SOCIEDADE BRASILEIRA DE ORTOPEDIA E TRAUMATOLOGIA
w w w . r b o . o r g . b r
Original
Article
Epidemiological
study
on
giant
cell
tumor
recurrence
at
the
Brazilian
National
Institute
of
Traumatology
and
Orthopedics
夽
Roberto
Clayton
Lima
Oliveira
Júnior
∗,
Marcelo
Glauber
da
Silva
Pereira,
Pedro
Braga
Linhares
Garcia,
Patrícia
Albuquerque
dos
Santos,
Amanda
dos
Santos
Cavalcanti,
Walter
Meohas
InstitutoNacionaldeTraumatologiaeOrtopedia(Into),RiodeJaneiro,RJ,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received13August2015 Accepted25August2015 Availableonline18June2016
Keywords: Giantcelltumor Recurrence Epidemiology
a
b
s
t
r
a
c
t
Objective:Giantcelltumorsarebenignboneneoplasmsthatarerelativelyrareinadults andtheirbiologicalbehaviorisstillunpredictable.Theincidenceoflocalrecurrencehas presentedvariationbetween0%and65%instudiesconductedworldwide,butfewdataare availableonthiscomplicationintheBrazilianpopulation.
Methods:Informationon155patientswithconfirmedhistologicaldiagnosesofgiantcell tumorwhoweretreatedinourinstitution’sorthopediconcologyservicebetweenJanuary 2000andJuly2014wasgathered.Demographiccharacteristicswereevaluatedandcompared betweenpatientswhopresentedlocalrecurrenceduringtheclinicalfollow-up.
Results:Localrecurrence wasobservedin26 patients(16.7%),ofwhom 22werefemale (84.6%). Themostcommonsiteoflocalrecurrencewasthedistalfemur(38.4%).Eleven patientspresentedearlyrecurrence,while15caseswerediagnosedafter15months, repre-senting42.3%and57.7%,respectively.Metastaseswereidentifiedinfivepatients(3.2%). Conclusion: Tumor-relatedfactorsdidnotshowanyincreasedincidenceoflocalrecurrence ofgiantcelltumors.Surgicaltreatmentwithanintralesionalmarginisavalidoptionfor treatinglocalrecurrencesanddoesnotshowanydifferenceindisease-freesurvivalin rela-tiontoothertypesofprocedures.Clinicaltreatmentisreservedforcasesofunresectable tumorsorwhensurgicaltreatmentisimpossible.
©2016SociedadeBrasileiradeOrtopediaeTraumatologia.PublishedbyElsevierEditora Ltda.ThisisanopenaccessarticleundertheCCBY-NC-NDlicense(http:// creativecommons.org/licenses/by-nc-nd/4.0/).
夽
StudyconductedatInstitutoNacionaldeTraumatologiaeOrtopedia(Into),RiodeJaneiro,RJ,Brazil. ∗ Correspondingauthor.
E-mail:oliveirajr.roberto@gmail.com(R.C.Júnior). http://dx.doi.org/10.1016/j.rboe.2016.06.004
Estudo
epidemiológico
de
recidiva
de
tumor
de
células
gigantes
no
Instituto
Nacional
de
Traumatologia
e
Ortopedia
Palavras-chave:
Tumoresdecélulasgigantes Recidiva
Epidemiologia
r
e
s
u
m
o
Objetivos: Otumordecélulasgigantes(TCG)éumaneoplasiaósseabenignarelativamente raraemadultos,porémseucomportamentobiológicoaindaéimprevisível.Aincidênciade recidivalocalapresentavariac¸ãoentre0–65%emestudosinternacionais,porémhápoucos dadosreferentesaessacomplicac¸ãoemnossapopulac¸ão.
Métodos:Foramcoletadasinformac¸õessobre155pacientescomdiagnósticohistológico con-firmadodeTCG,acompanhadosnoservic¸odeoncologiaortopédicadanossainstituic¸ão,de janeirode2000ajulhode2014.Ascaracterísticasdemográficasforamavaliadase compara-dasentreospacientesqueapresentaramrecidivalocalduranteoseguimentoclínico. Resultados:Houverecidivalocalem26pacientes(16,7%),dosquais22eramdosexofeminino (84,6%).Alocalizac¸ãomaiscomumderecidivalocalfoiofêmurdistal(38,4%).Onzepacientes apresentaramrecidivaprecoce,enquanto15casosforamdiagnosticadosapós15meses,o querepresenta,respectivamente,42,3%e57,7%.Metástasesforamidentificadasemcinco pacientes(3,2%).
