SOCIEDADE BRASILEIRA DE ORTOPEDIA E TRAUMATOLOGIA
w w w . r b o . o r g . b r
Update
article
Anterior
cruciate
ligament
–
updating
article
夽
Marcus
Vinicius
Malheiros
Luzo,
Carlos
Eduardo
da
Silveira
Franciozi
∗,
Fernando
Cury
Rezende,
Guilherme
Conforto
Gracitelli,
Pedro
Debieux,
Moisés
Cohen
UniversidadeFederaldeSãoPaulo,EscolaPaulistadeMedicina,DepartamentodeOrtopediaeTraumatologia,GrupodoJoelho,SãoPaulo, SP,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory: Received30June2015 Accepted2July2015 Availableonline6June2016
Keywords:
Anteriorcruciateligament Patellarligament
Jointinstability Knee
Reconstructivesurgicalprocedures
a
b
s
t
r
a
c
t
Thisupdatingarticleontheanteriorcruciateligament(ACL)hastheaimofaddressingsome ofthemostinterestingcurrenttopicsinthisfield.Withinthisstratifiedapproach,itcontains thefollowingsections:ACLremnant;anterolateralligamentandcombinedintraand extra-articularreconstruction;fixationdevices;andACLfemoraltunnelcreationtechniques.
©2016SociedadeBrasileiradeOrtopediaeTraumatologia.PublishedbyElsevierEditora Ltda.ThisisanopenaccessarticleundertheCCBY-NC-NDlicense(http:// creativecommons.org/licenses/by-nc-nd/4.0/).
Ligamento
cruzado
anterior
–
Artigo
de
atualizac¸ão
Palavras-chave:
Ligamentocruzadoanterior Ligamentopatelar
Instabilidadearticular Joelho
Procedimentoscirúrgicos reconstrutivos
r
e
s
u
m
o
Este artigo de atualizac¸ãosobre ligamentocruzado anterior (LCA) visaabordar alguns dos tópicosmaisinteressanteseatuaissobreotema.Dentrodessaabordagem estrati-ficadaincluem-se asseguintessec¸ões:remanescentedoLCA;ligamentoanterolaterale reconstruc¸õesextra-articularescombinadasaintra-articulares;dispositivosdefixac¸ão; téc-nicasdeconfecc¸ãodotúnelfemoral.
©2016SociedadeBrasileiradeOrtopediaeTraumatologia.PublicadoporElsevierEditora Ltda.Este ´eumartigoOpenAccesssobumalicenc¸aCCBY-NC-ND(http:// creativecommons.org/licenses/by-nc-nd/4.0/).
夽
StudyconductedattheUniversidadeFederaldeSãoPaulo,EscolaPaulistadeMedicina,DepartamentodeOrtopediaeTraumatologia, GrupodoJoelho,SãoPaulo,SP,Brazil.
∗ Correspondingauthor.
E-mail:cacarlos66@hotmail.com(C.E.d.S.Franciozi).
http://dx.doi.org/10.1016/j.rboe.2016.05.001
Introduction
Theanteriorcruciateligament(ACL)isoneofthemost stud-iedtopicsinorthopedicsnowadays.Duetonewtrends,such asthe conceptofanatomical reconstruction,which gained power in the last decade, new motivation has been given tothestudyofthisligament,withimportantadvancesand innovations. Supportedby basic science,the ACL remnant isincreasinglygainingprominenceinreconstructivesurgery, butthereisstillnoconsensusregardingthevarious recons-tructions techniquesand its preservation, atopic that will beaddressedinthisarticle. Theso-callednewligament of the knee, the anterolateral ligament, has recently gained prominenceandexplainsoldconceptsandtheoriesthat jus-tify its increased restrictive effect on pivoting due to the greaterleverarmrelativetothecentralpositionoftheACL. Thiselucidates partofthe biomechanics ofreconstruction andextra-articularreinforcements.Orthopedicsfollowsthe advancement ofmedicine and currently, a myriad of fixa-tiondevicesareavailableforsurgeons,who,inlightofsuch diversity, must improve their knowledge of the peculiari-ties, advantages, disadvantages, and comparisons between each one. Finally, also driven by the rediscovery of ACL anatomy, different techniques of femoral tunnel prepara-tionhavebeendeveloped,eachwithitsowncharacteristics, turning necessary a detailed analysis of the most used options.
Therefore,thisupdateontheACLaimedtoaddresssome ofthe mostinteresting and current topics on the subject. In this stratified approach, the following sections are:ACL remnant; anterolateral ligament and extra-articular com-bined withintra-articular reconstructions; fixation devices; andtechniquesforcreatingthefemoraltunnel.
ACL
remnant
PartialACLlesionsare common (5–38%);recently,the rem-nantfibershavereceivedmoreattention,aimingtopreserve andincorporatetheminACLreconstruction(ACLR). Remnant-preservingACLRshouldoptimizeligamentization,sincethe functionalremnantfibersbiomechanicallyprotectthegraft, thevascularizedsynovialenvelopeoftheremnantligament contributestothevascularizationofthegraft,thevalve mech-anismcreatedbythetissueremnantinthetunnelprevents theentryofsynovialfluidanddecreasestheenlargementof thetunnel, and themechanoreceptors presentinthe rem-nantassistinproprioception,asdemonstratedinhistological studies.1–12
ThedefinitionofACLremnant-preservingreconstruction surgery is controversialbecause it involves three different procedures grouped underthe same terminology: selective bundleaugmentation(SBA;ACLRinapartiallesioninvolving only the posterolateral or anteromedial bundle); augmen-tation (AG; ACLR in a partial lesion involving one or both bundleswithremnantfunctionaltissue);non-functional rem-nantpreservation(NFRP;ACLRinacompletelesioninvolving bothbundleswithnon-functionalremnanttissue).The defi-nitionoffunctionalornon-functionalremnantfibershouldbe
madearthroscopically,bypalpationwiththeprobe,withthe kneein90◦flexionandalsointhe“figure-of-4”position.1
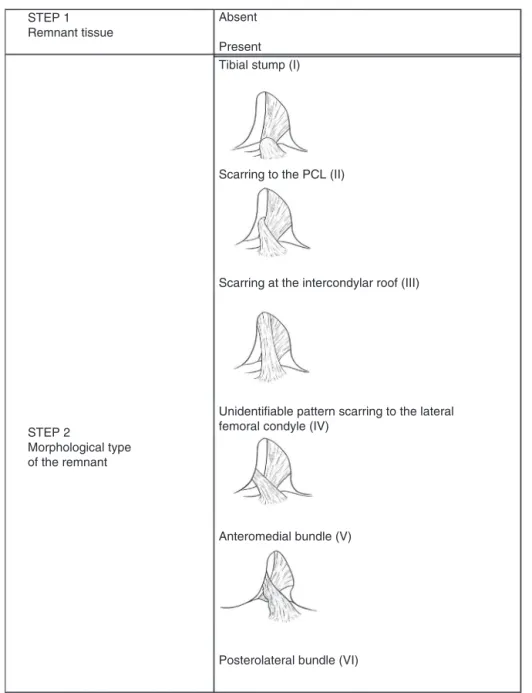
ForthearthroscopicclassificationofACLinjuriesinvolving theremnant,astagedapproachthatevaluatesthepresence orabsenceofremnanttissuemorphologyandfunctionalityis recommended.Thisstagedapproachinvolves(Fig.1):
