w w w . r e u m a t o l o g i a . c o m . b r
REVISTA
BRASILEIRA
DE
REUMATOLOGIA
Original
article
Secondary
hyperalgesia
occurs
regardless
of
unilateral
or
bilateral
knee
osteoarthritis
involvement
in
individuals
with
mild
or
moderate
level
Vanessa
Martins
Pereira
Silva
Moreira
a,∗,
Saulo
Delfino
Barboza
a,
Juliana
Borges
Oliveira
b,
Janser
Moura
Pereira
c,
Valdeci
Carlos
Dionisio
aaUniversidadeFederaldeUberlândia(UFU),FaculdadedeMedicina,ProgramadeMestradoemCiênciasdaSaúde,Uberlândia,MG,
Brazil
bUniversidadeFederaldeUberlândia(UFU),FaculdadedeEducac¸ãoFísica,Uberlândia,MG,Brazil cUniversidadeFederaldeUberlândia(UFU),FaculdadedeMatemática,Uberlândia,MG,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received12October2015 Accepted6February2016 Availableonline13April2016
Keywords:
Kneeosteoarthritis Pain
Pressurepainthreshold Secondaryhyperalgesia
a
b
s
t
r
a
c
t
Background:Secondary hyperalgesia in individuals with less severe levels of knee osteoarthritisremainsunclear.Theobjectiveofthisstudywastomeasurethepressure painthresholdofindividualswithmildormoderatekneeosteoarthritisandcomparewith noosteoarthritis.
Methods:Tenhealthycontrolsand30individualswithmildormoderatekneeosteoarthritis dividedintotwogroups(unilateralandbilateralinvolvement)wereincluded.Dermatomes inlumbarlevels(L1,L2,L3,L4andL5)andsacrallevel(S1andS2),myotomes(vastus medi-alis, vastuslateralis,rectusfemoris,adductor longus,tibialisanterior,peroneuslongus, iliacus,quadratuslumborum,andpopliteusmuscles),andsclerotomesinlumbarlevels (L1-L2,L2-L3,L3-L4,L4-L5supraspinousligaments),overtheL5-S1andS1-S2sacralareas, pesanserinusbursae,andatthepatellartendonpressurepainthresholdwereassessedand comparedbetweenindividualswithandwithoutkneeosteoarthritis.
Results:Kneeosteoarthritisgroups(unilateralandbilateral)reportedlowerpressurepain thresholdcomparedtothecontrolgroupinmostareas(dermatomes,myotomes,and scle-rotomes).Therewerenobetweengroupdifferencesinthesupra-spinousligamentsandover theL5-S1andS1-S2sacralareasofthesclerotomes.Nodifferencewasseenbetweenknee osteoarthritis.
Conclusion: Thesefindingssuggestthatindividualswithmildtomoderateknee osteoarthri-tis had primary and secondary hyperalgesia, independent of unilateral or bilateral involvement.Theseresultssuggestthatthepainhavetobeanassertivefocusintheclinical practice,independentofthelevelofseverityorinvolvementofkneeosteoarthritis.
©2016ElsevierEditoraLtda.ThisisanopenaccessarticleundertheCCBY-NC-ND license(http://creativecommons.org/licenses/by-nc-nd/4.0/).
∗ Correspondingauthor.
E-mail:vanessamartinsfisio@gmail.com(V.M.PereiraSilvaMoreira). http://dx.doi.org/10.1016/j.rbre.2016.03.014
A
hiperalgesia
secundária
ocorre
independentemente
do
envolvimento
unilateral
ou
bilateral
da
osteoartrite
de
joelho
em
indivíduos
com
doenc¸a
leve
ou
moderada
Palavras-chave: Osteoartritedejoelho Dor
Limiardedoràpressão Hiperalgesiasecundária
r
e
s
u
m
o
Introduc¸ão: Aocorrênciadehiperalgesiasecundáriaemindivíduoscomníveismenosgraves de osteoartritede joelhoaindaéincerta.Oobjetivodesteestudofoimedirolimiarde doràpressãodeindivíduoscomosteoartritedejoelholeveoumoderadaecompararcom indivíduossemosteoartrite.
Métodos: Foramincluídos10controlessaudáveise30indivíduoscomosteoartritedejoelho leveoumoderada,divididosemdoisgrupos(envolvimentounilateralebilateral).Foi avali-adoecomparadoolimiardedoràpressãoemdermátomosnosníveislombares(L1,L2, L3,L4,L5)eníveissacrais(S1eS2),miótomos(músculosvastomedial,vastolateral,reto femoral,adutorlongo,tibialanterior,fibularlongo,ilíaco,quadradodolomboepoplíteo) eesclerótomosnosníveislombares(ligamentossupraespinaisL1-L2,L2-L3,L3-L4,L4-L5), sobreasáreassacraisL5-S1eS1-S2,bolsaanserinaetendãopatelarentreosindivíduos comesemosteoartritedejoelho.
