www.bjorl.org
Brazilian
Journal
of
OTORHINOLARYNGOLOGY
ORIGINAL
ARTICLE
Facial
paralysis
after
superficial
parotidectomy:
analysis
of
possible
predictors
of
this
complication
夽
Renato
Fortes
Bittar
∗,
Homero
Penha
Ferraro,
Marcelo
Haddad
Ribas,
Carlos
Neutzling
Lehn
HospitaldoServidorPúblicoEstadual(IAMSPE),SãoPaulo,SP,Brazil
Received9June2015;accepted25August2015 Availableonline19December2015
KEYWORDS Salivarygland neoplasms; Parotidectomy; Superficial parotidectomy; Facialnerve; Facialparalysis
Abstract
Introduction:Salivary glandtumors represent3---10%ofall headandneckneoplasms.These tumorsoccurpredominantlyinmajorsalivaryglands.Theparotidglandisaffectedmostoften, rangingfrom36.6%to83%.Thepleomorphicadenomacomprises45---60%ofallsalivarygland tumors. Severalsurgicalapproacheshavebeendescribedto treatthistumor.Lesion ofthe facialnerveisoneofthemostseriouscomplicationsthatcanoccurafterparotidglandsurgery. Objectives: Todeterminepossiblepredictivefactorsrelatedtotheoccurrenceofperipheral facialparalysis(PFP)aftersuperficialparotidectomyinthesurgicaltreatmentofthe pleomor-phicadenomasoftheparotidgland.
Methods:Thiswasaprimary,observational,case-controlstudyperformedthroughtherevision ofpatients’chartsandhistopathological reports.Datawasobtainedfrom1995to2014.The analyzedeventswere:tumor’slengthanddepth;durationofthediseasereferredbythepatient (morethan1,5or10years);primaryorsecondarysurgicalapproach.
Results:Theanalysisshowedthattumorlengthsequalorsuperiorto3.0cmwereariskfactorof PFPwithanoddsratioof3.98(p=0.0310).Tumordepthsequalorsuperiorto2.0cmwerealso ariskfactorwithanoddsratioof9.5556(p=0.0049|).Whenthetestedeventwassecondary surgerytorecurrenttumorswehavefoundanoddsratioof6.7778(p=0.0029).
Conclusion: Tumorswith3.0cmormoreinlengthand/or2.0cmormoreindepthhavea signif-icanthigherriskoffacialnerveinjury.Secondarysurgerytorecurrenttumorsalsohasamuch higherriskofevolvingwithfacialpalsyaftersuperficialparotidectomy.
© 2015 Associac¸˜ao Brasileira de Otorrinolaringologia e Cirurgia C´ervico-Facial. Published by Elsevier Editora Ltda. This is an open access article under the CC BY license (http:// creativecommons.org/licenses/by/4.0/).
夽 Pleasecitethisarticleas:BittarRF,FerraroHP,RibasMH,LehnCN.Facialparalysisaftersuperficialparotidectomy:analysisofpossible
predictorsofthiscomplication.BrazJOtorhinolaryngol.2016;82:447---51.
∗Correspondingauthor.
E-mails:renatobittar@yahoo.com,rfbittar@gmail.com(R.F.Bittar). http://dx.doi.org/10.1016/j.bjorl.2015.08.024
PALAVRAS-CHAVE Neoplasiasde glândulassalivares; Parotidectomia; Parotidectomia superficial; Nervofacial; Paralisiafacial
Paralisiafacialapósparotidectomiasuperficial:análisedepossíveispreditivosdessa complicac¸ão
Resumo
Introduc¸ão:Ostumoresdeglândulassalivaresrepresentamde3a10%detodasasneoplasiasde cabec¸aepescoc¸o.Essestumoresocorrempredominantementenasglândulassalivaresmaiores. Aglândulaparótidaéafetadanamaioriadasvezes,variandode36,6a83%.Oadenoma pleomór-ficoabrange45---60%detodosostumoresdeglândulassalivares.Diversasabordagenscirúrgicas foramdescritasparaotratamentodessetumor.Alesãodonervofacialéumadascomplicac¸ões maisgravesquepodemocorrerapóscirurgiadeglândulaparótida.