Conclusão: Osfatoresrelacionadosaotumornãoevidenciaramaumentodaincidênciade recidivalocaldetumordecélulasgigantes.Otratamentocirúrgicocommargem intrale-sionaléumaopc¸ãoválidanotratamentoderecidivaslocaisenãoapresentadiferenc¸a desobrevidalivrededoenc¸aentreoutrostiposdeprocedimentos.Tratamentoclínicoé reservadoemcasosdetumoresirressecáveisouimpossibilidadedetratamentocirúrgico.
©2016SociedadeBrasileiradeOrtopediaeTraumatologia.PublicadoporElsevier EditoraLtda.Este ´eumartigoOpenAccesssobumalicenc¸aCCBY-NC-ND(http:// creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
Giantcell tumor(GCT),orosteoclastoma, isaneoplasmof indeterminatemalignancywithlocally aggressivebehavior, composedofmononuclearovoidneoplastictissueuniformly interposedbynumerousgiantcells.1–3
GCTrepresentsapproximately5%ofprimarybonetumors andabout23%ofbenignbonetumors.2,4Itoccursmostoften between20and40yearsofage,withaslightpredominancein females(ratioof1.2:1).Itisconsideredararetumorinchildren andadolescents,5andlessthan10%ofcasesoccurinpatients over65years.6
Themostcommonlocationistheepiphysealregionoflong bonesinskeletallymatureindividuals;itcanalsoaffectthe metaphysealregionofpatientswithopenphysis.1,2Themost affected areasare thedistalfemur, proximaltibia and dis-talradius.Axialinvolvementisunusual.7Despiteitsbenign behavior,thisdiseasecandevelopwithlocalcomplications andmetastasis,especiallyintothelungs.4,8,9
Relapseisdefinedassymptomaticorradiologicevidence of the disease, at least three months after the treatment, andisgenerallydetectedwithinthefirsttwoyearsof follow-up.10RecurrenceratesofprimaryGCTrangefrom0%to65%, dependingonthetypeoftreatmentandtumorsite presenta-tion.Despitetheirbenignnature,pulmonarymetastasesoccur in2–5%ofcases.11
GCTisarelativelyrarebenigntumorinadults;however, itsbiologicalbehaviorremainsunpredictable.Therearemany publishedstudiesthatreporttheexperiencesofinternational groups in developed countries, but there is little informa-tionaboutthedisease’sbehaviorindevelopingcountries.This
articlepresentstheepidemiologicaldataof155patients,with 14 years offollow-up, in a Brazilianorthopedic reference institution.
Methods
Datawere collectedonpatientswithconfirmedhistological diagnosis of GCT, followed-up at the OrthopedicOncology Service from January 2000 to July 2014. This study was approvedbytheethicscommitteeoftheinstitution.
Diagnostic investigation was conductedthrough clinical and radiological evaluation, which included conventional radiography,computedtomography,andmagneticresonance imaging.Subsequently,thepatientsunderwentneedlebiopsy forhistopathologicaldefinition.
Theexclusioncriteriawere:localrecurrenceinlessthan threemonthsaftersurgery;losstofollow-up;andincomplete clinicalandradiologicalrecord.
Theaffectedsite,thepresenceofmetastasesand/or patho-logicalfractures,theperiodofsymptomsevolution,clinical andradiologicalstagingandhistopathologicaldiagnosiswere assessed, as well asthe typeof surgery performed, surgi-calmargin,andtheuseofadjuvants.Thefollow-upperiod, disease-freetime,andlocation/numberofrelapseswerealso assessed.
Patientsweredividedintothreegroups,A,B,andC,
Tumor staging was followed the classification by Cam-panaccietal.,13dividedasfollows:I–quiescent,intraosseous
lesions;II–active,presentingintactperiosteum;III–
aggres-sive,withcortex rupture andinvasion ofsofttissues. This classificationhastherapeutic utility, and wasused tohelp definethesurgicalmarginasintralesional,marginal,wide,or radical.
