JPediatr(RioJ).2014;90(6):542---555
www.jped.com.br
REVIEW
ARTICLE
Exacerbation
of
asthma
and
airway
infection:
is
the
virus
the
villain?
夽
,
夽夽
Lusmaia
D.C.
Costa
a,∗,
Paulo
Sucasas
Costa
a,
Paulo
A.M.
Camargos
baDepartmentofPediatrics,SchoolofMedicine,UniversidadeFederaldeGoiás(UFG),Goiânia,GO,Brazil
bDepartmentofPediatrics,SchoolofMedicine,UniversidadeFederaldeMinasGerais(UFMG),BeloHorizonte,MG,Brazil
Received24April2014;accepted1July2014 Availableonline26September2014
KEYWORDS
Asthma; Exacerbation; Virus; Child;
Respiratorytract infection
Abstract
Objective: Toreviewtheavailableliteratureontheassociationbetweenacuteviralrespiratory tractinfectionandtheonsetofasthmaexacerbations,identifyingthemostprevalentviruses, detectionmethods,aswellaspreventiveandtherapeuticaspects.
Sources: AsearchwasconductedinPubMed,Lilacs,andSciELOdatabases,betweentheyears 2002and2013,usingthefollowingdescriptors:asthmaexacerbation,virus,child,andacute respiratoryinfection.
Summaryofthefindings: Atotalof42originalarticlesaddressingtheidentificationof respi-ratoryvirusesduringepisodesofasthmaexacerbationwereselected,mostlycross-sectional studies.Therewasawidevariationinthemethodologyoftheassessedstudies,particularlyin relationtothechildren’sageandmethodsofcollectionandviraldetection.Theresultsindicate that,inupto92.2%ofexacerbations,aviralagentwaspotentiallythemaintriggeringfactor, andhumanrhinoviruswasthemostfrequentlyidentifiedfactor.Thepatternofviralcirculation mayhavebeenresponsiblefortheseasonalityofexacerbations.Theassociationbetweenviral infectionsandallergicinflammationappearstobecrucialfortheclinicalandfunctional uncon-trolledasthma,butfewstudieshaveevaluatedothertriggeringfactorsinassociationwithviral infection.
Conclusions: Respiratory viruses are present in the majority of asthmatic children during episodes of exacerbation. The involved physiopathological mechanismsare yet to be fully established,andthesynergismbetweenallergicinflammationandviralinfectionappearsto determineuncontrolleddisease.Theroleofothertriggeringandprotectiveagentsisyettobe clearlydetermined.
夽 Pleasecitethisarticleas:CostaLD,CostaPS,CamargosPA.Exacerbationofasthmaandairwayinfection:isthevirusthevillain?J
Pediatr(RioJ).2014;90:542---55.
夽夽
StudyconductedattheDepartmentofPediatrics,UniversidadeFederaldeGoiás(UFG),Goiânia,GO,Brazil.
∗Correspondingauthor.
E-mail:lusmaiapneumoped@gmail.com,lusmaiacosta@uol.com.br(L.D.C.Costa). http://dx.doi.org/10.1016/j.jped.2014.07.001
Exacerbationofasthmaandviralinfection 543
PALAVRAS-CHAVE
Asma; Exacerbac¸ão; Vírus; Crianc¸a;
Infecc¸ãodotrato respiratório
Exacerbac¸ãodaasmaeinfecc¸ãodasviasaéreas:ovíruséovilão?
Resumo
Objetivo: Reveraliteraturadisponívelsobrearelac¸ãoentreinfecc¸ãoviralagudadotrato respi-ratórioeodesencadeamentodeexacerbac¸õesdaasma,identificandoosvírusmaisprevalentes, osmétodosdedetecc¸ão,bemcomoosaspectospreventivoseterapêuticos.
Fontedosdados: FoirealizadaumabuscanasbasesdedadosPubMed,SciELOeLilacsutilizando osdescritores:asma,exacerbac¸ão,vírus,crianc¸aeinfecc¸ãorespiratóriaaguda,entreosanos de2002e2013.
Síntesedosdados: Foramselecionados42 artigosoriginaisquetratavamdaidentificac¸ãode vírusrespiratóriosduranteepisódiosdeexacerbac¸ãodaasma,emsuamaioriaestudos transver-sais.Houveamplavariac¸ãonametodologiadostrabalhosavaliados,principalmenteemrelac¸ão àidadedascrianc¸asemétodosdecoletaedetecc¸ãoviral.Osresultadosapontamque,ematé 92,2%dasexacerbac¸ões,umagenteviralfoipotencialmenteoprincipalfatordesencadeante, sendo o rinovírus humano o mais identificado. O padrão de circulac¸ão viral pode ter sido responsávelpelasazonalidadedasexacerbac¸ões.Aassociac¸ãoentreinfecc¸ãoviraleinflamac¸ão alérgicapareceserdeterminanteparalevaraodescontroleclínico-funcionaldaasma,porém poucosestudosavaliaramoutrosfatoresdesencadeantesemassociac¸ãocomainfecc¸ãoviral.
Conclusões: Osvírusrespiratóriosestãopresentesnamaioriadascrianc¸asasmáticasdurante os episódios de exacerbac¸ão. Os mecanismos fisiopatológicos envolvidos ainda não estão totalmenteestabelecidoseosinergismoentreainflamac¸ãoalérgicaeinfecc¸ãoviral parece determinarodescontroledadoenc¸a.Opapeldosoutrosagentesdesencadeanteseprotetores nãoestãoclaramentedeterminados.
©2014SociedadeBrasileiradePediatria.PublicadoporElsevierEditoraLtda.Todososdireitos reservados.
Introduction
Asthmaisachronic,genetically-determineddisease,whose prevalence in the pediatric population ranges between 19.0%and24.3%amongbrazilianadolescentsand schoolchil-dren,respectively.1Fromthephysiopathologicalviewpoint, it is characterized by chronic inflammation with the involvement of several cell types, associatedwith airway hyperresponsiveness, with episodes of reversible airflow limitation.Itisclinicallymanifestedbyrecurrent exacerba-tions,alsocalled‘‘asthmaattacks’’or,moreappropriately, acute asthma, characterized by progressive worsening of dyspnea,coughing,wheezing,chesttightness,ora combi-nationofthese.2
Thelossofclinicalandfunctionalasthmacontrolusually occursgradually,butitcanoccurabruptlyinasubgroupof patients.2Itisoneofthemaincausesofemergency consul-tations, having been responsible, in 2007, for 195 deaths inchildrenyoungerthan19yearsinBrazil.3Publicpolicies havebeendevelopedtopromotebothscientificknowledge aboutthediseaseanditsmanagement,aswellastoorganize assistanceprogramsinpublichealth,whichinclude,among others,thedispensingofmedications.However, exacerba-tionscontinuetorepresentasignificantnumberinstatistics, withgreatimpactonpublicandprivatehealthcaresystems.2 The multifactorialorigin of the clinical-functional lack of disease control is well known; since the early 1970s, respiratory viruseshave been associated withthe trigger-ing of asthma exacerbations in adults and children.3 In the1990s,thedevelopmentof moresensitive andspecific moleculartechniquesallowedfortheincreaseinrespiratory virus detectionandtherefore, waystobetter explainthis
association.Studiesusingreversetranscriptasepolymerase chainreaction(RT-PCR)asthedetectiontechnique,isolated orcombinedwithtraditionalmethods,observed positivity forrespiratoryviruses inupto92.2%ofepisodesofacute asthmaexacerbationinchildren.4
Considering the possibility of a causal relationship between respiratory virus infection and the triggering of asthma attacks in children, the implications of this asso-ciation,aswellasthepossibilityofspecificprophylaxisand therapyfortheseagents,specialattentiontothissubjectis justified.Therefore,thisliteraturereviewaimedtoanalyze articles,published between 2002 and 2013, assessing the association between asthma exacerbation and acuteviral airwayinfection.
