REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
Official Publication of the Brazilian Society of Anesthesiologywww.sba.com.br
SCIENTIFIC
ARTICLE
Comparison
of
tramadol
and
lornoxicam
in
intravenous
regional
anesthesia:
a
randomized
controlled
trial
Hande
C
¸elik
a,
Ruslan
Abdullayev
b,∗,
Erkan
Y.
Akc
¸aboy
c,
Mustafa
Baydar
c,
Nermin
Gö˘
güs
¸
daAnesthesiologyDepartment,KocaeliGölcükNecatiC¸elikHospital,Kocaeli,Turkey bAnesthesiologyDepartment,AdiyamanUniversityResearchHospital,Adiyaman,Turkey cAnesthesiologyDepartment,AnkaraNumuneResearchHospital,Ankara,Turkey dAnesthesiologyDepartment,HititUniversityResearchHospital,C¸orum,Turkey
Received15June2014;accepted7July2014 Availableonline29March2015
KEYWORDS
Intravenousregional
anesthesia; IVRA; Prilocaine; Tramadol; Lornoxicam
Abstract
Backgroundandobjectives: Tourniquet pain is one of the major obstacles for intravenous regionalanesthesia.Weaimedtocomparetramadolandlornoxicamusedinintravenousregional anesthesiaasregardstheireffectsonthequalityofanesthesia,tourniquetpainand postopera-tivepainaswell.
Methods:Aftertheethicscommitteeapproval51patientsofASAphysicalstatusI---IIaged18---65 yearswereenrolled.Thepatientswere dividedinto threegroups.Group P(n=17)received 3mg/kg 0.5%prilocaine; groupPT (n=17)3mg/kg 0.5%prilocaine+2mL (100mg) tramadol andgroupPL(n=17)3mg/kg0.5%prilocaine+2mL(8mg)lornoxicamforintravenousregional anesthesia.Sensoryandmotorblockonsetandrecoverytimeswerenoted,aswellastourniquet painsandpostoperativeanalgesicconsumptions.
Results:SensoryblockonsettimesinthegroupsPTandPLwereshorter,whereasthe corre-spondingrecoverytimeswerelongerthanthoseinthegroupP.Motorblockonsettimesinthe groupsPTandPLwereshorterthanthatinthegroupP,whereasrecoverytimeinthegroupPL waslongerthanthoseinthegroupsPandPT.Tourniquetpainonsettimewasshortestinthe groupPandlongestinthegroupPL.Therewasnodifferenceregardingtourniquetpainamong thegroups.GroupPLdisplayedthelowestanalgesicconsumptionpostoperatively.
Conclusion:Addingtramadolandlornoxicamtoprilocaineforintravenousregionalanesthesia producesfavorableeffectsonsensoryandmotorblockade.Postoperativeanalgesicconsumption can bedecreased by adding tramadol andlornoxicam toprilocaine inintravenous regional anesthesia.
©2014SociedadeBrasileiradeAnestesiologia.PublishedbyElsevier EditoraLtda.Allrights reserved.
∗Correspondingauthor.
E-mail:ruslanjnr@hotmail.com(R.Abdullayev).
http://dx.doi.org/10.1016/j.bjane.2014.07.013
PALAVRAS-CHAVE
Anestesiaregional
intravenosa; IVRA; Prilocaína; Tramadol; Lornoxicam
Comparac¸ãodetramadolelornoxicamemanestesiaregionalporviaintravenosa,
umestudorandomizadoecontrolado
Resumo
Justificativaeobjetivos: Adorrelacionada aotorniquete éumdosmaioresobstáculospara aanestesiaregional intravenosa(ARIV).Nossoobjetivofoi comparartramadol elornoxicam usadosemARIVemrelac¸ãoaosseusefeitossobreaqualidadedaanestesia,dorrelacionadaao torniqueteedornopós-operatório.
Métodos: Apósaaprovac¸ãodoComitêdeÉtica,51pacientescomestadofísicoASAI---IIeidades entre18---65anosforaminscritos.Ospacientesforamdivididosemtrêsgrupos.GrupoP(n=17) recebeu3mg/kg deprilocaínaa0,5%;Grupo PT(n=17)3mg/kg deprilocaínaa0,5%+2mL (100mg) detramadol eGrupo PL(n=17) de 3mg/kg de prilocaína a0,5%+2mL (8mg)de lornoxicamparaARIV.Oiníciodobloqueiosensorialemotoreostemposderecuperac¸ãoforam registrados, bemcomo adorrelacionada ao torniquete eoconsumo de analgésicono pós-operatório.
