregionalblockandsurgeonswouldfeel comfort-abletoperformsuchblocks.
They may also provide additional options when cir-cumstances are unfavorable to perform a TPVB (such as coagulopathy,intoleranceofsympathectomyorinabilityto positionapatientproperly). Inaddition,thesecanbe tar-geted to unilateral or segmental surgery and can cover severaldermatomesandtheaxillawithoneinjection.They may also very easily be performed as continuous periph-eralnerveblockswithcatheters,whenextendedanalgesia
isrequired.Inourexperienceandfromdiscussionswithour surgeons,theseblocksdonotinterferewiththesurgicalfield becausetheLAisplacedbetweeninterfascialplanes.These blocksmayopen newdoorstoinvestigationregarding the recurrence of breastcancer and the incidence of chronic painafterbreastsurgery.27 Today,wedonothaveenough clinicaldatatocomparethesetechniqueswithother tech-niquesusedinpatientsundergoingbreastsurgery.
We consider that these new blocksmay have the fol-lowing indications,according toourexperience:thePec’s Iblockmaybeusedinsubpectoralprosthesissurgerywith orwithoutaxillaryapproach,aswellasforaxillarysurgery, remembering that it is also necessary to block the inter-costalnerves,hencethisblockshouldnotbeusedastheonly anesthetic technique. The SIFB anterior approach can be usedfornon-reconstructivebreastsurgeryandin combina-tionwithPec’sIblockinpatientsundergoingreconstructive surgery,andfor subpectoralprosthesistoblockthelateral intercostalbranchesandthepectoralnerves.TheSIFB lat-eralapproachcanbeusedformastectomy,lumpectomyas wellaxillaryclearance,andmaybeanalternativefor latis-simus dorsi flaps. The LAplaced in thisplane willdiffuse throughtheintercostalmuscles,thusblockingtheanterior andlateralintercostalbranches,producingsensorylossof the whole breast and diffusing anteriorly and posteriorly undertheribcage,reachingtheposterioraxillaryline.
Eventhoughourresultsareencouraging,wedeemedit unnecessarytosubmitalargenumberofpatientstoan inva-sive investigation, for a smallsample could bear out our theory.This studymightopenanewdoortotheanalgesia oftheaxilla.Wealsodidnotexploretheminimumamount of LArequiredtoblock theintercostalnerves thatsupply thebreastandaxilla.Despiteusingembalmedcadavers,the samelevelofadequatespreadwasdemonstrated‘‘invivo’’ byusingMRI.Thisisadescriptivestudy,furtherinvestigation iswarranted.
Conclusions
This study represents, in our opinion, the first detailed depiction of the anatomic characteristics of interfascial thoracicblockstoachievesensoryblockoftheaxilla (Inter-pectoralFasciaPlane(IPFP)andSIFBblocks).
Thesenovel techniques maybecome widelyused anal-gesic alternatives in axilla surgery given their low rate of complications and the characteristic single-puncture technique that allows simultaneous blockade of numer-ous dermatomes. Additional benefits of these techniques include applicability to the outpatient setting and to patients who have undergone a neuraxial block, may be safelypracticedinapatientundergeneralanesthesia,and thetimeconsumedtoblock,5---10min,doesnotaffect sur-gicaltime.
whoreceivedanerveblock,neededlesspost-operativepain relief from opioid drugs. We are waiting for a result of the observational studiesand randomizedcontrolled clin-icaltrials,thatareneededtoconfirmwhetherthethoracic interfascial block techniques are appropriate for routine clinical practice, and to determine the minimum amount of LA34 required for blockade as well as the serum local anestheticconcentrations.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
Acknowledgments
Theauthorswanttoexpresstheirgratitudetothefamilies whoparticipated in the cadaver donation program of the ‘‘UniversidadAutonomadeMadrid’’.Wewouldliketothank theDepartmentofAnatomyofthe‘‘UniversidadAutonoma de Madrid’’, especiallyDr. FranciscoClascá Cabré, Profe-sor ofAnatomy and HumanEmbriology, andAndrés Olaya Céspedes,AnatomyTechnician,fortheircontinuedsupport. WealsothankDr.TomislavStanic,Dr.LuisValdes,Dr.Carlos Salazarforhishelpinthereviewofthismanuscript.
References
1.CortenE,SchellekensP,HageJ,etal.Clinicaloutcomeafter pedicledsegmentalpectoralismajorislandflapsforheadand neckreconstruction.AnnPlastSurg.2009;63:292---6.
2.SchnabelA, Reichl SU, Kranke P, et al. Efficacy and safety of paravertebral blocks in breast surgery: a meta-analysis of randomized controlled trials. Br J Anaesth. 2010;105: 842---52.
3.Arsalani-ZadehR, ElFadl D, YassinN, et al. Evidence-based review of enhancing postoperative recovery after breast surgery.BrJSurg.2011;98:181---96.
4.Stecco A, Masiero S, Macchi V, et al. The pectoral fas-cia: anatomical and histological study. J Bodyw Mov Ther. 2009;13:255---61.
5.StrazisarB,BesicN.Comparisonofcontinuouslocalanaesthetic andsystemicpaintreatmentafteraxillarylymphadenectomyin breastcarcinomapatients---aprospectiverandomizedstudy. RadiolOncol.2013;47:145---53.
6.Strazisar B, Besic N, Ahcan U. Does a continuous local anaestheticpain treatmentafterimmediatetissue expander reconstructionin breastcarcinoma patients moreefficiently reduceacute postoperativepain ---aprospective randomised study.WorldJSurgOncol.2014;12:16.