Methods
544 CostaLDCetal.
Results
Respiratoryvirusesandimmuneresponse
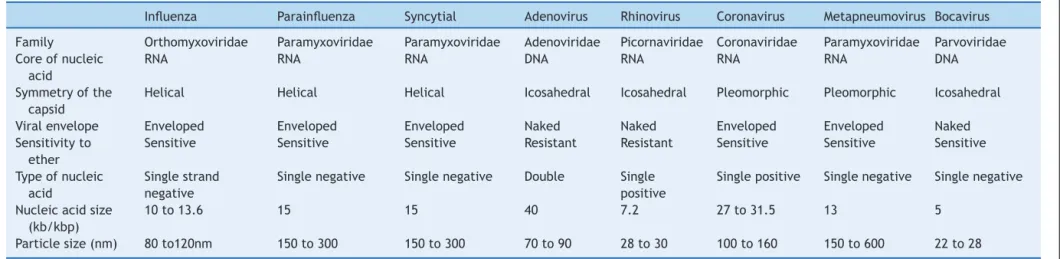
Themost frequentlyidentified respiratoryviruses in asso-ciation with asthma exacerbation were human rhinovirus (HRV),respiratorysyncytialvirus (RSV),humanadenovirus (hAdV),influenza(Flu),Parainfluenza(PFlu),human metap-neumovirus(hMPV),andhumancoronavirus(hCoV).Ofthe listed viruses, most have RNA as the nucleic acid; their biological characteristics and taxonomy5 are described in Table1.
The main transmission methods for these viruses are throughcontaminatedfomites,droplets,aerosols,ordirect contamination.Byinfectingthenasalepitheliumcells,these agentstriggeran immuneresponse,whichinvolvesmainly the dendritic cells and natural killer (NK) cells, inducing thereleaseofanumberofpro-inflammatorycytokinesand chemokinesbytheinfected epithelialcells, suchas inter-feron(IFN-1)andtumornecrosisfactoralpha(TNF␣),among others(Fig.1).
Inasthmapatients,theviralinfectioncauses an imbal-anceintheimmunehomeostasisoftherespiratorysystem. Several mechanisms related to viral infection and aller-gicinflammation, as well astheirrole in triggering acute asthma, have been proposed; among them, the deficient functionoftheepithelialbarriercausedbythevirus,which hasbeenimplicatedasapredisposingfactorbysome.6 How-ever,bothasthmaandatopyareassociatedwithepithelial damage,which maycontribute toincreasedsusceptibility toinfections, includingviraldiseases and sensitizationby aeroallergens.7 Another evaluatedfactor was mucus pro-ductionasanairwaydefensemechanism;inmicestudies,it wasdemonstratedthatallergicinflammationandviral infec-tionactsynergisticallyincreasingmucusproduction,which can lead to airway impaction and obstruction in asthma patients.8
Virus-inducedalterations in interferonproduction have also been observed. For instance, in vivo and in vitro
studiesin epithelial cells fromhealthy adultsand asthma patientsinfectedwithHRVdemonstratedadecreased pro-ductionoftypeIinterferon(␣and)inthelatter,making them more susceptible to infection associated with viral exacerbation.6,9Similarresultswereobtainedinstudies per-formed withchildren,where the productionof interferon andTh2cytokinesbybronchialepithelialcellswasassessed afterHRV-16infection.
Lowerinterferonproductionandhigherconcentrationsof viralRNAhavebeendemonstratedinchildrenwithasthma, regardlessoftheiratopicstatus,andinatopicchildren with-outasthma, suggestingthatanimpairedimmuneresponse to viral infection occurs not only in asthma patients, but in children with other disorders associated with Th2 lymphocytes.10 However, other studies failed to demon-stratethesamereductionininterferonproduction;others even found an increase in its production in exacerbated asthma.11,12
The bronchial epithelium produces some cytokines, including interleukin 25 and 33, as well as thymic stro-mallymphopoietin, which promotes thedifferentiation of innatelymphoidcells intoTh2.The lattercan beinduced byviralinfection, anditsproduction can beincreasedby
interleukin-4(IL-4),suggestingthattheinteractionbetween viruses andallergicairwayinflammationmayenhance the inflammatory Th2 response and potentially reduce the antiviralresponse.11,13
Collectionandviraldetectionmethods
Viral detection is highly dependent on the quality of the collectedsample,onthetimeofsymptomonsettothetime ofcollection(ideallywithin72hours),andontransportation andstorageof thesamplebeforetesting.The analysisfor respiratoryvirusesshouldbeperformedinmaterialfromthe airways.Upperairwaysecretionisusedinmostcases,and severalmethods areemployedfor thiscollection, suchas nasopharyngealaspirate(NPA),nasopharyngealswab(NPS), nasopharyngeallavage,andthecombinednasal-oralswab; thefirsttechniqueisconsideredthegoldstandard.14
Recently,newflockedswabs(Copan,Brescia,Italy)were developed,andpresentedbetterperformanceduringdata collection.Recentstudiesusingthistypeofswabpresented asensitivitycomparabletothatofNPAwhenthedetection isperformedbyPCR,suggestingthatthisswabcanbeused inepidemiologicalresearchandsurveillancestudies,dueto itsgreatertechnicalsimplicity.15,16
Therearefewdatatosupporttheuseofcombined oral-nasalswabsforvirus detection,anditssensitivityislower thanthatofthenasopharyngealswaboraspirate,whichcan beexplainedbythelowerviralloadintheoropharynxthan in thenasopharynx.The collectioncanalsobeperformed onmaterialfromthelowerairways,suchasinducedsputum andbronchiallavage.17
Themethodsfordetectionofrespiratoryvirusesare var-iedandincluderapidtestsfor antigendetection,culture, direct and indirectimmunofluorescence, and nucleic acid amplificationreactions, suchasRT-PCR,which candetect a singleagent (monoplex) or performmultiple detections (multiplex).Thesensitivityofthelatterishigher,anditwas usedinmostrecentstudies.18,19immunofluorescence reac-tionshave lowercost,arefaster toperform,andarealso abletodetectmultipleviruses.Apanelofsevenviruses(IFlu AandB,PFlu1to3,hAdV,andRSV)isgenerallyused.Some viruses, suchasHRV andBocavirus, canonly be detected throughnucleicacidamplificationreactions.17
Virusandexacerbation
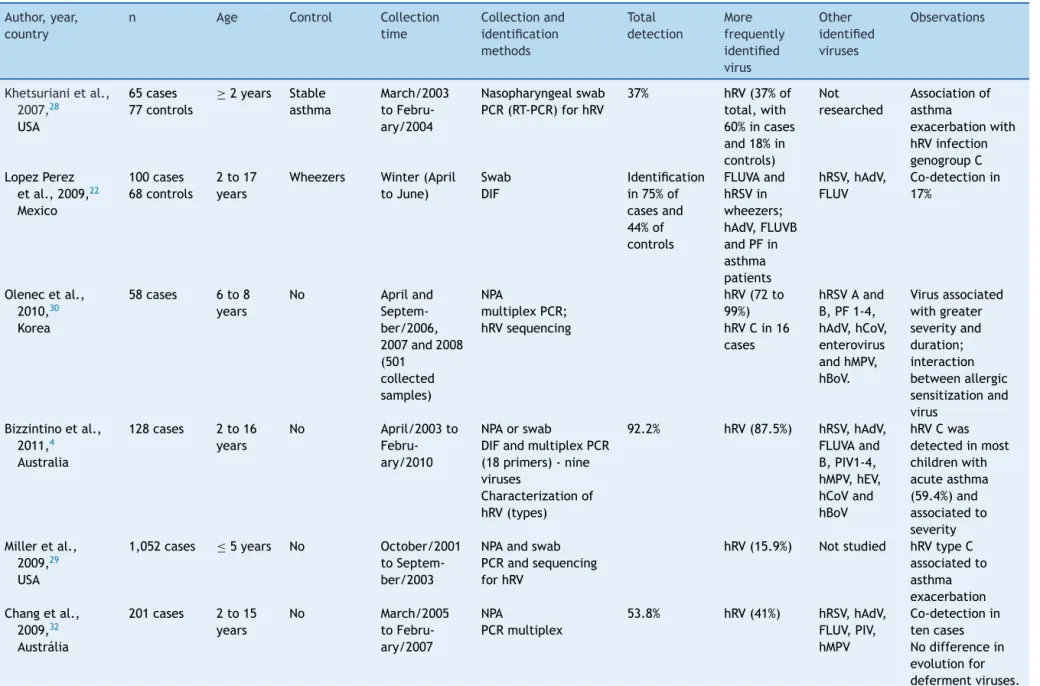
Several authors have performed studies aiming todetect viruses in respiratory secretions of exacerbated asthma patients, showinga prevalence of viralidentification that varies with several factors, such as patient age, time of the year, method of sample collection, and method of viraldetection. Table2 presentsthe originalarticles that demonstrateresultsofviraltestinginchildrenwith exacer-batedasthma.Moststudiesfoundprevalenceratesbetween 36.0%20and92.2%;5inthesecases,themostfrequently iden-tifiedviruswasHRV.
