www.bjorl.org
Brazilian
Journal
of
OTORHINOLARYNGOLOGY
ORIGINAL
ARTICLE
Orofacial-cervical
alterations
in
individuals
with
upper
airway
resistance
syndrome
夽
Pedro
Wey
Barbosa
de
Oliveira
a,
Luciano
Lobato
Gregorio
a,∗,
Rogério
Santos
Silva
b,
Lia
Rita
Azevedo
Bittencourt
c,
Sergio
Tufik
d,e,
Luis
Carlos
Gregório
aaDepartmentofOtorhinolaryngologyandHeadandNeckSurgery,EscolaPaulistadeMedicina,UniversidadeFederaldeSãoPaulo
(UNIFESP),SãoPaulo,SP,Brazil
bPost-graduateProgram,DepartmentofPneumology,FaculdadedeMedicina,UniversidadedeSãoPaulo(FM-USP),SãoPaulo,SP,
Brazil
cCentrodeEstudosdoInstitutodoSono,SãoPaulo,SP,Brazil
dEscolaPaulistadeMedicina,UniversidadeFederaldeSãoPaulo(UNIFESP),SãoPaulo,SP,Brazil
eDepartmentofPsychobiology,EscolaPaulistadeMedicina,UniversidadeFederaldeSãoPaulo(UNIFESP),SãoPaulo,SP,Brazil
Received28March2015;accepted29May2015 Availableonline6November2015
KEYWORDS
Sleepdisorders; Airwayresistance; Nasalobstruction
Abstract
Introduction:Studiesthatassesstheupperairwaysinsleep-relatedbreathingdisordershave been performed onlyinpatients with obstructive sleepapnea syndrome whoseek medical attention.Therefore,inadditiontotheneedforpopulationstudies,therearenodataonthe orofacial-cervicalphysicalexaminationinsubjectswithupperairwayresistancesyndrome. Objectives: Tocomparetheorofacial-cervicalexaminationbetweenvolunteerswithupper air-wayresistancesyndromeandwithoutsleep-relatedbreathingdisorders.
Methods:Through questionnaires, physical measurements, polysomnography, and otorhino-laryngological evaluation, thisstudy compared the orofacial-cervical physical examination, throughasystematicanalysisofthefacialskeleton,mouth,throat,andnose, between vol-unteerswithupperairwayresistancesyndromeandvolunteerswithoutsleep-relatedbreathing disordersinarepresentativesampleoftheadultpopulationofthecityofSãoPaulo.
Results:There were 1042 volunteers evaluated; 49 subjects (5%) were excluded as they didnot undergootorhinolaryngologicalevaluation, 381(36%) hadapnea---hypopneaindex>5 events/hour,and131(13%)hadoxyhemoglobinsaturation<90%.Amongtheremaining481 sub-jects(46%),30(3%)metthecriteriafortheupperairwayresistancesyndromedefinitionand 53(5%)metthecontrolgroupcriteria.Attheclinicalevaluationofnasalsymptoms,theupper
夽 Pleasecitethisarticleas:deOliveiraPWB,GregorioLL,SilvaRS,BittencourtLRA,TufikS,GregórioLC.Orofacial-cervicalalterationsin
individualswithupperairwayresistancesyndrome.BrazJOtorhinolaryngol.2016;82:377---84. ∗Correspondingauthor.
E-mail:gregorioluciano@me.com(L.L.Gregorio).
http://dx.doi.org/10.1016/j.bjorl.2015.05.015
airwayresistancesyndromegrouphadmoreoropharyngealdryness(17%vs.29.6%;p=0.025) andseptaldeviationgrades1---3 (49.1%vs.57.7%;p=0.025) whencompared tocontrols. In thelogisticregressionmodel,itwasfoundthatindividualsfromtheupperairwayresistance syndromegrouphad15.6-foldhigherchanceofhavingnosealterations,11.2-foldhigherchance ofbeinghypertensive,and7.6-foldhigherchanceofcomplainingoforopharyngealdrynesswhen comparedtothecontrolgroup.
Conclusion:Systematicevaluationofthefacialskeleton,mouth,throat,andnose,between vol-unteerswithupperairwayresistancesyndromeandvolunteerswithoutsleep-relatedbreathing disorders, showed thatthepresence ofupper airwayresistancesyndromeismainly associ-atedwithnasalalterationsandoropharyngealdryness,inadditiontotheriskofhypertension, regardlessofgenderandobesity.
© 2015 Associac¸˜ao Brasileira de Otorrinolaringologia e Cirurgia C´ervico-Facial. Published by Elsevier Editora Ltda. This is an open access article under the CC BY license (http:// creativecommons.org/licenses/by/4.0/).