7.DeOliveiraGSJr,ChangR,KhanSA,etal.Factorsassociated withthedevelopmentofchronicpainaftersurgeryforbreast cancer:aprospectivecohortfromatertiarycenterintheUnited States.BreastJ.2014;20:9---14.
8.KeithLM,AgurAMR,ArthurFD.Clinicallyorientedanatomy.In: MemBA,editor.Clinicallyorientedanatomy.5thed.Maryland CompositionCompany,Inc;2006.p.724---64.
9.FajardoM,LópezS,DiéguezP,etal.Abordajeecoguiadodelas ramascutáneasdelosnerviosintercostalesaniveldelalínea mediaaxilarparacirugíanoreconstructivademama.CirMay Amb.2013;18:3---6.
10.PerezMF,MiguelJG,delaTorreP.Anewapproachtopectoralis block.Anaesthesia.2013;68:430.
11.García P, Fajardo M, Álvarez S, et al. Ultrasound-assisted approachtoblockingtheintercostalnervesinthemid-axillary linefornon-reconstructivebreastand axillasurgery.RevEsp AnestesiolReanim.2013;60:365---70.
12.Blanco R,FajardoM,Maldonado T.Ultrasounddescriptionof PecsII(modifiedPecsI):anovelapproachto breastsurgery. RevEspAnestesiolReanim.2012;59:470---5.
13.BlancoR,GarcíaM,GarcíaP,etal.Eficaciaanalgésicadel blo-queo delosnervios pectoralesen cirugíade mama.CirMay Amb.2011;16:89---93.
14.Blanco R. The ‘pecs block’: a noveltechnique for providing analgesiaafterbreastsurgery.Anaesthesia.2011;66:847---8.
15.Fajardo M, Garcia FJ, López Alvarez S, et al. Bloqueo de las ramas cutáneas laterales y anteriores de los nervios intercostales para analgesia de mama. Cir May Amb. 2012;17:91---104.
16.FajardoM,CuchiC,PaniaguaMA,etal.Bloqueocontinuode los nervios pectorales para cirugía de mama. Cir May Amb. 2011;16:191---2.
17.López-MatamalaB,FajardoM,Estébanez-MontielaB,etal.A newthoracicinterfascialplaneblockasanesthesia fordifficult weaningduetoribcagepainincriticallyillpatients.Med Inten-siva.2013:26.
18.Andreae MH, Andreae DA. Local anaesthetics and regional anaesthesiaforpreventingchronicpainaftersurgery.Cochrane DatabaseSystRev.2012;10:CD007105.
19.CampbellI,CavanaghS,CreightonJ,etal.Toinfiltrateornot? Acuteeffectsoflocalanaestheticinbreastsurgery.ANZJSurg. 2014.
20.SidiropoulouT,BuonomoO,FabbiE,etal.Aprospective com-parisonofcontinuouswoundinfiltrationwithropivacaineversus single-injectionparavertebralblockaftermodifiedradical mas-tectomy.AnesthAnalg.2008;106:997---1001[tableofcontents].
21.Rawlani V, KrygerZB, Lu L, et al. A localanesthetic pump reducespostoperativepainandnarcoticandantiemeticusein breastreconstructionsurgery: arandomizedcontrolledtrial. PlastReconstSurg.2008;122:39---52.
22.ScottSR.Patient outcomesafteraxillarylymphnode dissec-tionfor breastcancer:useofpostoperativecontinuouslocal anesthesiainfusion.JSurgRes.2006;134:124---32.
23.BlancoR,ParrasT,McDonnellJG,etal.Serratusplaneblock:a novelultrasound-guidedthoracicwallnerveblock.Anaesthesia. 2013;68:1107---13.
24.delaTorrePA,GarciaPD,AlvarezSL,etal.Anovel ultrasound-guidedblock:apromisingalternativeforbreastanalgesia.Aesth SurgJAmSocAesthPlastSurg.2014;34:198---200.
25.WahbaSS,KamalSM.Thoracicparavertebralblockversus pec-toralnerve blockfor analgesiaafterbreast surgery.EgyptJ Anaesth.2014;30:129---35.
26.ThavaneswaranP,RudkinGE,CooterRD,etal.Briefreports: paravertebralblockforanesthesia:asystematicreview.Anesth Analg.2010;110:1740---4.
27.Chang YC, Liu CL, Chen MJ, et al. Local anesthetics induceapoptosisinhumanbreasttumorcells.AnesthAnalg. 2014;118:116---24.
28.ChiuM,BrysonGL,LuiA, et al.Reducingpersistent postop-erativepainanddisability1yearafterbreastcancersurgery: arandomized,controlledtrialcomparingthoracic paraverte-bral block to local anesthetic infiltration. Ann Surg Oncol. 2014;21:795---801.
29.WijayasingheN,Andersen KG,Kehlet H.Neural blockadefor persistent pain afterbreastcancer surgery.Reg Anesth Pain Med.2014;39:272---8.
30.Cho AR, Kwon JY, Kim KH, et al. The effects of anesthet-icsonchronicpainafterbreastcancersurgery.AnesthAnalg. 2013;116:685---93.
by ketamine, thiopental,and halothane, but not by propo-fol:mediatingmechanismsandprophylacticmeasures.Anesth Analg.2003:1331---9.
32.HeaneyA,BuggyDJ.Cananaestheticandanalgesictechniques affectcancerrecurrenceormetastasis?BrJAnaesth.2012;109 Suppl.1:i17---28.
33.ExadaktylosAK,BuggyDJ, MoriartyDC,etal.Cananesthetic techniqueforprimarybreastcancersurgeryaffectrecurrence ormetastasis?Anesthesiology.2006;105:660---4.