1. Remnanttissue:absent,present.
2. Morphologicaltypeofremnant:tibialstump(I),scarringto
thePCL(II),scarringtotheintercondylarroof(III),
uniden-tifiablepatternscarringtothelateralfemoralcondyle(IV),
anteromedialbundle(V),posterolateralbundle(VI). 3. Remnantfunctionality:functional,non-functional.
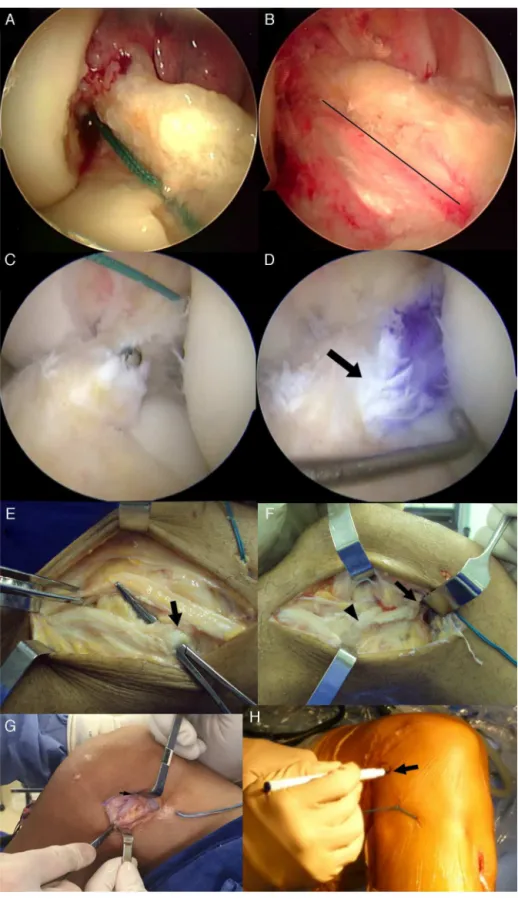
AfterACLR,steps1–3shouldberepeated,since,duringthe reconstruction,partoftheremnanttissuemaybedamaged, changingits initialstatus.Then,the typeofreconstruction thatpreservestheremnantisdetermined:SBA,AG,orNFRP. Oncethefinalpassofthegraftismade,thepercentageofgraft coveragebytheremnanttissuemustbeestimatedand docu-mented.Itisimportanttodocumenttheestimatedpercentage ofgraftcoveragetoassessitspossibleroleinthestabilityand postoperativefunction,sincesomestudieshaveshownthat highercoverageisrelatedtobetteroutcomes13(Fig.2).
Thepassageofthegraftwithpreservationoftheremnant canbeperformedintwomainways.Thegraftcanbepassed alongtheperipheryofthetibialfootprint,preservingthe rem-nanttissueandbeingpassedalongsideit,thusmaintaining thefunctional remnantfibersandtheirinserts(Fig.3Aand B).Anotherpossibilityistopassthegraftthroughthecenter ofthetibialfootprint,surroundingitwiththeremnanttissue, whichwillactasabiologicalsleeve,whetherthroughthe rem-nant synovialsheath,theremnantligamenttissue,orboth (Fig.3CandD).Inthislatterapproach,itisrecommendedto graduallywidenthetibialtunnelwithsuccessivelylargerdrill bits untilthefinaldiameterisreached;caremustbetaken tostoptheprogressionofdrillswhentheybreachthetibial plateau,sothatthedrillremainsinsidetheremnant.When thishappens,thereistheimpressionthattheACLremnant tissueis“dancing”duetothedrillactionwithintheremnant enclosure.Then,apathiscreatedinsidetheremnant enclo-surewithashaverthatopensitproximally,maintainingthe entireperipheraltissueandcreatingonlyacentralpathto passthegraft.14
STEP 1 Remnant tissue
Absent
Present Tibial stump (I)
Scarring to the PCL (II)
Scarring at the intercondylar roof (III)
Unidentifiable pattern scarring to the lateral femoral condyle (IV)
Anteromedial bundle (V)
Posterolateral bundle (VI) STEP 2
Morphological type of the remnant
Fig.1–ArthroscopicclassificationoftheACLremnant.
