www.jped.com.br
ORIGINAL
ARTICLE
Early
treatment
improves
urodynamic
prognosis
in
neurogenic
voiding
dysfunction:
20
years
of
experience
夽
,
夽夽
Lucia
M.
Costa
Monteiro
a,∗,
Glaura
O.
Cruz
a,
Juliana
M.
Fontes
a,
Eliane
T.R.C.
Vieira
b,
Eloá
N.
Santos
c,
Grace
F.
Araújo
a,
Eloane
G.
Ramos
daFundac¸ãoOswaldoCruz(Fiocruz),InstitutoNacionaldeSaúdedaMulher,daCrianc¸aedoAdolescenteFernandesFigueira(IFF),
AmbulatóriodeUrodinâmicaPediátrica,RiodeJaneiro,RJ,Brazil
bFundac¸ãoOswaldoCruz(Fiocruz),InstitutoNacionaldeSaúdedaMulher,daCrianc¸aedoAdolescenteFernandesFigueira(IFF),
Servic¸odeInformática,RiodeJaneiro,RJ,Brazil
cFundac¸ãoOswaldoCruz(Fiocruz),InstitutoNacionaldeSaúdedaMulher,daCrianc¸aedoAdolescenteFernandesFigueira(IFF),
DepartamentodeRadiologia,RiodeJaneiro,RJ,Brazil
dFundac¸ãoOswaldoCruz(Fiocruz),InstitutoNacionaldeSaúdedaMulher,daCrianc¸aedoAdolescenteFernandesFigueira(IFF),
DepartamentodePesquisaClínica,RiodeJaneiro,RJ,Brazil
Received22August2016;accepted4November2016 Availableonline19April2017
KEYWORDS
Urinaryincontinence; Neurogenicbladder; Urodynamics; Treatment; Kidneyfailure; Follow-up
Abstract
Objective: Toevaluatetheassociationbetweenearlytreatmentandurodynamicimprovement
inpediatricandadolescentpatientswithneurogenicbladder.
Methodology: Retrospective longitudinaland observational study (between 1990 and 2013)
includingpatientswithneurogenicbladderandmyelomeningoceletreatedbasedonurodynamic results.Theauthors evaluatedtheurodynamicfollow-up(bladdercomplianceandmaximum bladdercapacity andpressure) consideringthe first urodynamic improvement intwo years astheoutcome variableandearlyreferralastheexposurevariable,usingadescriptiveand multivariateanalysiswithlogisticregressionmodel.
Results: Among230patientsincluded,52%hadanearlyreferral.Themajoritywerediagnosed
asoveractivebladderwithhighbladderpressure(≥40cmH2O)andlowbladdercompliance
(3mL/cmH2O) and were treated with oxybutynin and intermittent catheterization.
Urody-namicfollow-upresultsshowed68%ofimprovementatthesecond urodynamicexamination decreasingbladderpressureandincreasingbladdercapacityandcompliance.Thepercentageof incontinenceandurinarytractinfectionsdecreasedovertreatment.Earlyreferral(one-yearold
夽
Pleasecitethisarticleas:MonteiroLM,CruzGO,FontesJM,VieiraET,SantosEN,AraújoGF,etal.Earlytreatmentimprovesurodynamic prognosisinneurogenicvoidingdysfunction:20yearsofexperience.JPediatr(RioJ).2017;93:420---7.
夽夽StudycarriedoutatFundac¸ãoOswaldoCruz(Fiocruz),InstitutoNacionaldeSaúdedaMulher,daCrianc¸aedoAdolescenteFernandes
Figueira(IFF),RiodeJaneiro,RJ,Brazil.
∗Correspondingauthor.
E-mails:lucia@fiocruz.br,lucia@iff.fiocruz.br,luciacostamonteiro@gmail.com(L.M.CostaMonteiro).
http://dx.doi.org/10.1016/j.jped.2016.11.010
or less)increasedby 3.5the probabilityofurodynamic improvementintwo years(95% CI: 1.81---6.77).
Conclusion: Treatment onsetwithin thefirst yearof lifeimproves urodynamic prognosis in
patientswithneurogenicbladderandtriplicatestheprobabilityofurodynamicimprovementin twoyears.Theroleofneonatologistsandpediatriciansinearlyreferralisextremelyimportant. ©2017SociedadeBrasileiradePediatria.PublishedbyElsevierEditoraLtda.Thisisanopen accessarticleundertheCCBY-NC-NDlicense(http://creativecommons.org/licenses/by-nc-nd/ 4.0/).
PALAVRAS-CHAVE
Incontinência urinária;
Bexiganeurogênica; Urodinâmica; Tratamento; Insuficiênciarenal; Seguimento
Tratamentoprecocemelhoraoprognósticourodinâmiconadisfunc¸ãomiccional deorigemneurogênica:20anosdeexperiência
Resumo
Objetivo: Avaliaraassociac¸ãoentretratamentoprecoceemelhoraurodinâmicaempacientes
pediátricoseadolescentesportadoresdebexiganeurogênica.
