www.rpped.com.br
REVISTA
PAULISTA
DE
PEDIATRIA
CASE
REPORT
Pathologic
aerophagia:
a
rare
cause
of
chronic
abdominal
distension
Lisieux
Eyer
de
Jesus
∗,
Ana
Beatriz
C.S.S.
Cestari,
Orli
Carvalho
da
Silva
Filho,
Marcia
Antunes
Fernandes,
Livia
Honorato
Firme
UniversidadeFederalFluminense(UFF),Niterói,RJ,Brazil
Received11November2014;accepted18January2015 Availableonline30June2015
KEYWORDS Aerophagy;
Pathologicdilatation; Gastricemptying
Abstract
Objective: Todescribeanadolescentwithpathologicaerophagia,arareconditioncausedby excessive andinappropriate swallowing ofair andto review itstreatment anddifferential diagnoses.
Casedescription: An11-year-oldmentallyimpairedblindgirlpresentingseriousbehavior prob-lemsandseveredevelopmentaldelaywithabdominaldistensionfromthelast8months.Her pasthistoryincludedaNissenfundoplication.AbdominalCTandabdominalradiographsshowed diffusegasdistensionofthesmallbowelandcolon.Hirschsprung’sdiseasewasexcluded.The distentionwasminimalatthemomentthechildawokeandmaximalatevening,andpersisted after controlofconstipation.Audiblerepetitive andfrequent movements ofairswallowing wereobserved.Thediagnosisofpathologicaerophagiaassociatedtoobsessive---compulsive dis-orderanddevelopmentaldelaywasmade,butpharmacologicaltreatmentwasunsuccessful. Thepatientwassubmitted toanendoscopicgastrostomy,permanentlyopenedandelevated relativetothestomach.Thedistentionwasresolved,whilemaintainingoralnutrition.
Comments: Pathologicaerophagiaisarareself-limitingconditioninnormalchildrenexposedto highlevelsofstressandmaybeapersistingprobleminchildrenwithpsychiatricorneurologic disease.Inthislastgroup,thediseasemaycauseseriouscomplications.Pharmacologicaland behavioraltreatments areill-defined.Severe cases may demandsurgical strategies, mainly decompressivegastrostomy.
© 2015 Sociedadede Pediatriade São Paulo. Publishedby Elsevier Editora Ltda. Allrights reserved.
DOIoforiginalarticle:http://dx.doi.org/10.1016/j.rpped.2015.01.003
∗Correspondingauthor.
E-mail:lisieux@uol.com.br(L.E.Jesus).
PALAVRAS-CHAVE Aerofagia;
Distensãopatológica; Esvaziamento gástrico
Aerofagiapatológica:umacausararadedistensãoabdominalcrônica
Resumo
Objetivo: Descreverocasodeumaadolescentecomaerofagiapatológica,umadoenc¸arara causadapeladeglutic¸ãoexcessivaeinapropriadadear,erevisarotratamentoeosdiagnósticos diferenciais.
Descric¸ãodocaso: Meninade11 anosportadoraderetardo mentalecegueira, apresentava problemascomportamentaisassociadosaretardododesenvolvimento,foiconsultadapor dis-tensãoabdominalpersistenteporoitomeses.Suahistóriapregressaincluíaumafundoplicatura àNissen.Tomografiaeradiografiasabdominaismostravamdistensãodifusadotratodigestivo porar, incluindo cólonedelgado. Doenc¸ade Hirschsprungfoi excluída. A distensão persis-tiumesmoapósocontroledaconstipac¸ãoeeramínimademanhãemáximaànoite.Ruídos audíveiserepetitivosdedeglutic¸ãodearforamobservadoseauscultados.Acrianc¸afoitratada farmacologicamentecomodiagnósticodeaerofagiapatológicaassociadoadistúrbioobsessivo compulsivo,semsucesso.Apacientefoisubmetidaagastrostomiadescompressivaendoscopia emantevenutric¸ãooral.