Resultados: OstemposdeiníciodobloqueiosensorialforammaiscurtosnosgruposPTePL, enquantoqueostemposderecuperac¸ãocorrespondentesforammaislongosqueosdoGrupo P. Ostemposdeiníciodobloqueio motornosgrupos PTe PLforammenores quenoGrupo P,enquantoqueotempoderecuperac¸ãodogrupoPLfoimaiorqueosdosgruposPePT.O tempoparainíciodadorrelacionadaaotorniquetefoimenornoGrupoPemaiornoGrupoPL. Nãohouvediferenc¸aemrelac¸ãoàdorrelacionadaaotorniqueteentreosgrupos.OGrupoPL apresentouomenorconsumodeanalgésicosnopós-operatório.
Conclusão:Aadic¸ãodetramadolelornoxicamàprilocaínaparaARIVproduzefeitosfavoráveis sobre o bloqueio sensorial e motor. O consumo de analgésicos no pós-operatório pode ser reduzidocomaadic¸ãodetramadolelornoxicamàprilocaínaemARIV.
©2014SociedadeBrasileira deAnestesiologia.PublicadoporElsevierEditoraLtda.Todosos direitosreservados.
Introduction
Intravenousregionalanesthesia(IVRA),commonlynameda
BierBlock,hasbeenintroducedin1908byKarlAugustBier.1
Easeof application of themethod,fast onsetof anesthe-sia, lower cost comparedwith general anesthesiaand no need fordeepsedationmakestheBier Blockamethodof choice for surgical procedures on extremities lasting less than an hour.2,3 IVRA can be used for emergency
opera-tions onextremities for thepatientswithfull stomach. It has a success rate of 96%---100% for upper extremity and is a good alternative for peripheral nerve block.4,5
Com-paredwithgeneralanesthesiaIVRAshortenshospitallength ofstay,necessitates30%lessnursecareand84%lessdrug need.6
Becauseofthehighpotentialofsystemictoxicity bupiva-caineandetidocainearenotpreferredforIVRA.Lidocaine andprilocainearethemostcommonlyusedlocal anesthet-icsforthis.Prilocainemetabolismisthefastestamongall localanesthetics.
One of the most important factors preventingthe use ofIVRAistourniquetpain.Manyadjuvantdrugshavebeen used to decrease the tourniquet pain, increase anesthe-sia qualityanddecrease postoperativepain.Among these aretramadol,ketorolac,lornoxicam,clonidine, dexametha-sone,paracetamol.7---9
Weaimedinourstudytocomparetheeffectsoftramadol and lornoxicam added toprilocaine for IVRA for patients undergoingupperextremitysurgery.
Methods
Fifty-onepatientsofASAphysicalstatusIandII,aged18---65 yearsold undergoing hand and wrist surgery (carpal tun-nelrelease,tendon repair, phalanx fracture repair, cystic hygroma, dupuytren contracture repair) were enrolled in the study after clinical trials ethical committee approval (T.C. Ankara Valili˘gi ˙Il Sa˘glık Müdürlü˘gü, 12.05.2009, n◦
051920).The study wasconducted inthe Ankara Numune ResearchHospital in 2009. Written informed consent was takenfromallthepatients.
Patients were premedicated by midazolam 0.15mg/kg and atropine 0.01mg/kg given intravenously from iv line opened onthe antecubital side of the non-operative arm 5mL/kg/h isotonicphysiologic saline solution wasstarted afterwards. In the operation room 24 gauge iv line was placedonthedorsalpartofthearmthatwillundergo oper-ation.Routine monitorization included non-invasive blood pressure(NIBP),electrocardiography(ECG) andperipheral oxygensaturation(SpO2).Extremitythatwillundergo
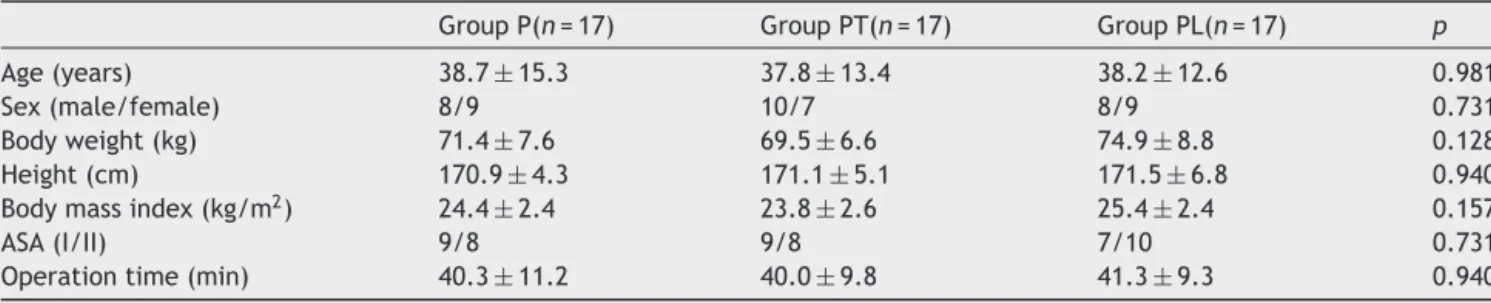
Table1 Demographiccharacteristics.
