REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
OfficialPublicationoftheBrazilianSocietyofAnesthesiologywww.sba.com.br
SCIENTIFIC
ARTICLE
Knowledge
of
anaesthesiologists
in
Recife
with
respect
to
potential
risks
in
the
operating
room----cross-sectional
study
Rafaela
de
Melo
Simões
Lima
a,
Giselle
Lauritzen
Duarte
b,
Tânia
Cursino
de
Menezes
Couceiro
a,∗,
Marcela
Kelly
Silva
do
Nascimento
a,
Luciana
Cavalcanti
Lima
a,baInstitutodeMedicinaIntegralProf.FernandoFigueira(Imip),Recife,PE,Brazil
bFaculdadePernambucanadeSaúde(FPS),Recife,PE,Brazil
Received10June2013;accepted25June2013 Availableonline4April2014
KEYWORDS
Anesthesiologist; Knowledge; Professionalrisk; Surgerycenter
Abstract
Objectives:the healthcareshouldbeasafe act,freeofadverseevents.However, indaily practice an excessive exposure to factorsthat endanger the health of the professional is observed.Thesurgicalcenterstandsoutasoneofthesiteswheretheprofessionalinvolved ismore vulnerable. Thisenvironment istheanaesthesiologist’s workplace,andthis profes-sionalmustdealwithitspotentialcomplicators.Thisstudyaimedtoevaluatetheknowledge ofanaesthesiologistsinRecifeonvarioussituationsofriskintheworkplace.
Method: across-sectionalstudyinwhichstructuredquestionnaires,completedvoluntarilyand anonymouslybytheanesthesiologistitself,wereappliedtoassesstheknowledgeofthe poten-tialrisksintheoperatingroom.DatawereanalyzedusingEpiInfoversion7.
Results:atotalof162anaesthesiologistsrespondedtothequestionnaire,38.02%ofthese pro-fessionalsregisteredatCooperativeofAnaesthesiologistsofPernambuco.Ofthese,3.7%read themanualoftheCommitteeonHospitalInfectionControl(ComissãodeControledeInfecc¸ão Hospitalar)oftheirinstitutionand40.74%chosethecorrectoption,‘‘technicaldirector’’,as responsibleforensuringproperworkingconditions.Ofthetotal,5.56%statedthatthe anaes-thetics’pollution indexinthe operating theater was monitored. Only1.85% ofthe sample wassubjectedtoperiodicscreeningfortuberculosis.By analyzingthehypotheticalsituation ofcontaminationwithapatientwithhepatitisC,only43.83%knewthatthereisnoeffective post-exposureprophylaxis.
Conclusion:educationalcampaignsshouldbeimplementedtoimprovetheknowledgeofhealth professionalsandclarifyinstitutionsandprofessionals’rightsandduties.
©2014SociedadeBrasileiradeAnestesiologia.PublishedbyElsevier EditoraLtda.Allrights reserved.
∗Correspondingauthor.
E-mail:taniacouceiro@yahoo.com.br(T.CursinodeMenezesCouceiro).
Introduction
Thehealthcareshouldbeasafeact,freeofadverseevents. However,whatisobservedindailypracticeisanexcessive exposuretofactorsthatendangerthephysicalandmental integrityofthehealthprofessional.
Amongthevariousscenariostoprovideservicestowhich thephysicianisexposed,thesurgicalcenterstandsoutas oneofthemostsignificant,inwhichtheprofessionalismore vulnerabletopotentialrisks.Thisscenarioisuniqueamong workplaces, with continuous exposure to noise pollution, chemicalfumes, ionizingradiation,infectious agents, and increasedlevelsofpsychologicalstress.1
This environment is the anaesthesiologist’s workplace, and thisprofessional must dealwithits potential compli-catorsanditis herethathelivesmostofhisdays.1Given
thisreality,itisofparamountimportancethatthe profes-sionalsinvolvedinthisactivitybeawareofalltherisksand thierconsequences,aswell asthe dutyofthehospitalto providedignifiedandsafeconditionsfortheexerciseofthe profession.