proventodecreasetunnelenlargementwhencomparedwith conventional ACLR with remnant debridement,due to the valvemechanismcreated,whichpreventsorreducestheentry ofsynovialfluid.6,12Severalstudiesemphasizethepotentialof bettergraftrevascularizationwhenpreservingtheremnant.A
randomizedclinicaltrial(RCT)thatusedmagneticresonance demonstratedtheaccelerationofthisprocess,whichcertainly enhancesligamentization.8
Some studies defend the potential benefit of preser-ving the remnant tissue in the ligamentization process,
Remnant tissue
Recommended ACLR type
Percentage of graft coverage by the remnant tissue
Estimated percentage
Estimated percentage Absent
Single-bundle, presence of functional remnant tissue
Presence of functional remnant tissue
Presence of non-functional remnant tissue
Conventional
SBA
AG
NFRP
particularlythesynoviumofthistissue,asapotentialsource ofmesenchymalcells.Thispotentialisinverselyproportional toinjurychronicityandsuggestsbetterresultswhen remnant-preservingACLRisperformedinmoreacutecases.18
Despite the supposed advantage of ACL remnant-preserving recosntruction shown in several studies with lowlevelofevidence, whenassessingRCTs,the functional outcomesandstabilityaresimilar,andthesuperiorityofACL remnant-preserving reconstruction is only demonstrated eventually. Thus, further studies are needed with larger samplesize,appropriatemethodology,andmostimportantly, consensusindefining the typeof ACLremnant-preserving reconstruction. The terminology SBA, AG, NFRP, and the methodologydescribedhereinaresuggested.2,4,5,10,11,13,15–17
Anterolateral
ligament
and
combined
intra-and
extra-articular
reconstruction
Rotationalstabilitycontrolisatopicthatattractstheattention ofexpertsinthefieldofACLRsurgery.Itremainsuncertain whetherthecurrentarthroscopicACLRtechniquesare suffi-cienttoproviderotationalstabilityinallcasesofthisligament injury,anditisnotfullyunderstoodhowthedifferentpatterns ofACLinjuriesbehave.19,20
Persistent rotational instability after ACLR has been describedandappearstocorrelatedirectlywithdecreasein satisfactionanddeficitinkneefunctiongainwithinthe post-operativeperiod.21,22Furthermore,thelackofkneerotational controlappearstoactasacausalfactorfornewchondraland meniscallesions.23
This discussion gained momentum after the growing debate over the anterolateral ligament (ALL) of the knee,
whoseinjuryappearstobeassociatedwithsomecasesofACL injury.In1879,Segondwasthefirsttodescribethisligament asa“resistantfibrousbundle”intheanterolateralknee com-partmentwiththeuniquefeatureoftensioninforcedinternal rotation.24
Later, some authors suggested that this structure was merely a capsular thickening of the anterolateral compartment.25However,somestudieshavedrawnattention totheimportanceofthisportion oftheiliotibial tract.The name anterolateral ligament was initially popularized in Brazil and published inthis journal.26 More recent studies havebroughtthiscontroversytolightagain,bydefiningthis structureasadifferentligament.27–29Moreover,after biome-chanicaltesting,aclosecorrelationwasestablishedbetween ALLinjuryandtheworseningofrotationalstability,defined byapositivepivot-shifttest.25,30Thus,authorswhoadvocate theassociationbetweenACLandALLinjurieshaveproposed theneedforcombinedintra-andextra-articularACLR,which appears reasonable from a biomechanical standpoint in the promotion ofcombined anteroposterior and rotational stability.28,31
Inarecentlypublishedmeta-analysisofRCTs,thepresent authors compared isolated ACLR techniques with com-bined intra- and extra-articular reconstruction techniques. Althoughthefunctionalscoresresultsweresimilarbetween the groups, there was an improvement in the knee sta-bility outcome observed in both pivot-shift and Lachman tests.32Despite previousstudies suggestedthattheserates would increase, no differences were observed in the rates ofkneestiffness,infection,andlateralcompartment arthri-tis among the study groups duringthe assessed follow-up time.32–34However,duetothelackoffunctionalimprovement associated with extra-articular reconstruction, the authors
femoralcondyle(IV).Remnantfunctionality(assessedwithprobe):nonfunctional.Apathwascreatedwithintheremnant shellwiththeshaver,whichopensitproximally(thetipoftheshavercanbeseenprotrudingthroughtheremainderofthe enclosure).Alltissueintheperipheryismaintained,andonlyacentralpathiscreated,topassthegraft.(D)ACL
Remnant-preservingreconstructiontypeNFRP.NFRP–nonfunctionalremnantpreservation:ACLRinacompletelesion involvingbothbundleswithnon-functionalremnanttissue.Thegraftwaspassedthroughthecenterofthetibialfootprint andencasedbytheremnanttissue,whichwillactasabiologicalsleeve,whetherbytheremnantsynovialsheath,remnant ligamenttissue,orboth.Estimatedpercentageofgraftcoveragebytheremnanttissue:60%.Arrowshowsgraftexitwithin theremnant.(E)Extra-articularACLreinforcementwithisolatediliotibialband(derivativemonoloop,similartothe extra-articulartechniquesbyMacIntoshandLemaire).Thecentralone-thirdoftheiliotibialtractisdissectedwith1–1.5cm thicknesses,maintainingitsdistalinsertionandreleasingitsproximalinsertion.ThisispreparedwithKrackowsuture withNo.5Ethbondwire.AKellyclampispasseddeeplyintothelateralcollateralligament(arrow)toallowforcentral iliotibialtractbandpassageafterproximalreleaseandpreparation.Thecentralthirdoftheiliotibialtractwith1–1.5cm thicknessesisalreadymade.(F)Centerbandoftheiliotibialtractalreadydeeplypassedbythelateralcollateralligament (arrowhead)andinsertedintothedistalinsertionofthelateralintermuscularseptumofthefemur,asshownbythearrow (oneoftherecommendedpointsforinsertionofextra-articularreinforcementsinACLR)aftersatisfactoryisometrictest. Thereinforcementisfixedwithaninterferencescreworanchorwithkneeat90◦flexionandneutralrotationafterACLR
concludedthatitisstilluncertainwhetherthisstabilitygain outweighsthemorbidityassociatedwiththeincreaseinthe useofthisprocedureintheanterolateralaspectoftheknee. Conversely, the same meta-analysis also included studies ofextra-articularreconstruction using possiblymore obso-letetechniques;adeeperunderstandingofALLcanenhance andlead tomoreanatomical andminimally invasive tech-niques for extra-articular reconstruction and improve its results.Furthermore,theauthorsconcludedthatthereisstill considerableroomforresearchinthefieldofintra-and extra-articularACLR,notonlyforimprovingthetechnique,butalso regardingthegroupsofindividualsthatwouldbenefitfromthe combinedprocedure.Infact,inarecentpublication, Sonnery-Cottetetal.35presentedarecommendationregardingwhich groupsofindividualsarecandidatesforpercutaneous intra-andextra-articularACLRthroughthetechniquedescribedin theirarticle:thosewithpivotgrade2or3,Segondfracture, chronicACLinjuries,high-levelsportsactivity(suchas soc-cer,rugby,handball,andbasketball)andradiographsshowing thenotchsign inthe lateralfemoralcondyle.According to thecriteriadescribedbytheseauthors,asimplerestorationof thecentralaxisthroughisolatedACLRwouldnotbeenough torestorerotationalstabilityandwouldrequireaperipheral strengtheningtothecentralpivotreconstruction.