PALAVRAS-CHAVE
Transtornosdosono; Resistênciasdasvias respiratórias; Obstruc¸ãonasal
Alterac¸ãocérvico-orofacialemindivíduoscomsíndromedaresistênciadeviaaérea
superior
Resumo
Introduc¸ão:Estudosqueavaliamaviaaéreasuperior(VAS)nosdistúrbiosrespiratórios rela-cionados ao sono(DRRS) foram realizadas somente em pacientes comSíndrome da apneia obstrutivadosono(SAOS)queprocuramoatendimentomédico.Portanto,alémdanecessidade deestudospopulacionais,nãohádadossobreoexamefísicocérvico-orofacialemindivíduos comSíndromedeResistênciadasViasAéreasSuperiores(SRVAS).
Objetivos: CompararoexamecérvicoorofacialentrevoluntáriocomSRVASesemDRRS. Método: Através de questionários, medidas físicas, polissonografia e avaliac¸ão otorrino-laringológicacomparou-seoexamefísicocérvicoorofacial,atravésdeumaanálisesistemática doesqueletofacial,boca,faringeenariz,entrevoluntárioscomSRVASevoluntáriossemDRRS emumaamostrarepresentativadapopulac¸ãoadultadacidadedeSãoPaulo.
Resultados: Avaliamos1042voluntários.Foramexcluídos:49indivíduos(5%)quenãorealizaram avaliac¸ãootorrinolaringológica;381(36%)apresentaramíndicedeapneiaehipopnéia(IAH)>5 eventos/horae131(13%)apresentaramsaturac¸ãodaoxihemoglobina<90%.Entreos481 volun-táriosrestantes(46%),30(3%)preenchiamoscritériosestabelecidosparaadefinic¸ãodeSRVASe 53(5%)quepreenchiamoscritériosdogrupocontrole.Naavaliac¸ãoclínicadossintomasnasais, ogrupo SRVASapresentou maisressecamento orofaríngeo(17%vs.29,6%;p=0,025),desvio septalgrau1a3(49,1%vs.57,7%;p=0,025),comparadoaocontrole.Nomodeloderegressão logísticaobservamosqueindivíduosdogrupoSRVASapresentaramumarazãodechance15,6 vezesmaiordeapresentaremnarizalterado;11,2vezesmaiordeseremhipertensose7,6vezes maiordesequeixaremderessecamentoorofaríngeoquandocomparadosaogrupocontrole. Conclusão:Aavaliac¸ãosistemáticadoesqueletofacial,boca,faringeenariz,entrevoluntários comSRVAS evoluntários semDRRS, mostrou que apresenc¸a de SRVASestá principalmente associadaàalterac¸õesnasaiseressecamentoorofaríngeo,alémdoriscodehipertensãoarterial, independentementedogêneroeobesidade.
© 2015 Associac¸˜ao Brasileira de Otorrinolaringologia e Cirurgia C´ervico-Facial. Publicado por Elsevier Editora Ltda. Este ´e um artigo Open Access sob uma licenc¸a CC BY (http:// creativecommons.org/licenses/by/4.0/).
Introduction
Upperairwayresistancesyndrome(UARS)wasfirstdescribed in1982inchildrenandadultsas‘‘excessivedaytime sleepi-ness.’’ At that time, such individuals were classified as having‘‘idiopathichypersomnia.’’1---3 It wasobservedthat anumberofpatientshadpolysomnographiccharacteristics in common, usually ignored in the sleep analysis at that time:progressiveincreaseinrespiratoryeffort(represented
Patientswithobstructivesleepapnea syndrome(OSAS) have a high degree of collapsibility of the UA. Among several theories, it is believed that the entity may be explained by the dysfunction of the afferent receptors in pharynx.4 This dysfunction is not found in patients with UARS.5 Some authors have suggested that patients withUARS havesmall breathingdifficulties,such asnasal valve collapse, inferior turbinate hypertrophy, and septal deviations.6,7Moreover,ithasbeenshownthatchangingthe sizeof the UAduringa respiratoryevent inpatients with UARSproducesa betterandfasterresponse,comparedto patients with OSAS.8 Such response may be a reflex that leads to a subcortical activation, and is depicted in the electroencephalogram.
