REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
PublicaçãoOficialdaSociedadeBrasileiradeAnestesiologiawww.sba.com.br
CLINICAL
INFORMATION
Anesthesia
for
lower
extremity
vascular
bypass
with
peripheral
nerve
block
Jordana
de
Fraga
Guimarães
a,∗,
Cristine
Formighieri
Angonese
b,c,
Rafael
Klein
Gomes
b,
Vasco
Miranda
Junior
a,b,
Carlos
Farias
b,daUniversidadeFederaldeCiênciasdaSaúdedePortoAlegre,PortoAlegre,RS,Brazil
bComplexoHospitalardaSantaCasadeMisericórdiadePortoAlegre,Servic¸odeAnestesiologia,PortoAlegre,RS,Brazil cHospitalSírioLibanês,SãoPaulo,SP,Brazil
dHospitalSantaClara,SantaCasadeMisericórdiadePortoAlegre,PortoAlegre,RS,Brazil
Received30June2014;accepted21July2014
Availableonline17September2016
KEYWORDS
Femoralnerveblock; Sciaticnerveblock; Vascularsurgery
Abstract Vascularbypass isa surgical procedurewidely used to treat peripheralvascular disease.Theintraoperativeanesthetictechniqueandthemostappropriatepostoperative anal-gesia for these high-risk patients remain controversial. We present the case of a patient undergoingfemoropopliteal-distalbypassinourservice,presentingwithrelevantcomorbidities tothechoiceofanesthetictechnique.Thispatienthadseveraldeterminingfactorsofdifficult airway,especiallythoracickyphoscoliosis,whichpreventedhimfrombeingproperlypositioned for airwaymanagement, andchroniclung disease.This patient wasalso taken antiplatelet drugs,whichisacontraindicationforneuraxialblock.So,wechosetheanesthetictechnique ofperipheralnerveblock,specificallytheblockadeoffemoralandsciaticnerves.
©2015SociedadeBrasileiradeAnestesiologia.PublishedbyElsevierEditoraLtda.Thisisan openaccessarticleundertheCCBY-NC-NDlicense( http://creativecommons.org/licenses/by-nc-nd/4.0/).
PALAVRAS-CHAVE
Bloqueiodenervo femoral;
Bloqueiodenervo isquiático; Cirurgiavascular
Anestesiaparabypassvascularemmembroinferiorcombloqueiodenervos periféricos
Resumo Acirurgiaparabypassvascularéumprocedimentoamplamenteusadoparao trata-mentodainsuficiênciavascularperiférica.Atécnicaanestésicaparaointraoperatórioepara analgesiapós-operatóriamaisapropriadaparaessespacientesdealtoriscoaindapermanece controversa.Apresentaremosocasodeumpacientesubmetidoabypassfemoropoplíteo dis-tal no nosso servic¸o, que apresentava comorbidades relevantes para a escolhada técnica
∗Correspondingauthor.
E-mail:jordanafguimaraes@yahoo.com.br(J.F.Guimarães). http://dx.doi.org/10.1016/j.bjane.2014.07.020
anestésica. Essepaciente apresentava fatoresdeterminantesde viaaéreadifícil, principal-mentecifoescoliosedacolunatorácica,queoimpediadeserposicionadoadequadamentepara omanejodaviaaérea,alémdeserportador depatologiapulmonarcrônica.Tambémfazia usodeantiplaquetáriosquecontraindicavamobloqueiodeneuroeixo.Porisso,optou-secomo técnicaanestésicapelobloqueiodenervosperiféricos,especificamenteobloqueiodosnervos femoraleisquiático.
©2015SociedadeBrasileiradeAnestesiologia.PublicadoporElsevierEditoraLtda.Este ´eum artigo OpenAccess sobumalicenc¸aCCBY-NC-ND( http://creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
Chronicocclusivearterialdiseaseofthelowerextremities is one of the main forms of atherosclerosis presenta-tion. This pathology, not only for its high prevalence, has a significant morbidity and mortality rate, and many patientsundergovascularbypasssurgeryfortreatment.The anesthetictechniqueforsurgeryandmoreadequate post-operative analgesia inthese high-risk patients undergoing femoropoplitealbypassremains controversial. We present the case of a patient with significant comorbidities for the choice of the anesthetic technique who underwent femoropoplitealbypassinourhospital.