Objetivos: Determinarpossíveisfatorespreditivosrelacionadosàocorrênciadeparalisiafacial periférica(PFP)apósparotidectomiasuperficialnotratamentocirúrgicodeadenomas pleomór-ficosdeglândulaparótida.
Método: Estudopreliminar, observacional, de caso-controle,realizado por meio de revisão dos prontuáriosde pacienteselaudos histopatológicos.Os dadosforamobtidosno período de1995---2014.Oseventosanalisadosforamotamanhodotumornomaiordiâmetroea pro-fundidade,otempodedoenc¸areferidopelopaciente(maisde1,5ou10anos)eaabordagem cirúrgicaprimáriaousecundária.
Resultados: Aanálisemostrouqueotamanhodotumorigualousuperiora3,0cmfoiumfatorde riscoparaPFP,comumrazãodechancede3,98(p=0,0310).Aprofundidadedotumorigualou superiora2,0cmtambémfoiumfatorderisco,comumarazãodechancede9,5556(p=0,0049). Quandooeventotestadofoicirurgiasecundáriaparatumoresrecorrentes,encontramosuma razãodechancede6,7778(p=0,0029).
Conclusão:Ostumoresde3,0cmoumaisdecomprimentoe/ou2,0cmoumaisdeprofundidade apresentamumriscosignificativamentemaiordelesãodonervofacial.Acirurgiasecundária paratumoresrecorrentestambémapresentaumriscomaiordeevoluircomparalisiafacialapós parotidectomiasuperficial.
© 2015 Associac¸˜ao Brasileira de Otorrinolaringologia e Cirurgia C´ervico-Facial. Publicado por Elsevier Editora Ltda. Este ´e um artigo Open Access sob uma licenc¸a CC BY (http:// creativecommons.org/licenses/by/4.0/).
Introduction
Salivaryglandtumorsrepresent3---10%ofallheadandneck neoplasms.1 These tumors occur predominantly in major
salivaryglands.2,3
The parotidglandis affectedmost often,ranging from 36.6%to83%.Malignanttumorsareaminority,occurringin 15---32%ofcases.1,4,5
Themostcommonmalignantandbenigntumorsarethe mucoepidermoidcarcinomaandthepleomorphicadenoma, respectively.6,7
Thepleomorphicadenomacomprises45---60%ofall sali-varyglandtumors.Approximately80%occurintheparotid gland,usuallyin the inferior pole of thesuperficial lobe; however,lessfrequently,itcanoccuratthedeeplobeorin theaccessoryparotidtissue.8
Several surgical approaches have been described to treat this tumor. In 1895, Senn described enu-cleation as the technique of choice. However, tumor removal was incomplete with an unacceptable rate of recurrence.9
Totalparotidectomyremovesallglandtissuelateraland medialtofacialnerve,whereas superficialparotidectomy removesparotidglandlateraltothefacialnerve.In extra-capsulardissection,itisnotperformedanydissectionofthe facialnerve.8,10---14
Lesion of the facial nerve is one of the most serious complicationsthatcanoccurinparotidglandsurgery.Itis estimatedthat30---65%ofallpatientsexperiencesomesort oftransientfacialweakness,and3---6%evolvewith perma-nentdysfunctionresultinginsignificantimpactinthequality oflife.14
Themainpurposeofthisstudywastodeterminepossible predictive factorsrelatedtotheoccurrence ofperipheral facialparalysisaftersuperficialparotidectomyinthe surgi-caltreatmentofthepleomorphicadenomasoftheparotid gland.
Methods
This was a primary, observational, case-control study performed through the revision of patients’ charts and histopathological reports. Data was obtained from 1995 to 2014. Patient’s names were not retrieved; all information was obtained through hospital’s registration numbers.