Exacerbation
of
asthma
and
viral
infection
545
Table1 Biologicalcharacteristicsandtaxonomyofthemajorrespiratoryviruses.
Influenza Parainfluenza Syncytial Adenovirus Rhinovirus Coronavirus Metapneumovirus Bocavirus Family Orthomyxoviridae Paramyxoviridae Paramyxoviridae Adenoviridae Picornaviridae Coronaviridae Paramyxoviridae Parvoviridae Coreofnucleic
acid
RNA RNA RNA DNA RNA RNA RNA DNA
Symmetryofthe capsid
Helical Helical Helical Icosahedral Icosahedral Pleomorphic Pleomorphic Icosahedral
Viralenvelope Enveloped Enveloped Enveloped Naked Naked Enveloped Enveloped Naked Sensitivityto
ether
Sensitive Sensitive Sensitive Resistant Resistant Sensitive Sensitive Sensitive
Typeofnucleic acid
Singlestrand negative
Singlenegative Singlenegative Double Single positive
Singlepositive Singlenegative Singlenegative
Nucleicacidsize (kb/kbp)
10to13.6 15 15 40 7.2 27to31.5 13 5
546
Costa
LDC
et
al.
Table2 Studiesthatinvestigatedviralinfectioninexacerbatedasthmaticchildrenincludedintheliteraturereview. Author,year,
country
n Age Control Collection time Collectionand identification methods Total detection More frequently identified virus Other identified viruses Observations
Khetsurianietal., 2007,28 USA
65cases 77controls
≥2years Stable
asthma
March/2003 to Febru-ary/2004
Nasopharyngealswab PCR(RT-PCR)forhRV
37% hRV(37%of
total,with 60%incases and18%in controls) Not researched Associationof asthma exacerbationwith hRVinfection genogroupC LopezPerez
etal.,2009,22 Mexico
100cases 68controls
2to17 years
Wheezers Winter(April toJune)
Swab DIF
Identification in75%of casesand 44%of controls FLUVAand hRSVin wheezers; hAdV,FLUVB andPFin asthma patients hRSV,hAdV, FLUV Co-detectionin 17%
Olenecetal., 2010,30 Korea
58cases 6to8 years
No Apriland
Septem-ber/2006, 2007and2008 (501 collected samples) NPA multiplexPCR; hRVsequencing
hRV(72to 99%) hRVCin16 cases
hRSVAand B,PF1-4, hAdV,hCoV, enterovirus andhMPV, hBoV. Virusassociated withgreater severityand duration; interaction betweenallergic sensitizationand virus
Bizzintinoetal., 2011,4 Australia
128cases 2to16 years
No April/2003to
Febru-ary/2010
NPAorswab
DIFandmultiplexPCR (18primers)-nine viruses
Characterizationof hRV(types)
92.2% hRV(87.5%) hRSV,hAdV, FLUVAand B,PIV1-4, hMPV,hEV, hCoVand hBoV
hRVCwas detectedinmost childrenwith acuteasthma (59.4%)and associatedto severity Milleretal.,
2009,29 USA
1,052cases ≤5years No October/2001
to Septem-ber/2003
NPAandswab PCRandsequencing forhRV
hRV(15.9%) Notstudied hRVtypeC associatedto asthma exacerbation Changetal.,
2009,32 Austrália
201cases 2to15 years No March/2005 to Febru-ary/2007 NPA PCRmultiplex
53.8% hRV(41%) hRSV,hAdV, FLUV,PIV, hMPV
Exacerbation of asthma and viral infection 547
Table2(Continued)
Author,year, country
n Age Control Collection time Collectionand identification methods Total detection More frequently identified virus Other identified viruses Observations
Ozcanetal., 2011,25 Turkey
104cases 31controls
3to17 yeras Stable Asthma patients 12months: Septem-ber/2009to Septem-ber/2010 Swab Real-timePCR
53.8% hRV(35.6%) FLUVAeB, PIV1-4, hCoV,hRSV, hRV,hMPV andhAdV Camaraetal.,
2004,43 Brazil
132cases 65controls
0to12 years Non-asthma patients October/1998 toJune/2000 NPA Immunofluorescence (IIF);cultureforhAdV andRT-PCRforhRV andhCoV
Cases(60.8%) Controls (13.3%)
RSVinthose youngerthan 2years hRVand hAdVin thoseolder than2years
hRSV,FLUV, PIV hAdV,hCoV
Therewasno association betweenvirus detectionand wheezing.Allergic sensitizationmore associatedwith exacerbation. Katoetal.,
2011,26 Japan 174cases 93controls Median 4.7years Stable Asthma patients Non-asthma patients November/2003 to October/2003 NPA
Kitdetectionof antigensand RT-PCR
79% hRV(33.9%) hRSV,hAdV, FLUVand PIV hEV
IL1,5,6,10and ECPwerehigherin exacerbationthan incontrols
Rawlinsonetal., 2003,19 Australia 179cases 79controls 1month to16 years Stable Asthma patients Non-asthma patients withURTI Winter,spring andsummer of2000to 2002
NPA
DIFPCRforhRVand hMPV
Cultureforvirus
hRV(50%in total:79%in casesand 17%in controls)
hAdV,FLUVA eB,hRSV, PIV3
Co-infectionwas common especiallyin winterandby hRSV
Fujitsukaetal., 2011,23 Japan 115 Mean 20.8 months No November/2007 to March/2009 Swab PCR
86.1% hRV(31.3%) hRSV,hAdV, PIV,FLUV, hMPV,hRV, hBoV,hEV
-Dawoodetal., 2011,27 USA 701asthma patientsin 2,165cases ofinfluenza
2to17 years
No 2003to2009 Swab
FLUVA,B,H1N1
- Only Influenza was screened Not screened
548
Costa
LDC
et
al.