Afterreviewingtheliterature,wefoundstudiesthat out-linetheprofile oftheanesthesiologistsandevaluatetheir qualityof life,2,3 in additiontoresearchinvestigating the
physicalandpsychologicalconsequencesoflong-term expo-suretotheunhealthyenvironmentoftheoperatingroom.1
However,studiesarelacking thatinquire aboutthe anaes-thesiologist’sknowledgeoftheriskssurroundingthe profes-sion,despitetheexistenceofextensiveliteraturedescribing theseaggravatingfactors.Theaimofthisstudywasto eval-uatethe knowledgeof anaesthesiologistsin Recife onthe varioushazardsituationsintheirworkenvironment.
Method
After approval by the Ethics Committee for Research on Humans of the Instituto de Medicina Integral Prof. Fer-nando Figueira (CEP/Imip), an descriptive cross-sectional studywasconductedbetweenOctober2011andMay2012, involving anaesthesiologists in Recife (PE) accredited at Anaesthetists’CooperativeofPernambuco(Coopanest/PE). Forparticipation inthis research,anaesthesiologistsin activity in hospitals in Recife who signed an informed consentformwereselected.Exclusioncriteriawere incom-pletelyfilledquestionnairesandanaesthesiologistswhodo notparticipateroutinelyinclinicalcarewithproceduresin theoperatingroom.
Themethodologyconsistedofdevelopingaquestionnaire thatincludedthepotentialrisksintheoperatingroom,with itemsabout physical risks,infectionandfire, andtheuse of electrocautery. The physician was informed about the purpose of this research and was asked to offer his/her collaboration.Thequestionnairewasthengiventothe par-ticipants at their workplaces. The participants received orientationonhowtoanswerthequestions;itwasexplained thatonlyanassertionwascorrect.Theauthorsofthisstudy wereavailableforanyclarificationneededaboutthe ques-tionnaire. The identityof the participantswaspreserved. Theresearchfollowedtheethicalprinciplesadoptedby Res-olution196/96oftheNationalHealthCouncil(CNS)andwas approvedbyCEP/IMIPundernumber2459.
Table1 Generalcharacteristicsofthesample.
Variable n %
AST 20 12.3
Master 09 5.5
Doctorate 03 1.8
Yearsofpracticeofanaesthesiology
0---5 46 28.4
5---10 11 6.7
10---15 29 17.9
>15 76 46.9
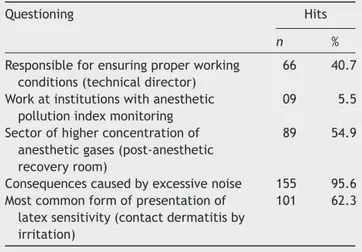
Table2 Knowledgeoftheanesthesiologistwithrespectto
physicalhazards.
Questioning Hits
n %
Responsibleforensuringproperworking conditions(technicaldirector)
66 40.7
Workatinstitutionswithanesthetic pollutionindexmonitoring
09 5.5
Sectorofhigherconcentrationof anestheticgases(post-anesthetic recoveryroom)
89 54.9
Consequencescausedbyexcessivenoise 155 95.6 Mostcommonformofpresentationof
latexsensitivity(contactdermatitisby irritation)
101 62.3
The variables studied were physical risks (anesthetic gases,radiation,allergicreactions,noisepollution), infec-tion (respiratory viruses, herpes viruses, hepatitis, acute immunodeficiencyvirus,tuberculosis,virusesinlasermist) variablesandoffiresanduseofelectrocautery(surgical spe-cialtiesinvolved,oxidizingagentsintheoperatingroom).
FordataanalysisweusedthesoftwareEpiInfoversion 7program.The resultswerepresentedintheformof fre-quencydistribution.
Results
Among the 426 accredited anaesthesiologists and those availableinthehospitalsystem,162agreedtoparticipate, correspondingto38% of thoseregistered in their Cooper-ative.Oftherespondents,46.9%practicethespecialtyfor over15years,12.3%haveahigherdegreeofanaesthesiology and5.5%anMSc(Table1).
Astothequestioningabouttheresponsibilityforensuring proper and decent working conditions for the anesthesi-ologist, only 40.7% chose the correct answer, ‘‘technical director’’(Table2).
Table3 Knowledge of anesthesiologist asto the risk of infection.