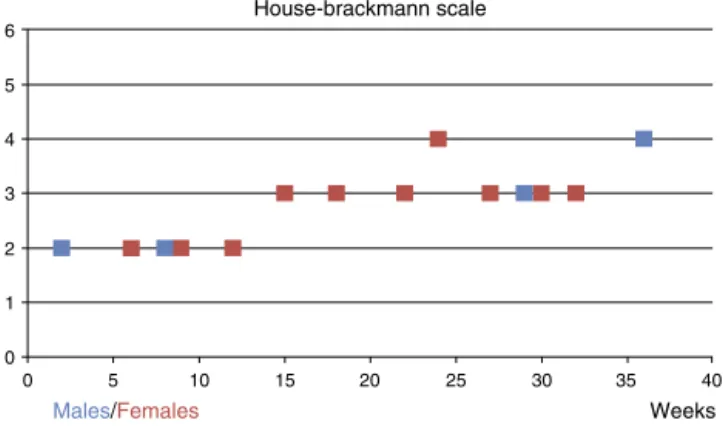
House-brackmann scale
Chart 1. Facial paralysis grade versus elapsed time until complete recovery. 6
5
4
3
2
1
0
0 5 10 15 20 25 30 35 40
Weeks Males/Females
Figure1 Facialparalysisgradeversuselapsedtimeuntil com-pleterecovery.
Wedividedthepatientsintogroupsaccordingtothe stud-iedevent:
Tumorlength
Event analyzed: tumor length ≥0.5cm, 1.0cm, 1.5cm,
2.0cm,2.5cmor≥3.0cm.
Outcome:Peripheralfacialparalysis.
Cases:Patientswhounderwentsuperficialparotidectomy withtumor length greater thanpreviously referred meas-ures.
Controls:Patientswhounderwentsuperficial parotidec-tomy with tumor length smaller than previously referred measures.
Tumordepth
Event analyzed: tumor depth ≥0.5cm, 1.0cm, 1.5cm or
2.0cm.
Outcome:Peripheralfacialparalysis.
Cases:Patientswhounderwentsuperficialparotidectomy with tumor depth greater than previously referred meas-ures.
Controls:Patientswhounderwentsuperficial parotidec-tomy with tumor depth smaller than previously referred measures.
Recurrenceofthedisease
Eventanalyzed:secondarysurgerytotreatrecurrenttumor.
Outcome:Peripheralfacialparalysis.
Cases:Patientswhounderwentsuperficialparotidectomy witharecurrenceofthetumorfromprevioussurgery.
Controls:Patientswhounderwentsuperficial parotidec-tomyforaprimarytumor.
Durationofthedisease
Event analyzed: Time referred by the patient from the momentthelesionwasnoticeduntilsurgicaltreatment.
Outcome:Peripheralfacialparalysis.
Table1 Case-controltable---tumor’slength.
Facialparalysis
Length Yes No
≥3.0cm 10 27
<2.9cm 4 43
Cases:Patientswithdurationofthediseasesuperiorto 1,5or10years.
Controls:Patientswithdurationof thediseaseinferior to1,5or10years.
Facialparalysiswasclassifiedandgraduatedaccordingto House-Brackmann’sscale(HBS).Patientswereevaluatedat thefirstandseventhpostoperativedays;first,thirdandsixth monthsaftersurgery.And,inthefirstyearaftersurgery.
Allpatients whose chartsandhistopathological reports didnotfulfillthesecriteriawereexcludedfromthestudy. Patientswhohave hadanykind offacialmotricity impair-mentprevioustosurgerywerealsoexcluded.
Datawas then analyzed tocalculate odds ratio, confi-denceinterval,z-statistic,andsignificancelevel(p<0.05).
Results
Duringthestudied period219patients weresubmitted to surgical approach in the parotid gland; 157 were due to pleomorphicadenoma.
Afterexcludingthosesubmittedtototalparotidectomy andthosewhose informationwasincompletetherewasa totalof 84 patients whounderwent superficial parotidec-tomy.
Males were 28 patients and females, 56. The average agewas56.7 years(17---89). Average length was2.892cm (0.8---6.0cm)andaveragedepthwas1.880cm(0.5---3.2cm). Therightsidewasaffectedin46cases,andtheleftside,in 38cases.