Resultados: Osgrupososteoartritedejoelho(unilateralebilateral)relatarammenorlimiar dedoràpressãoemcomparac¸ãocomogrupocontrolenamaiorpartedasáreas (dermá-tomos,miótomoseesclerótomos).Nãohouvediferenc¸asentreosgruposnosligamentos supraespinaiseaolongodasáreassacraisL5-S1eS1-S2dosesclerótomos.Nãofoiobservada qualquerdiferenc¸aentreosindivíduoscomosteoartritedejoelho.
Conclusão: Essesachadossugeremqueosindivíduoscomosteoartritedejoelholevea mod-eradatinhamhiperalgesiaprimáriaesecundária,independentementedoacometimento unilateraloubilateral.Essesresultadossugeremqueadorprecisaserumfocoassertivona práticaclínica,independentementedograudegravidadeouenvolvimentodaosteoartrite dejoelho.
©2016ElsevierEditoraLtda.Este ´eumartigoOpenAccesssobumalicenc¸aCC BY-NC-ND(http://creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
Thekneeisthemostcommonjointaffectedby osteoarthri-tis, and the prevalence increases with aging.1 Pain is the
mainsymptomofkneeosteoarthritis(KOA),anditspresence andseverityareimportantdeterminantsofdecreased func-tionalcapacity.2,3 Primaryhyperalgesiahasbeendefinedas
increasedactivityofprimaryafferentnociceptorsatthesite ofadeterminedinjuredtissue,whilesecondaryhyperalgesia isdefinedaspresenceofpain inareasbeyondtheoriginal injuredarea.4Primaryandsecondaryhyperalgesiamayoccur
inKOAand resultinmodulation ofnociceptorsand spinal hornneurons,respectively.5
Thepressure pain threshold (PPT) has been considered
the most reliable parameter to classify inflammation in
osteoarthritis,6,7 and hasbeen usedtodetect the presence
ofsecondary hyperalgesia indermatomes, myotomes, and
sclerotomes.2,5 PPTseems tohavedifferent levels between
individualswithandwithoutosteoarthritis,2,8however,
cur-rent evidence does not answer if PPT levels are different betweenthe different severities(e.g., mildor moderate) of KOA.2,9,10Inthepast,Gerecz-Simonetal.11evaluated
individ-ualswithkneeOA,butjustpainwasmildandmoderate.Also, theyusedonlytwopointsinlowerlimb.Recently,ithasbeen
demonstrated that individuals withmoderate KOA present
localizedpainandnotcontralateralhyperalgesia,12however,
in this study, although not mentioned, the characteristics
ofthe participantssuggests that individualshad unilateral KOA.Therefore,assessingPPTinmultiplespointsmightbring meaningfulinformationaboutthepain,aswellascontribute to clinical approach. As joint damage occurs gradually in osteoarthritis (i.e., with progressive function loss oftissue stabilizers),13 secondary hyperalgesiawould beexpectedto
occurinthedevelopmentprocessofosteoarthritis,and uni-lateral orbilateral involvementmightplayaroleon this,14
resultingindifferentpainfulpoints.Thus,thisstudyaimed tomeasurethePPTlevelsinmildormoderateKOA individ-ualswithunilateralandbilateralinvolvementandcompareto individualswithoutKOA.Wehypothesizedthatsomelevelof secondaryhyperalgesiawouldbepresentinindividualswith mildandmoderateKOAandwouldbeeffectofunilateralor bilateralinvolvement.
Materials
and
methods
Participants
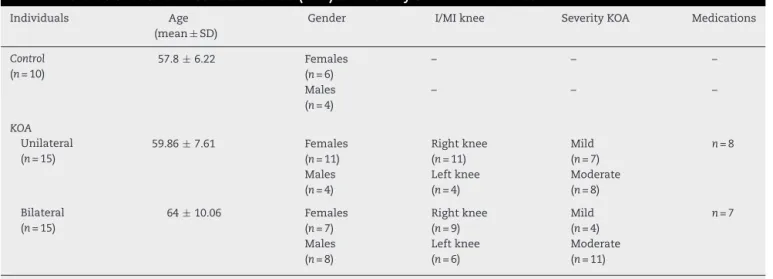
Table1–Characteristicsofkneeosteoarthritis(KOA)andhealthycontrolindividuals.
Individuals Age
(mean±SD)
Gender I/MIknee SeverityKOA Medications
Control (n=10)
57.8±6.22 Females
(n=6)
– – –
Males (n=4)
– – –
KOA Unilateral (n=15)
59.86±7.61 Females
(n=11)
Rightknee (n=11)
Mild (n=7)
n=8
Males (n=4)
Leftknee (n=4)
Moderate (n=8)
Bilateral (n=15)
64±10.06 Females
(n=7)
Rightknee (n=9)
Mild (n=4)
n=7
Males (n=8)
Leftknee (n=6)
Moderate (n=11)
SD,standarddeviation;I,involvedkneeinunilateralKOA;MI,moreinvolvedkneeinbilateralKOA.