GroupP(n=17) GroupPT(n=17) GroupPL(n=17) p
Age(years) 38.7±15.3 37.8±13.4 38.2±12.6 0.981 Sex(male/female) 8/9 10/7 8/9 0.731 Bodyweight(kg) 71.4±7.6 69.5±6.6 74.9±8.8 0.128 Height(cm) 170.9±4.3 171.1±5.1 171.5±6.8 0.940 Bodymassindex(kg/m2) 24.4±2.4 23.8±2.6 25.4±2.4 0.157
ASA(I/II) 9/8 9/8 7/10 0.731 Operationtime(min) 40.3±11.2 40.0±9.8 41.3±9.3 0.940
Patients were randomized into three groups by the
closedenvelopesystem.GroupP(n=17)received3mg/kg
0.5% prilocaine (Citanest, Astrazeneca), group PT (n=17)
received3mg/kg 0.5% prilocaine+2mL(100mg) tramadol
(Contramal, Abdi ˙Ibrahim) and group PL (n=17) received
3mg/kg 0.5% prilocaine+2mL (8mg) lornoxicam (Xefo,
Nycomed)forIVRA.
Thedrugsolutionswereappliedbytheanesthesiologist
from the iv line on the extremity that will be operated
throughout 90s period.After the application of the
solu-tionsensoryblockadeonsettimewasevaluatedbypinprick
testingfromthemedian,radialandulnardermatomesevery
30s.Sensoryblockadeonsettimewasnotedasthetimefrom
thefinishingofthedrugsolutioninjectiontothetimethat
all dermatomesof the arm and forearm arenegative for
pinpricktesting. Motorblockade onsettimewasnoted as
thetimefromthefinishingofthedrugsolutioninjectionto
thetimethatnoneofthefingersonthehandcanmove.A
sensoryblock assessmentwasdone byVisualAnalog Scale
(VAS). Modified Bromage Scale was used for motor block
assessmentoftheextremity.Afterthesensoryblockonset
onalltheextremitiestheproximaltourniquetwasdeflated
aftertheinflationofthedistaltourniquetandoperationwas
started.
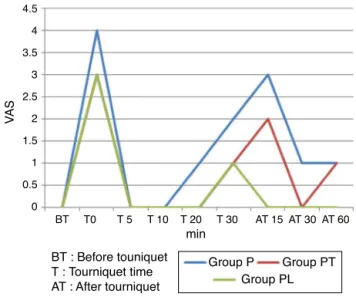
Tourniquetpainwasnotedasbeforetourniquetinflation
(BT),atthe5th,10th,20thand30thminutesoftourniquet
(T5,T10,T20,T30)andatthe15th,30thand60thminutes
afterthetourniquetdeflation(AT15,AT30,AT60).Fentanyl
wasusedasarescueanalgesicduringtheoperationandthe
dosewasnoted.Alltheside effectsduringtheanesthesia
andsurgicalprocedurewerenoted.
Tourniquettimewaskeptbetween30and90min range
regardlessofthedurationoftheoperation.Afterthe
defla-tionofthetourniquet,timetothepositivepinprickteston
median,radialandulnardermatomeswasnotedassensory
blockrecoverytimeandtimetothestartofthemovementof
thefingerswasnotedasmotorblockrecoverytime.Patients
werefollowed-upfor60mininthepost-anesthesiacareunit
andVASscoresfortourniquetpainwerenotedon15th,30th
and60thminutes.Diclofenaksodium(Voltaren,CibaGeigy)
75mgimwasusedasarescueanalgesicpostoperativelyand
24hanalgesicconsumptionwasnoted.Allthesideeffects,
ifany,werenoted.