Comentários: Aaerofagiapatológicaéumadoenc¸araraeautolimitadaemcrianc¸as,maspode serum problemagravee persistentenaquelascomproblemasneuropsiquiátricos, nasquais podecausarcomplicac¸õessérias.Ostratamentoscomportamentaisefarmacológicostêmpouco sucesso nesse grupo.Casos graves podem precisar detratamento cirúrgico, principalmente gastrostomiadescompressiva.
© 2015SociedadedePediatria de SãoPaulo. Publicado porElsevier EditoraLtda. Todosos direitosreservados.
Introduction
Pathologic aerophagia, caused by excessive and inappro-priate swallowing of air, is a rare condition in clinical Pediatrics.Thediseaseaffectsmainlynormalchildren deal-ing with stress situations, but approximately a quarter presentseverepsychiatricand/orneurologicproblems. Dif-ferentialdiagnosisprimarilyinvolvesothergastrointestinal dysfunctionalsyndromes.
Wedescribehereinacaseofseverepathologic aeropha-giainaschool-agedmentallyimpairedchildandreviewthe literatureonthetheme.
Case
description
An11-year-oldmentallyimpairedgirlwastransferredfrom another hospital to the Pediatric ward of Antonio Pedro University Hospital, Rio de Janeiro, Brazil, to be investi-gatedforpossibleaganglionicmegacolon.Thegirlwasblind, presented serious behavior problems and severe develop-mentaldelay andwasunabletocooperatewithanamnesis andphysicalexamination.Hermotherrecalledahistoryof abdominaldistensiononlyfromthelast8months, unrespon-sive torepetitiveenemas and associatedwith paincrises thatdemandedrepetitiveconsultationstoPediatric emer-gencyservices.Moderateconstipationwasnotedsincethe girl wasa toddler and dealt with by occasional usage of orallaxatives.Appetitewaspreservedduringthecrisesand therewerenosignsofgastricdysfunction,retchingor vomi-ting.
Her physical examination showed a seriously under-nourished prepubertal girl −14.5kg (<5th percentile of
WorldHealthOrganizationgrowthcurve);1102cm(<5th
per-centileof WorldHealthOrganizationgrowth curve)1,with
severediffuseabdominaldistension(abdominal circumfer-ence76cmattheleveloftheumbilicus)(Fig.1).Peristalsis wasnormal.Therewerenopalpablemassesorabdominal pain.Analandrectalexamination demonstrateda normo-tonictopicanus.Therectumwasfullofsolidfeces.
Neuropsychiatric evaluation confirmed severe develop-mental delay and disproportionate aggressiveness toward the medical team. Several repetitive stereotyped
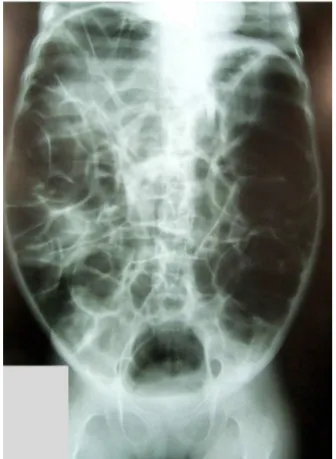
Figure2 Diffuse andseveregasdistension, attainingsmall intestineandcolon.
ments (repetitivebiting of the hands,moving the thorax forward and backwards and agitating a chatterbox) were observed. The patient was in chronic use of pericyazine (8mginthemorningand10mgatnight)thatwasgradually withdrawnduringadmission.
The childwasbornprematurelyafteratwingestation. Shepresentedcongenitalcataractandwassubmittedtoa fundoplication and gastrostomy at 3 months old to treat swallowingproblems,repetitiveaspirationandsymptomatic gastroesophageal reflux. After a difficult perinatal period thepatientwasabandonedbythemotherand institutional-ized.Hergastrostomywastakenoffandshewasthenorally fed.Thegirlwasadoptedat2-years-old,togetherwithtwo otherneurologicallyimpairedchildren.Thefamilyalready had other natural children and the father is wheelchair-bound.