Forinclusion,individualsshouldbe50-years-oldormore, have diagnosed KOA in the evaluation (unilateral or bilat-eral),andpainforatleast6months.Thediagnosis ofKOA wasbased onthe classificationoftheAmerican Collegeof Rheumatology,15 accompanied by radiological evidence of
osteoarthritisaffectingoneormorecompartments,according totheradiologicalcriteriaofKellgrenandLawrence.16
Indi-vidualswereexcludediftheyhadanyofthefollowing:other musculoskeletaldisorders;chronicdiffusepain(fibromyalgia),
chronicinflammatoryconditions, suchasautoimmune
dis-eases(rheumatoid arthritis,lupus, gout);diabetes mellitus; neuromusculardisorders,suchasParkinson’sdisease;vertigo orotherconditionsthatcouldaffectthesensorycapabilities andcontrolofmovement.Individualswhousedcentral con-trolofpainmedications,suchasantidepressantsalsowere excluded, but individuals who usedoralnonsteroidal anti-inflammatorydrugs,itwasallowedtocontinueitsuse.
Afterselection,30individualswithKOAwereincluded.Ten individualsolderthan50yearswhohadnohistoryofinjury, surgery,andpaininthe lowerextremitieswereselectedby conveniencetocomposethecontrolgroup.Allincluded par-ticipantssignedtheinformedparticipationconsent,andwere dividedintothreegroups:bilateralKOA(n=15),unilateralKOA (n=15)and control (n=10). Table 1shows the participants’ characteristics.
Painassessment
Adigitalforcegauge(ForceTENTMFDX,WagnerInstruments,
Greenwich,CT,USA)and withaflat
½
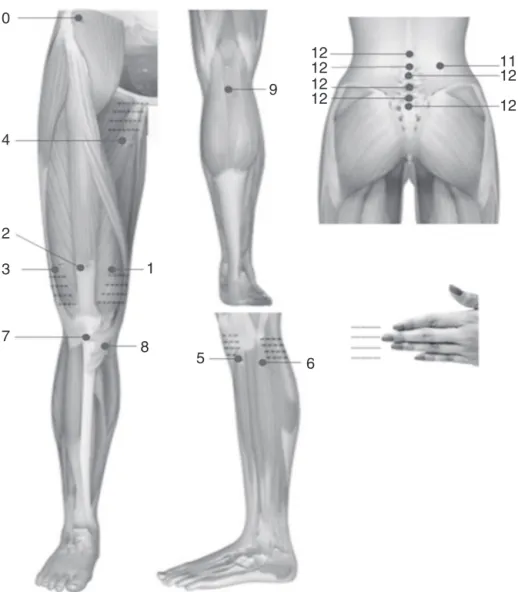
inchdiameterheadwereusedformechanicalquantificationofhyperalgesiaand allodyniaresultingfromperipheralorcentralnociceptive sen-sitization.Themeasurementswereperformedbilaterallyin thedermatomesatlevelsL1,L2,L3,L4,L5,S1andS2,using thepinch and rollmaneuverdescribed byImamura et al.5
Thesame wastaken formyotomes, atnine predetermined
locations (vastus medialis, vastus lateralis, rectus femoris, adductorlongus, tibialisanterior, peroneus longus,iliacus,
quadratus lumborum, and popliteus muscles). Finally, the
sclerotomeswereevaluatedintheL1–L2,L2–L3,L3–L4,L4–L5
supraspinous ligaments, over the L5–S1 and S1–S2 sacral
areas,pesanserinusbursae,andatthepatellartendon(Fig.1). Twoexperiencedresearcherscollectedallthedata,usingstrict criteriaforthelocationofthepoints.ThePPTwasexpressed inkg/cm2,withthehighestvaluesdenotinglesssevere
symp-toms.
Statisticalanalysis
Inmanysituationsitisnecessarytocheckwhetherthereisa significantdifferenceinmeantreatmentk(k>2).Onesolution wouldbetheFtestthroughtheanalysisofvariance(ANOVA), whichallowsustojointlytestthemeansofktreatments. How-ever, insomesituations themodel assumptions(normality andhomogeneityindependenceofresiduals)arenotsatisfied.