Patients with OSAS and UARS have similar complaints, suchasfatigueanddaytimesleepiness.However,patients withUARS do notmeet the diagnostic criteriafor OSAS,1 astheydonothaveasignificantnumberofapneasand/or hypopneas (AHI<5) associated withoxyhemoglobin desat-uration. These patients have, during sleep, a high and increasingresistancetoairflowduringinhalation.This resis-tance is not enough to cause a significant change in the airflowasinOSAS,butitisenoughtocauserecurrentbrief arousalsthatfragmentsleep,leadingtofatigueanddaytime sleepiness. Despite the syndrome overlap, thereare very importantdifferencesrelatedtothefrequencyofinsomnia, wakingperiodsduringthenight,anddifficultyfallingasleep orreturningtosleep,commoncomplaintsinpatientswith UARS.9
MoststudiesassessingtheUAinsleep-relatedbreathing disorders(SRBD)areperformedinpatients withOSASin a clinical population. Thereareno reportsin the literature on the orofacial-cervical physical assessment in subjects with UARS. The objective of this study was to compare theorofacial-cervicalphysicalassessmentthrougha system-aticevaluationofthefacialskeleton,mouth,pharynx,and nose,betweenvolunteerswithUARSandvolunteerswithout SRBDin apopulation sample representative ofthe cityof SãoPaulo,inordertoidentifypredictivecharacteristicsof UARS.
Methods
Atotal of1042 randomlyselected subjectswereincluded torepresenttheadult populationof thecity ofSãoPaulo according to gender, age (20---80 years), and socioeco-nomic status. This sampling was based on the updated dataofthepopulation,accordingtoestimatesofFundac¸ão SEADE, based on the 2000 census. The protocol was part of the larger project carried out in 2007, and was approved by the research ethics committee of the uni-versity (CEP 0591/09) and registered at ClinicalTrials.gov (NCT00596713).
All statisticalprocedureswere performed usingSPSSv. 17.0. The chi-squared test (2) withbimodal distribution wasusedasa measureofassociation tocomparethe fre-quenciesbetween the groups. A logistic regressionmodel usingthebackwardWaldmethodforinsertionofvariables inthemodelwasalsousedtoidentifythemainpredictors ofUARS.Asignificancevalueof≤5%(p<0.05)wasusedfor theinterpretationofresults.
Standardsforstaging
Sleep was staged according to the criteria proposed by Rechtschaffen and Kales.10 The arousals and periodic leg movementswerestagedaccordingtothecriteriaproposed by the AmericanAcademy of Sleep Medicine in 2007.10,11 Respiratory events were analyzed according withthe fol-lowingdefinitions:
Apneas(recommendedrule):reduction≥90%inthe ampli-tudeofnasalairflow,lasting≥10s.
Hypopneas (alternative rule): reduction≥50% in the amplitude, lasting≥10s, associated with a decrease in SpO2≥3%and/orwakingepisodeattheEEG.
Airflowlimitation:ratiobetweenthetotaltimeofairflow limitationbytotalsleeptime,expressedasapercentage. Subjectswhoseratiowasbelowthemedianofallassessed volunteerswereconsideredashavingairflowlimitationat thepolysomnography.
The otorhinolaryngological assessment was performed by six previously trained otorhinolaryngologists whowere familiarwiththeroutineofthisexamination,immediately prior to polysomnography preparation. Nasal complaints, physical examination of theUA, andfacial skeletonwere assessed.The investigationofnasalcomplaintsaddressed: nasalobstruction,nasaland/ororopharyngealdryness,oral breathing,anduseoforal ortopicaldecongestantsatthat moment. Complaints were considered present when they occurredeverydayoralmosteveryday.
Thephysicalexaminationconsistedofsystematic inspec-tion of the face, nasal endoscopy, and rhinoscopy. The body mass index (BMI) of individuals was also calculated using the formula: weight (kg)/height2 (m2), in
addi-tion to measures of neck circumference (measuring tape placed over the cricothyroid membrane and measured in cm). Nutritional status was classified as follows: normal weight (BMI<25kg/m2), overweight (BMI≥25kg/m2 and
<30kg/m2),andobese(BMI≥30kg/m2).
The neck circumference was considered altered when >43cminmenor>38cminwomen.
The evaluation of the facial skeleton, performed by inspection,wasconductedby creatingavirtual line pass-ingbytheouteredgeofthelowerlipperpendicularlytothe floor,straightdowntothechin,withtheindividualseated intheFrankforthorizontalposition.Whentheanteriorchin prominencewasatadistance>2mmbackwardsinrelation tothedrawnline, thesubjectwasconsidered ashavinga suggestivesignofmandibularretrognathia.