Surgicaltreatmentfollowedtheprotocolrecommendedby theinstitution,whichprioritizesless aggressiveprocedures that allow joint preservation. Among surgical treatments, intralesional resection associated with the use of spheri-cal dental bur was performed, followed by local filling of bonedefectswithpolymethylmethacrylate(PMMA), autolo-gousbonegraft,orallograft.Extensivesurgerywasperformed incases inwhich tumorextension preventedintralesional resectionorintumorslocatedinexpendablebones,suchas theheadofthefibulaorthedistalulna.
Clinical follow-up was done after 1, 3, 6, 12, 18, and 24 months. After 24 months, evaluations were performed accordingtotherecommendationsoftheattendingphysician. Evaluationsincludedphysicalexaminationandradiological investigation(conventionalandchestX-rays),inordertomake anearlydiagnosisofrecurrencesormetastases.Incaseof sus-pectedlocalrecurrence,complementaryimagingtestswere ordered,whichincludedcomputedtomographyandmagnetic resonanceimaging.
Theoutcomeofthepatientsincludedinthisstudywere classifiedasfavorableorunfavorable,accordingtotheclinical follow-up.Afavorableoutcomeindicatedthatthepatienthad nolocalrecurrenceormetastasisduringfollow-up.Patients whoexperiencedthesecomplicationswereplacedinthe unfa-vorableoutcomegroup.
The data obtainedwas included in adatabase inExcel 2013(Microsoft)andstatisticallyassessed.Thedemographic profilewasdescribedaspercentages,means,standard devia-tions,andminimumandmaximumvalues.Acomparisonof thedemographiccharacteristicsofpatientswithandwithout recurrencewasmadeusingtheMann–Whitneytestandthe associationwastestedusingthechi-squaredtest,atthe95% significancelevel.Event-freesurvivalwasassessedaccording tofollow-uptimeinmonths,consideringthedateofthefirst visituntiltheoccurrenceofthe event(metastasisor recur-rence).Patientswhoremainedalivewerecontacted,andthe dateofthelastconsultationwasregardedastheendof follow-up.Thecumulativesurvivalprobabilitieswereestimatedwith theKaplan–Meiermethodand,forthestatisticalanalysisof thecurvesbetweenclinicalgroups,thelog-ranktestwasused. AllstatisticaltestswereperformedinGraphPadPrismversion 5.00forWindows(GraphPadSoftware–SanDiego,California, USA.[www.graphpad.com]).Ap-value<0.05wasconsidered tobestatisticallysignificant.
Results
FromJanuary2000toJuly2014,158patientswerediagnosedin ourinstitutionwithGCT;ofthese,threewereexcludedfrom thestudy,followingtheaforementionedexclusioncriteria.
Theanalysisincluded155patients;60(38.7%)weremale and95(61.3%),female.Themeanfollow-upperiodwas56.7 months(3.9–158.9).Pathologicalfractureswereobservedin20 patients,representing12.9%ofcases.
Tumors were foundmainly in long bones: 32.9% in the femur (51/155), 29% in the tibia (45/155), and 16.7% in the
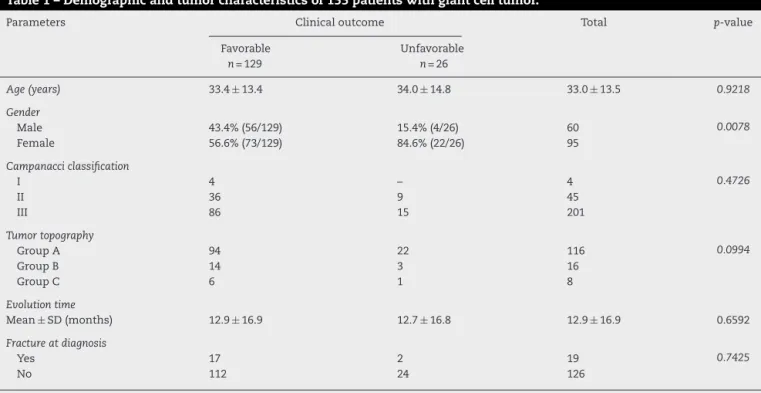
Table1–Demographicandtumorcharacteristicsof155patientswithgiantcelltumor.