Therefore we recommendthe use ofnon-parametric tests,
i.e.,anon-parametricinference.Inthisworkweappliedthe
Kruskal–Wallis test consisting ofa non-parametric ANOVA
because the assumptions of parametric ANOVA were not
met.17
Results
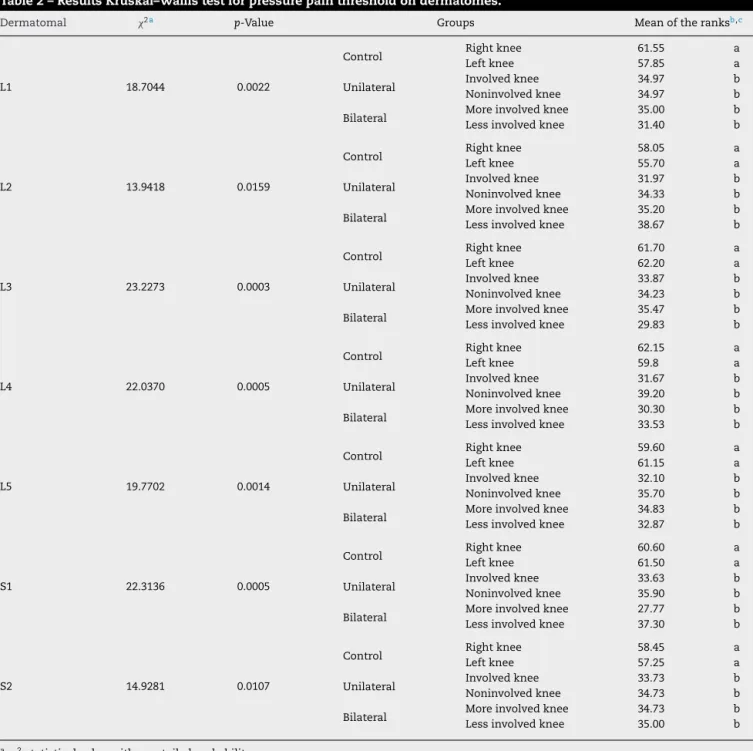
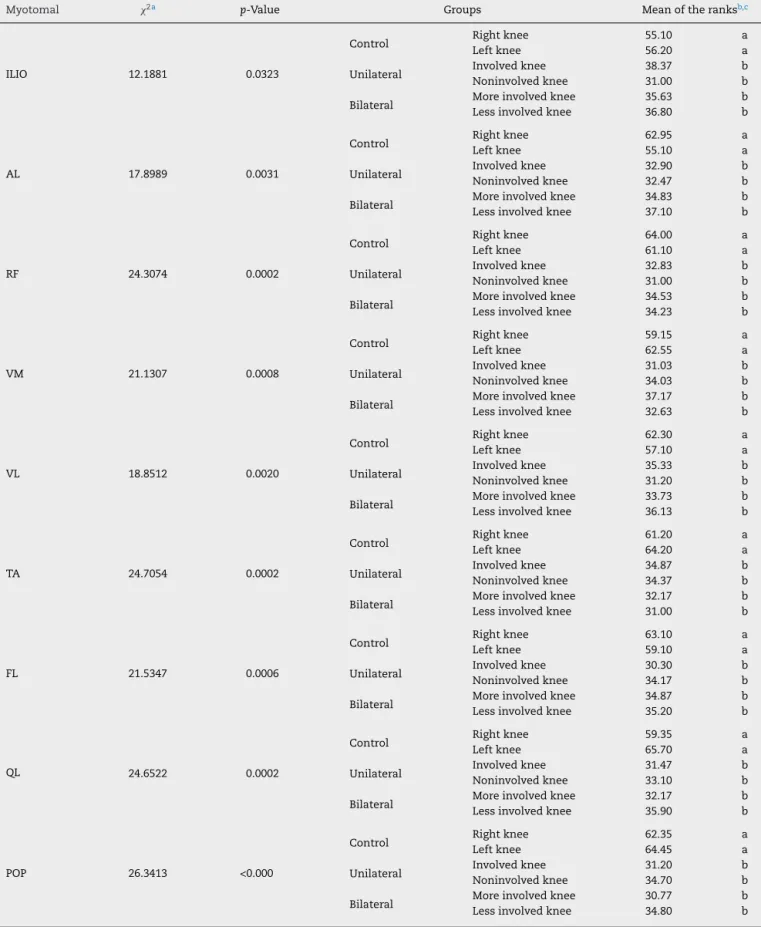
Significant difference in the mean values of the PPT was
foundbetweencontrolandKOAunilateralandbilateralgroups (p<0.03), whileno differencewas foundbetweenKOA
uni-lateral and bilateral groups. The KOA groups had a lower
pain thresholdinmostareas ofthe dermatomes (Table2), myotomes(Table3),andsclerotomes(onlythepesanserinus bursaeandpatellartendon;Table4).However,therewasno differenceinthemeanvaluesofthePPT(p>0.05)inthe scle-rotomes ofthesupraspinous ligaments,overthe L5-S1and S1-S2sacralareas(Table4).