Table2(Continued)
Author,year, country
n Age Control Collection time
Collectionand identification methods
Total detection
More frequently identified virus
Other identified viruses
Observations
Leungetal., 2010,31 China
209cases 77controls
3to18 years
Stable Asthma patients
12months January/2007 to Febru-ary/2008
NPAorswab multiplexPCR
51% hRV hRSV,hAdV,
PIV,FluV, hMPV,hRV, hBoV,hEV
Noagentwas correlatedwith severity
Thumerelleetal., 2003,24
France
82cases 27controls
2a16 years
Stable Asthma patients
9months October/1998 toJune/1999
Swab IIFandPCR
Asthma patients (45%)and controls (3.7%)
hRV(12%) FLUVAand B;PIV1-3; hAdV;RSV; hCoV Mycoplasma and chlamydia
Serology7.4% Atypical10%
Maffeyetal., 2010,21 Argentina
209cases 3months to16 years
No 12months
January/2006 to Decem-ber/2006
NPAorswab IIFandPCR
78% RSVandhRV hRSV,hAdV
PIV1-3, FLUVAeB) hEV,hMPV, hBoV, mycoplasma and chlamydia
Co-detectionin 20%,
Seasonal
circulation:three peaks:startof October(hRV); winter(hRSV)and spring(hSV,hRV andhMPV) Mandelcwajg
etal.,2010,20 France
232cases 107 controls
1.5to15 years
Exacerbated asthma patients Non-hospitalized
2005to2009 Novemberto March
NPA DIFandPCR
47% (hospi-talized) 31% (non-hospitalized)
hBoVand RSV
FLUVAand B,hAdV, PIV-3,hMPV
hRVnotscreened
Exacerbationofasthmaandviralinfection 549
Bronchial obstruction
Goblet cell hyperplasia
IL4 IL5 IL6 IL10 IL13 IL10 IL12 IL1
DC DC
TH2
Neutrophils: Eosinophils: Mast cells:
Penetration of allergens and irritants
Damage to bronchial epithelial cells
Release of mediators from bronchial epithelial cells
Recruited cells or those already present in the airways
Legend
Virus Chemokines CCL5 CCL10 CXCL8 Cytokines IFN1 TNFα IL6 IL25 IL33 TSLP
Allergen
Mucus lgE Inflammation
TSLP
Vasoactive amines; Platelet-activating factor; Arachidonic acid derivatives;
Cytokines; Granule proteins: ECP (eosinophil
cationic protein), EDN (eosinophil-derived neurotoxina) Leukotrienes and prostaglandins;
Cytokines; Chemokines. Cytokines;
Elastase; Myeloperoxidase;
Figure1 Immuneprocessinvolvedinresponsetorespiratoryvirusesandtheirassociationtoallergicinflammation.Respiratory virusesinfectbronchialepithelialcells(BECs)throughtool-likereceptors(TLRs).Duringreplication,theytriggeraninflammatory processwithinductionofcytokineandchemokineproductionbyBECs,amongtheminterferon(IFN-1),tumornecrosisfactoralpha (TNF-␣),interleukins(IL-33,IL-25),andthymicstromallymphopoietin(TSLP).Thedendriticcells(DCs),componentsoftheinnate immunity,aredirectedtosecondarylymphoidorgansaftercapturingviralantigens,wheretheystimulatethelymphoidcells,the protagonistsofthespecificimmune response.Inasthma patients,theproductionofIFNs isreduced,allowingfor greaterviral replicationandunderstimulationofTSLP,thereisadeviationfromlymphoidprofiletohelperTlymphocyte2(Th2),promoting lowerantiviralresponseandincreasedallergicinflammation,withbronchialhyperreactivityandincreasedproductionofmucus, causingbronchialobstructionandasthmaexacerbation.
of asthma was based on the criteria of Castro-Rodriguez for children younger than 3 years,and onthe Global Ini-tiative for Asthma (GINA) criteriafor thoseolder than 3. ImmunofluorescenceandPCR wereperformedin nasopha-ryngealsecretionsofthechildrenandshowedapositiverate of78.0%forvirusesingeneral;hRVandhRSVwerethemost frequently identified types. There wasalso 20.0% of dual detection,withtheinvolvementofallanalyzedviruses.21
In México, the frequency of the viral positivity at the immunofluorescence was higher in children with asthma (75.0%)thaninacontrolgroupofwheezingchildren with-outasthma(44.0%).hRVwasnotincludedinthatstudy,and IFlu, PFlu, and hAdV were the most frequently identified virus inthegroup ofasthma patients.22 InJapan, respira-tory viruses were detected by multiplex PCR in 86.1% of 115childrenwithexacerbatedasthma,withameanageof 20.8months.The hRSVwasrelatedtoasingleepisodeof wheezing(p<0.05).23hRVwasmorefrequentlyobservedin patientswithahistoryofasthma(p<0.05).
Agroupof82Frenchchildrenwithexacerbationtreated at home was compared to 27 stable asthmatic chil-dren. Immunofluorescence, PCR, and serology for viruses (MycoplasmapneumoniaeandChlamydophilapneumoniae) detectedapathogenin45.0%ofsamples,withsignificantly higher frequency in cases than in controls (3.7%). Viral detectiontestswerepositivein38%ofcases,andhRVwas
themostcommon(12.0%).In10.0%ofcases,theserologic testswerepositiveforbothatypicalpathogens.24
Anotherseriesof 104childrenwithexacerbation, com-paredto31stablechildren,wasstudiedbyTurkishauthors andshowedpositivityof53.8%inthecasesand22.6%in con-trols,throughRT-PCRreaction.hRVwasthemostcommonly foundvirusin35.6%ofthesamples.25InJapan,174children withacuteasthma were comparedto79 stableasthmatic childrenand14childrenwithoutasthma.Usinganantigen detectionkitandRT-PCR,respiratoryvirusesweredetected in79.0%ofnasalaspiratesamplesinexacerbatedasthmatic children,andhRVwasthemostcommon(33.9%).Inparallel, theassessment of inflammatorymarkers showed a signifi-cantelevation(p<0.01)ofinterleukinsIL-1,5,6,and10in serumandinthenasalaspiratesofpatientsinexacerbation, aswellasanincreaseinserumeosinophiliccationicprotein (ECP)levels(p<0.01).26
550 CostaLDCetal.
Another study compared exacerbated children treated inhospitals(n=232)withthosetreatedathome(n=107). Immunofluorescencefor Flu,hAdV,hRSV,andPIVwas per-formed,aswellasPCRforBocavirus.A36.0%rateofviral detection was obtained, but no difference was observed regarding the viral profile between inpatients and out-patients. The most frequently observed viruses were RSV (15.0%)andBocavirus(12.0%),buthRVwasnotincludedin theviralpanelofthisstudy.20
Agroupof179Australianchildrenagedupto16yearshad their nasalsecretions collectedin threeperiods between 2000and2002,andwerecomparedwithacontrolgroupof non-asthmaticchildrenwithupperrespiratorytract infec-tion (URTI) in the same period and another group of 28 children with controlled asthma, assessed during routine consultations.hRVandhMPVwerescreenedbyRT-PCRanda panelofsevenviruses(FLUV-AandB,PIV-1to3,hAdV,and hRSV) was studied by immunofluorescence. hRV infection accountedfor50.0%oftheURTIofnon-asthmaticchildren, and co-infection was common, especially with the hRSV, especiallyinchildrenyoungerthan2years.
Childrenwithsymptomaticasthmahadthehighestrates ofhRVinfection(79.0%vs.52.0%amongallchildren).Finally, childrenwithcontrolledasthmahadthelowestratesofhRV identification(17.0%vs.79.0%).19
Studiesconductedin200728and200929aimedtothe iden-tificationofhRVinexacerbatedasthmaticpatientsthrough RT-PCR, found an overall frequency of viral identification of 37.0% and 15.9%, respectively. The first study used a groupofcomparisonconsistingofstableasthmapatients,in whichtheidentificationratewaslower(18.0%)thaninthe casegroup(60.0%).Bothstudiesfoundagreaterassociation betweenexacerbationsandthepresenceofhRVC.