Avarietyoftechniquesaredescribedintheliteraturefor combinedintra-andextra-articularACLR.28Classically, ten-odesiswiththeuseofacentralbundleoffascialatahasbeen usedsincetheearlyisolatedextra-articularACLRdescribedby Lemaire36in1967.Otherauthorshaveusedminimally inva-sivetechniquestoextendthesemitendinosusgraft passing throughtheoverthetoppositionoralsoasanextensionofthe femoraltunnelofintra-articularACLR.31However,such tech-niquesarebasedmoreontheprincipleofprovidingperipheral stabilizationoftheanterolateralaspectofthekneethan prop-erly on different anatomical points that take into account thestructureoftheanterolateralligament.Therefore,an in-depth study ofthe anterolateralcompartment ofthe knee anatomyisveryimportantwithregardtobetter understand-ingoftheanatomicalcharacteristicsandisometricsofALL, inadditiontothebestgraftoptionforreconstruction.Thus, reconstructionsthatreproducetheanatomyofthisligament withlesssurgicalmorbiditymayemerge,possiblyimproving theresults.Moreclinicalstudiesarealsoneededtodetermine theactualneedofcombinedreconstructionwithinthegeneral populationofindividualswithACLinjuryorifonlyspecific groupsofindividualswouldbenefitfromthesetechniques,as forexampleincaseofACLRrevision,chronicinjuries,orcases withexcessiverotationalinstabilityevidencedbyanexplosive pivot-shiftatclinicalevaluation(Fig.3E–H).
Fixation
devices
Sincethesuccessofthereconstructiondependsunequivocally on graft position,the development offixationdevices that keepthisneoligamentintheproperpositiondespite move-ments and post-operative rehabilitation techniques allows rehabilitationtobeginearlyandextensivelywithoutlossof thispositioning,whichinturnreducestheriskof complica-tionssuchasarthrofibrosisanddeepveinthrombosis,among
others.Asuitableattachmentmechanismmustkeepthegraft firmlyinthedesiredplaceforatleasteightweeks,sothatit hasachancetoestablishcontinuitywiththebonetissue.37 Currently, the existing techniques can be subdivided into intra-andextra-tunnelfixations.Thesearesubdivided into suspensory,transfemoralinthebuttressposition,and trans-femoraltransfixationtechniques.38Thosearerepresentedby compression/interferencefixationdeviceswiththebone-graft interface.39Thefactisthatthereisnogoldstandardforgraft fixationinACLR.40
Biomechanical studies have comparedthe different fix-ation methods under different perspectives. Fixation in terms of strength, stiffness, and elongation was favorable tosuspensorymethodswhencomparedtothebuttressand compression methods.41 Thesame wasobservedregarding graftsliding.42Theloadrequiredtocauselossoffixationwas lower withinterferencescrewswhencomparedwith extra-tunnel methods (Endobutton and cross-pin).42 In contrast, suspensory fixation devices have particular complications, whether the “bungee-effect” (or pistoning)43 or the “wind-shieldeffect.”44Suchcomplicationscanpotentiallyleadtoa delayingraftintegrationinitsbonebedandtotunneldilation overtime,whichmayimpairorevenmakeasinglerevision surgeryimpossibleintheeventofre-injury.However,noneof thesecouldbeassociatedwithworseningofclinical parame-ters.
Inordertoresolvetheissue,Colvinetal.40 conducteda level-1 meta-analysis that compared intra-tunnel (interfer-encescrews)withextra-tunnelfixationmethods(Endobutton andshearpins)forhamstringtendongraftfixationinACLR. Thus, following the Cochraneand Quorum methodologies, those authors selected eight studies (RCTs), five of which wereincludedinthemeta-analysis.Afterdataanalysis,they observedthattherewasnodifferencebetweenfixation meth-odsfortheoutcomesregardingthefunctionandqualityof life withinthestipulated follow-up period. However,when theanalyzedoutcomewastreatmentfailureduringsurgery, despite theabsence ofstatistical significance(RR=0.52;CI: 0.1794–1.3122;p=0.1542),therewasacleartrendinfavorof theinterferencescrew,whichpresentedfewerfailuresinall retrievedstudies.40Thoseauthorssuggestedthataclose fixa-tionofthejointmaybebiomechanicallyfavorable.45Similarly, Saccomannoetal.46conductedasystematicreview(level1) andcomparedthesuspensoryfixation(Endobutton)with fix-ation in thebuttress position(transverse pin). Five studies (317patients)were includedafterasearch thatonceagain followedtheCochraneprotocols.Nodifferencesbetween fixa-tionmethodswereobservedregardingtheLysholmandIKDC scores(theonlyscoresinwhichthemeta-analysiscouldbe performed). Althoughthere were statistically lower tunnel enlargementwiththeuseoftransversepins,thisfacthadno clinicalconsequences.46
thesedatashouldbeanalyzedinlightofthelimitationsthat werenotassessed(interferenceinpost-operativeimagingand greaterdifficultyinrevisionsurgerieswithmetalscrews).The authorsalsofoundatendency(notstatisticallysignificant)of higherinflammatoryactivitywhenthebioabsorbablematerial wasPGA,andbetterLysholmscorewithPLLA.
It is noteworthy that femoral fixation can be properly achievedwithoutany fixationmethod.ConceivedinFrance inthe1980s,thepress-fitmethodconsistsofmakingabone plug slightly larger than the femoral tunnel. This plug is insertedintothetunnelunderpressureand becomesstuck inside,asa“champagnecork.”Sarzaeemetal.48 promoted a RCT comparing this press-fit fixation with the interfer-encescrew.Ina12-monthfollow-upstudywith158patients dividedintotwogroups,nodifferenceswereobservedinany oftheoutcomemeasures(Lysholm,IKDC,KT-1000,Lachman, pivot).
Insummary,despitethesmallbiomechanicaldifferences amongthemethods,eachofthemwaseffectiveandefficient ingraftfixationintheperiodbetweenthepostoperativeperiod andligamentization.Nonetheless,attentionshouldbegiven notonlytoindividualfixation(tibialandfemoral),butalsoto therelationshipbetweenthem,sinceaverylargediscrepancy betweenthetwofixationmethodscangenerateaweaklinkin thereconstruction,whichcanleadtoanoverlapofonepoint overanotherand,consequently,failure.49
Techniques
for
creating
the
femoral
tunnel
Inrecentyears,anincreasehasbeen observedinthe indi-cations of independent techniques for femoral drilling in ACLR,representedbythetransportalorinside-outtechnique (TP),outside-in (OI), and OI retrograde. In2013, the Cana-dianOrthopedicAssociationreported that68% ofsurgeons usedindependenttechniques forfemoraldrilling and only 31%usedthetranstibialtechnique(TT).50Despitethis tech-nicalchangeinACLRinthepastdecade,thereisstilldoubt aboutitsobjectiveandsubjectiveclinicalsuperiority,aswell asthebiomechanicaladvantagesofthedifferenttechniques used.