Discussion
TheaimofthisstudywastomeasurethePPTofindividuals withmild and moderateKOA (withunilateraland bilateral
involvement) and compare with those without KOA. The
10
9
12
12
12
12
11
12
12
4
2
3
7
8
5
6
1
Fig.1–Theanatomicsitesusedintheevaluationofthepressurepainthreshold(PPT)ofthemuscles,patellartendon,and pesanserinusbusaeintheanterior,posterior,andlateralviews.(1)Vastusmedialismuscle;(2)rectusfemorismuscle;(3) vastuslateralismuscle;(4)adductorlongusmuscle;(5)anteriortibialismuscle;(6)peroneuslongusmuscle;(7)patellar tendon;(8)pesanserinusbursae;(9)poplitealmuscle;(10)iliacmuscle;(11)quadratuslumborummuscle;(12)supraspinous ligamentsandsacralareasbetweenL5-S1andS1-S2.FigureadaptedfromImamuraetal.5
no difference occurred between unilateralor bilateral KOA involvement.
AccordingCourtneyetal.,18primaryhyperalgesiaseemsto
bebasedonsensitizationofperipheralC-fibernociceptorsof deepsomatictissueswhenastimulusisappliedatthelocation oftheinflammation.Thisprocessprogressesifthe nocicep-tivestimulationpersists.Insuchcases,thenerveendingsof
the centralnervous system may bealtered because ofthe
increaseinthereceptivefield,makingthemmoresensitive tostimuli.5Theincreaseinsynapticexcitabilityincreasesthe
responsetobothnoxiousand non-noxiousstimuli,leading toallodyniaandsecondaryhyperalgesia.Insecondary hyper-algesia,astimulusoutofthelesionareacausespaininthe individual.18
AlthoughtheprocessofdegenerationinKOAisnotclear, theresults ofthis study revealed thatthe individuals with
mild to moderate KOA had primary and secondary
hyper-algesia,whereasthehealthycontrolsdidnot.Comparingthe data from this study with those of Imamura et al.,5 it is
suggestedthatwhenKOAprogresses,secondaryhyperalgesia alsoincreases.Imamuraetal.5alsoreportedthepresenceof
secondaryhyperalgesiaindistantregionsoftheknee, includ-ingthelumbarregion,insevereKOAindividuals.Incontrast, inthepresentstudy,theindividualswithmildtomoderate
KOA showedno alterationsinthe lumbarregion.However,
therewerechangesinthepainthresholdofdistantpartsofthe kneethatexhibitedsecondaryhyperalgesia(Tables2and3). Therefore, our results suggest the secondary hyperalgesia wouldoccuralongthedegenerationprocessandwouldnotbe afeaturepresentonlyintheseverelevelofKOA.Similarresults wereshowedbyRakeletal.,12however,thePPTpointswere
onlyinonepointeachprimaryandsecondaryhyperalgesia, andthewaytodeterminateofthemildKOAwasconsidereda limitationofthestudybyauthors.Thepresentstudyusedthe classificationoftheAmericanCollegeofRheumatology,15and
therefore,itconfirmstheresultsofRakeletal.,12addingthe
Table2–ResultsKruskal–Wallistestforpressurepainthresholdondermatomes.
Dermatomal 2a p-Value Groups Meanoftheranksb,c
L1 18.7044 0.0022
Control RightLeftkneeknee 61.5557.85 aa
Unilateral InvolvedNoninvolvedkneeknee 34.9734.97 bb
Bilateral MoreLessinvolvedinvolvedkneeknee 35.0031.40 bb
L2 13.9418 0.0159
Control RightLeftkneeknee 58.0555.70 aa
Unilateral InvolvedNoninvolvedkneeknee 31.9734.33 bb
Bilateral MoreLessinvolvedinvolvedkneeknee 35.2038.67 bb
L3 23.2273 0.0003
Control Rightknee 61.70 a
Leftknee 62.20 a
Unilateral InvolvedNoninvolvedkneeknee 33.8734.23 bb
Bilateral MoreLessinvolvedinvolvedkneeknee 35.4729.83 bb
L4 22.0370 0.0005
Control Rightknee 62.15 a
Leftknee 59.8 a
Unilateral Involvedknee 31.67 b
Noninvolvedknee 39.20 b
Bilateral MoreLessinvolvedinvolvedkneeknee 30.3033.53 bb
L5 19.7702 0.0014
Control Rightknee 59.60 a
Leftknee 61.15 a
Unilateral Involvedknee 32.10 b
Noninvolvedknee 35.70 b
Bilateral Moreinvolvedknee 34.83 b
Lessinvolvedknee 32.87 b
S1 22.3136 0.0005
Control Rightknee 60.60 a
Leftknee 61.50 a
Unilateral Involvedknee 33.63 b
Noninvolvedknee 35.90 b
Bilateral Moreinvolvedknee 27.77 b
Lessinvolvedknee 37.30 b
S2 14.9281 0.0107
Control RightLeftkneeknee 58.4557.25 aa
Unilateral Involvedknee 33.73 b
Noninvolvedknee 34.73 b
Bilateral Moreinvolvedknee 34.73 b
Lessinvolvedknee 35.00 b
a 2statisticalvaluewithone-tailedprobability˛.
b ThemeanranksderivethemeansofPPTcollectedandwasrepresentedbylowercaseletters.
c Differentlowercaselettersinthecolumn,themeansoftheranksofthePPTdifferbyKruskal–Wallistestat5%significancelevel.