Metodologia: Estudoobservacionallongitudinalretrospectivo(entre1990-2013)empacientes
combexiganeurogênicaemielomeningoceletratadoscombasenodiagnósticourodinâmico. Avaliamosaevoluc¸ãourodinâmica(complacência,capacidadeepressãovesical)considerando primeiramelhoraurodinâmicaematédoisanoscomovariáveldesfechoeencaminhamento pre-coce(primeiraurodinâmicaatéumanodevida)comoexposic¸ão.Foirealizadaanálisedescritiva emultivariadacommodeloderegressãologística.
Resultados: Entre230pacientesincluídos52%foramencaminhadosprecocemente.Amaioria
tinhabexigahiperativacompressãomaiorque40cmH2O,complacênciaabaixode3ml/cmH2O
efoitratadacomoxibutininaecateterismointermitente.Naevoluc¸ãourodinâmica,68% apre-sentou melhorajá nosegundo exame comreduc¸ão dapressãoe aumentoda capacidadee dacomplacênciavesical.Opercentualdeincontinênciaeinfecc¸ãourináriadiminuiuaolongo dotratamento.Oencaminhamentoprecoceaumentou3,5vezesaprobabilidadedemelhora urodinâmicaatédoisanosemrelac¸ãoaosencaminhadosapósoprimeiroanodeidade(CI95% 1,81-6,77).
Conclusão: Tratarnoprimeiro ano devidamelhoraoprognósticourodinâmico depacientes
com bexiga neurogênica, triplicando a probabilidade de melhoraurodinâmica em até dois anos.A atuac¸ãodoneonatologistaedopediatra,reconhecendoeencaminhandoopaciente precocementeparaodiagnósticoéextremamenteimportante.
©2017SociedadeBrasileiradePediatria.PublicadoporElsevierEditoraLtda.Este ´eumartigo OpenAccesssobumalicenc¸aCCBY-NC-ND(http://creativecommons.org/licenses/by-nc-nd/4. 0/).
Introduction
Chronickidneydisease (CKD)isaworldwidepublichealth problem.1 Evidence has confirmed the increase in cases,
withmillionsofindividualsbeingtreatedbyrenal replace-ment therapy --- dialysis or kidney transplantation. Its prevalenceintheworld’spopulationexceeds10%andmay reach 50% in high-risk subpopulations,2 includingpatients
with neurogenic bladder,3 a neurological dysfunction of
the lower urinary system that changes the phases of fill-ing and emptying of the bladder. Neural tube congenital malformations,suchasmyelomeningocele,arethemost fre-quentcauses ofneurogenic bladderin childhood.Atleast 25%of themostsevere symptomsinpediatricurology are associatedwithneurogenicbladder.4Approximately40%of
children withneurogenicbladder develop somedegree of renalimpairment.5
The appropriate process of urination depends on the synergybetweenthebladderandtheurinarysphincter com-plex.This allowsthebladdertoremainrelaxedandunder low pressureduring thefilling phase,which characterizes
bladdercompliance.The emptyingphasebeginswhenthe bladdercapacityisreached,whichgeneratesacontraction ofthebladderwithelevationof theintravesicalpressure, ideally up to 40cmH2O, accompanied by sphincter relax-ation,allowingcompleteemptyingwithoutpost-voidurinary residue.
The main risk factors for renal impairment related to the diagnosis of neurogenic bladder are increased pres-sure, reduced bladder capacity and compliance, detrusor sphincter dyssynergia, and post-void residue. To reduce renal morbidity, it is necessary to identify and treat these risk factors as early as possible. The urodynamic evaluation is recognized as the gold standard diag-nostic method,6---9 because it is the only examination
The assessment of the evolution of patients with neu-rogenic bladder based on clinical criteria and diagnostic imaging,asseenin mostpublications,isofutmost impor-tance.However,thepresent studyfocused onprevention, with the follow-up based on the improvement of urody-namicindicators, which notoriouslyrepresent risk factors forrenalimpairment.Thisservicehasbeenrecommending early diagnosis and treatment for twodecades, consider-ingtheevaluationofpatientevolutionbasedonurodynamic improvementand,consequently,onthereductionofkidney failureassociatedwithneurogenicbladder.
This study aimed to evaluate the association between earlytreatment andurodynamic improvementof patients withneurogenicbladderinapediatrichospital.
Methods
Thiswasaretrospective, longitudinal,observationalstudy ofpediatricandadolescentpatientswithneurogenic
blad-der treated between 1990 and 2013 at the Pediatric
Urodynamic and Urinary Dysfunction Outpatient Clinic of InstitutoFernandesFigueira/FIOCRUZ.Afterapprovalbythe ResearchEthicsCommittee(CEP-IFF,Opinion281,768),the medicalrecordswereselectedthroughanactivesearchin theMedicalDocumentationandArchiveService.The inclu-sion criteria for the search were: referral to the service between1990and2013withadiagnosisof myelomeningo-celeandneurogenicbladder(ICDQ05andN31.9).Alleligible patientswereincluded.