Ribohetal.51publishedasystematicreviewthatincluded six RCTs. Four compared OI versus TT and two, TP versus TT.Inthatreview,26biomechanicalstudiesandstudiesthat analyzedthepositioningofthegraftincadaversandinvivo werealsoincluded.TheclinicaloutcomesmeasuredinRCTs showednodifferencebetweenthetechniqueswhen consid-eringtheincidenceoffailure, objectiveIKDC,andscales of physicalactivities such as Tegner. When evaluated by the Lysholmscore,aslightsuperiorityofTTwasobserved. How-ever, despite the proven statistical difference, it was not consideredclinicallyrelevant(mean:−0.62,95%CI:−1.09to −0.15).RCTsshowedloweranteriorloosenessinfavorof
inde-pendenttechniqueswhenmeasuredbyarthrometersinmm (mean:0.33,95%CI:0.10–0.55).51
In the same review, the biomechanical studies and the studiesthatassessedgraftpositioninginvivoandincadaver showed that the independent technique, OI, also showed lessanteriortranslationwhenmeasuredbyLachman(mean: 2.2,95%CI:0:34–4:07),lessanteriortranslationwithstrength
of134N(mean:1.0, 95%CI:0.29–1.71), andincreased rota-tionalstability(mean:3.36,95%CI:1.88–4.85)whencompared withTT.Independenttechniquesalsoshowedamoreoblique femoraltunnelinthecoronalandsagittalplane,resultingin greatersimilaritybetweentheoriginalstrengthsofthenative ACL,buthadahigherriskofexplosionoftheposteriorwallof thelateralfemoralcondyleduringdrilling.51
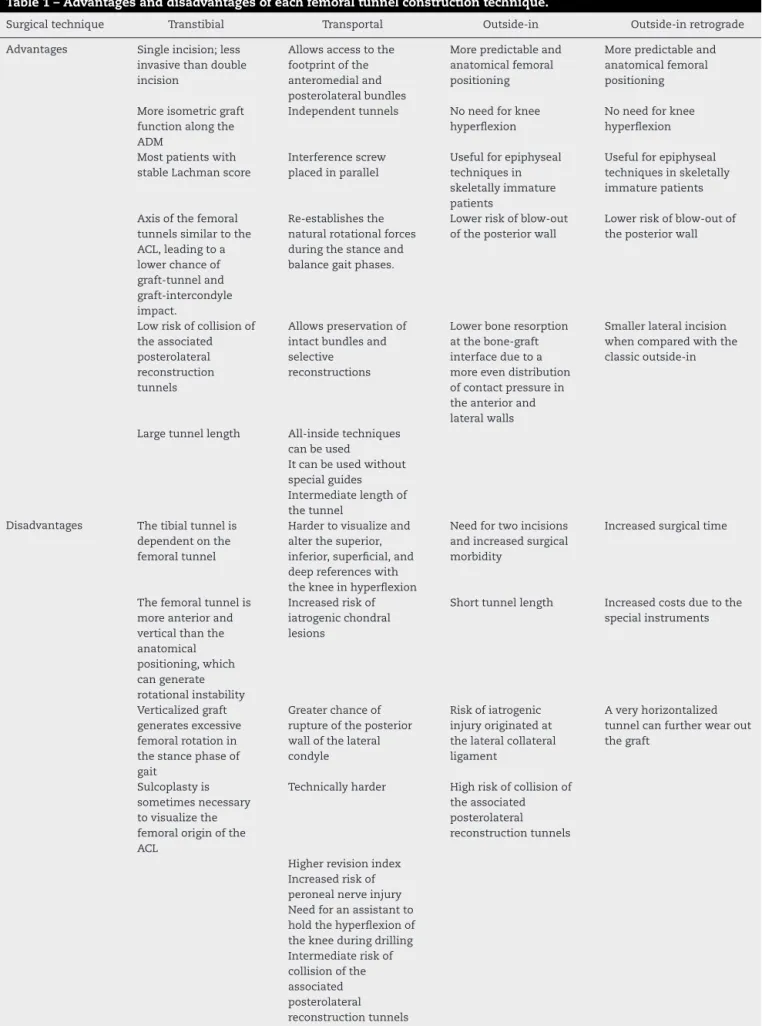
Recently, Robin et al.52 published a systematic review withoutmeta-analysisthatincludedtenclinicalstudies,ten descriptionsofsurgicaltechnique,fivecadavericstudies,one kinematicstudy,andoneliteraturereview.Thereview identi-fiedtheadvantagesanddisadvantagesofthedifferentACLR techniques.Themainresults,aswellasotherspointedoutby theauthorsofthisstudy,aresummarizedinTable1.
Rahr-Wagner et al.53 compared the results of different ACLRtechniquesfromtheDanishnationalregister, consid-ered one ofthe best and most complete records of global medicaldata.Inthatretrospectivestudy,1945TP reconstruct-ionsand 6430TTreconstructionswere analyzed, including failureastheprimaryoutcome,determinedbyACLRrevision, andassecondaryoutcomesthepivot-shifttestandfunctional scores (KOOSand Tegner). Asignificantly increasedriskof ACLR revisionwas observedwith TP,with amean relative riskof2.04(95%CI:1.39–2.99)whencomparedwithTT. Sur-prisingly,TPalsoshowedincreasedrelativerisktothepivot, withmean RR=2.86 (95%CI:2.40–3.41),andincreased rela-tive risk foranterior instability, with mean RR= 3.70 (95% CI:3.09–4.43).Inaddition,therewerenodifferencesbetween the techniquesregardingfunctional scores.That study had somelimitations,amongthemthebiasesofanyretrospective study ofdata, besidesthe probablelearningcurve,by Dan-ishphysicians,oftheTPincludedintheevaluationperiodof thestudy,duetotherecentadoptionofthetechniqueinthat country.53
TheincreasedriskofrevisionusingTPwasalsoobserved in aprospectivecohort study that compared TPtechnique versusTTwithpatellargraft.54 Anotherarticleshowedthat theanatomicalreconstructionoftheAMbundleplacesmore tension onthe graft than theAM bundleinahigher posi-tion,similartothatachievedbyTTtechnique.Therefore,a graftplacedmoreanatomicallythanisometricallywouldbe subjecttohighertensionandmoresusceptibletorupture.In TT,the graftwouldbesubjectedtoless tension,but would theoreticallydissipatetheloadthroughotherintra-articular structures, suchas the cartilage and meniscus.Only long-term prospectiveand randomizedstudieswilldemonstrate whethertheindependenttechniquesoffemoraldrillingwill be able to prevent joint degeneration and osteoarthritis.55 Among other possible explanations for the increased risk of re-rupture by independent drilling techniques, OI, are shorter femoral tunnels, which generate less integration between the graft-bone and cases ofblow-out ofthe pos-terior wallof the lateral condyle, which compromise graft integration.56–58
Table1–Advantagesanddisadvantagesofeachfemoraltunnelconstructiontechnique.