Hassanet al.3 noted thatdrugs could acton peripheral
and/or central pain mechanisms. However, in the present
study,partoftheparticipants(n=15;Table1)wereusing,but thisseemstonotinterfereinPPT,sincemostofthePPTpoints
were more sensitive compared with control group. These
resultsreinforcetheevidencethatdrugsusuallyhavelimited actioninchronicpain,andunsatisfactoryinpainrelief.19
Tay-loretal.20 reportedthatbothphysiciansandpatients(51%
ofrespondents)areunhappywiththeinadequatecontrolof KOAprovidedbytraditionalanti-inflammatorynon-steroidal therapy.Their studyincluded patientswithmild(31%)and moderateorsevereKOA(60%).Inaddition,theseresults sug-gestthatforsecondaryhyperalgesiatreatmentandcontrolof
paininKOA,centralpaindrugscouldbeuseful,sinceNSAIDs actonlyonperipheralpainmechanisms.21
Riddle and Stratford14 found pain influence about the
sideofinvolvement(unilateralorbilateral)measuredby self-report,but ourresultsshowedthatpainnotinfluencedthe sideofinvolvementandnotsupportedtheresultsofthe Rid-dle andStratford.14 Despite ofimportantdifferenceofsize
samplebetweenthesestudies,weshouldconsideratethatan objectivemechanismofpainmensuration(PPT)couldbe dif-ferentoftheself-reportmeasure.RiddleandStratford14also
Table3–ResultsKruskal–Wallistestforpressurepainthresholdonmyotomes.
Myotomal 2a p-Value Groups Meanoftheranksb,c
ILIO 12.1881 0.0323
Control RightLeftkneeknee 55.1056.20 aa
Unilateral InvolvedNoninvolvedkneeknee 38.3731.00 bb
Bilateral MoreLessinvolvedinvolvedkneeknee 35.6336.80 bb
AL 17.8989 0.0031
Control Rightknee 62.95 a
Leftknee 55.10 a
Unilateral InvolvedNoninvolvedkneeknee 32.9032.47 bb
Bilateral MoreLessinvolvedinvolvedkneeknee 34.8337.10 bb
RF 24.3074 0.0002
Control Rightknee 64.00 a
Leftknee 61.10 a
Unilateral Involvedknee 32.83 b
Noninvolvedknee 31.00 b
Bilateral MoreLessinvolvedinvolvedkneeknee 34.5334.23 bb
VM 21.1307 0.0008
Control Rightknee 59.15 a
Leftknee 62.55 a
Unilateral Involvedknee 31.03 b
Noninvolvedknee 34.03 b
Bilateral Moreinvolvedknee 37.17 b
Lessinvolvedknee 32.63 b
VL 18.8512 0.0020
Control Rightknee 62.30 a
Leftknee 57.10 a
Unilateral Involvedknee 35.33 b
Noninvolvedknee 31.20 b
Bilateral Moreinvolvedknee 33.73 b
Lessinvolvedknee 36.13 b
TA 24.7054 0.0002
Control RightLeftkneeknee 61.2064.20 aa
Unilateral Involvedknee 34.87 b
Noninvolvedknee 34.37 b
Bilateral Moreinvolvedknee 32.17 b
Lessinvolvedknee 31.00 b
FL 21.5347 0.0006
Control RightLeftkneeknee 63.1059.10 aa
Unilateral InvolvedNoninvolvedkneeknee 30.3034.17 bb
Bilateral MoreLessinvolvedinvolvedkneeknee 34.8735.20 bb
QL 24.6522 0.0002
Control RightLeftkneeknee 59.3565.70 aa
Unilateral InvolvedNoninvolvedkneeknee 31.4733.10 bb
Bilateral MoreLessinvolvedinvolvedkneeknee 32.1735.90 bb
POP 26.3413 <0.000
Control RightLeftkneeknee 62.3564.45 aa
Unilateral InvolvedNoninvolvedkneeknee 31.2034.70 bb
Bilateral MoreLessinvolvedinvolvedkneeknee 30.7734.80 bb
ILIO,iliacusmuscle;AL,adductorlongusmuscle;RF,rectusfemorismuscle;VM,vastusmedialismuscle;VL,vastuslateralismuscle;TA,tibialis anteriormuscle;FL,peroneuslongusmuscle;QL,quadratuslumborummuscle;POP,popliteusmuscle.
a
2statisticalvaluewithone-tailedprobability˛.
b ThemeanranksderivethemeansofPPTcollectedandwasrepresentedbylowercaseletters.