Statistical evaluation was done using SPSS 11.5
soft-ware.Student’sttestswereusedforcomparisons ofdata
whicharecommonly expectedtobenormallydistributed,
e.g. demographics, time of the onset and recovery of
sensory and motor block, duration of the operation and
tourniquet, duration of analgesia, and intraoperative and
postoperative analgesic use. The Kruskal---Wallis test was
usedforintraoperativeandpostoperativeVAS.Significance
wasassumedat p≤0.05.Usingpooleddatafromprevious
IVRAlornoxicam/lidocaineandtramadol/lidocainestudies,
wecalculatedthatasamplesizeof15patientswouldpermit
aTypeIerrorof˛=0.05andapowerof80%.
Results
Therewasnostatisticallysignificantdifferencebetweenthe
groupsregardingdemographiccharacteristicsandoperation
times(p>0.05)(Table1).
Sensory block onset times in groups PT and PL were shorterthanthatingroupP.Thisdifferencewasstatistically significant(p<0.001).Althoughthesensoryblockonsettime ingroupPLwasshorterthanthatingroupPT,thisdifference wasnotstatisticallysignificant.
Sensoryblockrecovery timesingroupsPT andPLwere longerthanthatingroupP.Thisdifferencewasstatistically significant(p<0.001).Sensoryblockrecoverytimeingroup PLwaslongerthanthatingroupPTandthisdifferencewas statisticallysignificant(p<0.001)(Table2).
MotorblockonsettimesingroupsPTandPLwereshorter thanthatingroupP,thisdifferencewasstatistically signif-icant (p<0.001). Although the motor block onset time in groupPLwasshorterthanthatingroupPT,thisdifference wasnotstatisticallysignificant.
Motorblock recoverytimeingroupPL waslongerthan thatingroupsPandPTandthisdifferencewasstatistically significant(p<0.001)(Table3).
Table2 Sensoryblockonsetandrecoverytimes.
GroupP GroupPT GroupPL p
Sensoryblockonsettime(min) 8.0±0.68 6.0±1.17 5.5±0.77 <0.001a
Sensoryblockrecoverytime(min) 4.6±0.70 5.2±0.77 6.9±1.06 <0.001a
Table3 Motorblockonsetandrecoverytimes.
GroupP GroupPT GroupPL p
Motorblockonsettime(min) 11.9±1.11 9.1±0.67 8.8±0.98 <0.001a
Motorblockrecoverytime(min) 5.1±1.20 4.6±1.34 7.9±1.34 <0.001a
a p<0.05.
Table4 Tourniquetpainandfentanylconsumption.
GroupP GroupPT GroupPL p
Distaltourniquettime(min) 45.3±11.2 45.6±9.5 46.3±9.3 0.963 Patientswithtourniquetpain 10(58.8%) 4(23.5%) 9(52.9%) 0.086 Tourniquetpainonsettime(min) 32.5±4.9 33.7±7.5 39.2±7.3 0.081 Patientnumberneedingintraoperativefentanyl 9(52.9%) 3(17.6%) 8(47.1%) 0.078 Intraoperativefentanylconsumption(g) 66.7±25 50±0 50±0 0.129
BT T0 T 5 T 10 T 20 T 30 AT 15 AT 30 AT 60 4.5
4
3.5
3
2.5
2
1.5
1
0.5
0
min
Group P Group PT Group PL
VA
S
BT : Before touniquet T : Tourniquet time AT : After tourniquet
Figure1 TourniquetpainVASscores.
There was nostatistically significant differenceamong
the groups as regards the tourniquet times. The
tourni-quet painonset timewasshortestin group Pandlongest
ingroupPL,butthisdifferencewasnotstatistically
signif-icant(p>0.05).Rescue fentanylneedwaslowestin group
PT,butagainthisdifferencewasnotstatisticallysignificant
(p>0.05)(Table4).
Patients’tourniquetpainVASscoresaregiveninFig.1. Therewasnostatisticallysignificantdifferenceamongthe groups(p>0.05).
Table5 Postoperativeanalgesicconsumptionfor24h. Postoperativediclorone
consumption
Yes No p
GroupP 14(82.4%) 3 0.018a
GroupPT 11(64.7)% 6
GroupPL 6(35.3%) 11
a p<0.05.
Table 5 illustrates the 24h analgesic consumption of
the patients. There was statistically significant differ-enceamongthe groups regarding postoperative diclorone consumption(p<0.05).GroupPLdisplayedthelowest con-sumptionofdiclorone.