Regardingthebonystructuresoftheoralcavity,the pres-enceofogivalhardpalateandtypeofdentalocclusionwas assessed.Angle’sclassIIdentalocclusioncorrespondstothe presenceoftheretrudedmandibleinrelationtothe max-illa,suggestive retrognathia.As forthesofttissues ofthe oralcavityandoropharynx,thevolumeofthetongue,soft palateanduvula,tonsilsize,andthemodified Mallampati indexwereassessed.Thetonguewasconsideredlargewhen itwasmarkedbyteeth,suggestingan alterationbetween content(tongue)andcontinent(oralcavity).
lowinsertionoftheposteriortonsillarpillarintheuvula,and thick,whenitshowedthepresenceofedema.Thetonsillar pillarswereconsideredmedializedwhentheywerecloseto theoropharyngealmidline.The uvulawasconsideredlong whenitwasclosetothebaseofthetongueandthickwhen itshowedthepresenceofedema.
The modified Mallampati index wasperformed as pro-posedbyFriedmanetal.,12 withthepatientinthesitting position, with maximal mouth opening, and the tongue relaxedandpositionedwithintheoralcavity.Thesubjects wereclassified into four grades: grade I(it is possible to visualizetheentire oropharynx, includingthe softpalate, thetonsillarpillars,thetonsils,andthetipoftheuvula), gradeII(itispossibletovisualizetheupperpoleofthe ton-silsandtheuvula),gradeIII(itispossibletovisualizepart of thesoft palate and the uvula), andgrade IV(only the hardpalateandpartofthesoftpalatecanbevisualized). Thepalatinetonsils12,13wereclassifiedas:gradeI (intrave-lar),gradeII(extendingbeyondtheanteriortonsillarpillar), gradeIII (extending upto three-quarters of themidline), gradeIV(completelyobstructingtheoropharynx).For indi-vidualssubmittedtotonsillectomy,thenomenclatureused wasA0.GradesIandIIwereconsideredasnon-obstructive hypertrophic palatine tonsils, and grades III and IV as obstructive.
Rhinoscopywasusedtoevaluatethepresenceofpossible nasalseptaldeviation(NSD)andinferiorturbinate hypertro-phy(ITH).NSDwasclassifiedasgradeI(deviationdoesnot touchtheinferiorturbinate),gradeII(deviationtouchesthe inferiorturbinate),orgradeIII(deviationtouchesthelateral wall,compressingtheinferiorturbinate).ITHwasclassified aspresent orabsent.The nosewasconsideredobstructed or‘‘altered’’inthepresenceof:
SeptaldeviationgradeIIorIII,or;
SeptaldeviationgradeI--- nasalobstruction complaintor inferiorturbinatehypertrophy,or;
Inferior turbinate hypertrophy --- nasal obstruction com-plaint.
Theoropharynxwasconsideredunfavorable13,14 whenit hadatleastthreeofthefollowingvariables:
PalatinetonsilsgradeIIIorIV Abnormaluvula(longand/orthick) Abnormalpalate(posteriorand/orthick) Webpalate
Medializedpillars.
Thefacialskeletonwasconsideredunfavorablewhenit showed some of the following features: dental occlusion classII,retrognathia,ogivalhardpalate.
This UA assessment protocol in OSAS has been used andupdatedbytheDepartmentofOtorhinolaryngologyand HeadandNeckSurgeryoftheuniversitywherethepresent studywasconductedforthewritingoftheses/dissertations, articles, resident training, classes for undergraduate stu-dents,courses,andconferences.
InclusioncriteriaforthegroupwithUARS
Thevolunteersthatmetthefollowingcriteriawereincluded intheUARSgroup:
1. AHI<5events/hour.
2. Oxyhemoglobinsaturation>90%duringsleep. 3. AwakeningIndex>15events/hour.
4. Airflowlimitation>6%.
5. Positive clinical picture: Epworth Sleepiness Scale (ESS)>10and/orfatiguescale>4.
Inclusioncriteriaforthecontrolgroup
Thevolunteersthatmetthefollowingcriteriawereincluded inthecontrolgroup:
1. AHI<5events/h.
2. Oxyhemoglobinsaturation>90%duringsleep. 3. AwakeningIndex<10events/h.
4. Airflowlimitation<6%.
5. Negative clinical picture: ESS<10 and/or fatigue scale<4.
Results
During the EPISONO 2007 project, 1042 volunteers were assessed.Atotalof49subjects(5%)wereexcluded,asthey didnotundergootorhinolaryngologicalassessment.Among the993subjects(95.30%)submittedto otorhinolaryngologi-calassessment,381(36%)whohadanAHI>5events/hwere excluded, and 131 (13%) who had oxyhemoglobin satura-tion<90%wereexcluded.Amongtheremaining481subjects (46%),30(3%)wereassessedwhometthecriteriaforUARS definitionand 53(5%) whomet thecontrol groupcriteria (Fig.1).