Table4–ResultsKruskal–Wallistestforpressurepainthresholdonsclerotomes.
Sclerotomal 2a p-Value Groups Meanoftheranksb,c
TP 24.5637 0.0002
Control RightLeftkneeknee 63.6061.30 aa
Unilateral InvolvedNoninvolvedkneeknee 34.4333.53 bb
Bilateral MoreLessinvolvedinvolvedkneeknee 29.0035.77 bb
PG 19.6622 0.0014
Control RightLeftkneeknee 59.8059.95 aa
Unilateral InvolvedNoninvolvedkneeknee 33.6739.33 bb
Bilateral MoreLessinvolvedinvolvedkneeknee 31.7731.40 bb
L1-L2 3.9834 0.1364
Control Rightknee 48.00 a
Leftknee 43.20 a
Unilateral InvolvedNoninvolvedkneeknee 43.2739.83 aa
Bilateral MoreLessinvolvedinvolvedkneeknee 41.6330.47 aa
L2-L3 2.3155 0.3142
Control Rightknee 37.22 a
Leftknee –
Unilateral Involvedknee 37.58 a
Noninvolvedknee –
Bilateral MoreLessinvolvedinvolvedkneeknee 45.60– a
L3-L4 4.4425 0.1085
Control Rightknee 37.62 a
Leftknee –
Unilateral Involvedknee 47.48 a
Noninvolvedknee –
Bilateral Moreinvolvedknee 35.43 a
Lessinvolvedknee –
L4-L5 1.5373 0.4636
Control Rightknee 40.30 a
Leftknee –
Unilateral Involvedknee 36.85 a
Noninvolvedknee –
Bilateral Moreinvolvedknee 44.28 a
Lessinvolvedknee –
L5-S1 3.3315 0.1890
Control RightLeftkneeknee 47.45– a
Unilateral Involvedknee 41.10 a
Noninvolvedknee –
Bilateral Moreinvolvedknee 35.27 a
Lessinvolvedknee –
S1-S2 0.3497 0.8396
Control RightLeftkneeknee 39.30– a
Unilateral InvolvedNoninvolvedkneeknee 39.32– a
Bilateral MoreLessinvolvedinvolvedkneeknee 42.48– a
PT,patellatendon;PG,pesanserinusbursae;L1-L2,L1-L2supraspinousligament;L2-L3,L2-L3supraspinousligament;L3-L4,L3-L4supraspinous ligament;L4-L5,L4-L5supraspinousligament;L5-S1,L5-S1sacralarea;S1-S2,S1-S2sacralarea.
a 2statisticalvaluewithone-tailedprobability˛.
b ThemeanranksderivethemeansofPPTcollectedandwasrepresentedbylowercaseletters.
c Differentlowercaselettersinthecolumn,themeansoftheranksofthePPTdifferbyKruskal–Wallistestat5%significancelevel.
withpsychologicalstateaccordingtoWiseetal.,22whichcould
haveinfluencedtheresultsofRiddleandStratford.14
Finally,inthisstudytworesearchersmadethecollection ofthedataandwedidnotassesstheinter-raterreliability, whatcanbeconsideredalimitationofthestudy,sincethere
couldbeaslightdifferenceinthelocationsoftheanatomical points.However,theywerebothexperiencedandusedstrict criteriaforthelocationofthepoints.AsreportedbyFisher,6
Takingalltogether,individualswithmildtomoderateKOA hadprimaryandsecondaryhyperalgesia,independentof uni-lateralorbilateralinvolvement.Theseresultssuggestthatthe painhavetobeanassertivefocusintheclinicalpractice, inde-pendentofthelevelofseverityorinvolvementofKOA.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
Acknowledgments
Weappreciatethecontributionofallstudentsofthe Labora-toryofPhysicalTherapyandNeuromechanicaloftheFaculty ofPhysicalEducation,UniversidadeFederaldeUberlândia,for assistanceintechnicalanddiscussionsaboutit.
WethanktheFundac¸ãodeAmparoaPesquisadoEstado
deMinasGerais(FAPEMIG)fortheirsupportofresearch(Grant
APQ-01110-10) and the Conselho Nacional de
Desenvolvi-mentoCientíficoeTecnológico(CNPq)forscholarshiptothis research.
r
e
f
e
r
e
n
c
e
s
1. ShakoorN,FurmanovS,NelsonDE,LiY,BlockJA.Painandits relationshipwithmusclestrengthandproprioceptioninknee OA:resultsofan8-weekhomeexercisepilotstudy.J
MusculoskeletNeuronalInteract.2008;8:35–42.