None of the patients experienced any side effects regardinglocalanesthetictoxicity.
Discussion
Themainoutcomeofourstudywasthatpostoperative anal-gesic consumption was markedly less in the group where lornoxicam was added to prilocaine. In the groups with tramadoland lornoxicam sensory block onset times were shorterandrecoverytimeswerelonger.Again,inthegroups withtramadolandlornoxicammotorblockonsettimeswere shorter,whereasinthegroupwithlornoxicammotorblock recoverytimewasmarkedlylonger.
Tanetal.10 haveobservedshorteronsetofsensoryand
motorblockandless tourniquetpainwithtramadol50mg added to lidocaine for IVRA, even if it was statistically insignificant.
Acalovschi et al.11 have reported significantly shorter
onsettimeofsensoryblockwithtramadoladdedforIVRA.In thegroupwithtramadoltheyhavedisplayedlonger recov-erytimesfortouchsensation.Theyattributedtheinability oftramadoltomakechangesonthemotorblockonitslow concentration.They speculatedthattramadolusedinlow concentrationsaffectssmallnervesandnerveendingsand higherconcentrationsshouldbeusedtoaffectnervetrunks. They used tramadol in 0.25% concentration. But Kapral etal.12havedisplayedthattramadolin0.25%concentration
addedtomepivacaineforbrachialplexusblockadeprolongs thedurationofsensoryandmotorblock.Tramadolmayhave different pharmacodynamics in IVRA and brachial plexus blockade.Inbrachialplexusblockadeanestheticagents pen-etratemixed nerves simultaneously, whereas in IVRA the firsteffectplaceisnerveendingsfollowedbynervetrunks.13
Langloisetal.14haveusedlidocaine3mg/kgwithtramadol
tramadoltoprilocaineprolongstourniquetpainonsettime andreducesfentanylneedduringtheoperation.
Senetal.15 usedlornoxicamforIVRAandfoundshorter
sensoryandmotorblockonsettimes.Theyhave displayed increased tourniquet tolerance, faster onset and better qualityofanesthesia,lessanalgesicconsumptionduringand aftertheoperationwithoutanysideeffectswithlornoxicam addedtolidocaineforIVRA.Ourfindingsarecompatiblewith these.We alsoobserved less fentanylconsumption in the groupwithtramadol, eventhough thedifferencewasnot statisticallysignificant.
Kol et al.’s9 study was the only study investigating
lornoxicam addedtoprilocainefor IVRA in theliterature. Thisstudyhasdemonstratedlongersensoryandmotorblock recoverytimes,longeranalgesia andtourniquettolerance timeswithlornoxicam addedforIVRA. 24h analgesic con-sumptionwasalso less inthe group withlornoxicam. Our findingswerecoherentwiththese.
As itisknown,localanestheticdrugs havespecific pKa
andpH of IVRA solutioncan be increasedtoapproximate physiologicalpH, thus showingmore permeabilitythrough the cell membrane resulting in faster onset of action of localanesthetics.15,16Senetal.15 measuredpHoflidocaine
6.7,lornoxicam8.7andlornoxicam---lidocainemixturetobe 7.6.Theyhavestatedthatthefaster onsetofsensoryand motorblockademayhavebeenattributedtothe alkaliniza-tionofthelocalanestheticsolutionbyaddinglornoxicam. Wehavenotmeasured thepH valuesof thedrugsusedin our study, but we know that pH of prilocaine is 6.9 and oflornoxicam is 8.7.We think,similartoSen etal.,that addition of lornoxicam may have increased the pH value ofprilocaineresultinginfasteronsetofsensoryandmotor block.
Sen et al.15 stated that prolonged motor block of the
extremitycanprevent thedistributionof localanesthetic intothe systemiccirculation, thus preventing local anes-thetic toxicity. We have observed prolonged motor block ingroupswithtramadolandlornoxicamcomparedwiththe controlgroup.Nofindingsofsystemictoxicityoflocal anes-thetics have been observed in our study and we are in agreementwithSenetal.’sopinion.