Case
report
IAB (male patient), 75 years old, white, presenting with congestive heart failure (class II), ischemic heart disease (acutemyocardial infarctionthree yearslater, with coro-narystentimplantation),chronicatrial fibrillation,former smoker (quit smoking for 13 years). He also had impor-tant scoliosis and thoracolumbar kyphosis. Distal right femoropoplitealbypassfor atherosclerotic peripheral vas-culardiseasewasproposed.Thepatientreportsnothaving heartandrespiratorysymptomsduringdailyactivities, func-tionalcapacityof4METs,thoughdifficulttoassessclinically. Classified as ASA III; denies allergies; takenthe following medications:aspirin200mg.day−1,clopidogrel75mg.day−1,
pentoxifylline 400mg 2×.day−1, simvastatin 40mg.day−1,
furosemide40mg.day−1,isosorbide10mg3
×.day−1,digoxin
0.25mg.day−1andomeprazole20mg.day−1.
Account of previous procedures: angioplasty with stenting (2011) with sedation, left popliteal angioplasty (2011) with sedation and amputation of the left forefoot (2011) with regional block, all uneventful. Complete fast for eighthours.The patientandhisfamilywereinformed about the surgical andanesthetic procedure andpossible complications.Afteracceptingtheanestheticprotocol,the informedconsentformwassigned.Onphysicalexamination, weight51kg,height1.70m,blood pressure150/70mmHg, heart rate 88bpm; lucid, oriented, and collaborative; cardiacauscultationwithirregularrhythm,normalsounds, without murmurs; respiratory auscultation reveled breath soundswithout adventitioussounds. Mallampati4, limited neckmobility.Hehadimportantscoliosisandthoracicspine
kyphosis, which prevents the supine position; claims to beabletosleeponlyin thelateralposition.Preoperative tests: hemoglobin 14g.dL−1; hematocrit 41%; platelets
22,4000mL; creatinine 1.5mg.dL−1; urea 53mg.dL−1;
potassium 4.3mEq.L−1; sodium 141mEq.L−1; INR 1, APTT
38/2;ECG withventricularrate of 100beats.min−1, atrial
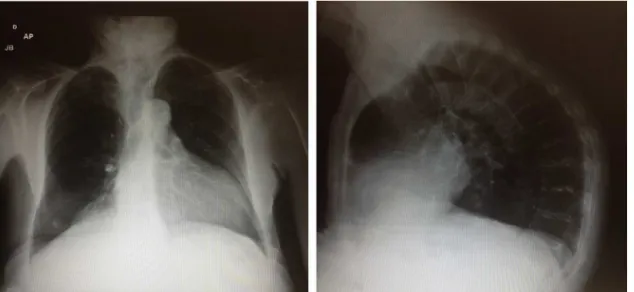
fibrillation and inferoposterior inactive zone; chest X-ray withincreasedheartvolumeandnodularimageintheright lungbase(Fig.1).
In the operating room, the patient was placed supine with back and neck supported on cushions, so that the head remained supported (Fig. 2). Monitoring performed with cardioscopy, pulse oximetry, and noninvasive blood pressure.Peripheralvascularaccessperformedwith Abbo-cath 18G. Oxigen (3L.min−1) was offered through nasal
catheter.Materialfor difficult airwaypreparedintheOR. Intravenous cefazolin 1g wasadministered. Sedation was performedinitiallywithbolusmidazolam1mgandfentanyl 75 mcg.Femoral and sciatic nerve block was performed, infraglutealapproach(Rajtechnique)withtheaidof neu-rostimulatorandA100mmneedle.Ropivacaine0.75%(total dose 300mg)+lidocaína 1% were administered without vasoconstrictor (total dose 50mg). Intraoperatively, the patientreceivedcontinuousinfusionofpropofol,clonidine, and ketamine, maintaining a conscious sedation level. Duringtheprocedure,heparin5000unitswasadministered before clamping the femoral artery and reversed with protamine2500unitsbytheendofsurgery.Theprocedure lastedthreehoursand30minwithoutcomplications.Inthe postoperativevisitthenextday,thepatientpresentedwith minimal pain in the right lower limb (3/10 on numerical scale) and without motor blockade; he was receiving analgesiawith oral non-opioid analgesics and intravenous anti-inflammatory.
Discussion
Figure1 PreoperativechestX-ray.