Parameters Clinicaloutcome Total p-value
Favorable
n=129
Unfavorable
n=26
Age(years) 33.4±13.4 34.0±14.8 33.0±13.5 0.9218
Gender
Male 43.4%(56/129) 15.4%(4/26) 60 0.0078
Female 56.6%(73/129) 84.6%(22/26) 95
Campanacciclassification
I 4 – 4 0.4726
II 36 9 45
III 86 15 201
Tumortopography
GroupA 94 22 116 0.0994
GroupB 14 3 16
GroupC 6 1 8
Evolutiontime
Mean±SD(months) 12.9±16.9 12.7±16.8 12.9±16.9 0.6592
Fractureatdiagnosis
Yes 17 2 19 0.7425
No 112 24 126
Topography:humerus,radius,femur,tibia. TopographyB:ulna,fibula,talus.
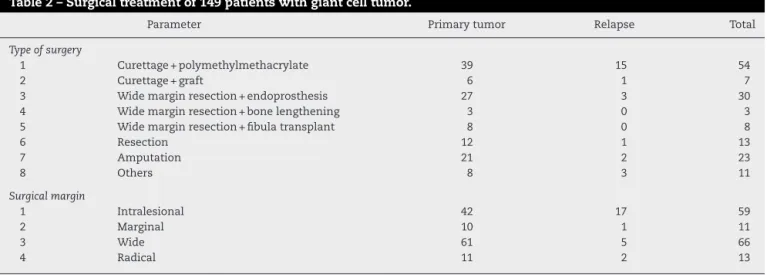
Table2–Surgicaltreatmentof149patientswithgiantcelltumor.
Parameter Primarytumor Relapse Total
Typeofsurgery
1 Curettage+polymethylmethacrylate 39 15 54
2 Curettage+graft 6 1 7
3 Widemarginresection+endoprosthesis 27 3 30
4 Widemarginresection+bonelengthening 3 0 3
5 Widemarginresection+fibulatransplant 8 0 8
6 Resection 12 1 13
7 Amputation 21 2 23
8 Others 8 3 11
Surgicalmargin
1 Intralesional 42 17 59
2 Marginal 10 1 11
3 Wide 61 5 66
4 Radical 11 2 13
radius(26/155),asshowninTable1.GroupAtotaled123cases (79.3%),whileBgrouphad25(16.2%).Aminorityofpatients wereincludedingroupC(sevencases,4.5%).
According to the Campanacci radiological classification, gradesI,II,andIIIrepresented,respectively,2.7%(4/150),30% (45/150),and67.3%(101/150)ofthepatients.Fivepatientshad noradiographic records inthe imagebank, therefore were excludedduetothiscriterion.
Onehundredandfiftypatientsunderwentsurgical treat-ment of the primary lesion, three of them in another institution.Oneofthecaseswasnotincludedinthepresent analysis,asnoinformationontheprocedureperformedcould beobtained(Table2).Fivepatientswerenottreatedsurgically, astheydidnotagreewiththeproposedprocedure.Resection withintralesionalmarginwasaccomplishedin39.3%(59/150) ofpatients;44%(66/150)underwenttreatmentwithwide mar-gin.Marginalandradicalmarginsaccountedfor7.3%(11/150) and8.6%(13/150)ofthecases,respectively.Themost com-monlyperformedprocedure was curettage associatedwith theuse ofPMMA(36%, 54/150),followed bywide resection withuseofunconventionalendoprosthesis(20%;30/150)and amputation(15.3%;23/150).
Localrecurrencewasobservedin26patients(16.7%).The demographiccharacteristicsandtreatmentdataofpatients withandwithoutrecurrencewerecompared.Softtissuelesion wasidentifiedinsixcases.Fifteenpatientsagedbetween20 and40yearsatthediagnosisoftheprimarytumorwere iden-tified,accountingfor57.7%ofrelapsedcases.Eightpatients (30.7%)wereagedover40yearsatinitialdiagnosis.Regarding thegender,22patientswerefemale(84.6%).