Facial paralysis occurred in 14 out of 84 patients (16.66%),fourmalesandtenfemales.
Facial paralysis was graded according to HBS. Five patientshadanHBSII,sevenHBSIIIandtwoHBSIV.None wasclassifiedasHBSVorVI.
Timeelapsedfrominitialparalysistocompleterecovery wasevaluatedin weeks.One patientwith HBSII had full recoverywithintwoweeks.Onthe otherhand, anHBS IV patienthadfullrecoveryonlyonthe36thweek.Nopatient remainedwithfacialparalysisafter36weeks.Mediumtime untilfullrecoverywas19.19weeks(Fig.1).
To evaluate tumor’s dimensions several values were sequentiallytestedina0.5cminterval.Regardingtumor’s length we have found no statistical significance when tumor’slengthwaslessthan2.5cm;however,whena3.0cm cutoffpointwassetupwehavefoundanoddsratioof3.98 witha confidence interval of 1.1345---13.9728 (p=0.0310) (Table1).
Thesamewasdonewithtumor’sdepth,andwitha2.0cm depthwehave foundanoddsratioof9.5556witha confi-denceintervalof1.9832---46.0422(p=0.0049)(Table2).
Table2 Case-controltable---tumor’sdepth.
Facialparalysis
Depth Yes No
≥2.0cm 12 27
<1.9cm 2 43
Table 3 Case-control table --- primary versus secondary surgery.
Facialparalysis
Yes No
Secondary 7 9
Primary 7 61
Table4 Case-controltable --- durationofthe disease (1 year).
Facialparalysis
Yes No
≥1year 12 57
<1year 2 13
Table5 Case-controltable --- durationofthe disease (5 years).
Facialparalysis
Yes No
≥5year 0 11
<5year 14 59
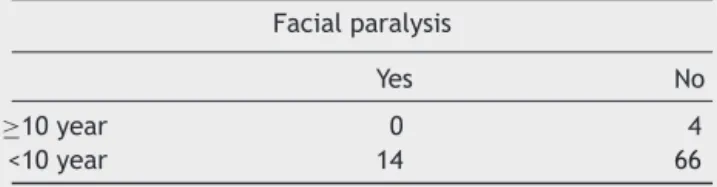
Table6 Case-controltable ---durationofthedisease(10 years).
Facialparalysis
Yes No
≥10year 0 4
<10year 14 66
a confidence interval of 1.9227 to 23.8928 (p=0.0029) (Table3).
Consideringthe durationof the disease,the evaluated parameters were more than 1, 5 and 10 years. We have found oddsratios of 1.3684 with a confidence intervalof 0.2725---6.8709(p=.7032),0.1784withaconfidenceinterval of 0.0099---3.2072 (p=0.2423), and 0.5096 with a confi-denceinterval of0.0260---9.9975 (p=0.6571), respectively (Tables4---6).
Discussion
Thiswasaretrospective, case-controlstudythatanalyzed asignificant numberofpatientsandusedthepleomorphic adenoma’sclinicalandmorphologicalfeaturestodetermine
possiblepredictivefactorsoffacialparalysisafter superfi-cialparotidectomy.
Tothebestofourknowledge,wehavefoundnoprevious similarstudyinthereviewedliterature.
Theexclusionofdoubtfuldataandtheusageofmeasures obtained from high quality clinical and histopathological reportsmadetheevaluationverypreciseandreliable.
Inthisstudy,thesurgerieswereperformedbyresidents under the strict supervision of a senior Head and Neck surgeon. Patients withlarger and/or deeper or recurrent tumorswereoperatedbyseniorsurgeons.
Thismay beconsidered abiasof thestudy sincemore thanonesurgeonperformedthesurgeries;however,thisfact reflectsbesttherealityofmostmedicalresidencecentersin Brazil.Therefore,thisinformationcouldbeusefultopredict andbestpreventthisundesirableoutcomebythehandsof trainingresidents.