Virusandexacerbationseverity
Anotherimportantissueinthecomplexassociationbetween viruses and asthma is related to the intensity of the association of exacerbations with viral infection. In this sense,severalstudies4,30---34 presentedinconclusiveresults, although hRV was associated with increased severity or worse response to treatment.30,33,34 The association betweenviralinfectionandacuteasthmaseveritywas eval-uated in 128 children aged 2 to 16 years. A positivity rate of 92.2% for the presence of virus was observed by direct immunofluorescence (DIF) and multiplex PCR; hRV wasdetectedin 87.5%of cases,and typeCwasobserved inhalfthecasesandwasassociatedwithgreaterseverity.4 Fifty-eight asthmatic children aged 6 to 8 years were monitored for a period of five weeks between April and Septemberof2009.Theyhadnasallavagesamplescollected weeklyformultiplexPCRanalysis,inadditiontoasymptom diary,peakexpiratoryflow,andnotesonrescuemedication use.Aviruswasdetectedin36.0%to50.0%ofthespecimens; hRVwasidentifiedin72.0%to99.0%ofthepositivesamples, andwasassociatedwithgreatersymptomseverity.30
Nonetheless, viral testing by multiplex PCR for 20 pathogens in 209 children withexacerbated asthma com-pared with 77 controlled asthma patients, performed in Hong Kong between 2007 and 2008, showed no associa-tionbetween the presence of the virus and exacerbation
severity. One virus was identified in 51.0% of cases, and this detectionwas, in general,moreassociated with exa-cerbations(OR2.77;95%CI:1:51to5:11;p<0.01).When analyzedindividually,noviruswasassociatedwith exacer-bation,althoughhRVwasthemostfrequent,beingidentified in26.2%ofexacerbatedandin13.0%ofcontrolledasthma patients,butwithnosignificantdifference(p=0.27).31
Nasopharyngealaspiratesamplesof201asthmatic chil-drenagedbetween2and15yearscollectedduringepisodes ofexacerbationwerereferredforviralidentificationbyPCR. Thepositivityratewas53.8%;themostfrequentlyobserved werehRV (41.0%),followed byhRSV(9.0%).Therewasno associationwithexacerbationseverity.32
A study compared the response to treatment with bronchodilators between exacerbated children with viral respiratoryinfectionsymptoms(n=168)andagroup with-out suchsymptoms(n=50). The meanage was6.6years, and exacerbationseverity did not differbetween groups. Children withviral symptoms had poor response to bron-chodilators,requiringmoredosesofbeta-agonistsafter6, 12,and24hours.Theviralscreeningwasconductedin77.0% ofcases;hRVwasthemostfrequentlyfoundvirus(61.4%).33 Inanotherstudy,78exacerbatedchildrenweretreated at the hospitalandcompared to78asymptomatic adults. Multiplex PCR reactions for eight respiratory viruses and monoplexPCTforEnterovirus,hRV,andBocavirusdetected thepresence of respiratoryviruses in65.4% ofcases;hRV wasonceagainthemostfrequentlyobservedvirus(52.6%). Genotyping showed a higher frequency (56.0%) of type C hRV and association withtype A showed a worse clinical outcome.34
Seasonalityofexacerbations
Asthmaexacerbationshaveseasonaldistribution,occurring cyclicallyinbothadultsandchildren,andcanbeexplained by the viral circulation pattern or change in the level of pollutants andaeroallergens. Oneexampleis whatoccurs intemperatecountries,whereahigherrateofoccurrence ismore likelytobeobservedinthefallandspringamong schoolchildren.35Acombinationoffactorsmayexplainthis phenomenon, suchas increasedcirculation of hRV in late summerandearlyautumn,increasedcirculation of pollut-antsandaeroallergens, andthe returntoschoolafterthe summer vacations. The influence of the return to school activitiesmaybeexplainedbyloweradherenceto mainte-nancetreatmentduringthevacationperiod.Thecirculation of other viruses has been reported in other countries in the northern hemisphere,especially hRSVduring autumn-winter,Fluinwinter,PIV-1and2inthefall,andPIV-3in thespring.36,37
Exacerbationofasthmaandviralinfection 551
Fewpublisheddataregardingtheseasonalityof exacer-bationswerefound.Tomakeaparalleltoviruscirculation andtheoccurrenceofexacerbations,theauthorsanalyzed dataobtainedinsomestudies,suchasthestudyconducted intheFederalDistrict,whichobservedahigherfrequency inthemonthofMarch.39 StillintheMidwestregion,inthe stateofGoiás,anincreasedfrequencyofrespiratory symp-toms, not specified as asthma, wasobserved in winter.40 An observation regarding the distribution of the occur-renceof asthma in thestate of Minas Gerais alsoshowed higherconcentrationsinfall-winter,betweenMayandJuly,41 indicating a predominance of respiratory and/or asthma symptomsintheBrazilianfall-winterseasons.
Viralinfectionandallergicsensitization
Inadditiontotheseasonalvariationofthevirus,other fac-tors involved in the genesis of asthma exacerbation may explainthisvariation,suchasaeroallergensandpollutants, whichalsovarythroughoutthedifferentseasons.Itislikely thatthecombinationoftheseandotherfactorsresultinthe observedseasonalpeaksinexacerbations.Inthemonthof Apriloftheyears2006and2008,astudywasconductedin Koreaaimingtomonitorviralinfectionandtoidentify sen-sitizationtoaeroallergensin58childrenwithacuteasthma ordiagnosisofacold,whosemeanagewas6.5years. Chil-drenwithallergicsensitizationpresentedthesamenumber ofviralinfections,butwithmoresymptomsthanthose non-sensitized.30
Inanotherstudy,conductedinManchester,England, 84 children hospitalized for exacerbation were compared to children with stableasthma and children hospitalized for non-respiratory disease. The authors concluded that the association between viralinfection and allergenexposure increasedtheriskofhospitaladmissionby19.4-fold.42
In Brazil,Camara etal.43 investigatedthe roleof viral infections,sensitization,andexposure toaeroallergensas riskfactorsforwheezinginchildrenagedupto12years.In thoseyoungerthan2years,thefrequencyofviralpositivity was significantly higher in cases (60.8%) than in controls (13.3%).In older children,therewasnosignificant differ-ence:69.7%ofcasesand43.4%ofthepositivecontrols.They concludedthat in children younger than2 years, therisk factorsassociatedwithwheezingwereviralinfectionanda familyhistoryofatopy;amongolderchildren,sensitization toinhalantallergenswasthemostimportanteventforthe onsetofcrises.
Pollutantsandaeroallergens
The effect of air pollutants is usually disregarded in the presenceofvirusesorallergens.However,thereisevidence thatacuteexposuretospecificpollutantsmaycontributeto thesymptomsandseverityofexacerbations.Forinstance, cigarettesmokeinducesamodelofnon-eosinophilic inflam-mationwithrelativeresistancetocorticosteroids.44Passive smokingis quitecommon inhomesof asthmaticchildren, causinganegativeimpactondiseasecontrol.InScotland, the 2006legislation that bannedsmokingin public places reducedhospitalizationsforasthmaby18.2%.45
Other pollutants appear to contribute to asthma exa-cerbations,suchasthoseresultingfromthecombustionof naturalgasandengineoil,suchasnitrogen dioxide(NO2). Childrenspendmostoftheirtimeoutsideandbreatheina greateramountofpollutants perkilogramofweightwhen comparedto adults, and the increased levels of NO2 are associatedwiththeseverityofvirus-inducedexacerbations. Thisemphasizesa potentialsynergismbetween thesetwo inflammatorystimuli.44
Moreover,controlledexposureinasthmapatients demon-stratedthatNO2increasestheresponsetoinhaledallergens. Acohortof114asthmaticchildrenagedbetween8and11 yearsweremonitoredforsymptoms,measurementofpeak expiratoryflow,measurementofexposuretoNO2,and pres-enceofvirusinnasalsecretionduringaperiodof13months. Oneormorevirusesweredetectedin78%ofthereported episodesofrespiratorysymptoms;itwasdemonstratedthat exposuretohighconcentrationsofNO2intheweekbefore theonsetofaviralrespiratoryinfectionwasrelatedtothe exacerbationseverity.46
AlongitudinalstudyconductedintheUnitedStates mea-suredexposure tocigarette smoke in 1,444 children with asthmaandNO2 inasubset of663ofthem,over aperiod ofninemonths.Theydemonstratedincreasedsymptomsin thoseexposedtoNO2,butonlyamongnon-atopicchildren, witha relativeriskof 1.8(95% CI:1.1to2.8).There was noassociation betweensymptomsandincreasedcigarette smoke exposure.47 Two cross-sectional studies compared childrenexposedtodifferentlevelsofcigarettesmokeand showedthatthoseexposedtohighlevelshadhigher symp-tom scores (p<0.01), nocturnal symptoms (OR 3.4; 95% CI:1.3 to 8.8), and need for relief(p=0.03) and control (p=0.02)medications.48
A study in which 937 children agedbetween 5 and 11 yearswererandomizedtointerventionwithenvironmental educationguidelinesaimedat reducing exposure,showed areductioninexposureinthegroupthatreceived instruc-tionsforaperiodof14months.Theinterventiongrouphad fewerdayswithsymptoms(p<0.01)afteroneyearof follow-up,in addition toa decrease in the levels of dust mites (Dermatophagoides pteronyssinus and Dermatophagoides farinae)andcockroachantigensinthehomeenvironment.49 Fungalsensitizationisprevalentinchildrenwithasthma, althoughfewstudieshaveaddressedthisissue,comparedto studiesrelatedtodustmites.Onestudydemonstratedthat childrenwithapositiveskintestforfungihadmoredaysof symptomswhencomparedtothosewithnegativetests(6.3
vs.5.7 for twoweeks, p=0.04). Duringthe study period, fungiweregrownfromtheintra-andextra-domestic envi-ronment;increasedexposure tofungiwasassociatedwith increaseddaysofsymptomsandunscheduledphysicianvisits forasthma.44