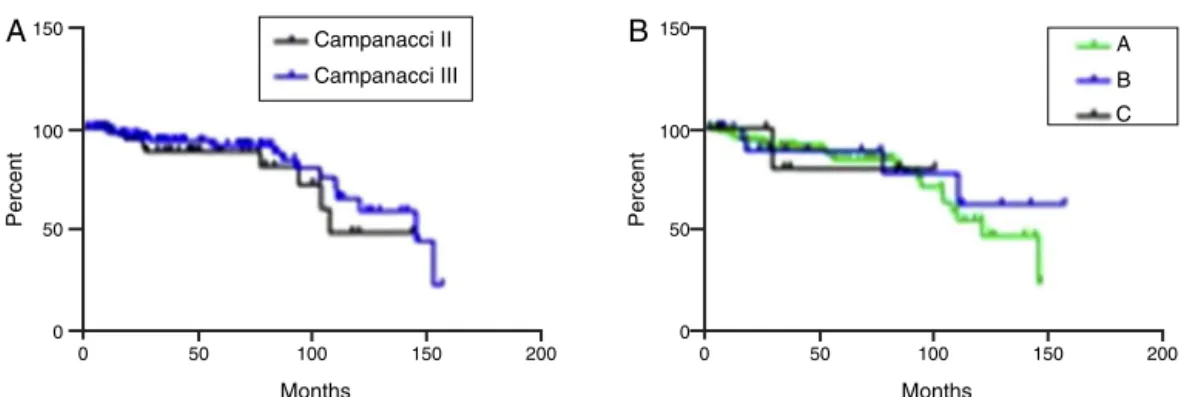
Onepatientfromthegroupthatpresentedrecurrencehad pulmonarymetastasis.Infiveyears,event-freesurvivalwas 88%(Fig.1).ConsideringtheCampanacci groups,therewas nodifference inevent-free survivalatfiveyears:88.5% for CampanacciIIand91.5%forCampanacciIII(Fig.2A).
Simi-larly,consideringthetopographyofgroups,therewasalsono differenceinevent-freesurvival(Fig.2B).
ThehighestnumberofrecurrenceswasobservedinGroup A(n=22;84.6%),followedbyGroupB(n=3;11.5%),andgroup C (n=1; 3.8%). The most common site of local recurrence wasthedistalfemur(n=10;38.4%).Elevenpatientshadearly recurrencewhile15 caseswere diagnosedafter15months,
representing 42.3%and 57.7%,respectively.Fifteenpatients who hadundergone curettageanduse ofPMMAdeveloped localrecurrence.
Twenty-fourpatientsdiagnosedwithlocalrecurrencewere treatedsurgically,sixofwhom(25%)underwent new curet-tageassociatedwiththeuseofPMMA.Fivecases(20.8%)were treatedbywide resectionanduse ofendoprosthesis,while fourpatients(16.6%)underwentamputation.Twopatientsdid notundergosurgerybecausetheydidnotacceptthe surgi-calindication,andweresubmittedtoclinicaltreatmentwith theuseofbisphosphonates(alendronate).Fourpatients pre-sentednewrecurrenceafterthesecondsurgery,andonecase hadathirdrelapse.
Metastases wereobservedinfivepatients(3.2%),among whom onlyone had local recurrence duringevolution. All metastaseswerediagnosedinthelungs.
Afterclinicalfollow-up,30patientsdiagnosedwithprimary GCT(19.3%)hadanunfavorableoutcome;25withdiagnosisof localrecurrence,fourwithmetastases,andonewho devel-opedbothcomplications.
Discussion
Gouin et al.14 did not observe any tumor-related risk fac-tors that increase the incidence of local recurrence after intralesional treatment in appendicular skeleton injuries.
120
100
80
60
40
0 50 100 150
Months
Percent survival
200
150
100
50
0
0 50 100 150 150
Months
Percent
150
100
50
0
Percent
200 0 50 100
Months
200 Campanacci II
Campanacci III
A
B
C
A
B
Fig.2–Event-freesurvivalinpatientswithgiantcelltumorregardingtheCampanacciclassification(A)andtopography(B). GroupAincludedlesionsinthefemur,tibia,humerus,andradius.GroupBcomprisedtumorslocatedinthescapula,fibula, ulna,andbonesofthehandsorfeet.GroupCcomprisedtumorslocatedintheaxialskeleton.