An abdominal CT and several abdominal radiographs showeddiffusegasdistensionofthesmallbowelandcolon (Fig.2).
Herconstipationwascontrolledwithdailyenemasfor15 days, after which the girl evacuated spontaneously daily. A rectal biopsy excluded Hirschsprung’s disease. Clinical observationdemonstratedthatherdistensionwasminimal atthemomentthechildawokeinthemorning(mean abdom-inalcircumferenceof68cm)andmaximalatevening(mean abdominalofcircumference74cm).Audiblerepetitiveand frequent movements of air swallowing wereobserved. To test the hypothesis of pathologic aerophagia in a patient incapable of burping, her abdominalperimeter was mea-sured(76cm)andanasogastric catheterwasinstalledand
opened for 24h. At the end of the period, her abdomi-nalperimeter was61cm.Afew hoursaftertaking offthe catheterherabdominalperimeterreached78cm.
Departing fromthe diagnosis of pathologic aerophagia associatedtoobsessive---compulsive disorder and develop-mentaldelay,treatmentwithrisperidone1.5mg/day(0.5mg in the morning and 1.0mg at night) for 3 weeks was unsuccessful. The usage of oral carbon was considered unpractical.
The child wassubmittedtoan endoscopicgastrostomy withoutcomplications. Thefamilywastaughttomaintain thegastrostomyopenedandelevated>30cmrelativetothe stomach as frequently as possible, to allow the elimina-tionof swallowed air, avoid the loss of gastric secretions and at the same time enable normal oral nutrition. This waspossible by using an elongating device connected to the gastrostomy tube and fixed to the anterior thoracic wallin a superior direction when the child wassitting or standing,duringtheday,andthechronicabdominal disten-sionresolved.Thechild,however,maintainedtherepetitive swallowingmovements.
Atthemomentofthisreport,thefamilyreportsconstant drainageofairfromthegastrostomyandrecurrenceofthe abdominaldistensionwheneverthegastrostomystaysclosed fora long period.Chronicconstipation didnotrecur. The girlstaysunderpsychotherapytreatmentandsocialservices supervision.
Discussion
Inchildren,70%ofthebowelgascomesfromswallowedair.2
The radiological expression of aerophagia is the presence ofgasthroughout thesmallbowel,whichisphysiologic in newbornsand infants,but limitedtospecificsituations in olderchildren.
Rome criteria defined pathological aerophagia as air swallowingcausingabdominaldistensionand/or repetitive flatulence/belching,present for >12weeksin ayear. This standardmaybeproblematicinmentallyimpairedchildren presentingconstipationandpreviouslysubmittedto fundo-plication, both of which are common in this population. Thosepatientsarefrequentlyunabletoburpandrectalfecal masseslimittheeliminationofflatus.Onlyourpatientand twoothersreportedcases3,4have beenpreviously
submit-tedtofundoplications,which mayhaveexaggerated their pathologicalaerophagia,duetotheimpossibilityofburping andbelching.Mostpatientswithpathologicalaerophagiaare school-aged children andadolescents.The diseaseis rare andchronic:almosthalfofthepatientspresentsymptoms for≥1yearatthetimeofdiagnosis.