Questioning Hits
n %
Hadaccessto/readCCIHmanual 06 40.7
Classificationofthesurgicalcenter (criticalarea)
94 58
Sectorresponsibleformonitoringthe professionalafterpercutaneous exposure(committeeoflocal infection)
146 90.1
Profileofpatientswithahigher prevalenceofinfectiousdiseases (patientstreatedintraumahospitals)
117 72.2
PeriodicscreeningforM.tuberculosis
infection
03 1.8
Testedseroprevalencetoanti-HBs 95 58.6
Anesthesiologistpreviouslyvaccinated andresponsive,afterexposuretoa patientwithhepatitisB(prophylaxisis notrequired)
103 63.9
Professionalunresponsivetocomplete hepatitisBvaccinationprogram (repeatcompleteschedule)
101 62.3
ExposuretopatientwithhepatitisC(no prophylaxisavailable)
71 43.8
BiologicalfluidswithoutriskofHIV transmission
130 80.2
ElectivesurgeryinapatientwithTB 72 44.4
With regard to the consequences caused by excessive noise,95.6% answered satisfactorily andidentifiedloss of attention andirritability, elevation of blood pressureand releaseofcatecholaminesaspossibleevents.Contact der-matitis by irritation was identified correctly by 62.3% as the most common form of latex sensitivity presentation (Table2).
Astotherisksofinfection,only3.7%ofanaesthesiologists haveaccess/readtheirworkplacemanualofhospital infec-tioncontrol,58%correctlyclassifiedthesurgicalcenteras acriticalareaand90.1%wouldlookforthelocalinfection commission afterpercutaneous exposure. Withrespect to thosepatientswithhigherprevalenceofinfectiousdiseases, 72.2%ofthe anaesthesiologistschosecorrectly theoption ‘‘patientstreatedattraumahospitals’’(Table3).Only1.8% of anaesthesiologists included in this study had periodic screening for infection with Mycobacterium tuberculosis, and58.6%testedseroprevalenceofanti-HBsafter comple-tionofthevaccinationscheduleforhepatitisB(Table3).
Inthehypotheticalcase ofcontactofapreviously vac-cinatedandresponsiveanesthesiologistwithHBsAg-positive patients,63.9% of respondentschose correctly,answering thatthereisnoneedofpost-exposureprophylaxis.Incase ofnon-responsivenesstothecompletehepatitisB vaccina-tionprogram,62.3%agreedtoindicatearepetitionofthe fullthree-doseschedule.Byanalyzingthehypothetical situ-ationofcontaminationwithahepatitisCcarrier,only43.8% knewthataneffectivepost-exposureprophylaxisdoesnot exist(Table3).
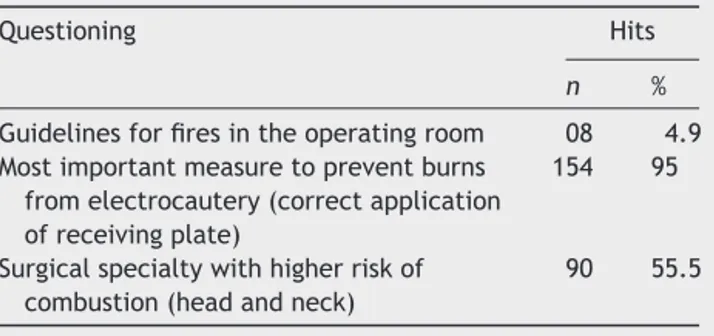
Table 4 Use of electrocautery and fire prevention and
hazards.
Questioning Hits
n %
Guidelinesforfiresintheoperatingroom 08 4.9 Mostimportantmeasuretopreventburns
fromelectrocautery(correctapplication ofreceivingplate)
154 95
Surgicalspecialtywithhigherriskof combustion(headandneck)
90 55.5
Astotheoccupationaltransmissionofhuman immunode-ficiency virus, 80.2% ofanaesthesiologists recognizedthat biological fluids pose norisk of infection. In thequestion about theright conduct inperformingan elective surgery in a patient with tuberculosis, less than half the sample (44.4%)correctlychosetopostponetheprocedureuntilthe patientwasnolongerinfectious(Table3).Regarding guide-linesforfiresintheoperatingroom,only4.9%saidthatthey had receivedsomekind of instructionin their workplaces (Table4).Regardingthepreventionofburnscausedby elec-trocautery,themajorityofrespondents(95%)recognized‘‘a correctapplicationofthereceivingplate’’asthemore rele-vantconduct.Whenaskedaboutthesurgicalspecialtymost likelytopromoteoxidizingreactions,55.5%chosecorrectly the‘‘headandneck’’(Table4)option.
