revbrashematolhemoter.2017;39(4):354–356
w w w . r b h h . o r g
Revista
Brasileira
de
Hematologia
e
Hemoterapia
Brazilian
Journal
of
Hematology
and
Hemotherapy
Case
Report
Recurrent
thromboembolism
after
splenectomy
in
a
patient
with
complex
hemoglobin
disease:
a
case
report
Laura
Maria
Silva
Thiersch
a,
André
Rolim
Belisario
b,
Suely
Meireles
Rezende
a,∗aUniversidadeFederaldeMinasGerais(UFMG),BeloHorizonte,MG,Brazil
bFundac¸ãoHemominas,BeloHorizonte,MG,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received27October2016 Accepted24April2017 Availableonline17May2017
Introduction
Somehematologicaldiseasescanbenefitfromsplenectomy foreitherdiagnosisortreatment.Whendealingwithpatients with thalassemia, splenectomy is a common therapeutic option,particularlyindicatedwhenthepatienthasincreased transfusiondemand,symptomaticsplenomegalyoranysigns ofpoorhealth,leucopenia,andthrombocytopenia.1However,
splenectomycanleadtothromboembolicevents,particularly insplenectomizedpatientswiththalassemia intermedia.1,2
Thromboemboliccomplications insplenectomizedpatients withcomplexhemoglobindiseasesareseldomreporteddue totherarityoftheseconditions.Wethereforereportacaseofa womanwithhemoglobin(Hb)C/0-thalassemiaandrecurrent venousthromboembolismaftersplenectomy.Thepatientand allfamilymemberssignedaconsentform.
∗ Correspondingauthorat:DepartmentofInternalMedicine,FacultyofMedicine,UniversidadeFederaldeMinasGerais(UFMG),AvAlfredo
Balena,190,2ndfloor,Room243,30130-100BeloHorizonte,MG,Brazil.
E-mails:srezende@medicina.ufmg.br,suely.rezende@uol.com.br(S.M.Rezende).
Case
report
Aforty-year-oldwomanwasreferredtothehematologyclinic withmild microcytichypochromic anemiaand thrombocy-tosis. Her blood film revealed anisocytosis, poikilocytosis, microcytosis,hypochromia,stomatocytes,targetcells, eryth-roblastsandmacroplatelets(Figure1).
Shereportedafamilyhistoryofthalassemiaandapersonal historyofsplenectomyin2001duetoapainfulsplenomegaly. Shedeniedtransfusion-dependency.In2002,shesuffereda pulmonaryembolism,which recurredin2003.In2004,she hadadeepvenousthrombosisofherrightlowerlimb.This hadoccurredthreedaysafteralaparoscopictubal steriliza-tionprocedure,whenwarfarinwassuspendedforfourdays before surgery.All thromboembolic eventswere objectively confirmed.
http://dx.doi.org/10.1016/j.bjhh.2017.04.006
revbrashematolhemoter.2017;39(4):354–356
355
Figure1–Bloodfilmoftheproband.Bloodfilmshowing anisocytosis,poikilocytosis,microcytosis,hypocromia, stomatocytes(arrows),targetcells(smallarrows), erythroblasts(cross)andmacroplatelets.
In2005,aDopplerechocardiographyrevealedpulmonary hypertension with an estimated pulmonary pressure of 53mmHg.Finally,in2007,shewasdiagnosedwithcongestive heart failure (New York Heart Association III/IV). Throm-bophiliascreeningwasperformed,revealingabsenceofthe prothromboticmutations:factorVLeidenandprothrombin G20210A.Antiphospholipidantibodieswerealsoabsent.She isunderanticoagulationwithwarfarinindefinitelyandsince thenshehasnotpresentedanythromboembolicevent.