This indicates that the factors related to reduced risk of localrecurrencewereeffectivenessandearlinessofsurgical treatment.12,14Theriskoflocalrecurrenceintumorslocated inthedistalradiusandproximalfemurwashigher,although itwasnotstatisticallysignificant.Theuseofautograftwas consideredanindependentriskfactorforlocalrecurrence.14 Extension to soft tissues and radiological aggressiveness were also reported as prognostic factors, what highlights the importance of the Campanacci classification.13–15 In a meta-analysis,Lietal.16indicatedthatageyoungerthan20 years,tumorslocatedinthedistalradius,andintralesional surgerywith or without bonegrafting may be risk factors forrelapseinappendiculartumors,butthiswasnot statisti-callyconfirmed.16Inthepresentstudy,thesiteswithhighest localrecurrenceratewerethedistalfemur,proximaltibia,and distalradius.Thedemographicparametersevaluatedherein, suchasgender,age,location,andradiologicalclassification, werenotsignificantlyrelatedtotheclinicaloutcome.
Severalfactorsareimportantwheninterpretingtheresults. Inthisstudy,threepatientswhohadbeenpreviouslytreated inotherinstitutionswereincluded.Thismaylimitthe con-clusionsabouttherecurrencerateofthesepatients,sinceit wasnotpossibletoobtainconsistentintraoperativedata.In addition,ourinstitutionisareferencethatreceivespatients fromotherlocations,whichmayaffectthefollow-up.
Surgicaltreatment withlocaldisease control, combined with localadjuvant, is the standard care for appendicular lesions in our institution. The risk of recurrence in these casesis12–18%,consistentwiththedataobtained.14,15 The treatmentusedforprimarylesionswasintralesional curet-tagefollowedbyenlargementofthecavitywithaspherical dentalbur.Thissurgicaloptionislessinvasiveandusually allowsthejointand adjacenttissuetoremaindisease-free. TheadjuvantoptionsarePMMA,hydrogenperoxide,phenol, andcryotherapy.PMMAisthecompoundmostwidelyusedin ourinstitutionduetoitsavailability,easeofapplication,and provenefficacy.TheimpactofPMMAisrelatedtothetoxicand thermaleffectsthatoccurafterapplication,whichpromote betterlocalcontrol.15Widemarginsurgerywasindicatedin caseswheretumorextentpreventedintralesionalresection ortumorsinvolvingexpendable bones,suchastheheadof thefibulaanddistalulna.11
Pelvic injuries are rare, representing approximately 1.5–6.1% ofcases, but they are moreassociatedwith early recurrence and metastasis (7–75% and 2–9.1% of patients, respectively).Duetotheirlocation,somecasesmaybe con-sideredunresectable.ThereisnostandardtreatmentforGCT inthepelvis.Althoughcurettagepreservestheintegrityofthe pelvis,localrecurrenceraterangesfrom6.3%to43%.Wide resection is intended to prevent recurrence, but is associ-atedwithhighratesofcomplications.17Threecasesofpelvic lesions (1.9%) were found, two in the ischium and one in theacetabulum.Localrecurrenceoccurredinonecase,after tumorresectionfromtheischium.AccordingtoGuoetal.,17 thewideresectionofpelviclesionspresentsalowerrateof recurrences,withgoodfunctionalresults.Thesedataare con-sistent withthe clinical outcomes observedin the present study.
GCTlocatedintheaxialskeletonrepresent3–7%ofcasesof boneGCTandupto4%ofvertebralbonetumors.Treatment oftheselesionsisachallenge,assurgerywithintralesional marginisconsideredtobeatechnicallycomplexprocedure withloweffectiveness.Wideresectionwithfreemarginsis hardlyfeasible,duetotheassociatedrisk.Embolizationcan reduceintraoperativebleeding.Radiotherapy hasbeen suc-cessfullyemployedinsomesacrallesions,particularlywhenit isarelapse.18Inthepresentstudy,twosacraltumorsandtwo lumbartumorswereobserved,withoverallincidenceof2.5% ofcases.Twopatientsunderwentsurgicaltreatment: corpec-tomy,andanteriorandposteriorarthrodesis.Onepatientlater receivedradiationtherapyandarterialembolization.Onlyone patientdidnotundergosurgery,duetorefusaloftheproposed treatment. Therewasnoevidenceofrecurrenceduringthe clinicalfollow-up(meanof3.8years).