Treatmentwasindicatedbasedontheinitialurodynamic diagnosis performed after myelomeningocele correction. Oxybutyninwasindicatedforthecontrolofoveractive blad-derand low bladdercompliance,when maximum bladder pressurewas≥40cmH2O.
Intermittent catheterization wasindicated when blad-der emptying was ineffective. Nocturnal catheterization was indicated for patients with recurrent urinary tract infections, renaland urinarytract evolution worseningat the ultrasound (US; onset or worsening of hydronephro-sis),presence ofgrade4and5 vesicoureteralreflux,very elevated urodynamic pressure levels, and renal function deterioration.10 The use of antibiotics was indicated for
treatment in urinary tract infections confirmed clinically andthrough laboratory exams,according to the suscepti-bilitytest,aswellasaprophylacticmeasure,accordingto theclinicalandlaboratoryhistoryofrecurrenturinarytract infections.
The evolutionanalysiswasbasedontheresultsof uro-dynamicexamsperformedsubsequently,at intervalsofsix months to one year, depending on the severity observed at thefirstexamination. Consequently, for thisstudy,the dateofthe firsturodynamicevaluationwasconsidered as ‘‘pointzero’’.Onthisoccasion,theinitialbladderbehavior was classified into one of four categories: normal blad-der (relaxed during filling, sustained bladder contraction upon reaching maximum capacity with relaxed sphincter, completeemptyingwithoutpost-voidresidue);underactive bladder (incapable of generating or sustaining contrac-tion that allowed bladder emptying); overactive bladder (detrusorcontractions during filling,elevated intravesical pressures, and early emptying before reaching maximum
bladder capacity) and low bladder compliance (loss of bladdercapacitytoremainrelaxedduringfilling, progres-sive increase in intravesical pressure, elevated bladder pressures,andearlyemptying).Overactivebladderandlow bladdercomplianceareat-riskurodynamicdiagnoses.
At the subsequent urodynamic assessments, when the bladder showed normalization during the evolu-tion in response to the treatment received, the term ‘‘compensated bladder’’ was used. The collected urody-namic variables were: maximum bladder pressure, loss pressure, bladder capacity in relation to the expected capacityforage,andbladdercompliance.
Regarding the clinical history, the following symptoms related to the urinary system were observed: presence, degree,andtimeofurinarycontinence,aswellasepisodes ofurinarytractinfectionandbacteriuria.
All urodynamic evaluations were reviewed by special-ists.Fromtheurodynamicevolutionstandpoint,urodynamic improvement was considered in relation to the previous examination when therewas reduction in pressure levels (maximumbladderpressureandlosspressure),increasein bladdercapacityandbladdercompliance,andreductionin the frequency of unconstrained detrusor contractions, in casesofoveractivebladder.Thestudyoutcomewasthefirst urodynamicimprovementinuptotwoyearsoftreatment; earlyreferral, definedasthereferralinuptooneyear of life,wasconsideredtheexposurevariable.
Treatmentadherencewasalsoassessedanddetermined based on information present in the medical records, considering attendance to scheduled appointments and examinations,continuoususeofprescribedmedication,and intermittent catheterization as indicated throughout the diseaseevolution.
Acollectionformandadatabasewerespecifically devel-oped for the study. The studied variables were selected based on the search for indicators in the literature and discussions on the subject in specialized congresses and multidisciplinary meetingswithexpertsfromtheresearch group, considering the outcomes to be tested. The fol-lowing initial data were recorded in the collectionform: gender, age at referral, decade of referral and adher-ence; and the following data were collected at each urodynamicevaluation: urodynamicdiagnosis, urodynamic indicators, indicated treatment, andsymptoms relatedto neurogenic bladder. The considered symptoms were diur-nal and nocturnal urinary incontinence and urinary tract infection.
Adescriptiveanalysisofallvariablesstudiedatthetime of the first evaluation was carried out, using frequency tablesandnumericalsummarystatistics.Bivariateanalyses werethenperformedamongthestudyvariablesatthetime ofthefirstevaluationandtheoutcomevariable,usingthe chi-squaredtest.Atthisstep,cruderelativeriskwas calcu-latedasameasureoftheassociation betweeneach study variableandtheoutcome.