Intraoperative neural monitoring (IONM) was not rou-tinely useddue to hospital’s limitation quota. Therefore, itsusewasreservedtorecurrenttumors.
Femaleswere56cases,andmales,28.Ofthe14patients withpostoperativefacialparalysis,10werefemalesandfour weremales. Nopermanentlesionswerereported,andall patients werefullyrecovered within36 weeks.No severe facialparalysis(HBSVor VI)wasalsoreportedduringthe studiedperiod.
Transientfacialpalsyremainsthemostcommon compli-cationinparotidglandtumor14 andanimportantfactor of
distressbothtopatientsandthesurgicalteam.Permanent palsyisseenin0---19%ofthecases.15---21
Ifthelesionispermanenttheconsequencesare tremen-dous,resultinginpossiblecorneaulcers,facialasymmetry, dysphasia,anddrooling.
Superficial parotidectomy remains the most efficient techniqueyet available,allowing thesurgeonthroughthe complete facial nerve dissection, with better chances of preservingitsfunction.22
Itis stilla matter of debate whetherthe incidence of facialparalysisis higheraftermalignanttumorsresection, duetoamoreaggressivesurgicalapproach,23orafterbenign
lesions,usuallywithalongerdurationofthedisease, asso-ciatedwithtumor’sadherenceandadjacent inflammatory process.19
It is quite intuitive to relate the increase of tumor’s dimension to a higher incidence of complications. In this study, we have demonstrated that tumors with3.0cm or moreinlengthand2.0cmormoreindepthhave a signif-icant risk of evolvingwithfacialparalysis. This shouldbe takenintoaccountinthepre-operativeevaluation,and con-sequently,demanda muchmorecarefultechnique during nervedissection.
Allofthe16casesofrecurrenceoccurredafter enucle-ationofthelesionperformedelsewhere,sincethisapproach isnotpreconizedatourinstitution.Asseeninthisstudy,the secondarysurgeryhasamuchhigherriskofresultinginfacial palsy,surelyduetoperilesionalinflammation,fibrosis and lackofanatomicallandmarks.
moreriskysurgeryandduringthesecondarysurgeryitself, sincetherisksoffacialnerveinjuryaresignificantlyhigher. Ontheotherhand,durationofthediseasehadno correla-tionwithahigherriskoffacialnerveinjuryduringsuperficial parotidectomy.Thecalculatedoddsratioswere1.3684with aconfidenceintervalof0.2725---6.8709(p=0.7032);0.1784 with a confidence interval of 0.0099---3.2072 (p=0.2423), and 0.5096 with a confidence interval of 0.0260---9.9975 (p=0.6571),with1,5or10yearsofdisease,respectively.
One might expectto find a higher risk of facial nerve injurywithlongerdiseaseperiod.Theexplanationwhythat wasnotfoundinthisstudyremainsunclear.Furtherstudies focusingat howthe microscopic ultrastructureof tumor’s boundarieschangesovertimemightraisemoreinformation onthismatter.
Conclusion
Facialnerveinjuryduringsuperficialparotidectomyremains themostcommonandmostfearedcomplication.
In this study, we have found that tumors with 3.0cm or morein length and/or 2.0cmor more indepth have a significanthigherriskoffacialnerveinjury.
Secondary surgerytorecurrent tumorsalsohasamuch higher risk of evolving with facial palsy after superficial parotidectomy.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.ForestaE,TorroniA,DiNardoF,deWaureC,PosciaA,Gasparini G, et al. Pleomorphicadenoma and benignparotid tumors: extracapsulardissectionvssuperficialparotidectomy---review ofliteratureandmeta-analysis.OralSurgOralMedOralPathol OralRadiol.2014;117:663---76.
2.LoyolaAM,AraújoVC,deSousaSOM,deAraújoNS.Minor sali-varygland tumors. A retrospective study of 164 cases in a Brazilianpopulation.OralOncolEurJCancer.1995;31:197---201. 3.NandaKDP,MehtaA,NandaJ.Fine-needleaspirationcytology: areliabletoolinthediagnosisofsalivaryglandlesions.JOral PatholMed.2012;41:106---12.