Psychiatricdiseasesattain1/4ofpathological aeropha-gia cases, mostly mental retardation, autism and Rett syndrome.5 Althoughpathologicalaerophagia israre,8.8%
of institutionalized mentally impaired children present aerophagia.2 Pathological aerophagia may represent the
birthofsiblings,divorceofparents,hospitaladmission).In thosecasespathologicalaerophagia tendstodisappear as thestressfulsituationresolves,butlanguageand/or behav-ior problems are common,together withobvious signs of anxiety.Insomepatientspathologicalaerophagiaissimply substitutedbysomeotherexpressionofanxiety.6
Somespecialistsevenassociatepathologicalaerophagia toself-destructingbehavior.Mentallyimpairedchildrenalso sufferfromanxiety,butitsmanifestationsmaybeatypical andmoredifficulttodetectandtotreatinthispopulation. Pathological aerophagia may complicate with volvu-lus,intestinalnecrosis/perforationandevendeath.3,7,8All
reportedsurgicalcomplicationsattainedmentallyimpaired patients.VanderKolketal.describenineseverelyretarded institutionalized adultswithsevere surgical complications (gastric perforation, gastric necrosis and volvulus, one death),whichpresentedpathologicalaerophagiafrom child-hood. Those authors suggest that untreated pathological aerophagia in neurologically impaired children may per-sistaftermaturityandleadtoseriouscomplicationsinthe long-term, which maybe prevented by the insertionof a gastrostomy.9
The disease might be caused either by psychogenic myoclonus-likeairswallowingmovements(asweobserved in our index patient) or by repetitive reflex air swallow-ing movements due to paroxysmal openings of the upper esophagealsphincterinmentallyimpairedpatients.
Pathologicalaerophagiapatientsnormallypresenttothe doctorbecauseofsevere persistentabdominaldistension, typicallyminimalwhenthepatientawakesinthemorning (duetolessairswallowingduringsleepandeliminationof flatusduringthenightperiod)andmaximalatlateevening. Associatedabdominalpainisfrequent.Belching/burpingis also common. Audible air swallowing sounds are pathog-nomonicof thecondition. Associatedfunctionalintestinal disordershave beenreported,mainlyconstipation.6
Occa-sionallythereissomedegreeofrespiratoryrestrictiondue toextremeabdominaldistension.Anabdominalradiograph shows gastric and diffuse intestinal distension, including smallbowel,without signsof intestinalobstruction. Fluo-roscopymaydemonstratethetypicalswallowingmovements andabnormalpharyngoesophagealcoordination.10
The differential diagnosis is with functional gastroin-testinal problems (chronic intestinal pseudoobstruction, severeconstipation,Hirschsprung’sdisease),malabsorption syndromes,anatomicalintestinalobstructionand tracheoe-sophagealfistulae.Gasbloatsyndromemaybeconsidered inpatientswhohadapreviousfundoplication.The diagno-sisofpathologicalaerophagiaisrareanddependsonclinical awareness.Theexclusionofotherconditionsmaydemand complexcomplementaryexamsanddelaytreatment.Inour case, the diagnosis was based on exclusion of intestinal muscularor neuronalabnormalities by biopsy,persistence ofsymptomsaftercontrolofconstipationandpresenceof largequantitiesofairinthesmallintestine,without radio-logicsignsofintestinalobstruction(whichexcludeintestinal pseudoobstruction).
Littleinformationconcerningtreatmentofpathological aerophagiaisavailable,withaverylowlevelofevidence. Variouspharmacological treatmentshave been suggested. Simethicone and anti-spasmodics can be tried, with low effectivity.Oralcarbontabletsasairabsorbentshavebeen
used,buttheirdosagesandefficacyareunclear.6,11 Inthe
context of the good results of benzodiazepines to treat myoclonus-like syndromes and the observation that low dose intravenous clonazepan can abolish the pathological swallowingmovementsinpathologicalaerophagiapatients, Hwang et al. prospectivelytreated 15 mentally impaired childrenwithpathologicalaerophagiawithaloworaldose of clonazepan(0.025mg/kg/day intwodoses, slowly aug-mentedto0.1mg/kg/dayasneeded)for4months(orfora monthafterthepatientwasasymptomatic).The drugwas slowlytaperedoff.Noserioussideeffectswereobserved. Whencomparedtoacontrolgrouptreatedwithonly reas-surance (n=7), 67% of the clonazepan group and 14% of the reassurance group resolved the symptoms (p=0.032), both without recurrence.10 The effectof clonazepan may
becentrallymediated,duetocontrolof anxietyoraffect directlythepathologicalmechanismthattriggersthe repet-itiveswallowingmovements.