Preventiveandtherapeuticaspects
552 CostaLDCetal.
thealterationsthatareusuallyfoundinpatientsduring asth-maticcrises,suchashyperinsufflation,fluidextravasation, andatelectasisassociatedwithhypoxemia,51 the misinter-pretationofthesefindingsasasignofpneumoniaiscommon and,consequently,unnecessaryprescriptionofantibiotics.
Amulticenterstudyof734asthmaticpatientstreatedin emergencyroomsevaluatedtherequestforadditionaltests, inthiscase,chestradiographyandbloodtests.Severelyill patients,thoseunder1year,andthosewithacomorbidity wereexcluded.Atotalof 302(41.0%)children underwent additionaltests,suchaschestradiography(27.0%)andblood tests(14.0%). Afterexcluding febrileor hypoxicpatients, 32.0%werestillsubjectedtoat leastoneoftheexams.50 DespitethelackofBraziliandata,theroutineofpediatric emergencycare servicesinthecountryappearstoadhere tothisrule.
Inordertopreventthedisseminationofviralagents,due tothe high capacity of viralspread through dropletsand fomites,handwashing,andtheuseofrespiratorymasksare simplestrategiesthathavebeenproven tobeeffective.52 Stayingawayfromsituationsthat favorclustersofpeople duringperiodsof increasedviralcirculationhasbeen rec-ommended,althoughtherearenostudiesthatprovedthe effectivenessofthisstrategy.52,53Theuseofsubstancessuch asherbal preparations includingEchinacea and vitamin C hasbeen evaluated, but double-blind, placebo-controlled studiesfailedtodemonstratetheirbenefit.54
The preventionof viralinfectionsthroughvaccineshas beenthemosteffectivewaytocontroldiseasescausedby viruses.Inthecaseofrespiratoryviruses,theonlyvaccine availableisforFlu,although thereareongoing studiesfor thedevelopmentofvaccinesfor otherrespiratoryviruses, especiallyHRV.However,theirgreatantigenicdiversity hin-dersresearchsuccess;recentstudieshavetriedtoestablish amoreadequateantigenictargetintheviralstructure.54,55 SpecificRSVimmunoglobulinhasbeensuccessfullyusedin reducing hospitalizations for viral bronchiolitis, and new perspectivesforthe treatment ofexacerbations triggered byviralinfections have emergedfromstudies directedto syntheticagonistsofTLR3receptor,IFN-agonist,and IL33-andIL25-antagonists,amongothers.56,57
There is no specific treatment for most respiratory viruses.Someantiviralshave beensuccessfullyused,asin thecaseofFluinfection,suchasamantadine,rimantadine, oseltamivirphosphate,andzanamivir;thelatterisnot indi-catedforpatientswithasthma.Ribavirinisindicatedforthe treatmentofsevereinfectionscausedbyRSV.Other antivi-ralagentsarebeingstudiedandhavenotyetbeenapproved forclinicaluse,suchaspleconaril,vapendavir,pirodavir,and rupintrivir.54
Glucocorticoids have potent anti-inflammatory effects andhavebeensuccessfullyusedinmaintenancetreatment inpatientswithpersistentasthma,controllinginflammation andpreventingexacerbations.Somestudieshaveassessed its effect on virus-induced asthma. The suppression of thereleaseofpro-inflammatorymediatorsinducedbyHRV infectioninvitroinbronchialepithelialcells,suchasCCL5, CCL10, CXCL8, and IL6, as well as the reduction of fac-tors associated with remodeling, was achieved after the use of budesonide.58 Other in vitro studies documented theactionofothercorticosteroidsaloneorincombination withbronchodilatorsorleukotrieneantagonistsinreducing
thereleaseofseveralinflammatorymolecules,with poten-tialmodulationofthedeleteriouseffectsofvirusesonthe asthmatic population.51,59 Despite the proven benefits of inhaled corticosteroids in the control ofasthma triggered by multiple factors, theiraction onvirus-induced exacer-bations is unclear. The use of low-to-moderate doses of inhaledcorticosteroidsasmaintenancetherapycannot pre-ventintermittentviral-inducedwheezing.60,61
However, better results have been obtained with the intermittentuseofinhaledcorticosteroidsathighdoses.62
Discussion
The use of viral detection techniques with high sensitiv-ityandspecificityhasincreasedtheidentification ofsome respiratory viruses in children with asthma exacerbation. The direct or indirect immunofluorescence reactions still havegreatpracticalimportance,astheycandetectapanel ofsevenviruses(FLUV-AandB,PIV-1-3,hAdVandhRSV), beinganaffordableandfastmethod,withgoodsensitivity, especiallyinchildren.18ItiscurrentlyusedbytheBrazilian Ministry of Healthfor the screening of respiratory viruses inthediagnosisofsevereacuteflu-likeillnessandFlu-like illnessinsentinelunits.
The techniques for nucleic acid amplification (RT-PCR) are more expensive, but more sensitive; thus, they are usedinresearchandbytheBrazilianMinistryofHealthfor theidentificationandgenotypingof Flu.38 Furthermore,it allowsfortheidentificationofsomeviruseswithsignificant clinical and epidemiological importance, suchas hRV and
Bocavirus,notidentifiedbyimmunofluorescence.17,54 Asforthemethodusedtoobtainthesample,itisworth mentioningthecontroversialissueofnasopharyngealswab in viral research. Although its use has been consolidated for bacterialinfections (S.pneumoniaeandS.aureus),its role in viral infections still deserves some consideration. The authors agreethat, fromthe practical point of view, itismorefeasible, eliminatingtheuseofsuctionsystems, probes, andmorespecialized training,whencomparedto aspirateorlavagesamples.However,onlythosewithmore advanced technology (flocked swab), which providesbest capture and release of cells and, therefore, of thevirus, areequivalenttothe aspirateinterms of sample quality. Nevertheless,thisswabisnotroutinelyusedinservicesand researchesinBrazil.38
Exacerbationofasthmaandviralinfection 553
variationregardingthedetectionmethodsandinrelationto someoutcomes.