4.KayembeMK,Kalengayi MM. Salivarygland tumorsin Congo (Zaire).OdontostomatolTrop.2002;25:19---22.
5.SatkoI,StankoP,LongauerovaI.Salivaryglandtumorstreated inthestomatological clinicsinBratislava.JCraniomaxillofac Surg.2000;28:56---61.
6.Long-JiangL,YiL,Yu-mingW,Hong-weiZ.Clinicalanalysisof salivaryglandtumorcasesinWestChinainpast50years.Oral Oncol.2008;44:187---92.
7.LimaSS,SoaresAF,deAmorimRF,FreitasR,deA.Epidemiologic profileofsalivaryglandneoplasms:analysisof245cases.Braz JOtorhinolaryngol.2005;71:335---40.
8.ZbärenP,VanderPoortenV,WittRL,WoolgarJA,ShahaAR, Tri-antafyllouA,etal.Pleomorphicadenomaoftheparotid:formal parotidectomyorlimitedsurgery?AmJSurg.2013;205:109---18. 9.Senn N. The pathology and surgical treatment of tumors.
Philadelphia,PA:W.B.Saunders;1895.
10.WittRL.Thesignificanceofthemargininparotidsurgeryfor pleomorphicadenoma.Laryngoscope.2002;112:2141---54. 11.KlintworthN,ZenkJ,KochM,IroH.Postoperativecomplications
afterextracapsular dissection ofbenignparotid lesions with particular reference to facial nerve function. Laryngoscope. 2010;120:484---90.
12.RohJL,KimHS,ParkCI.Randomizedclinicaltrialcomparing partialparotidectomyversussuperficialortotalparotidectomy. BrJSurg.2007;94:1081---7.
13.MalardO,WagnerR,JoubertM,DelemazureAS,RioE,Durand N,etal.Prognosticfactorsforsecondaryrecurrenceof pleo-morphicadenoma:a 20-year,retrospective study.JLaryngol Otol.2013;127:902---7.
14.ZhangSS,MaDQ,GuoCB,HuangMX,PengX,Yu GY. Conser-vation of salivary secretion and facial nerve function in partialsuperficial parotidectomy.Int JOral Maxillofac Surg. 2013;42:868---73.
15.LaccourreyeH,LaccourreyeO,CauchoisR,JouffreV,Ménard M, Brasnu D. Total conservative parotidectomy for primary benign pleomorphic adenoma of the parotid gland: a 25-year experience with 229patients. Laryngoscope. 1994;104: 1487---94.
16.Witt RL. Facial nerve function after partial superficial parotidectomy: an 11-year review (1987---1997). Otolaryngol HeadNeckSurg.1999;121:210---3.
17.Koch M, Zenk J, Iro H. Long-term results of morbidity afterparotidgland surgeryin benigndisease. Laryngoscope. 2010;120:724---30.
18.Guntinas-Lichius O, Klussmann JP, Wittekindt C,Stennert E. Parotidectomy for benign parotid disease at a university teachinghospital:outcome of963operations.Laryngoscope. 2006;116:534---40.
19.GaillardC,PériéS,SusiniB,StGuilyJL.Facialnervedysfunction afterparotidectomy:theroleoflocalfactors.Laryngoscope. 2005;115:287---91.
20.DulguerovP,MarchalF,LehmannW.Postparotidectomyfacial nerve paralysis: possible etiologic factors and results with routine facial nerve monitoring. Laryngoscope. 1999;109: 754---62.
21.O’Brien CJ, Malka VB, Mijailovic M. Evaluation of 242 con-secutiveparotidectomiesperformedforbenignandmalignant disease.AustNZJSurg.1993;63:870---7.
22.JohnsonJT, FerlitoA, FaganJJ,Bradley PJ,RinaldoA. Role oflimitedparotidectomyinmanagementofpleomorphic ade-noma.JLaryngolOtol.2007;121:1126---8.