Yanagisawaetal.19described11casesofGCTdistaltothe radiocarpalandtibiotarsaljoints;fivepatientsweremaleand sixfemale,withameanof24.7years.Thelocationandthe most frequentradiological classificationwere, respectively, themetacarpals(45.45%)andCampanacciII(54.54%).Inthe
presentstudy,13patientswerediagnosedwithlesionsinthe aforementioned topography. The mostcommon siteswere themetacarpals (4/13)and tarsalbones(4/13).Thepatients with injuries classified as Campanacci I or IIwere
classifiedasCampanacciIIIweretreatedwithradicalmargin
–eitheramputationorenblocresection(27.2%).Therewere twocasesoflocalrecurrenceandonecaseoflungmetastasis. Thisfindingwasconsistentwithpreviousstudies.19
The treatment of tumor recurrence is considered con-troversial.According toKlenkeetal.,11resectionwithwide marginsisthemostappropriateoption,duetolower recur-rence rates and longer disease-free survival. Nevertheless, surgery with intralesional margin is a valid option in the treatmentofrecurrentGCT.Thistreatmentshouldbeused regardless of tumor extension to soft tissues; wide mar-gin resection should be reserved for cases where there is extensivebone involvementorinjury tothe neurovascular structures. Wide margin resection often requires complex bonereconstructions, associatedwithhigherratesof surgi-calcomplicationsandfunctionaldeficit.Thepotentialriskof lungmetastases isnotassociatedwiththe typeofsurgery performed.11,12
Recent studies indicate the use of specific clinical treatment in cases of tumors that are considered to be unresectable,especiallythoseinthesacrumandspine.The recommended drugs include bisphosphonates and deno-sumab,whichinhibitthereceptoractivatorofnuclearfactor kappaB(RANK)system.20,21Inthepresentstudy,twopatients diagnosedwithlocalrecurrencedidnotundergosurgery,as theydidnotaccepttheproposedprocedure.Theuseof bis-phosphonates(alendronate)wasofferedasatreatmentoption inthesecases,achievinggoodlocalcontrolduringfollow-up. Themetastasisratefoundinthepresentstudyisconsistent withthatoftheliterature.Fivepatients(3.2%)hadlung metas-tases,amongwhomonlyonehadlocalrecurrenceduringthe follow-up.4,22
Metastases occur primarilyinthe lungs, and their inci-dence isbetween 1%and 9%.22 Riskfactors forthis event includeprimarysite, localrecurrence, andtypeofprimary tumor treatment. The interval between the diagnosis of theprimary tumorand the detectionofmetastasesranges between0 and 10 years (mean of 3.5).The mostcommon primary metastasis sites is the distal radius, followed by the femur and sacrum. Local aggressiveness and multiple recurrenceshavebeenassociatedwithincreasedincidenceof metastases.22Fivepatients(3.2%)hadlungmetastases,among whomtherewasonecaseoflocalrecurrenceduring follow-up.Theprimarysiteswerethedistaltibia(2/5),distalradius (1/5),metacarpal(1/5),andproximalhumerus(1/5).Therewas nostatisticalassociationbetweenlocalrecurrenceortumor locationontheincidenceofmetastasis.
Conclusion
GCT recurrence was observed in 26 patients (16.7%). The factorsrelated tothetumordidnot evidenceanincreased incidenceofthiscomplication, althoughit wasmore com-moninfemales.Surgicaltreatmentwithintralesionalmargin isavalidoptionforthetreatmentoflocalrecurrencesand presentsnodifferenceregardingdisease-freesurvivalwhen comparedtootherprocedures.Clinicaltreatmentisusedin casesofunresectabletumorsorsurgicaltreatment impossi-bility.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1.SchajowiczF.Neoplasiasosseaselesõespseudotumorais.Rio deJaneiro:Revinter;2000.