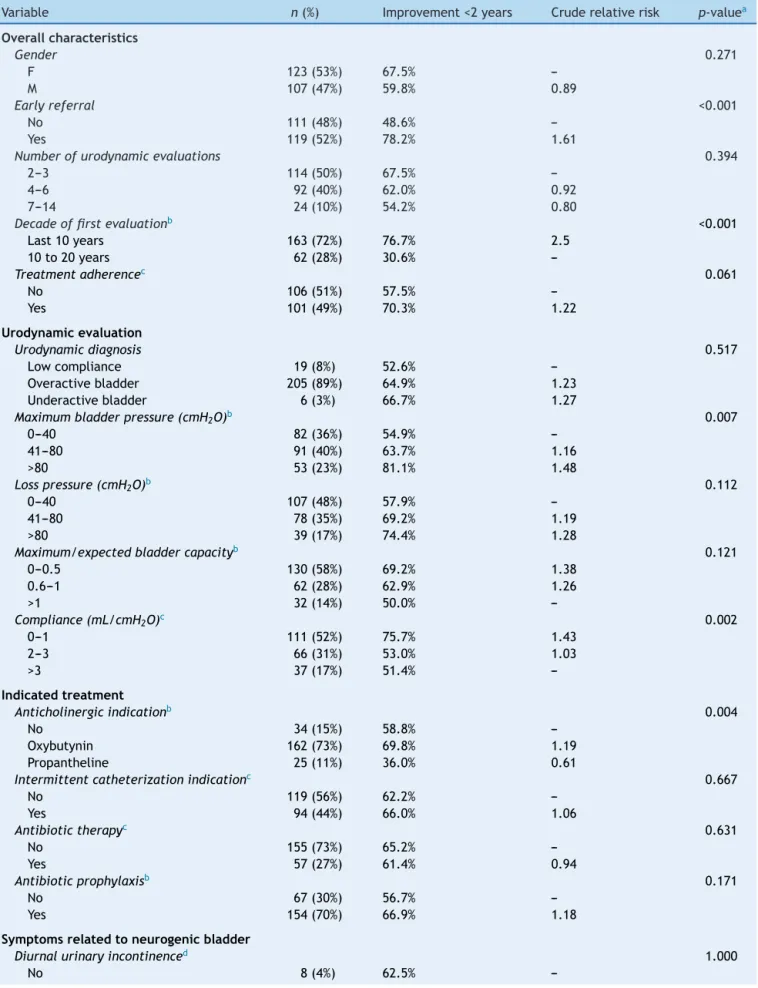
Table1 Characteristicsofthepopulationatthefirsturodynamicevaluationandassociationwithimprovementinuptotwo yearsoftreatment,1990and2013.
Variable n(%) Improvement<2years Cruderelativerisk p-valuea
Overallcharacteristics
Gender 0.271
F 123(53%) 67.5%
---M 107(47%) 59.8% 0.89
Earlyreferral <0.001
No 111(48%) 48.6%
---Yes 119(52%) 78.2% 1.61
Numberofurodynamicevaluations 0.394
2---3 114(50%) 67.5%
---4---6 92(40%) 62.0% 0.92
7---14 24(10%) 54.2% 0.80
Decadeoffirstevaluationb <0.001
Last10years 163(72%) 76.7% 2.5
10to20years 62(28%) 30.6%
---Treatmentadherencec 0.061
No 106(51%) 57.5%
---Yes 101(49%) 70.3% 1.22
Urodynamicevaluation
Urodynamicdiagnosis 0.517
Lowcompliance 19(8%) 52.6%
---Overactivebladder 205(89%) 64.9% 1.23
Underactivebladder 6(3%) 66.7% 1.27
Maximumbladderpressure(cmH2O)b 0.007
0---40 82(36%) 54.9%
---41---80 91(40%) 63.7% 1.16
>80 53(23%) 81.1% 1.48
Losspressure(cmH2O)b 0.112
0---40 107(48%) 57.9%
---41---80 78(35%) 69.2% 1.19
>80 39(17%) 74.4% 1.28
Maximum/expectedbladdercapacityb 0.121
0---0.5 130(58%) 69.2% 1.38
0.6---1 62(28%) 62.9% 1.26
>1 32(14%) 50.0%
---Compliance(mL/cmH2O)c 0.002
0---1 111(52%) 75.7% 1.43
2---3 66(31%) 53.0% 1.03
>3 37(17%) 51.4%
---Indicatedtreatment
Anticholinergicindicationb 0.004
No 34(15%) 58.8%
---Oxybutynin 162(73%) 69.8% 1.19
Propantheline 25(11%) 36.0% 0.61
Intermittentcatheterizationindicationc 0.667
No 119(56%) 62.2%
---Yes 94(44%) 66.0% 1.06
Antibiotictherapyc 0.631
No 155(73%) 65.2%
---Yes 57(27%) 61.4% 0.94
Antibioticprophylaxisb 0.171
No 67(30%) 56.7%
---Yes 154(70%) 66.9% 1.18
Symptomsrelatedtoneurogenicbladder
Diurnalurinaryincontinenced 1.000
---Table1 (Continued)
Variable n(%) Improvement<2years Cruderelativerisk p-valuea
Yes 193(96%) 66.3% 1.06
Nocturnalurinaryincontinenced 0.514
No 11(6%) 54.5%
---Yes 187(94%) 66.8% 1.23
Urinarytractinfectione 0.214
No 134(74%) 67.2%
---Yes 46(26%) 56.5% 0.84
aChi-squaredtest. b Missingdata:upto5%. c Missingdata:upto10%. d Missingdata:upto15%. e Missingdata:22%.
themodel.Thesignificanceofeachcoefficientestimatedin thefinalmodelwasdeterminedusingWaldtest.