Behavioral/psychologicaltherapymaybetried,butthe efficacyisquestionableinmentallyimpairedpatients. Reas-surance/psychotherapy was efficient in half of the cases treated byDelapetriereetal.6 Inourchild,we tried
spe-cific pharmacological treatment for obsessive/compulsive disorderwithoutsuccess.
Phonoaudiologictreatmenthasbeensuccessfullytriedin 3/13patients6butisnotanoptionincasesofserious
psychi-atricdiseaseand/orcognitivedeficit.Inourpatientspeech therapistsjudgedthatreconditioningwasnotpossible.
Decompression with a nasogastric tube can be used in cases of acute distension. Surgical treatments are rarely needed, almost exclusively in mentally impaired patients. Gastrostomy is the most frequent proposal, but maynotalways beeffective, asin thecasesof Fukuzawa and Gauderer.3,12 Recently Fukuzawa et al.3 proposed an
esophagogastric separation and an abdominal esophageal decompressivestomatotreattwoseverelyaffectedpatients unresponsive togastrostomy(both previously complicated withvolvulusandnecrosis).
In conclusion, pathological aerophagia is a rare condi-tionthatoccursin normalchildrenexposed tohighlevels of stress, for whom the disease is normally self-limited, or in children with psychiatric or neurologic disease. In this lastgroup,the diseasemay persistand causeserious complications.Pharmacological andbehavioraltreatments areill-defined and their successis doubtful. Severe cases maydemandsurgicalstrategies,mainlydecompressive gas-trostomy.
Funding
Thisstudydidnotreceivefunding.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
childrenand adolescents.Bull WorldHealth Organ.2007;85: 660---7.
2.Loening-Baucke V. Aerophagia as cause of gaseous abdom-inal distension in a toddler. J Pediatr Gastroenterol Nutr. 2000;31:204---7.
3.Fukuzawa H, Urushihara N, Fukumoto K, et al. Esoph-agogastric separation and abdominal esophagostomy via jejunal interposition: a new operation for extreme forms of pathologic aerophagia. J Pediatr Surg. 2011;46: 2035---7.
4.LecineT,MichaudL,GottrandF,etal.Childrenwhoswallow air.ArchPediatr.1998;5:1224---8.
5.HwangJB,ChoiWJ,KimJS,etal.Clinicalfeaturesof patho-logic childhood aerophagia: early recognition and essential diagnostic criteria. J Pediatr Gastroenterol Nutr. 2005;41: 612---6.
6.DelaperrièreN,OregaM,MaurageC,etal.Pathologicchildhood aerophagia.ArchPediatr.2007;14:10---4.
7.TrillisF Jr,GaudererMW,PonskyJL,MorrisonSC. Transverse colonvolvulusinachildwithpathologicaerophagia.JPediatr Surg.1986;21:966---8.
8.BasaranUN,InanM,AksuB,CeylanT.Colonperforationdue topathologicaerophagiainanintellectuallydisabledchild.J PediatrChildHealth.2007;43:710---2.
9.VanderKolkMB,BenderMH,GorisRJ.Acuteabdomenin men-tallyretardedpatients:roleofaerophagia.Reportofninecases. EurJSurg.1999;165:507---11.
10.HwangJB,KimJS,AhnBH,JungCH,LeeYH,KamS.Clonazepan treatmentofpathologicchildhoodaerophagiawith psychologi-calstresses.JKoreanMedSci.2007;22:205---8.
11.Rosenbach Y, Zahavi I,Nitzan M, DinariG. Pathologic child-hood aerophagy: an under-diagnosed entity. Eur J Pediatr. 1988;147:422---3.