Table 1 shows the comparison of anthropometric and sociodemographic characteristics of the controland UARS groups.Womenaccountedfor59%ofthecontrolgroupand 66.7% of the group with UARS (p<0.46).The UARS group hadfewerindividualsaged20---29years(41.5%vs.6.7%)and feweragedbetween60and80years(3.8%vs.13.3%).
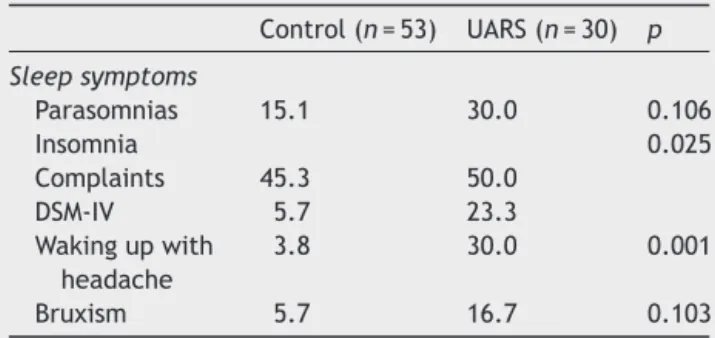
Therewerenosignificantdifferencesbetweenthe con-trol group and UARS when habits and behaviors were assessed:consumptionofcaffeine,alcohol,smoking,illicit druguse,sleeping pills,andsedentary behavior(Table2). When thesleepsymptomswereassessed,it wasobserved that the UARS group had more individuals with insom-nia (complaints: 45.3% vs. 50%; DSM-IV: 5.7% vs. 23.3%), complaintsofnocturnal awakeningduetoheadache(3.8%
vs. 30%), and fatigue and daytime sleepiness (ESS>9: 0%
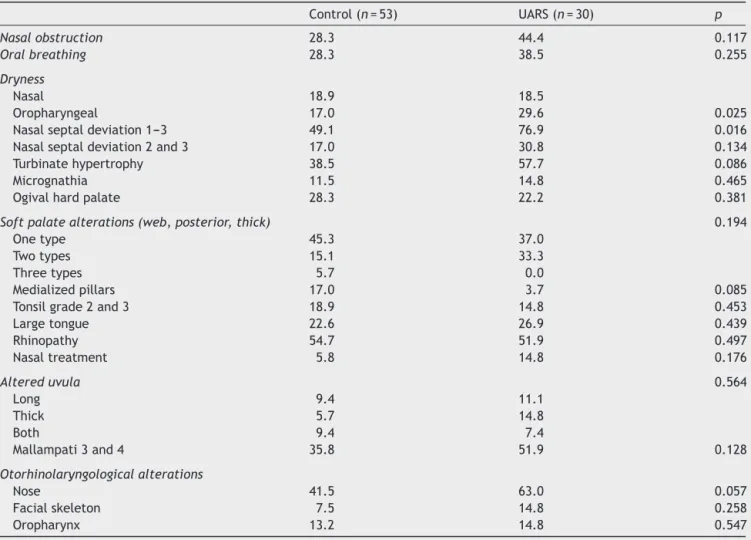
vs. 53.3%).Table 3 shows a comparisonof the systematic physical examination of thefacialskeleton, nose,mouth, and pharynx performed in the control and UARS groups. In the clinical evaluation of nasal symptoms, the UARS group had more oropharyngeal dryness (17% vs. 29.6%;
p=0.025)andseptaldeviationgrades1---3(49.1%vs.57.7%;
N=1042
n=49 (5%)
n=993
n=381
n=612
n=481
UARS group (n=30)
Control group (n=53) n=131 (13%)
Figure1 ProjectEPISONO2007flowchartwithgradualexclusionofparticipantsuptopointwhentheonlyremainingparticipants werethosewhomettheinclusioncriteria.
Table1 Frequency(%) of volunteersin thecontrol and UARSgroups,accordingtotheanthropometricand sociode-mographiccharacteristics.
Control(n=53) UARS(n=30) p
Gender 0.462
Female 58.5 66.7
Male 41.5 33.3
Age(years) 0.011
20---29 41.5 6.7
30---39 26.4 30.0
40---49 18.9 33.3
50---59 9.4 16.7
60---80 3.8 13.3
Overweight (BMI>25kg/m2)
3.8 10.0 0.262
Obesity
(BMI>30kg/m2)
0.0 6.7 0.059
Socioeconomicclass
High 15.1 30.0
Middle 75.5 60.0
Low 9.4 10.0
UARS,upperairwayresistancesyndrome;BMI,bodymassindex.