Nonsurgical treatment includes control of risk factors, exercise, and drug therapy. Surgical treatment options include percutaneous endovascular techniques and sur-gical repairs. The indications for revascularization or bypasssurgery for occlusions belowthe inguinal ligament include intermittent claudication, ischemic rest pain, or ulceration/gangrene.1Usually,theusedautologousgraftis
saphenousvein,andpatencyratesandwiththisapproach are59%in5yearsand38%in10years.2,3
Inthepreoperative evaluation,it isimportanttoknow the drugs routinely used by patients. Antiplatelet and/or anticoagulant are veryoften prescribedand guidance for suspension/maintenance must be evaluated individually
and together with the surgical team. For patients with chronic use of beta-blockers and aspirin, itsmaintenance isimportant.3
The intraoperative anesthetic technique and the most appropriate postoperative analgesia for these high-risk patientswithchronicperipheralvasculardisease undergo-ing femoropopliteal bypassremains controversial. Several techniqueshavebeensuccessfullyusedforlowerlimb vas-cularreconstruction,suchasgeneralanesthesia(balanced ortotalintravenous),regionalanesthesia(spinalor epidu-ral),orcombined.Peripheralnerveblocksareanalternative togeneralanesthesiaandregionalneuraxialblocksinsome infrequentclinicalsituations.2,4
General anesthesiaoffers theadvantageofeasy hemo-dynamiccontrolduringsurgeryandnopatientdiscomfortin longprocedures;however,itdoesnotinhibitpostoperative hypercoagulability.Ontheotherhand,regionalblockadeis effectiveinblockingtheresponsetosurgical stressandin postoperativeanalgesia;however,itisadifficulttechnique, particularlyinpatientswhoareobese,uncooperative,with kyphoscoliosisor previous spinalinstrumentation, in addi-tion to its limited duration for long procedures, such as spinalanesthesia.Anotherpointtobeconsideredisthe com-monuseofantiplatelets,anticoagulants,andthrombolytics inthispopulationthatcontraindicatetechniquesaddressing theneuraxis.2,5
Inthiscontext,manyauthorshaveconsideredtheuseof peripheral nerve block techniques, especially when there is relative contraindication to regional block due to the use of drugs affecting coagulation. Postoperative analge-sia induced by peripheral nerve block techniques can be extended forupto24h. Astheairwayinstrumentation or theuseofinhaledagentsor neuromuscularblockersisnot required, it is a good option for patients withsignificant pulmonarydisease.
The useofthistechnique,however,mustbedonewith cautioninanticoagulatedpatients,particularlyifthenerve tobeblockedisclosetodeepormajorvascularstructures. Oneshouldalsobeawareofsystemictoxicityrelatedtohigh dosesoflocalanesthetics, usuallyrequired forlowerlimb blockades.2 Lowerlimbperipheral nerveblock
contraindi-cationsarepatientrefusal,coagulopathy, infectionat the puncturesiteandsystemic,hypersensitivitytolocal anes-thetics,andpreviousneurologicaldamage.Possibleadverse effects include neurological damage by intraneural injec-tion, local anesthetic intoxication, local and/or systemic infection,andbruisingatthepuncturesite.6,7
In short, one should opt for the specific anesthetic technique for each patient and more familiar to each institution.2 Regardlessof thetechniqueused,theoverall
improvementofperioperativecaremustbeemphasized,as itis thesinglemostimportant factorrelatedtoimproved postoperativeoutcomes.3
Intraoperativemonitoring,besidescontinuousECGwith ST-segment analysis, should include in most cases intra-arterial pressure, in order to improve blood flow to the operated limb andfacilitate bloodsample collection. The indwellingcatheterisroutineduetothedurationofsurgery and to assess intravascular volume. The central venous access should be considered in patients with significant renalorheartfailureorthosewithinappropriateperipheral venousaccess.2,3
Morbidity and mortality in this kind of surgery is mainly of cardiac origin, often appears in the postop-erative period. The incidence of perioperative cardiac events is 10 times higher in patients undergoingvascular surgery than in non-vascular surgical patients. The pub-lishedstudiescomparinggeneralversusregionalanesthesia for lower limb bypass showed no significant differences in mortality, myocardial infarction, myocardial ischemia, or congestive heart failure. Only some changes in sec-ondaryorcombinedcardiacoutcomeswerefoundinsome studies.2,3
Asecondarybutsignificantclinicalfindingofthese stud-iesisthebeneficialeffectofregionalanesthesiaonlower
limb graft patency in the postoperative period. Regional anesthesia was associated with a five-fold reduction of the vascular graft occlusion rate. Most graft occlusions occur between the first and third day after surgery, and this difference in outcome between different anesthetic techniques remained for a longer period (six weeks or more).