Discussion
The study onthe potential risksin the operating room is partoftheanesthesiologisttraining.Knowledgeand preven-tionarethebasicstepstoreduceexposureanditspossible consequences.Thus,everyinstitutionmusthaveactive edu-cational programs on occupational hazards and develop appropriatetechniques topreventoccupational exposure, since failure tocomply with the standards of protection, orthesubmissiontounsafeworkingconditions,canleadto drasticconsequencesinhealthandqualityoflife.
The main professional responsible for ensuring proper workingconditionsandtheessentialmeanstoagood medi-calpractice,inhis/herworkofsupervisionandcoordination ofalltechnicalservicesofthehealthfacility,isthetechnical directoroftheinstitution.4Itwasobservedinourresearch
thatlessthanhalfoftheanaesthesiologistscovered(40.7%) knewpersonallytheprofessionalresponsiblefor this func-tion---afactorthatmayhindertheresolutionofunhealthy conditionsintheworkplace.
Theenvironmentalpollutionofsurgerycentersby anes-theticgasesisanotheraggravatingfactortothewelfareof healthprofessionals,withahighdegreeofrelationshipwith theanesthesiologist.Eveninroomswithproperventilation andequipmentcleaning,highconcentrationsofanesthetic gasesweredetected.1Only5.5%ofrespondentsstatedthat
The uncertainty about the true risks of this continued exposureoftenturnstheprofessionalintoaninsecure per-son,especiallyin thecase offemaleanaesthesiologistsin reproductiveage,astherearenostudies thatdefinitively establishdirectrelationsofthisexposurewithmiscarriage andcongenitalabnormalities.1Measuresshouldbetakento
minimizetheoccupationalexposuretochemicalagentswith knownor probabletoxicpotential.It iscrucialthat these professionalscontinuefightingforbetterequippedsurgical centers,withadequateventilationandexhaustsystemsas wellaswithgoodqualitymaintenanceschemes.
The noise levels in the operatingroom may also have adverse influence onthe abilityof theanesthesiologist to perform his/her tasks. Noise pollution should be quanti-fied andtheir intensity and number of hoursof exposure shouldbedetermined.1Thecomplexpsychomotoractivities
associatedwithanesthesia,suchasmonitoringand surveil-lance, areparticularly sensitive to the adverse affectsof noisepollution.Withregardtotheconsequencescausedby excessivenoise,95.6%answeredsatisfactorilyandidentified lossofattention,irritability,elevationofbloodpressureand releaseofcatecholaminesaspossibleevents.
The Committee onHospital InfectionControl wasborn with the mission of knowing the infection rates in hospi-tals,anditsprimaryresponsibilityistheimplementationof biosafetyactions.5 Everyhealthcare organizationoffers a
manual toinstructtheir professionals properly. Only 3.7% of respondents had access to or read the anaesthesiolo-gists’ manual of Committee onHospital Infection Control (CCIH)intheirinstitution.Consideringthatthe anaesthesi-ologists dealintimatelywithpotentialaggravating factors in the surgical center, the implementationof educational projectsiscrucialtofacilitatetheiraccesstothispreventive tool.
The concept of critical area, into which the surgi-cal center is encompassed, refers tothe sector in which thereisincreasedriskfor developmentof care-associated infections,eitherbyrunningprocessesinvolvingcritical arti-cles or biological material, by the realization of invasive proceduresorthepresenceofpatientswithincreased sus-ceptibilitytoinfectiousagentsorcarriersofmicroorganisms of epidemiological importance.6 Among the
anaesthesiol-ogists interviewed, 58% classified correctly the operating centerasacriticalarea.Withrespecttothepatientswith higherprevalence ofinfectious diseases, 72.2%of respon-dents selected the correct option, ‘‘patients treated at trauma hospitals’’. Measures should be implemented to ensure that all anaesthesiologists be aware of the classi-ficationoftheirworkingarea.