Table2 Frequency(%) of volunteersin thecontrol and UARSgroups,accordingtosleepsymptoms.
Control(n=53) UARS(n=30) p
Sleepsymptoms
Parasomnias 15.1 30.0 0.106
Insomnia 0.025
Complaints 45.3 50.0
DSM-IV 5.7 23.3
Wakingupwith headache
3.8 30.0 0.001
Bruxism 5.7 16.7 0.103
UARS,upperairwayresistancesyndrome;chi-squaredtest(2)
p<0.05.
Atthelogisticregressionmodel(Table4),itwasobserved that individuals in theUARS group had a15.6-fold higher oddsratioofhavinganalterednose;11.2-foldtimeshigher chanceofbeinghypertensive,and7.6-foldhigherchanceof
complainingof oropharyngealdryness, whencompared to thecontrolgroup.
Discussion
Thisstudycomparedsociodemographiccharacteristics, clin-icalsymptomsrelatedtosleep,andphysicalexaminationof volunteerswithUARSandvolunteerswithoutSRBDina popu-lationsamplefromSãoPaulo.Usingasystematicassessment ofthefacialskeleton,nose,mouth,andpharynx,important, statisticallysignificantdifferenceswerefoundbetweenthe twogroupsandregardingseveralvariables,especiallythose relatedtothenose.
Inthe assessment ofthe nasalseptaldeviation,at the physicalexaminationitwasobservedthatindividualswith UARSshowedanincreasedfrequency ofsometypeof sep-tal deviation whencompared tothe control group. When assessing the turbinate hypertrophy, a trend (p=0.08) to a higher frequency of occurrence in the UARS group was observedwhencomparedtothecontrolgroup.Itisknown that septal deviations are not the only cause of nasal obstructions,butratheroneofanumberofalterations,such asinferiorturbinatehypertrophy,nasalvalvedisorders,and others.Forthisreason,avariabletoencompassthesetwo variablestogetherwascreated,termed‘‘alterednose.’’
The variable‘‘altered nose,’’ which has been used in other studies,14 concomitantly assessesthe threepossible gradesofseptaldeviationanditsassociationwiththe infe-riorturbinates, whether or not hypertrophic, in order to determine whetherthe nose has airflow obstruction. This variablewascreatedtodifferentiatea‘‘normal’’nosefrom anosewithsignificantalterationsinnasalairflowduringa typical assessment performed by an otorhinolaryngologist duringaconsultation.Themaincriticismofthisvariableis thatthis classificationis a subjective assessmentof nasal patencyandmayvarybetweendifferentphysicians. Acous-ticrhinometry,however,providesanobjectiveassessment ofnasalpatency,butitisnotacommonlyusedmethodin clinicalpractice.Duringroutineassessment, otorhinolaryn-gologistsusetheclinicalcomplaintofnasalobstructionand thephysicalexaminationofthenosetohelpdiagnosenasal obstruction, which arethe same parameters used in this study.
Table3 Frequency(%)ofvolunteersinthecontrolandUARSgroups,accordingtothesystematicphysicalexaminationofthe facialskeleton,nose,mouth,andpharynx.
Control(n=53) UARS(n=30) p
Nasalobstruction 28.3 44.4 0.117
Oralbreathing 28.3 38.5 0.255
Dryness
Nasal 18.9 18.5
Oropharyngeal 17.0 29.6 0.025
Nasalseptaldeviation1---3 49.1 76.9 0.016
Nasalseptaldeviation2and3 17.0 30.8 0.134
Turbinatehypertrophy 38.5 57.7 0.086
Micrognathia 11.5 14.8 0.465
Ogivalhardpalate 28.3 22.2 0.381
Softpalatealterations(web,posterior,thick) 0.194
Onetype 45.3 37.0
Twotypes 15.1 33.3
Threetypes 5.7 0.0
Medializedpillars 17.0 3.7 0.085
Tonsilgrade2and3 18.9 14.8 0.453
Largetongue 22.6 26.9 0.439
Rhinopathy 54.7 51.9 0.497
Nasaltreatment 5.8 14.8 0.176
Altereduvula 0.564
Long 9.4 11.1
Thick 5.7 14.8
Both 9.4 7.4
Mallampati3and4 35.8 51.9 0.128
Otorhinolaryngologicalalterations
Nose 41.5 63.0 0.057
Facialskeleton 7.5 14.8 0.258
Oropharynx 13.2 14.8 0.547
UARS,upperairwayresistancesyndrome;chi-squaredtest(2)p<0.05.
itcanbesaidthatthevolunteerswithUARShasmorenasal obstruction,observedduringthephysicalexamination,than thevolunteerswithoutSRBD.