Inadditiontothedifferencesinsample collections,all these studies were cross-sectional, which does not allow fortheestablishmentofacause-effectassociationbetween viralinfectionand theonsetof exacerbation,butsuggest suchan association. In relationtoother factors knownto beassociatedwithuncontrolledasthma, suchasallergens andirritants,moststudies didnotinclude thesevariables in the evaluation.When theinflammatory process typical of asthma is associated witha viralrespiratory infection, thereisatendencytogreaterseverityandduration,aswell asapoorerresponsetoconventionaltreatmentoftheacute episode.32,33Theinvolvedmechanismsstillneedtobefully elucidated,evidencingthesynergisticeffectbetweenviral infectionandallergicairwayinflammationinthe pathogen-esisofexacerbations.30,43
Another pertinent issue is the role of inhaled cortico-steroids in attenuating the inflammation triggered by the virus, also seldom mentioned in these studies. Its action in thecontrol and reductionof morbidity associatedwith asthma is well established,2 but it is still a controversial subject regarding the prevention of viral-induced wheez-ing.Itseffectivenessintheinflammatoryprocesstriggered byavirushasbeendemonstratedininvitrostudies,51,58,59 butstudiesevaluatingitsclinicalbenefithaveyettoreach conclusiveresults.61,62
Regardlessofthedirectionofvirus-allergeninteraction, thepresentfindingsstronglysuggestthatanadequate strat-egytopreventvirus-inducedexacerbationsshouldfocuson twocourses,namelytheimprovementofantiviralresponse andthereductionofallergicsensitizationorinflammation. The lattercanbeachievedwithappropriatetreatmentof theasthmapatientatriskwithmedicationsthatreduce air-wayinflammation.Conversely,thepreventivemeasuresfor viralinfectionacquisitionanditstimelydiagnosisallowfor a proper managementof exacerbations, and reductionof thenumberofhospitalizations andunnecessaryadditional tests,especiallyinchildrenwhoarefebrileatthetimeof assessment.
The association between viral infection and asthma in childhood still has several points that need clarification, especiallytheactualroleofvirusesintriggering exacerba-tionsandthatofinhaledcorticosteroidsinitsattenuation.
Funding
Fundac¸ão de Amparo à Pesquisa do Estado de Goiás (N◦
20120267001128).
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
Acknowledgements
To the Laboratory of Virology of the Instituto de Patolo-giaTropicaleSaúdePúblicaoftheUniversidadeFederalde Goiás.
References
1.SoléD,WandalsenGF,Camelo-NunesIC,NaspitzCK.Prevalência desintomasdeasma,riniteeeczemaatópicoentrecrianc¸ase adolescentesbrasileirosidentificadospeloInternationalStudy of Asthma and Allergies (ISAAC): fase 3. J Pediatr (Rio J). 2006;82:341---6.
2.Global Strategy for Asthma Management and Prevention. Global Initiative for Asthma (GINA) 2012. Available from: http://www.ginasthma.org/
3.GreggI,HornM,BrainE,InglisJM,YeallandSJ.Proceedings: Theroleofviralinfectioninasthmaandbronchitis.Tubercle. 1975;56:171.
4.BizzintinoJ,LeeWM,LaingIA,VangF,PappasT,ZhangG,etal. AssociationbetweenhumanrhinovirusCandseverityofacute asthmainchildren.EurRespirJ.2011;37:1037---42.
5.ButelJS.Virologia.In:BrooksGF,CarrollKC,ButelJS,Morse SA,MietznerTA,editors.MicrobiologiamédicadeJawetz, Mel-nickeAdelberg.25th ed.PortoAlegre:McGraw-Hill;2010.p. 373---93.
6.Contoli M,Message S,Laza-Stanca V, Edwards MR,Wark PA, Bartlett NW, et al. Role of deficient type III interferon-lambdaproductioninasthmaexacerbations.NatMed.2006;12: 1023---6.
7.Holgate ST. Epitheliumdysfunctionin asthma.J Allergy Clin Immunol.2007;120:1233---44.
8.HashimotoK, GrahamBS,HoSB,Adler KB,CollinsRD,Olson SJ,etal.Respiratorysyncytialvirusinallergiclung inflamma-tionincreasesMuc5acandGob-5.AmJRespirCritCareMed. 2004;170:306---12.
9.PapadopoulosNG,ChristodoulouI,RohdeG,AgacheI,Almqvist C, Bruno A, et al. Viruses and bacteria in acute asthma exacerbations–a GA(2) LEN-DARE systematic review. Allergy. 2011;66:458---68.
10.BaraldoS,ContoliM,BazzanE,TuratoG,PadovaniA,Marku B, et al. Deficient antiviral immuneresponses in childhood: distinct roles of atopy and asthma. J Allergy Clin Immunol. 2012;130:1307---14.
11.Gavala M, Bashir H, Gern J. Virus/allergen interactions in asthma.CurrAllergyAsthmaRep.2013;13:298---307.
12.HoltP,SlyP.Interactionbetweenadaptiveandinnateimmune pathwaysinthepathogenesisofatopicasthma:operationofa lung/bonemarrowaxis.Chest.2011;139:1165---71.
13.HamsE,FallonPG.Innatetype2cellsandasthma.CurrOpin Pharmacol.2012;12:503---9.
14.ChanKH,PeirisJS,LimW,NichollsJM,ChiuSS.Comparisonof nasopharyngealflockedswabsandaspiratesforrapiddiagnosis ofrespiratoryvirusesinchildren.JClinVirol.2008;42:65---9. 15.SungRYT,ChanPKS,ChoiKC,YeungAC,LiAM,TangJW,etal.
Comparativestudyofnasopharyngealaspirateandnasalswab specimensfordiagnosisofacuteviralrespiratoryinfection.J ClinMicrobiol.2008;46:3073---6.
16.BlaschkeAJ,AllisonMA,MeyersL,RogatchevaM,HeyrendC, MallinB,etal.Non-invasivesamplecollectionforrespiratory virustestingbymultiplexPCR.JClinVirol.2011;52:210---4. 17.GinocchioCC,McAdamAJ.Currentbestpracticesfor
respira-toryvirustesting.JClinMicrobiol.2011;49:S44---8.
18.SheRC,PolageCR,CaramLB,TaggartEW,HymasWC,Woods CW, et al. Performance of diagnostic tests to detect respi-ratory viruses in older adults. Diagn Microbiol Infect Dis. 2010;67:246---50.
19.RawlinsonWD,WaliuzzamanZ,CarterIW,BelessisYC,Gilbert KM,Morton JR. Asthma exacerbationsin childrenassociated withRhinovirusbutnothumanmetapneumovirusinfection.J InfectDis.2003;187:1314---8.
554 CostaLDCetal.
21.Maffey AF, Barrero PR, Venialgo C, Fernández F, Fuse VA, Saia M, et al. Virusesand atypicalbacteria associated with asthma exacerbations in hospitalized children. Pediatr Pul-monol.2010;45:619---25.
22.Lopez Perez G, Morfin Maciel BM, Navarrete N, Aguirre A. Identificationofinfluenza,parainfluenza,adenovirusand respi-ratory syncytial virus during rhinopharyngitis in a group of Mexican childrenwithasthmaand wheezing. RevAlergMex. 2009;56:86---91.
23.Fujitsuka A, Tsukagoshi H,Arakawa M, Goto-SugaiK, Ryo A, OkayamaY,etal.Amolecularepidemiologicalstudyof respira-toryvirusesdetectedinJapanesechildrenwithacutewheezing illness.BMCInfectDis.2011;11:168.
24.ThumerelleC,DeschildreA,BouquillonC,SantosC,SardetA, ScalbertM,etal.Roleofvirusesandatypicalbacteriain exacer-bationsofasthmainhospitalizedchildren:aprospectivestudy inthe Nord-PasdeCalais region(France). PediatrPulmonol. 2003;35:75---82.
25.OzcanC,ToyranM,CivelekE,Erkoc¸o˘gluM,Altas¸AB,AlbayrakN, etal.Evaluationofrespiratoryviralpathogensinacuteasthma exacerbationsduringchildhood.JAsthma.2011;48:888---93. 26.Kato M, Tsukagoshi H, Yoshizumi M, Saitoh M, Kozawa K,
YamadaY,etal.Differentcytokineprofileandeosinophil acti-vationare involvedinrhinovirus-and RSvirus-inducedacute exacerbationofchildhoodwheezing.PediatrAllergyImmunol. 2011;22:e87---94.