2. Arendt-NielsenL,NieH,LaursenMB,LaursenBS,Madeleine P,SimonsenOH,etal.Sensitizationinpatientswithpainful kneeosteoarthritis.Pain.2010;149:573–81.
3. HassanBS,DohertySA,MockettS,DohertyM.Effectofpain reductiononposturalsway,proprioception,andquadriceps strengthinsubjectswithkneeosteoarthritis.AnnRheumDis. 2002;61:422–8.
4. HunterDJ,McDougallJJ,KeefeFJ.Thesymptomsof osteoarthritisandthegenesisofpain.MedClinNorthAm. 2009;93:83–100.
5. ImamuraM,ImamuraST,KaziyamaHHS,TarginoRA,Hsing WT,deSouzaLPM,etal.Impactofnervoussystem
hyperalgesiaonpain,disability,andqualityoflifeinpatients withkneeosteoarthritis:acontrolledanalysis.Arthritis Rheum.2008;59:1424–31.
6. FischerAA.Pressurealgometryovernormalmuscles. Standardvalues,validityandreproducibilityofpressure threshold.Pain.1987;30:115–26.
7. SuokasAK,WalshDA,McWilliamsDF,CondonL,MoretonB, WyldeV,etal.Quantitativesensorytestinginpainful
osteoarthritis:asystematicreviewandmeta-analysis. OsteoarthritisCartilage.2012;20:1075–85.
8.LeeYC,LuB,BathonJM,HaythornthwaiteJA,SmithMT,Page GG,etal.Painsensitivityandpainreactivityinosteoarthritis. ArthritisCareRes.2011;63:320–7.
9.Graven-NielsenT,WodehouseT,LangfordRM,
Arendt-NielsenL,KiddBL.Normalizationofwidespread hyperesthesiaandfacilitatedspatialsummationof deep-tissuepaininkneeosteoarthritispatientsafterknee replacement.ArthritisRheum.2012;64:2907–16.
10.StubhaugA,BreivikH.Kneeosteoarthritispatientswith intactpainmodulatingsystemsmayhavelowriskof persistentpainafterkneejointreplacement.ScandJPain. 2015;6:41–2.
11.Gerecz-SimonEM,TunksER,HealeJ-A,KeanWF,Buchanan WW.Measurementofpainthresholdinpatientswith rheumatoidarthritis,osteoarthritis,ankylosingspondylitis, andhealthycontrols.ClinRheumatol.1989;8:467–74. 12.RakelB,VanceC,ZimmermanMB,Petsas-BlodgettN,
AmendolaA,SlukaKA.Mechanicalhyperalgesiaandreduced qualityoflifeoccurinpeoplewithmildkneeosteoarthritis pain.ClinJPain.2015;31:315–22.
13.HeijinkA,GomollAH,MadryH,DrobnicM,FilardoG, Espregueira-MendesJ,etal.Biomechanicalconsiderationsin thepathogenesisofosteoarthritisoftheknee.KneeSurg SportsTraumatolArthrosc.2012;20:423–35.
14.RiddleDL,StratfordPW.Unilateralvsbilateralsymptomatic kneeosteoarthritis:associationsbetweenpainintensityand function.Rheumatology.2013;52:2229–37.
15.AltmanR,AschE,BlochD,BoleG,BorensteinD,BrandtK, etal.Developmentofcriteriafortheclassificationand reportingofosteoarthritis:classificationofosteoarthritisof theknee.ArthritisRheum.1986;29:1039–49.
16.KellgrenJH,LawrenceJS.Radiologicalassessmentof osteo-arthrosis.AnnRheumDis.1957;16:494–502.
17.ConoverWJ.Practicalnonparametricstatistics.3rded.New York:Wiley;1999.
18.CourtneyCA,KavchakAE,LowryCD,O’HearnMA. Interpretingjointpain:quantitativesensorytestingin musculoskeletalmanagement.JOrthopSportsPhysTher. 2010;40:818–25.
19.AmbroseKR,GolightlyYM.Physicalexerciseas
non-pharmacologicaltreatmentofchronicpain:whyand when.BestPractResClinRheumatol.2015;29:120–30. 20.TaylorSD,EverettSV,TaylorTN,WatsonDJ,Taylor-StokesG.A
measureoftreatmentresponse:patientandphysician satisfactionwithtraditionalNSAIDsforosteoarthritiscontrol. OpenAccessRheumatolResRev.2013:69–76.
21.BatlouniM.Anti-inflamatóriosnãoesteroides:efeitos cardiovasculares,cérebro-vasculareserenais.ArqBras Cardiol.2010;94:556–63.