Adescriptiveanalysisofurodynamicevolutionand symp-tomsrelatedtoneurogenicbladderovertimewasperformed throughproportionsandmediansforcategoricaland numer-icalvariables,respectively.
Results
A total of 322 patients met the inclusion criteria. Ten patientswerelostduetomissingdata:urodynamic evalu-ation(sevenpatients), initialdiagnosis (onepatient),and improvement throughout treatment (two patients). Addi-tionally,76patientswerelost,astheyunderwentonlyone urodynamicevaluation.Sixpatientswereexcludedbecause theyhadanormalbladderatthefirsturodynamic evalua-tion.The results shown belowrefer tothe remaining230 patients.
Thecharacteristicsofthesepatientsatthetimeofthe firsturodynamicevaluationaredescribedinTable1.There wasnosignificantdifferenceregardinggenderproportions. Thepatient’sageatthetimeofthefirsturodynamic eval-uation,consideredhereasthe‘‘pointzero’’oftheanalysis, rangedfrom14daysto19years,withameanof2.9years anda median of 0.85 years (10.2 months). Mostpatients (80%)hadtheirurinarysystem evaluatedforthefirsttime inearlychildhood;52%werereferredearlyandunderwent thefirsturodynamicevaluationwithinthefirstyearoflife (Table1).However,9%ofpatientswerereferredforthefirst timewhentheywereolder than9yearsofage.The num-berofurodynamicevaluationsperformedperpatientwithin theperiodrangedfromtwoto14.Mostpatients(77%)were includedinthestudylessthantenyearsago.
The most common urodynamic diagnosis found at the firstevaluationwasoveractivebladder(89%;Table1).Most patientshadbladderpressure>40cmH2O,being>80cmH2O in23%ofthem.Thelosspressurewas>40cmH2Oin approx-imately50%ofthepatients,andin17%,itwas>80cmH2O. More than 80% of the patients had bladder compliance <3mL/cmH2Oandbladdercapacitybelowtheexpectedfor age (Table 1). Most patients had been treated with anti-cholinergics(mainly oxybutynin) since the first diagnosis. Intermittentcatheterization wasindicated in a little less than50% of the totalcases. Antibiotictherapy tocontrol
urinary tractinfection was indicated in 27% of cases and maintenanceofaprophylacticantibiotictherapy,in70%.
Regardingthemainsymptomsrelatedtoneurogenic blad-der, 96% had diurnal urinary incontinence and 94% had nocturnalincontinence,associatedornotwithfecal incon-tinence.Urinaryinfectionwaspresentin26% ofthecases (Table1)andthisvariablewasshowedthelargest percent-ageofmissingdata(22%).
Approximatelyhalfoftheincluded patientsadheredto thetreatment,receivingregulartreatmentasindicatedand attendingallscheduledappointmentsandexams.
Thefirsturodynamicimprovementwasobservedinupto twoyearsoftreatmentin64%ofthepatients;28%presented thefirstimprovementaftertwoyearsand8%didnotshow improvementduringtheentirefollow-upperiod.
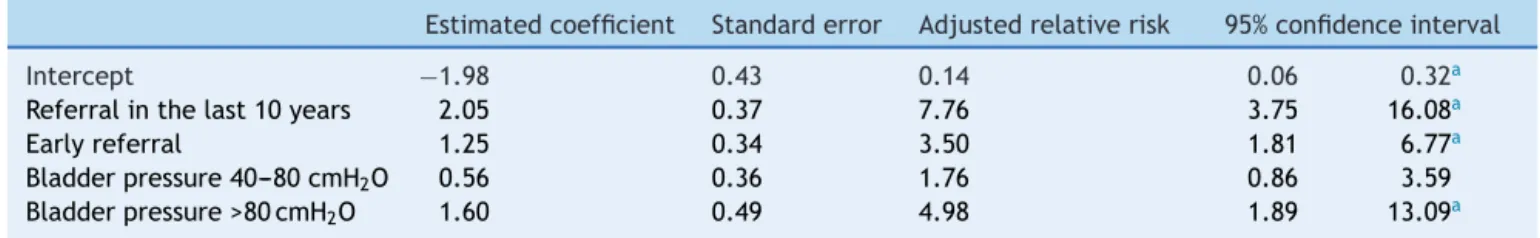
The following variables showed p-value <0.1 at the bivariate analysis and were selected for the modeling process: early referral, decade of the first evaluation, treatment adherence, bladder pressure, bladder compli-ance,andindicationofanticholinergicdrugs.Afteradjusting for thelogistic regression model, early referral remained significantly associated with the outcome urodynamic improvementinuptotwoyearsoftreatment(Table2).The probabilityofurodynamicimprovementinuptotwoyears amongthosewhowerereferredearlyforspecialized treat-mentwas3.5timeshigherthanforthosereferredafterthe firstyearoflife(95%CI:1.81---6.77).Patientsreferredinthe last ten yearsor with bladder pressure>80cmH2O at the firstevaluationalsohadagreaterprobabilityofurodynamic improvementintwoyears.