27.DawoodFS,KamimotoL,D’MelloTA,ReingoldA,GershmanK, Meek J, et al. Children with asthmahospitalized with sea-sonalorpandemicInfluenza,2003-2009.Pediatrics.2011;128: e27---32.
28.Khetsuriani N, Kazerouni NN, Erdman DD, Lu X, Redd SC, AndersonLJ,etal.Prevalenceofviralrespiratorytract infec-tionsinchildrenwithasthma.JAllergyClinImmunol.2007;119: 314---21.
29.MillerEK,EdwardsKM,WeinbergGA,IwaneMK,GriffinMR,Hall CB,etal.Anovelgroupofrhinovirusesisassociatedwithasthma hospitalizations.JAllergyClinImmunol.2009;123:98---1040. 30.OlenecJP, KimWK,LeeW-M,VangF,PappasTE,SalazarLE,
etal.Weeklymonitoringofchildrenwithasthmaforinfections andillnessduringcommoncoldseasons.JAllergyClinImmunol. 2010;125:1001---6,e1.
31.Leung TF, To MY, Yeung ACM, Wong YS, Wong GWK, Chan PKS. Multiplex molecular detection of respiratory pathogens in children with asthma exacerbation. Chest. 2010;137: 348---54.
32.Chang AB, Clark R, Acworth JP, Petsky HL, Sloots TP. The impactofviralrespiratoryinfectionontheseverityand recov-eryfromanasthmaexacerbation.PediatrInfectDisJ.2009;28: 290---4.
33.RueterK,BizzintinoJ,MartinAC,ZhangG,HaydenCM, Geel-hoedGC,etal.Symptomaticviralinfectionisassociatedwith impairedresponsetotreatmentinchildrenwithacuteasthma. JPediatr.2012;160:82---7.
34.ArdenKE,ChangAB,LambertSB,NissenMD,SlootsTP,Mackay IM.Newlyidentifiedrespiratoryvirusesinchildrenwithasthma exacerbationnotrequiringadmissiontohospital.JMedVirol. 2010;82:1458---61.
35.SearsMR,JohnstonNW.UnderstandingtheSeptemberasthma epidemic.JAllergyClinImmunol.2007;120:526---9.
36.LitwinCM,BosleyJG.Seasonalityandprevalenceofrespiratory pathogensdetectedbymultiplexPCRatatertiarycaremedical center.ArchVirol.2014:65---72.
37.Johnston SL. Innate immunity in the pathogenesis of virus-induced asthma exacerbations. Proc Am Thorac Soc. 2007;4:267---70.
38.de Mello Freitas FT. Sentinel surveillance of influenza and otherrespiratoryviruses,Brazil,2000-2010.BrazJInfectDis. 2013;17:62---8.
39.Valenc¸a LM, Restivo PCN, Nunes MS. Variac¸ão sazonal nos atendimentosdeemergênciaporasmaemGama.BrasilJBras Pneumol.2006;32:284---9.
40.SilvaJuniorJL,PadilhaTF,RezendeJE,RabeloEC,FerreiraAC, RabahiMF.Effectofseasonalityontheoccurrenceofrespiratory symptoms ina Braziliancity witha tropical climate.JBras Pneumol.2011;37:759---67.
41.EzequielOdaS,GazetaGS,FreireNM.Prevalênciados atendi-mentosporcrisesdeasmanosservic¸ospúblicosdoMunicípio deJuizdeFora(MG).JBrasPneumol.2007;33:20---7.
42.MurrayCS,PolettiG,KebadzeT,MorrisJ,WoodcockA,Johnston SL,etal.Studyofmodifiableriskfactorsforasthma exacerba-tions:virus infectionandallergenexposureincreasetherisk of asthmahospital admissions in children. Thorax. 2006;61: 376---82.
43.Camara AA, Silva JM, Ferriani VPL, Tobias KR, Macedo IS, PadovaniMA,etal.Riskfactorsforwheezinginasubtropical environment:Roleofrespiratoryvirusesandallergen sensitiza-tion.JAllergyClinImmunol.2004;113:551---7.
44.Dick S, Doust E, Cowie H, Ayres JG, Turner S. Associations betweenenvironmentalexposuresandasthmacontroland exa-cerbationsinyoungchildren:asystematicreview.BMJopen. 2014;4:e003827.
45.MackayD,HawS,AyresJG,FischbacherC,PellJP.Smoke-free legislationandhospitalizationsforchildhoodasthma.NEnglJ Med.2010;363:1139---45.
46.Chauhan AJ, Inskip HM, Linaker CH, Smith S, Schreiber J, JohnstonSL,etal.Personalexposuretonitrogendioxide(NO2) andtheseverityofvirus-inducedasthmainchildren.Lancet. 2003;361:1939---44.
47.Kattan M, Gergen PJ, Eggleston P,Visness CM, Mitchell HE. Health effects of indoornitrogen dioxide and passive smok-ing on urban asthmatic children. J Allergy Clin Immunol. 2007;20:618---24.
48.Morkjaroenpong V, Rand CS, Butz AM, Huss K, Eggleston P, MalveauxFJ,etal.Environmentaltobaccosmokeexposureand nocturnalsymptomsamonginner-citychildrenwithasthma.J AllergyClinImmunol.2002;110:147---53.
49.Morgan WJ, CrainEF, Gruchalla RS, O’Connor GT, Kattan M, Evans R 3rd, et al. Results of a home-based environmental interventionamongurbanchildrenwithasthma.NEnglJMed. 2004;351:1068---80.
50.GentileNT,UfbergJ,BarnumM,McHughM,KarrasD.Guidelines reduceX-rayandbloodgasutilizationinacuteasthma.AmJ EmergMed.2003;21:451---3.
51.MatsukuraS,KurokawaM,HommaT,WatanabeS,SuzukiS,Ieki K,etal.BasicResearchonvirus-inducedasthmaexacerbation: inhibitionofinflammatorychemokineexpressionbyfluticasone propionate.IntArchAllergyImmunol.2013;161:84---92. 52.AhanchianH,JonesC,ChenY-s,SlyP.Respiratoryviral
infec-tions in children with asthma: do they matter and can we preventthem?BMCPediatr.2012;12:147.
53.WeedonKM,RuppAH,HeffronAC,KellySF,ZhengX,Shulman ST,etal.Theimpactofinfectioncontroluponhospital-acquired influenzaand respiratory syncytialvirus. ScandJ Infect Dis. 2013;45:297---303.
54.JacobsSE,LamsonDM,KirstenS,WalshTJ.Humanrhinoviruses. ClinMicrobiolRev.2013;26:135---62.
55.PapiA,ContoliM.Rhinovirusvaccination:thecaseagainst.Eur RespirJ.2011;37:5---7.
56.JacksonDJ,SykesA,MalliaP,JohnstonSL.Asthma exacerba-tions:origin,effect,andprevention.JAllergyClinImmunol. 2011;128:1165---74.
57.ChristopherME,WongJP.Useoftoll-likereceptor3 agonists against respiratory viral infections. Antiinflamm Antiallergy AgentsMedChem.2011;10:327---38.
Exacerbationofasthmaandviralinfection 555
inflammatory mediator production by bronchial epithelial cells infected with rhinovirus. Clin Exp Allergy. 2009;39: 1700---10.
59.BochkovY,BusseW,Brockman-SchneiderR,EvansMD,Jarjour NN,McCraeC,etal.Budesonideandformoteroleffectson rhi-novirusreplicationandepithelialcellcytokineresponses.Respir Res.2013;14:98.
60.AlvarezAE,MarsonFAL,BertuzzoCS,ArnsCW,RibeiroJD. Epi-demiologicaland genetic characteristicsassociated withthe
severity of acute viral bronchiolitis by respiratory syncytial virus.JPediatr(RioJ).2013;89:531---43.
61.WilsonN,SloperK,SilvermanM.Effectofcontinuoustreatment withtopicalcorticosteroidonepisodicviralwheezeinpreschool children.ArchDisChild.1995;72:317---20.