2.GreenspanA.Radiologiaortopédica.RiodeJaneiro: GuanabaraKoogan;2006.
3.ReidR,BanerjeeSS,SciotR.Giantcelltumour.In:FletcherCD, UnniKK,MertensF,editors.Pathologyandgeneticsof tumoursofsofttissuesandboné.Lyon:IARCPress;2002.p. 310–3.
4.CanalleST.CirurgiaortopédicadeCampbell.Barueri,SP: Manole;2006.
5.CampanacciM.Giantcelltumorofbone.In:Boneandsoft tissuetumors.2nded.SpringerVerlag:Berlin;1999.p.99–132. 6.ColeyBL.Neoplasmsofboneandrelatedconditions.2nded.
NovaIorque:Hoeber;1960.p.196–235.
7.ScottDL,PedlowFX,HechtAC,HornicekFJ.Primarybenign andmalignantextraduralspinetumors.In:FrymoyerJW, WieselSW,editors.Theadultandpediatricspine.
Philadelphia:LippincottWilliams&Wilkins;2003.p.191–245. 8.O’DonnellRJ,SpringfieldDS,MotwaniHK,ReadyJE,Gebhardt
MC,MankinHJ.Recurrenceofgiant-celltumorsofthelong bonesaftercurettageandpackingwithcement.JBoneJoint SurgAm.1994;76(12):1827–33.
9.RockMG,PritchardDJ,UnniKK.Metastasesfrom histologicallybenigngiant-celltumorofbone.JBoneJoint SurgAm.1984;66(2):269–74.
10.DahlinDC,CuppsRE,JohnsonEWJr.Giant-celltumor:astudy of195cases.Cancer.1970;25(5):1061–70.
11.KlenkeFM,WengerDE,InwardsCY,RosePS,SimFH. Recurrentgiantcelltumoroflongbones:analysisofsurgical management.ClinOrthopRelatRes.2011;469(4):1181–7. 12.TakeuchiA,TsuchiyaH,NiuX,UedaT,JeonDG,WangEH,
etal.TheprognosticfactorsofrecurrentGCT:acooperative studybytheEasternAsianMusculoskeletalOncologyGroup.J OrthopSci.2011;16(2):196–202.
13.CampanacciM,BaldiniN,BorianiS,SudaneseA.Giant-cell tumorofbone.JBoneJointSurgAm.1987;69(1):106–14. 14.GouinF,DumaineV,FrenchSarcomaandBoneTumorStudy
GroupsGSF-GETO.Localrecurrenceaftercurettagetreatment ofgiantcelltumorsinperipheralbones:retrospectivestudy bytheGSF-GETO(FrenchSarcomaandBoneTumorStudy Groups).OrthopTraumatolSurgRes.2013;996Suppl:S313–8. 15.BeckerWT,DohleJ,BerndL,BraunA,CserhatiM,EnderleA,
etal.Localrecurrenceofgiantcelltumorofboneafter intralesionaltreatmentwithandwithoutadjuvanttherapy.J BoneJointSurgAm.2008;90(5):1060–7.
16.LiR,HuY.Meta-analysisofriskfactorsofrecurrencein patientswithgiantcelltumoronextremities.ZhonghuaYi XueZaZhi.2014;94(47):3778–83.
17.GuoW,SunX,ZangJ,QuH.Intralesionalexcisionversuswide resectionforgiantcelltumorinvolvingtheacetabulum: whichisbetter?ClinOrthopRelatRes.2012;470(4):1213–20. 18.RaskinKA,SchwabJH,MankinHJ,SpringfieldDS,HornicekFJ.
Giantcelltumorofbone.JAmAcadOrthopSurg. 2013;21(2):118–26.
19.YanagisawaM,OkadaK,TajinoT,TorigoeT,KawaiA,Nishida J.Aclinicopathologicalstudyofgiantcelltumorofsmall bones.UpsJMedSci.2011;116(4):265–8.
symptomaticbenignbonetumors:along-termprospective studyoftoleranceandefficacy.Bone.2014;58:11–6. 21.XuSF,AdamsB,YuXC,XuM.Denosumabandgiantcell
tumourofbone–areviewandfuturemanagement considerations.CurrOncol.2013;20(5):e442–7.