Urodynamicevolution
Overall, 910 evaluations were reviewed for the analysis of urodynamic evolution. However, since the number of patients with seven or more evaluations was very small, they were excluded from the statistical analysis; there-fore, 867 evaluations were available, related to the first sixevaluationsperformed.Themeantimeintervalbetween urodynamicevaluationswas1.6years,withamedianof1.3 years.Mostpatientsrepeatedtheexaminationafteraperiod ofsixto12months(21%)and12---18months(34%).
Table2 Logisticregressionmodelforurodynamicimprovementinuptotwoyearsoftreatment.
Estimatedcoefficient Standarderror Adjustedrelativerisk 95%confidenceinterval
Intercept −1.98 0.43 0.14 0.06 0.32a
Referralinthelast10years 2.05 0.37 7.76 3.75 16.08a
Earlyreferral 1.25 0.34 3.50 1.81 6.77a
Bladderpressure40---80cmH2O 0.56 0.36 1.76 0.86 3.59
Bladderpressure>80cmH2O 1.60 0.49 4.98 1.89 13.09a
a p-value<0.05(Waldtest).
Table3 Urodynamicevolutionduringfollow-up.
UDY n Improvement compared withthe previous examination
Compensated bladder
Bladder pressure ≤40cmH2O
Loss pressure ≤40cmH2O
Bladder capacity (median)
Bladder compliance: mL/cmH2O
(median)
Years between urodynamic assessments (median)
1 230 --- 0% 35.7% 46.5% 0.44 1.0
---2 230 68% 14% 40.9% 52.6% 0.68 2.2 1.1
3 167 60% 20% 47.9% 57.5% 0.67 3.0 1.3
4 117 52% 29% 54.7% 64.1% 0.59 4.2 1.4
5 75 64% 28% 52% 62.7% 0.59 3.9 1.4
6 48 56% 31% 52.1% 64.6% 0.55 5.2 1.4
UDY,urodynamicassessment.
Bladdercapacity:maximumbladdercapacitymeasuredduringexamination/bladdercapacityexpectedforage.
Table4 Evolutionofurinarysymptomsduringfollow-up.
UDY Diurnal urinary incontinence
Nocturnal urinary incontinence
Urinarytract infection
1 84% 81% 81%
2 82% 80% 80%
3 75% 73% 73%
4 66% 68% 68%
5 77% 72% 72%
6 75% 67% 67%
UDY,urodynamicassessment.
tothepreviousurodynamicevaluationwas68%atthe sec-ondevaluationandrangedfrom52%to64%at subsequent evaluations. Theproportionof patientswithcompensated bladderatthesecondevaluationwas14%,andthis propor-tionincreased throughout the treatment. The percentage of patients who had maximum bladder pressure and loss pressure <40cmH2O increased over time and stabilized
after the fourth urodynamic evaluation. The same was observed for bladder capacity in relation to the capac-ityexpectedforage,whilebladdercomplianceshowedan upwardtrendthroughouttheanalyzedperiod.Themedian timebetweenevaluationsincreaseduntilthefourth evalu-ationandremainedconstantthereafter.
Regarding urinary symptoms, there wasa reductionin thepercentageofpatientswithdiurnalandnocturnal uri-nary incontinence, as well as in the percentage of those withurinarytractinfectionthatwasdiagnosedandtreated (Table4).
Of the five patients with normal urodynamic pattern atthefirstevaluationwhomaintainedthefollow-up,four developedoveractivebladderatasubsequentexamination andonehasnotbeenreevaluatedyet.
Eleven patients progressed with some degree of renal impairmentand are being followed-up by a nephrologist; noneofthemhasdialysisindication.
Discussion
The importance of urodynamic diagnosis in pediatric
patients with neurogenic bladder has been demonstrated sincethe 1980s.11,12 In 2012, the International Children’s
ContinenceSociety published a consensus document con-firming the need to perform a urodynamic study in all children born withmyelomeningocele asa diagnostic pri-ority;theexamshouldbeperformedassoonastheclosure oftheneurologicallesionisstabilized.13Thepresentstudy
confirmedtheassociationbetweenearlyreferralfor special-izeddiagnosisandtreatmentandurodynamicimprovement. Patientstreateduptothefirstyearof lifewere3.5times morelikelytoimprovewithintwoyears.