Surgicaltechnique Transtibial Transportal Outside-in Outside-inretrograde
Advantages Singleincision;less invasivethandouble incision
Allowsaccesstothe footprintofthe anteromedialand posterolateralbundles
Morepredictableand anatomicalfemoral positioning
Morepredictableand anatomicalfemoral positioning
Moreisometricgraft functionalongthe ADM
Independenttunnels Noneedforknee hyperflexion
Noneedforknee hyperflexion
Mostpatientswith stableLachmanscore
Interferencescrew placedinparallel
Usefulforepiphyseal techniquesin skeletallyimmature patients
Usefulforepiphyseal techniquesinskeletally immaturepatients
Axisofthefemoral tunnelssimilartothe ACL,leadingtoa lowerchanceof graft-tunneland graft-intercondyle impact.
Re-establishesthe naturalrotationalforces duringthestanceand balancegaitphases.
Lowerriskofblow-out oftheposteriorwall
Lowerriskofblow-outof theposteriorwall
Lowriskofcollisionof theassociated posterolateral reconstruction tunnels
Allowspreservationof intactbundlesand selective
reconstructions
Lowerboneresorption atthebone-graft interfaceduetoa moreevendistribution ofcontactpressurein theanteriorand lateralwalls
Smallerlateralincision whencomparedwiththe classicoutside-in
Largetunnellength All-insidetechniques canbeused
Itcanbeusedwithout specialguides Intermediatelengthof thetunnel
Disadvantages Thetibialtunnelis dependentonthe femoraltunnel
Hardertovisualizeand alterthesuperior, inferior,superficial,and deepreferenceswith thekneeinhyperflexion
Needfortwoincisions andincreasedsurgical morbidity
Increasedsurgicaltime
Thefemoraltunnelis moreanteriorand verticalthanthe anatomical positioning,which cangenerate rotationalinstability
Increasedriskof iatrogenicchondral lesions
Shorttunnellength Increasedcostsduetothe specialinstruments
Verticalizedgraft generatesexcessive femoralrotationin thestancephaseof gait
Greaterchanceof ruptureoftheposterior wallofthelateral condyle
Riskofiatrogenic injuryoriginatedat thelateralcollateral ligament
Averyhorizontalized tunnelcanfurtherwearout thegraft
Sulcoplastyis sometimesnecessary tovisualizethe femoraloriginofthe ACL
Technicallyharder Highriskofcollisionof theassociated posterolateral reconstructiontunnels
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1. daSilveiraFrancioziCE,InghamSJ,GracitelliGC,LuzoMV,Fu FH,AbdallaRJ.Updatesinbiologicaltherapiesforknee injuries:anteriorcruciateligament.CurrRevMusculoskelet Med.2014;7(3):228–38.
2. ColombetP,DejourD,PanissetJC,SieboldR,French ArthroscopySociety.Currentconceptofpartialanterior cruciateligamentruptures.OrthopTraumatolSurgRes. 2010;968Suppl.:S109–18.
3. CrainEH,FithianDC,PaxtonEW,LuetzowWF.Variationin anteriorcruciateligamentscarpattern:doesthescarpattern affectanteriorlaxityinanteriorcruciateligament-deficient knees?Arthroscopy.2005;21(1):19–24.
4. BudaR,RuffilliA,ParmaA,PagliazziG,LucianiD,RamponiL, etal.PartialACLtears:anatomicreconstructionversus nonanatomicaugmentationsurgery.Orthopedics. 2013;36(9):e1108–13.
5. DejourD,NtagiopoulosPG,SagginPR,PanissetJC.The diagnosticvalueofclinicaltests,magneticresonance imaging,andinstrumentedlaxityinthedifferentiationof completeversuspartialanteriorcruciateligamenttears. Arthroscopy.2013;29(3):491–9.
6. Demira ˘gB,ErmutluC,AydemirF,DurakK.Acomparisonof clinicaloutcomeofaugmentationandstandard
reconstructiontechniquesforpartialanteriorcruciate ligamenttears.EklemHastalikCerrahisi.2012;23(3): 140–4.
7. DhillonMS,BaliK,VasisthaRK.Immunohistological evaluationofproprioceptivepotentialoftheresidualstump ofinjuredanteriorcruciateligaments(ACL).IntOrthop. 2010;34(5):737–41.
8. GohilS,AnnearPO,BreidahlW.Anteriorcruciateligament reconstructionusingautologousdoublehamstrings:a comparisonofstandardversusminimaldebridement techniquesusingMRItoassessrevascularisation.A randomizedprospectivestudywithaone-yearfollow-up.J BoneJointSurgBr.2007;89(9):1165–71.
9. HongL,LiX,ZhangH,LiuX,ZhangJ,ShenJW,etal.Anterior cruciateligamentreconstructionwithremnantpreservation: aprospective,randomizedcontrolledstudy.AmJSportsMed. 2012;40(12):2747–55.
10.MunetaT,KogaH,JuYJ,HorieM,NakamuraT,SekiyaI. Remnantvolumeofanteriorcruciateligamentcorrelates preoperativepatients’statusandpostoperativeoutcome. KneeSurgSportsTraumatolArthrosc.2013;21(4): 906–13.
11.PujolN,ColombetP,PotelJF,CucuruloT,GraveleauN,HuletC, etal.Anteriorcruciateligamentreconstructioninpartial tear:selectiveanteromedialbundlereconstruction conservingtheposterolateralremnantversussingle-bundle anatomicACLreconstruction:preliminary1-yearresultsofa prospectiverandomizedstudy.OrthopTraumatolSurgRes. 2012;988Suppl.:S171–7.