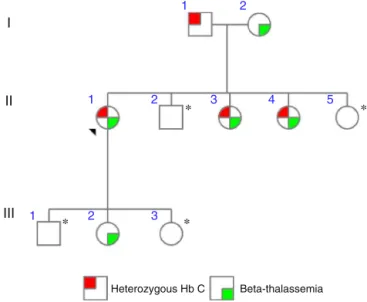
DNAanalysisrevealedacompoundheterozygosityforHbC (HBB:c.19G>A)/0-thalassemia(HBB:c.118C>T).Afamilystudy wascarriedout (Figure2).Herfatherwasheterozygousfor HBB:c.19G>A(I-1–Figure2).Hewasasymptomaticwith unre-markableblood countandfilm.Hermother (I-2– Figure2)
I
1 1 1 2 2 3 3 4 5 2II
∗
∗
∗
∗
III
Heterozygous Hb C Beta-thalassemia
Figure2–Pedigreeofthefamily.Moleculargenetic analyseswereperformedforsixfamilymembers.The arrowheadindicatestheproband(II-1).*Indicatesmembers inwhombloodwasnotcollected.Themutationcausing heterozygous0-thalassemiawasCD39(HBB:c.118C>T).
andoneofherdaughters(III-2–Figure2)wereheterozygous forHBB:c.118C>T.Liketheproband,twosistersalsocarried HbC/0-thalassemia (II-3andII-4 –Figure2).Theyreported transfusionsonlyduringlabor,butdeniedsplenectomyand neverhadathromboembolicevent.Theirbloodcountshowed mildmicrocytichypochromicanemia.
Discussion
Thalassemiaitself,especially-thalassemiaintermedia,isa well-knowncauseofahypercoagulablestatedueto abnormal-itiesinvolvingplatelets,redbloodcells(RBC),endothelialcells andthrombinactivation.3,4,5Otherhemostaticchangesmay
includealterationsinthelevelsofprocoagulantor anticoagu-lantfactors,and/orchronicactivationofendothelialcells,or whitebloodcells.4Splenectomymayalsoincreasetheriskof
thrombosis.1,2
Patientswith-thalassemiahavechronicplatelet activa-tion,increasedplateletaggregation,expressionofCD26Pand CD63and shortenedplatelet lifespan related toenhanced consumption.5 Moreover, there are major RBC alterations
due to the formation and precipitation of hemichromes, presence of reactive oxygen species and an increased thrombin generationrelatedtotheexpressionof procoagu-lant negatively-chargedphospholipids onthe RBCsurface.2
Indeed,lossofthehemocathereticfunctionofthespleenleads toanincreasednumberofabnormalcirculatingRBCs,which arecapableofgeneratingthrombin.6 Thisexplainswhythe
lackofregulartransfusionsincreasestheriskofthrombosis.5
The patient reported herein had three thromboembolic events, two unprovoked pulmonary embolisms and a pro-vokeddeepvenousthrombosis.Splenectomizedpatientswith thalassemia with high RBC counts, thrombocytosis, pul-monaryhypertensionandtransfusionnaivetyareathigher risk to develop thromboembolic events.1 This patient had
all these risk factors. Due to the occurrence of recurrent thrombosisandtothedescribedriskfactorsforthrombosis, a long-term secondary prophylaxiswith warfarin was rec-ommendedwithatargetinternationalnormalizedratio(INR) between2and3.Thiswashighlyeffective,asshehasnothad anythromboticeventssince.
Oneimportantquestionwhileattendingpatientswith tha-lassemiaand highthrombotic riskishow tomanagethem whileinhigh-risk situationsforthrombosissuchasbefore splenectomy,immobilizationandhospitalization?Sincehigh quality evidence for recommending thromboprophylaxis is lacking,wemanagepatientswiththalassemiasimilartothe generalpopulation.Therefore,furtherstudiesonthisissueare warranted.
Conclusion
356
revbrashematolhemoter.2017;39(4):354–356in patients with hemoglobin diseases before they indicate splenectomy.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1.TaherAT,MusallamKM,KarimiM,El-BeshlawyA,BelhoulK, DaarS,etal.Splenectomyandthrombosis:thecaseof thalassemiaintermedia.JThrombHaemost.2010;8(10):2152–8.
2.CappelliniMD,RobbioloL,BottassoBM,CoppolaR,FiorelliG,
MannucciPM.Venousthromboembolismand
hypercoagulabilityinsplenectomizedpatientswith thalassemiaintermedia.BrJHaematol.2000;111(2):467–73.
3.TaherAT,OtrockZK,UhtmanI,CappelliniMD.Thalassemia andhypercoagulability.Blood.2008;22(5):283–92.
4.SirachainanN.Thalassemiaandthehypercoagulablestate. ThrombRes.2013;132(6):637–41.
5.CappelliniMD,MusallamKM,PoggialiE,TaherAT.
Hipercoagulabilityinnon-transfusion-dependentthalassemia. BloodRev.2012;26(1):S20–3.