Earlyurologicalinterventionisessentialtoreduce mor-bidity to the upper urinary system. Altered urodynamic findingsin pediatric patients withneurogenic bladder are predictiveofrenaldeteriorationinadults,14andthetimeof
delayedtreatment isdirectly proportionaltonephropathy severity.15
Theprotocolusedispreventiveandincludesearly urologi-calevaluationfromthefirstmonthoflife,beforetheonset of urinary symptoms (urinary incontinence or infection), withurodynamicevaluationinallcases;treatmentis initi-atedbasedontheurodynamicevaluationresults.According toVerpoorten,18 the therapeutic objective should not be
limited to treating secondary damages to the lower and upperurinarytract,butratheritshouldbetoensurenormal renaland bladderdevelopment, withsafepressure levels andurinarycontinence.
Theauthorshavetriedtodisseminatethispracticealso amongtheservicesthatreferpatientstothisservice. Nev-ertheless,despite allefforts,patientsarestillreferredat alatestage.Inthisstudy,48%ofthecasesunderwentthe firsturodynamicevaluationafterthefirstyearoflife,and approximatelyoneinevery12patientswasevaluatedonly aftertheageofnine.Mostpatientshadanoveractive blad-derandat-riskurodynamicevaluation,withbloodpressure levels>40cmH2Oandreducedbladdercapacityand compli-ance.
During the urination process, the bladder filling stage is the longest. The capacity of the bladder to act as a low-pressure reservoir is essential for the health of the urinarysystem,mainlyrenal.Theincreaseinbladder pres-suretolevels>40cmH2Oduringthefillingstageinterferes withtherenalfiltrationanddrainagesystemandis there-forea risk factor. The association between thereduction inglomerularfiltrationandelevated bladderpressurewas experimentally demonstrated in 1988.19 During the
emp-tying phase,the risk lies in the lack of synergy between bladdercontractionandsphincterrelaxation,withurinary retentionandincreaseinbladderpressuretoovercomethe obstacleandexpeltheurine.Theassociatedclinical reper-cussionsarerecurrenturinarytractinfection,vesicoureteral reflux,andhydronephrosis.The correspondingurodynamic diagnosesareoveractive bladder,low bladder compliance (themostcommonlyobserveddiagnosisinthisstudy),and detrusorsphincterdyssynergia,whichwasnotdiagnosedin thepresentpatientsduetoproblemsinthe electromyogra-phydevice.
Itwasshown thaturodynamicimprovementthroughout thetreatmentwasaccompaniedbyimprovementinurinary incontinenceandinfection.Urinaryincontinenceis primar-ilyrelatedtoloss ofstoragecapacitycausedby increased intravesicalpressureduringfillingandreductioninbladder complianceandcapacity,whichoccurinpatientswith over-active bladder and low compliance.Urinary incontinence wasthe symptom most commonly associated with neuro-genicbladder.Althoughnotariskfactor,itresultsinstigma andlowself-esteem,especiallyinadolescentswithchronic urinaryincontinence,withanimpactonqualityoflife.20
A lower percentage of cases of urinary tractinfection wasobservedinthepresentstudywhencomparedwiththe literature. The differential diagnosis between bacteriuria andurinaryinfectionisoftendifficult,especiallyinpatients whohaveintermittentcatheterization.Thepercentagesof antibiotictherapyindicationandcasesofurinaryinfection werecompatible,suggestingthisinformationwasfactualin thestudiedgroup.
Notwithstanding the recognized difficulties, retrospec-tive studies are advantageous to understand and assess the effectiveness of the used approach and to qualify
evidence-based care, provided they are methodologically well-designed.21Thevariablesofthepresentstudyshowing
thehighestpercentagesofmissingdatawerethoserelated tosymptoms.Theurodynamicvariables,whicharethoseof interest for the object,were recovered by reviewing the resultsoftheexaminations,notfromthedescriptionofthe medicalrecords.Theexposurevariablewasobtainedfrom thedateofbirth,whichisgenerallywelldocumented.The researcher responsiblefor thedesign andanalysisof data wasnotinvolvedinpatientcareordatacollection,reducing theriskofbias.
Studiesconductedinasinglecenterusuallyhavelower externalvalidity.However,thefactthatthisisareference centerformyelomeningoceletreatment,aswellasahuman resourcetrainingcenterfortheBrazilianUnifiedHealth Sys-tem(SistemaÚnicodeSaúde[SUS])promotestheinclusion ofpatientsandtheparticipationofprofessionalsfromother centers.
Asdemonstrated,earlytreatmentimprovesurodynamic prognosis in neurogenic voiding dysfunction. Treatment onsetinthefirstyearoflifeincreasesbythree-foldthe prob-abilityofurodynamicimprovementinuptotwoyears.The roleoftheneonatologistandthepediatricianinrecognizing andreferringpatientstodiagnosisisextremelyimportant, ensuringthestartofspecializedtreatmentwithinthefirst yearoflife.