12.ZhangQ,ZhangS,CaoX,LiuL,LiuY,LiR.Theeffectof remnantpreservationontibialtunnelenlargementinACL reconstructionwithhamstringautograft:aprospective randomizedcontrolledtrial.KneeSurgSportsTraumatol Arthrosc.2014;22(1):166–73.
13.NakamaeA,OchiM,DeieM,AdachiN,ShibuyaH,OhkawaS, etal.Clinicaloutcomesofsecond-lookarthroscopic
evaluationafteranteriorcruciateligamentaugmentation: comparisonwithsingle-anddouble-bundlereconstruction. BoneJointJ.2014;96-B(10):1325–32.
14.Sonnery-CottetB,FreychetB,MurphyCG,PupimBH,Thaunat M.Anteriorcruciateligamentreconstructionand
preservation:theSingle-AnteromedialBundleBiological Augmentation(SAMBBA)technique.ArthroscTech. 2014;3(6):e689–93.
15.AbatF,GelberPE,ErquiciaJI,PelfortX,TeyM,MonllauJC. Promisingshort-termresultsfollowingselectivebundle reconstructioninpartialanteriorcruciateligamenttears. Knee.2013;20(5):332–8.
16.KazusaH,NakamaeA,OchiM.Augmentationtechniquefor anteriorcruciateligamentinjury.ClinSportsMed.
2013;32(1):127–40.
17.MifuneY,OtaS,TakayamaK,HoshinoY,MatsumotoT, KurodaR,etal.Therapeuticadvantageinselectiveligament augmentationforpartialtearsoftheanteriorcruciate ligament:resultsinananimalmodel.AmJSportsMed. 2013;41(2):365–73.
18.LeeDH,NgJ,ChungJW,SonnCH,LeeKM,HanSB.Impactof chronicityofinjuryontheproportionofmesenchymal stromalcellsderivedfromanteriorcruciateligaments. Cytotherapy.2014;16(5):586–98.
19.LoganMC,WilliamsA,LavelleJ,GedroycW,FreemanM. Tibiofemoralkinematicsfollowingsuccessfulanterior cruciateligamentreconstructionusingdynamicmultiple resonanceimaging.AmJSportsMed.2004;32(4): 984–92.
20.RistanisS,StergiouN,PatrasK,VasiliadisHS,GiakasG, GergoulisAD.Excessivetibialrotationduringhigh-demand activitiesisnotrestoredbyanteriorcruciateligament reconstruction.Arthroscopy.2005;21(11):
1323–9.
21.ChouliarasV,RistanisS,MoraitiC,StergiouN,GeorgoulisAD. Effectivenessofreconstructionoftheanteriorcruciate ligamentwithquadrupledhamstringsandbone-patellar tendon-boneautografts:aninvivostudycomparingtibial internal-externalrotation.AmJSportsMed.
2007;35(2):189–96.
22.KocherMS,SteadmanJR,BriggsKK,SterettWI,HawkinsRJ. Relationshipsbetweenobjectiveassessmentofligament stabilityandsubjectiveassessmentofsymptomsand functionafteranteriorcruciateligamentreconstruction.AmJ SportsMed.2004;32(3):629–34.
23.StergiouN,RistanisS,MoraitiC,GeorgoulisAD.Tibial rotationinanteriorcruciateligament(ACL)-deficientand ACL-reconstructedknees:atheoreticalpropositionforthe developmentofosteoarthritis.SportsMed.2007;37(7): 601–13.
24.SegondP.Recherchescliniquesetexpérimentalessurles épanchementssanguinsdugenouparentorse.Paris: NationalLibraryofFrance;1879.p.1–85.Availablefrom
http://www.patrimoine.edilivre.com/recherches-cliniques-et- experimentales-surles-epanchements-sanguins-du-genou- par-entorse-parpaul-segond-segond-paul-ferdinand-dr-1879-ark-12148-bpt6k5712206r.html.
25.HugstonJC,AndrewsJR,CrossMJ,MoschiA.Classificationof kneeligamentinstabilities.PartII.Thelateralcompartment.J BoneJointSurgAm.1976;58(2):173–9.
26.CohenM,VieiraEA,SilvaRT,VieiraELC,BerlfeinPAS.Estudo anatômicodotratoiliotibial:revisãocríticadesua
27.ClaesS,VereeckeE,MaesM,VictorJ,VerdonkP,BellemansJ. Anatomyoftheanterolateralligamentoftheknee.JAnat. 2013;223(4):321–8.
28.DoddsAL,HalewoodC,GupteCM,WilliamsA,AmisAA.The anterolateralligament:anatomy,lengthchanges,and associationwiththeSegondfracture.BoneJointJ. 2014;96(3):325–31.
29.HelitoCP,DemangeMK,BonadioMB,TíricoLE,GobbiRG, PécoraJR,etal.Anatomyandhistologyoftheknee anterolateralligament.OrthopJSportsMed.2013;1(7),
http://dx.doi.org/10.1177/2325967113513546.Availablefrom
http://ojs.sagepub.com/content/1/7/2325967113513546.full. pdf+html.
30.MonacoE,FerrettiA,LabiancaL,MaestriB,SperanzaA,Kelly MJ,etal.NavigatedkneekinematicsaftercuttingoftheACL anditssecondaryrestraint.KneeSurgSportsTraumatol Arthrosc.2012;20(5):870–7.
31.MarcacciM,ZaffagniniS,GiordanoG,IaconoF,PrestiML. Anteriorcruciateligamentreconstructionassociatedwith extra-articulartenodesis:aprospectiveclinicaland radiographicevaluationwith10-to13-yearfollow-up.AmJ SportsMed.2009;37(4):707–14.
32.RezendeFC,deMoraesVY,MartimbiancoAL,LuzoMV,da SilveiraFrancioziCE,BellotiJC.Doescombinedintra-and extraarticularACLreconstructionimprovefunctionand stability?Ameta-analysis.ClinOrthopRelatRes. 2015;473(8):2609–18.
33.AndersonAF,SnyderRB,LipscombABJr.Anteriorcruciate ligamentreconstruction:aprospectiverandomizedstudyof threesurgicalmethods.AmJSportsMed.2001;29(3):272–9.
34.Sonnery-CottetB,ArchboldP,ZayniR,BortollettoJ,Thaunat M,ProstT,etal.Prevalenceofsepticarthritisafteranterior cruciateligamentreconstructionamongprofessional athletes.AmJSportsMed.2011;39(11):2371–6.