Itisknownthatnotonlythealterationsdetectedatthe physical examination determine whether or not a patient hasnasalobstruction.Thesefindingsshouldalwaysbe corre-latedwithclinicalsymptoms.Inthepresentstudy,thegroup withUARShad more complaintsof oropharyngealdryness thanthecontrolgroup,indicativeoforal breathingduring
sleep.Conversely,regardingtheclinicalcomplaintofnasal obstruction, theauthorsdidnot finda statistically signifi-cantdifferencebetweenthetwogroups,butratherfound agreatertendencyfor thistypeofcomplaintinthegroup withUARS(p<0.11).
The mouth andoropharyngeal assessment of the study volunteers showed data consistent with the available lit-erature,i.e., lowprevalence ofmicrognathia,ogival hard palate,tonsillarhypertrophy,andlargetongueinindividuals
Table4 LogisticregressionmodelofUARSpredictors.
B S.E. p OR 95%CI
Age 0.09 0.03 0.007 1.1 1.0---1.2
Hypertension 2.41 0.81 0.003 11.2 2.3---54.4
Alterednose 2.75 0.86 0.001 15.6 2.9---84.0
Oropharyngealdryness 2.03 0.82 0.013 7.6 1.5---37.5
Rhinopathy −1.85 0.79 0.019 0.2 0.0---0.7
Constant −6.56 1.71 0 0.0
UARS,upperairwayresistancesyndrome;logisticregressiontestwithbackwardWaldmethod.
withUARS.Thesealterationsaremostfrequentlyobserved inpatientswithOSASandarenotclassicallyassociatedwith patientswithUARS.Inthisregard,itcanbesaidthat indi-vidualswithUARSaresimilartoindividualswithoutSRBD.
The investigation of thevariableoropharynxalteration inthisstudyshowedthatbothgroupshadlowprevalenceof patientswiththisalteration.Thisvariable,likethealtered nosevariable,consistsinasetofdataobtainedduringthe physicalexaminationoftheoropharynx,inorderto differ-entiate a normal oropharynxfrom one disclosing a series ofalterationsthatmightberelatedtoSRBD.Manyauthors believethatoropharyngealalterationsaremorerelatedto OSASthattoUARS.
Regarding the other variables measured in this study, results similar to those described in the literature were observed.Therewerenodifferencesregardinggenderand socioeconomicdistributionwhenthetwogroupswere com-pared. Despite the trend toward a higher percentage of obese individuals in the UARS group (p=0.06), there was averysmallnumberofvolunteerswithBMI>30,andthese resultsareconsistentwithclassiccharacteristicsofpatients withUARSwho,ingeneral,arenotobese.When investigat-ingclinicalsymptomsrelatedtosleep,theauthorsobserved resultsconsistentwithcharacteristicsthatarewell estab-lished intheUARSliterature, i.e.,increasedfrequencyof insomnia andnocturnal headachecomplaintsinthe group withUARS.
The typical respiratory event of UARS is the awaken-ingassociatedwithrespiratoryeffort,orrespiratoryeffort relatedarousal (RERA).Itcauses increasedUAresistance, generating a progressive increase in inspiratory nega-tivepressure,withconcomitant decreaseinnasal airflow, withoutapnea/hypopneaandoxyhemoglobindesaturation, followed by awakening, with immediate decrease in UA resistance.2The gold standardfor RERAdetectionis mea-surementofesophagealpressurebyanesophagealballoon thatshowsaprogressiveincreaseinnegativeintrathoracic pressure that culminates in cortical awakening.1 This is aninvasiveanduncomfortabletechnique,thatimpairsthe onsetormaintenanceofsleepand,therefore,isnotwidely usedinbasalpolysomnographyliteraturestudies;forthese reasons,itwasnotusedinthepresent studyeither,which comprisesastudylimitation.
However,althoughcontroversial,someauthorsmaintain thattheefficiencyofthenasalpressuretransducercoupled tothenasalcannula,whetherornotassociatedtoa thermis-tor,mayyieldasimilarresulttoanesophagealcatheterto identifyincreasedrespiratoryeffortandairflowlimitation, atechniquethatismorecomfortableandlessinvasive.15---17 In additiontothestudy limitationregardingtheuseof theesophagealballoon,theinterpretationandassessment byaphysicianmayintroduceabias.Inan attemptto sys-tematizetheexaminationandtheclassificationstobeused, aiming at reducing the bias, only otorhinolaryngologists wererecruitedtoperformpatientphysicalexamination,and the number of physicians who assessed patients was also limited (n=6). Furthermore, prior to patientassessment, theprofessionalsweretrainedandfamiliarizedwithallthe classificationsused.