One possible explanation for this finding is that gen-eralanesthesiais associatedwitha hypercoagulablestate postoperatively(increasedlevelsoffibrinogenandplatelet reactivityassociatedwithsurgicalstress),whichismitigated byregional anesthesia. Anothermechanism for increasing lowerlimbgraft patencywithregionalanesthesiamaybe theincreased blood flow tothe limb associated withthe sympathectomy.2,3
Postoperative analgesia and anxiety are an important pointto beconsidered, asthe response tosurgical stress and risk of myocardial ischemia are maximum in that moment. Epidural techniques with local anesthetics and opioids administered by continuous infusion or patient-controlledanalgesiaandintravenoustechniquesclassically administeredbypatient-controlledanalgesiaareboth cor-relatedwithgoodpaincontrol.
Theintravascularvolumeshouldbeenhancedwith care-ful control of heart rate and blood pressure. One should beawareof thesympathectomyresolutiontime,withthe intravascularspace contractionand therisk ofcongestive heart failure. Anemia should be avoided by maintaining hemoglobin above 9g.dL−1. Peripheral pulses should be
checkedfrequentlytoassessthegraftpatency.3
Sciaticnerveblock----posteriortechnique(Raj’s technique)
Sciaticnerveblockiseasyandquicktoperformwhenusing neurostimulatorand/orsonographictechniques.Besidesits uncommoncomplications,itisagoodtechniqueforlower limbanesthesiaandanalgesia.Itcanbecombinedwithother blocks,suchasfemoralorsaphenousnerveblockade,to vir-tuallyanysurgical procedurebelow thekneethatrequire notourniquet(femorocutaneous,obturator,femoral,3-1or saphenous).Associatedwithfemoralnerveblock,itprovides knee,leg,andfootanalgesia.Associatedwithposterior lum-barplexusblock,itprovidesfemur,thigh,knee,leg,andfoot analgesia.6
The sciatic nerve is formed by the union of the lum-bosacral trunk L4---L5 and anterior branches of the S1---S3 roots.6,8 This is the largest of the four major peripheral
nervesinlowerlimbs.Itemergesfromthepelvisthroughthe sacrumsciatic foramen, passes below thepiriformis mus-cleinadeepplane inthe glutealregion,then goesdown themidline of the back of the thigh, and divideitself in thepoplitealfossaintibialnerveandfibular(orperoneal) commonnerve.
for sensory and motor innervation throughout the back of the leg and plantar foot (plantar flexion). The com-monperoneal nerve is responsible for sensory and motor innervation of the entire dorsal surface of the foot (dorsiflexion).3,6
Severalapproacheshavebeenreportedforsciaticnerve block.Duetoitsgreatlength,itcanbeblockedatvirtually anypoint.Inourpatient,wechoseRaj’stechnique (poste-riorapproach).Forsuch,thepatientshouldbeplacedinthe lithotomyposition,supportedbyanassistant.Thereference pointsarethegreatertrochanterandtheischialtuberosity (ischium),inwhichalineshouldbedrawn.A22G,9cm nee-dlewiththeneurostimulatorisinsertedperpendiculartothe skininthemiddleofthislineandslowlyadvanced,withan initialcurrentof2mA.