35.Sonnery-CottetB,ThaunatM,FreychetB,PupimBH,Murphy CG,ClaesS.Outcomeofacombinedanteriorcruciate ligamentandanterolateralligamentreconstruction techniquewithaminimum2-yearfollow-up.AmJSports Med.2015;43(7):1598–605.
36.LemaireM.Rupturesanciennesduligamentcroiseanterieur dugenou.JChir.1967;93:311–20.
37.SchefflerSU,SudkampNP,GockenjanA,HoffmanRF,Weiler A.Biomechanicalcomparisonofhamstringandpatellar tendongraftanteriorcruciateligamentreconstruction techniques:theimpactoffixationlevelandfixationmethod undercyclicloading.Arthroscopy.2002;18(3):304–15.
38.ClarkR,OlsenRE,LarsonBJ,GobleEM,FarrerRP.Cross-pin femoralfixation:anewtechniqueforhamstringanterior cruciateligamentreconstructionoftheknee.Arthroscopy. 1998;14(3):258–67.
39.McGuireDA,BarberFA,ElrodBF,PaulosLE.Bioabsorbable interferencescrewsforgraftfixationinanteriorcruciate ligamentreconstruction.Arthroscopy.1999;15(5):463–73.
40.ColvinA,SharmaC,ParidesM,GlashowJ.Whatisthebest femoralfixationofhamstringautograftsinanteriorcruciate ligamentreconstruction:ameta-analysis.ClinOrthopRelat Res.2011;469(4):1075–81.
41.MilanoG,MulasPD,ZiranuF,PirasS,ManuntaA,Fabbriciani C.Comparisonbetweendifferentfemoralfixationdevicesfor ACLreconstructionwithdoubledhamstringtendongraft:a biomechanicalanalysis.Arthroscopy.2006;22(6):660–8.
42.AhmadCS,GardnerTR,GrohM,ArnoukJ,LevineWN. Mechanicalpropertiesofsofttissuefemoralfixationdevices foranteriorcruciateligamentreconstruction.AmJSports Med.2004;32(3):635–40.
43.FuFH,BennettCH,LattermannC,MaCB.Currenttrendsin anteriorcruciateligamentreconstruction.PartI:biologyand
biomechanicsofreconstruction.AmJSportsMed. 1999;27(6):821–30.
44.KousaP,JarvinenTL,VihavainenM,KannusP,JarvinenM. Thefixationstrengthofsixhamstringtendongraftfixation devicesinanteriorcruciateligamentreconstruction.AmJ SportsMed.2003;31(2):174–81.
45.RodeoSA,KawamuraS,KimHJ,DynybilC,YingL.Tendon healinginabonetunneldiffersatthetunnelentranceversus thetunnelexit.AmJSportsMed.2006;34(11):1790–800.
46.SaccomannoMF,ShinJJ,MascarenhasR,HaroM,VermaNN, ColeBJ,etal.Clinicalandfunctionaloutcomesafteranterior cruciateligamentreconstructionusingcorticalbutton fixationversustransfemoralsuspensoryfixation:a systematicreviewofrandomizedcontrolledtrials. Arthroscopy.2014;30(11):1491–8.
47.DebieuxP,FrancioziCE,LenzaM,FaloppaF,BellotiJC, TamaokiMJS.Bioabsorbableversusmetallicinterference screwsforgraftfixationinanteriorcruciateligament reconstruction.CochraneDatabaseSystRev.2012;(4):1–5.
48.SarzaeemMM,NajafiF,RaziM,NajafiMA.ACLreconstruction usingbone-patellatendon-boneautograft:press-fittechnique vs.interferencescrewfixation.ArchOrthopTraumaSurg. 2014;134(7):955–62.
49.MonacoE,LabiancaL,SperanzaA,AgròAM,CamillieriG, D’ArrigoC,etal.Biomechanicalevaluationofdifferent anteriorcruciateligamentfixationtechniquesforhamstring graft.JOrthopSci.2010;15(1):125–31.
50.ChechikO,AmarE,KhashanM,LadorR,EyalG,GoldA.An internationalsurveyonanteriorcruciateligament reconstructionpractices.IntOrthop.2013;37(2):201–6.
51.RibohJC,HasselbladV,GodinJA,MatherRC3rd.Transtibial versusindependentdrillingtechniquesforanterior cruciateligamentreconstruction:asystematicreview, meta-analysis,andmeta-regression.AmJSportsMed. 2013;41(11):2693–702.
52.RobinBN,JaniSS,MarvilSC,ReidJB,SchillhammerCK, LubowitzJH.Advantagesanddisadvantagesoftranstibial, anteromedialportal,andoutside-infemoraltunneldrillingin single-bundleanteriorcruciateligamentreconstruction:a systematicreview.Arthroscopy.2015;31(7):1412–7.
53.Rahr-WagnerL,ThillemannTM,PedersenAB,LindMC. Increasedriskofrevisionafteranteromedialcomparedwith transtibialdrillingofthefemoraltunnelduringprimary anteriorcruciateligamentreconstruction:resultsfromthe DanishKneeLigamentReconstructionRegister.Arthroscopy. 2013;29(1):98–105.
54.Alentorn-GeliE,LajaraF,SamitierG,CugatR.Thetranstibial versustheanteromedialportaltechniqueinthearthroscopic bone-patellartendon-boneanteriorcruciateligament reconstruction.KneeSurgSportsTraumatolArthrosc. 2010;18(8):1013–37.
55.XuY,LiuJ,KramerS,MartinsC,KatoY,Linde-RosenM,etal. Comparisonofinsituforcesandkneekinematicsin anteromedialandhighanteromedialbundleaugmentation forpartiallyrupturedanteriorcruciateligament.AmJSports Med.2011;39(2):272–8.
56.GolishSR,BaumfeldJA,SchoderbekRJ,MillerMD.Theeffect offemoraltunnelstartingpositionontunnellengthin anteriorcruciateligamentreconstruction:acadavericstudy. Arthroscopy.2007;23(11):1187–92.
57.ChangCB,YooJH,ChungBJ,SeongSC,KimTK.Oblique femoraltunnelplacementcanincreaserisksofshortfemoral tunnelandcross-pinprotrusioninanteriorcruciateligament reconstruction.AmJSportsMed.2010;38(6):1237–45.
59.LinkoE,HarilainenA,MalmivaaraA,SeitsaloS.Surgical versusconservativeinterventionsforanteriorcruciate ligamentrupturesinadults.CochraneDatabaseSystRev. 2005;18(2):CD001356.