ThecriteriaforUARSdefinitionarestillcontroversialin theliterature.The lackofa consensusamongresearchers creates great difficulty in performing studies involving
patientswithUARSand,consequently,hinderstheadvance ofknowledge aboutthis disease.Nevertheless,this study, usingawell-definedUARS criterion,involved an otorhino-laryngologicalassessmentcarriedoutinapopulationsample representativeof one of the mostimportant cities in the world. Therefore, in accordance with these results, the authorsbelievethat,UARSisamultifactorialdiseasewith increased risk of associated comorbidities; however, the nosehasakeyroleinthephysiopathologyofthediseaseand shouldalwaysbethoroughlyassessedinapatientdiagnosed withUARS.
Conclusions
Systematicassessmentofthefacialskeleton,mouth, phar-ynx, and nose in volunteers with UARS and volunteers withoutSRBD,throughorofacial-cervicalphysical examina-tioninapopulationsamplerepresentativeofthecityofSão Paulo,showedthatthepresence ofUARSis mainly associ-atedwith nasalalterations and oropharyngealdryness, in additionto the risk of high blood pressure, regardless of genderandpresenceofobesity.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.AmericanSleepDisorders Association.Theinternational clas-sification of sleep disorders, revised: diagnostic and coding manual.Rochester,MN:AmericanSleepDisordersAssociation; 1997.
2.GuilleminaultC,WinkleR,KorobkinR,SimmonsB.Childrenand nocturnal snoring:evaluationof theeffects ofsleeprelated respiratoryresistiveloadanddaytimefunctioning.EurJPediatr. 1982;139:165---71.
3.GuilleminaultC,StoohsR,ClerkA,CetelM,MaistrosP.Acause ofexcessivedaytimesleepiness.Theupperairwayresistance syndrome.Chest.1993;104:781---7.
4.Edström L, LarssonH, Larsson L. Neurogenic effects onthe palatopharyngeal muscle in patients with obstructive sleep apnoea:amusclebiopsystudy.JNeurolNeurosurgPsychiatry. 1992;55:916---20.
5.GuilleminaultC,LiK,ChenN-H,PoyaresD.Two-pointpalatal discrimination in patients withupper airway resistance syn-drome,obstructivesleepapneasyndrome,andnormalcontrol subjects.Chest.2002;122:866---70.
6.Chen W, Kushida CA. Nasal obstruction in sleep-disordered breathing.OtolaryngolClinNorthAm.2003;36:437---60.
7.GoldAR,Schwartz AR.The pharyngealcriticalpressure.The whysandhowsofusingnasalcontinuouspositiveairway pres-surediagnostically.Chest.1996;110:1077---88.
8.TerzanoMG,ParrinoL, SherieriA, ChervinR,ChokrovertyS, GuilleminaultC,etal.Atlas,rules,andrecordingtechniquesfor thescoringofcyclicalternatingpattern(CAP)inhumansleep. SleepMed.2001;2:537---53.
9.KrygerMH,RothT,DementWC.Principlesandpracticeofsleep medicine.4thed.Philadelphia,PA:Elsevier/Saunders;2005.
11.Aurora RN, Kristo DA, Bista SR, Rowley JA, Zak RS, Casey KR,et al.Thetreatmentofrestless legssyndromeand peri-odiclimbmovementdisorderinadults---anupdatefor2012: practiceparameterswithanevidence-basedsystematicreview andmeta-analyses.Sleep.2012;35:1037.
12.FriedmanM.Sleepapneaandsnoringsurgicalandnon-surgical therapy.Edinburgh:Saunders/Elsevier;2009.
13.ZonatoAI,BittencourtLR, MartinhoFL,Júnior JFS,Gregório LC,TufikS.Associationofsystematicheadandneckphysical examinationwithseverityofobstructivesleepapnea---hypopnea syndrome.Laryngoscope.2003;113:973---80.
14.Zonato AI, Martinho FL, Bittencourt LR, de Oliveira Cam-ponês Brasil O, Gregório LC, Tufik S. Head and neck
physical examination: comparison between nonapneic and obstructive sleep apnea patients. Laryngoscope. 2005;115: 1030---4.
15.MontserratJM,FarréR,BallesterE,FelezMA,PastóM,Navajas D.Evaluationofnasalprongsforestimating nasalflow.AmJ RespirCritCareMed.1997;155:211---5.
16.Epstein MD, Chicoine SA, Hanumara RC. Detection of upper airway resistance syndrome using a nasal cannula/pressure transducer.Chest.2000;117:1073---7.