The exposure to potentially contaminated biological materialsisasignificantrisktothehealthprofessional. Stud-iesconducted in this arearevealthat accidents involving blood and other body fluids correspond to the most fre-quentlyreportedexposures.7
Injuries fromneedles and sharps, in general, are con-sideredextremelydangerous,forbeingpotentiallyableto convey more than 20 different types of pathogens. The infectiousagentscommonlyinvolvedarehuman immunode-ficiencyvirus(HIV)andhepatitisBandhepatitisCviruses.7
Inthesamplereviewedinthisstudy,only43.8%knewabout theinexistenceofaneffectiveprophylaxisafterexposureto hepatitisCvirus.Educationalactionsshouldbeencouraged
byhospitaladministrators,intendingthefullknowledgeof therisksencouragedbytheprofessionalsinvolved.
The hepatitis B vaccine is highly effective. Thus, all health professionals should have access to this resource. Anotherkey point is to test seroconversion to clarify the effectivenessof the method.In our survey,only 58.6% of respondentstestedseroconversion.Basedonthisresult,one shouldgivegreateremphasistotheintensificationof cam-paignsaimingtorepeatthevaccination schedulein those professionalswhohavenotresponded satisfactorilytothe method.
Highprevalencesoftuberculosisinfectionandincidences ofthisdiseaseamonghealthprofessionalsarereported,as wellashigherprevalencesandincidences inprofessionals performingactivitiesthatputthemincontactwithpatients withsuspectedordiagnosedtuberculosisintheworkplace.8
The Ministry of Health recommends the vaccination of healthcareprofessionals andof newly hired employees in theseservices,providedthattheyaretuberculinnegative.9
Inourstudy,only1.8%ofrespondentsunderwentscreening for M. tuberculosis infection. As that tuberculosis is an endemic disease in Brazil, the screening for tuberculosis shouldbeextendedtoallhealthprofessionals.
The anesthesiologistplaysa keyrolein theprevention offiresin theoperatingroom,recognizespossiblesources ofignitionandadministersoxygenrationally,especiallyin thecase ofopensystems.Thefirststeptofireprevention must be the constant reminder of the possibility of fire, which,despitebeinga rareevent,isa potentiallyserious complication.10 Only asmallportion of thesample (4.9%)
reportedreceivingguidelinesonthesubjectand55.5% cor-rectlyidentifiedthe‘‘headandneck’’specialtyasthatof highestriskforthiscomplication.
Infaceoftheseriousconsequencescaused by combus-tionin theoperatingroom,workshopsshouldbemounted toclarifyaspectsofitsprevention,thesurgicalspecialties mostinvolved,andwhatstepsmustbefollowedintheevent ofitsoccurrence.
Conclusion
Therisktowhichanaesthesiologistsareexposedisvariable andignored bythe classitself.This may resultin profes-sionalillness,withpersonalloss.Itwasobservedinthisstudy fromsomeofthequestionssubmittedthatlessthanhalfof thesampleansweredcorrectlyandaverysmallpercentage oftheevaluatedprofessionalsreadtheCCIHmanualoftheir institution.Theseresultsreinforcetheimportanceof edu-cationalcampaignsinordertoimprovetheknowledgeand alsotoclarifytherightsanddutiesoflaborinstitutions.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
Acknowledgement
References
1.BarashPG,CullenBF,StoeltingRK.Anestesiaclínica.Riscosna saladeoperac¸ões.4a
ed.SãoPaulo:EditoraManole;2004.p. 63---87.
2.PilauMM,BagatiniA,BondanLG,etal.Oanestesiologistano RioGrandedoSul.RevBrasAnestesiol.2000;50:309---16. 3.CalumbiRA,AmorimJA,MacielCMC,etal.Avaliac¸ãoda
quali-dadedevidadosanestesiologistasdacidadedoRecife.RevBras Anestesiol.2010;60:42---51.
4.http://www.bvsms.saude.gov.br/bvs/publicacoes/ cremerj37manual diretor tecnico.pdf
5.http://www.portaleducacao.com.br/arquivos/arquivossala/ media/objetodeaprendizagemfuncaodacomissaocontrole hospitalar.pdf
6.www4.anvisa.gov.br/base/visadoc/CP/CP[3631-1-0].PDF 7.http://bvsms.saude.gov.br/bvs/publicacoes/protocoloexpos
matbiologicos.pdf
8.http://www.cienciasdasaude.famerp.br/racsol/Vol-11-4/10% 20-%20id%2044.pdf
9.http://portal.saude.gov.br/portal/arquivos/pdf/manual tuberculose.pdf