Funding
PIP (IFF/FIOCRUZ Research Support Program) and FAPERJ (PP-SUS).
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
Acknowledgements
To Merlin P. Jimenez (database development) and scien-tific initiation fellows: Debora F.L. Diufrayer; Rafaela C. Carvalho;RenataA.Araújo;andThamiresC.Guimarães.
References
1.NogueiraPC,PazI,deP.Signsandsymptomsof developmen-talabnormalitiesofthegenitourinarytract.JPediatr(RioJ). 2016;92:S57---63.
2.Eckardt K-U, Coresh J, Devuyst O, Johnson RJ, Köttgen A, Levey AS, et al. Evolving importance of kidney disease: fromsubspecialtytoglobalhealthburden.LancetLondEngl. 2013;382:158---69.
3.PanickerJN,deSèzeM,FowlerCJ.Rehabilitationinpractice: neurogenic lower urinary tract dysfunction and its manage-ment.ClinRehabil.2010;24:579---89.
4.BauerS.Neuropathologyofthelowerurinarytract.In:Belman AB,KingLR,StephenAK,editors.Clinicalpediatricurology.4th ed.MartinDunitz;2002.p.371---408.
6.Costa Monteiro LM. Avaliac¸ão urodinâmica na infância. In: D’AnconaCAL,NettoNRJr,editors.Aplicac¸õesclínicasda urod-inâmica.3rded.SãoPaulo:Atheneu;2001.
7.DrzewieckiBA,BauerSB.Urodynamictestinginchildren: indi-cations, technique, interpretation and significance. J Urol. 2011;186:1190---7.
8.SpinoitA-F,DecalfV,Ragolle I,PloumidisA, ClaeysT,Groen L-A, et al. Urodynamic studies in children: standardized transurethral video-urodynamic evaluation. J Pediatr Urol. 2016;12:67---8.
9.BauerSB.Neurogenicbladder:etiologyandassessment.Pediatr NephrolBerlGer.2008;23:541---51.
10.KoffSA,GigaxMR,JayanthiVR.Nocturnalbladderemptying: asimpletechniqueforreversingurinarytractdeteriorationin childrenwithneurogenicbladder.JUrol.2005;174:1629---31. 11.McGuire EJ, Woodside JR, Borden TA. Upper urinary tract
deterioration in patients with myelodysplasia and detrusor hypertonia:afollowupstudy.JUrol.1983;129:823---6. 12.BauerSB, Hallett M, Khoshbin S, Lebowitz RL, Winston KR,
GibsonS,et al.Predictivevalueofurodynamicevaluationin newbornswithmyelodysplasia.JAMA.1984;252:650---2. 13.BauerSB,AustinPF,RawashdehYF,deJongTP,FrancoI,Siggard
C,etal.InternationalChildren’sContinenceSociety’s recom-mendationsfor initialdiagnostic evaluation andfollow-up in congenitalneuropathicbladderandboweldysfunctionin chil-dren.NeurourolUrodyn.2012;31:610---4.
14.Thorup J, Biering-Sorensen F, Corte D. Urological outcome aftermyelomeningocele:20yearsoffollow-up.BrJUrolInt. 2010;107:994---9.
15.Rodríguez-Ruiz M,Somoza I, Curros-Mata N.Study ofkidney damageinpaediatricpatientswithneurogenicbladderandits relationshipwiththepatternofbladderfunctionandtreatment received.ActasUrolEsp.2016;40:37---42.
16.Costa Monteiro LM [Dissertation] Valor da avaliac¸ão uro-dinamica em crianc¸as com mielomeningocele. Campinas, São Paulo, Brazil: Universidade Estadual de Campinas (UNI-CAMP); 1991. Available from: http://www.bibliotecadigital. unicamp.br/document/?code=000028194[cited09.08.16]. 17.Lins CON[Dissertation] Investigac¸ãourológica econduta em
crianc¸asportadorasdemielomeningocelenoprimeiroanode vida. Rio de Janeiro: Instituto Fernandes Figueira/FIOCRUZ; 1997. Available from: http://www.acervosbibliograficos. cict.fiocruz.br/F/?func=find-b&findcode=WRD&localbase= IFF&request=LINS%2C+Cristiana+Osorio+Navarro&Submit=OK& adjacent=Y[cited13.08.16].
18.Verpoorten C, Buyse GM. The neurogenic bladder: medical treatment.PediatrNephrolBerlGer.2008;23:717---25.
19.SteinhardtGF,GoodgoldHM,SamuelsLD.Theeffectof intrav-esical pressure onglomerular filtrationrate inpatients with myelomeningocele.JUrol.1988;140:1293---5.
20.Soares AH, Moreira MC, Costa Monteiro LM. A qualidade de vidadejovensportadoresdeespinhabífidabrasileirose norte-americanos.CienSaudeColet.2008;13:2215---23.