The tibial nerve expected motor response is plantar flexion of the foot and toes; and the common peroneal nerveresponseisdorsiflexionorfooteversionandextension of the toes. The reported local anesthetics are bupiva-caine 0.375% with or without vasoconstrictor, lidocaine 1.5%withorwithoutvasoconstrictor,ropivacaine0.5---0.75% withvolumesofapproximately20---30mL.Localanesthetic shouldbeinjectedwithaminimalevokedmuscleresponse of 0.5mA. It should be noted that this technique does not block the posterior cutaneous nerve of the thigh and an assistant is required for properly positioning the patient.3,6,8,9
Femoralnerveblock
The femoral or crural nerve is also a quick and easy procedure to be performed; it may be combined with otherregional blocks(femoralcutaneous,obturator, 3-1). The technique may beapplied withor without nerve sti-mulator aid (doubly guided). Classically, this blockade is usedfor anesthesia and postoperative analgesia for knee (arthroplasty, reconstruction of the anterior and poste-riorcruciateligament,tibialplateaufracture,andpatella fracture), hip (arthroplasty, femoral neck fracture), and thigh(transtrochanteric, diaphysealfemoral, andfemoral condylefractures)surgeries.Thisblockadeisalsousefulto facilitatethetransportandplacementofpatientswithhip fracture,earlyphysicaltherapyrehabilitation,aswellasfor earlymobilizationofpatients.7,8
FemoralnerveisformedbytherootsofL2---L4,entersthe thighposteriortotheinguinalligamentandpasseslaterally tothefemoralvessels.Itislocatedinaslightlydeeper posi-tion(0.5---1.0cm)andlateraltothefemoralartery(about 1.5cm).Therearetwofascias:fascialata,whichpassesover thenerveandover thevessel,andiliacfasciathatpasses over the nerve, but below the femoral vessels. This sup-pliesmotorinnervation totheanteriorthighmusclestore and originates the internal saphenous nerve, which is a sensory branch to the internal anterior side of the knee andleg.3,7,8
Femoral nerveblock providesanalgesiain the anterior sideofthethighskin,mostofthehipjoint,femoral perios-teum,kneejoint,quadricepsmuscle,andskinofthemedial sideof the leg andfoot (saphenoussensory branch).In a variablepercentageofpatients,thisblockadealsoextends tothethighlateralcutaneous(analgesiaoftheskinonthe
lateralsideofthethigh)andobturatornerves(medialthigh andadductormusclesofthethigh),andthuscontributesto analgesiaofhipandkneejoints.7---9
The patient should be positioned supine and the leg to be blocked should be slightly rotated externally. Ref-erence pointsarethe anteriorsuperior iliacspine, lateral edge of the pubis, and inguinal ligament. One should palpate the femoral artery pulse, protect it with two fingers ---- 2cm below the inguinal ligament and 1cm lateral to the femoral artery pulse is the intradermal injection point. The neurostimulation needle (22G, 4cm) should be slowly introduced in cranial direction. The expectedmotorresponseistheupwardjerkofthepatella and quadriceps contraction with 0.3---0.5mA. The vol-ume of local anesthetic used is 20---30mL after negative aspiration.3,7,8
Thepresenceoffemoralvasculargraftisarelative con-traindicationtothistechnique.Furthermore,theremaybe importantanatomicalvariations,suchasfemoralnervefar fromfemoralarteryorthinandwidefemoralnerve,which canhampertheblockade.7
Conclusion
There are several possible anesthetic techniques for patients undergoing femoropopliteal bypass. In this case, the patient’s condition, associated with the presence of various comorbidities, difficult airway, severe pulmonary disease, spinal deformity, as well as a formal contraindi-cationtoneuraxialblockade,ledustochoosetheregional anesthesia. Thus, aftertaking all precautionsand options tomanageadifficultairwayifnecessary,wechose periph-eral nerve block asan anesthetic technique, in this case the blockade of femoral and sciatic nerves. The surgery wentsafely anduneventfulandwithoutdiscomforttothe patient,inadditiontoprovidingaqualityandsatisfactory postoperativeanalgesiaforthepatient.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.Helayel PE, Conceic¸ão DB, Feix C, et al. Bloqueio isquiati-cofemoral guiado por ultrassom para revisão de coto de amputac¸ão. Relato de caso. Rev Brasil Anestesiol. 2008;58: 480---4.
2.MillerRD,ErikssonLI,FleisherL,Wiener-KronishJP,YoungWL. Miller’sAnesthesia.7thed.ChurchillLiverstone:Londres;2013. 3.CangianiLM,SlullitelA,PotérioGMB,etal.Tratadode
anestesi-ologia.7thed.SãoPaulo:EditoraAtheneu;2011.
4.Yazigi A, Madi-Gebara S, Haddad F, et al. Combined sci-atic and femoral nerve blocks for infrainguinal arterial bypass surgery: a case series. J Cardiothorac Vasc Anesth. 2005;19:220---1.
5.NooraniR,RockP.Regionalversusgeneralanesthesiaforvascular surgerypatients.AmSocAnestesiol.2009.
RiodeJaneiro:SociedadeBrasileiradeAnestesiologia/SBA;2013. p.369---82.
7.RuziRA.Bloqueiodonervofemoral.In:LuizMarcianoCangiani, EduardoRenNakashima,etal.,editors.Atlasdetécnicasde blo-queiosregionais.3rded.RiodeJaneiro:SociedadeBrasileirade Anestesiologia/SBA;2013.p.391---6.
8.JegierMA,LeoneFJ,etal.ManualdeAnestesiologia:Conceitos eAplicac¸õesparaaPráticaDiária.3rded.PortoAlegre:Artmed; 2007.