Reuben and Duprat17 have demonstrated that
non-steroidalanti-inflammatorydrugs(NSAID)decreaseafferent nociceptive signals and inflammatory mediators from the surgicalfield.TheeffectofNSAIDsisthoughttobethrough cyclooxygenase-2 (COX-2) enzyme inhibition, but other mechanisms may have been involved. NSAIDs may inhibit theconductanceofC-fiberswhichareinvolvedin propaga-tionoftourniquetpainimpulses.18Besidesthis,someNSAIDs
exhibittheirperipheral antinociceptiveactionsthroughK+
channels.18ActivationofNO-cGMPpathwaymayalsoinduce
antinociceptionthroughK+channels.18,19Positiveeffectsof
NSAIDslikelornoxicamorketorolaconanalgesiawhenused forIVRAarethoughttobethroughamechanismotherthan COX-2inhibition.15,20Ischemiaandoxidativestresshavealso
beenblamedintourniquetpain.21Lornoxicamwasfoundto
haveantioxidativeeffectsonrats,22thusitspositiveeffects
on tourniquet pain can be attributed to its antioxidative properties.Jankovicetal.20havestatedthatanalgesic
prop-ertiesofNSAIDsmaybeduetotheirantioxidantproperties. Kanbaketal.23havecomparedketorolacandtenoxicamfor
IVRAandfoundtenoxicamtobebetterasregardstourniquet
pain. They related this phenomenon tothe antioxidative propertiesoftenoxicam.
Inour study 14(82.4%) patients in group P,11 (64.7%) patients in groupPT and only 6(35.3%) patients in group PL needed rescue analgesics during the first 24h period postoperatively.Lornoxicamprovidedbetteranalgesia post-operatively compared with tramadol. Optimal dose of lornoxicamforIVRA isnotknown.Weusedroutineivdose in our study.Steinberg etal.24 have displayed that 20mg
ketorolac used for IVRA is aseffective as60mg. Possible mechanismsfor thisarehigh concentrationofthe drugin thesurgicalfield,24bindingofthedrugtothelocaltissueor
longstayinthesurgicalfield.25Studiesidentifyanoptimal
doseoflornoxicamforIVRAcanbeperformed.
Conclusions
In conclusion, adding tramadol and lornoxicam to prilo-caine for IVRA produces favorable effects onsensory and motor blockade. Postoperative analgesic consumption can bedecreasedby addingtramadolandlornoxicam to prilo-caineinIVRA.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.Erdine S. Rejyonel Anestezi 2. Istanbul: Baskı, Nobel Mat-baacılık;2008.p.104---7.
2.DaviesNJH,CashmanJN.Lee’s synopsisofanaesthesia.13th ed;1993.p.428---9.
3.KayhanZ.KlinikAnestezi3. ˙Istanbul:Baskı,LogosYayıncılık; 2004.p.527---8.
4.BrillS,MiddletonW,BrillG,etal.Bier’sblock;100yearsoldand stillgoingstrong.ActaAnaesthesiolScand.2004;48:117---22.
5.HaasioJ,HiippalaS,RosenbergP.Intravenousregional anaes-thesiaofthearm.Anaesthesia.1989;44:19---21.
6.ChanVW,PhilipWH,KaszasZ,etal.Acomparativestudyof generalanesthesia,intravenousregionalanesthesiaandaxillary blockfor outpatienthandsurgery:clinicaloutcomeand cost analysis.AnesthAnalg.2001;93:1181---4.
7.YurtluS,HancıV,KargıE,etal.Theanalgesiceffectof dexke-toprofen when added to lidocaine for intravenous regional anaesthesia: a prospective, randomized, placebo controlled study.JIntMedRes.2011;39:1923---31.
8.Hoffmann V,Vercauteren M,Van Steenberge A, et al. Intra-venousregionalanesthesia.Evaluationof4differentadditives toprilocaine.ActaAnaesthesiolBelg.1997;48:71---6.
9.KolIO,OzturkH,KaygusuzK, etal.Additionof dexmedeto-midine or lornoxicam to prilocaine in intravenous regional anaesthesiafor handor forearmsurgery: arandomized con-trolledstudy.ClinDrugInvest.2009;29:121---9.
10.Tan SM, Pay LL, Chan ST. Intravenous regional anaesthe-siausing lignocaineand tramadol.Ann AcadMedSingapore. 2001;30:516---9.
11.AcalovschiI,CristeaT,Margarit S, etal. Tramadol addedto lidocainefor intravenous regional anesthesia. Anesth Analg. 2001;92:209---14.
13.Rosenberg PH. Intravenous regional anesthesia: nerve block by multiple mechanisms. 1992 ASRA Lecture. Reg Anesth. 1993;18:1---5.
14.LangloisG,EstebeJP,GentiliME,etal.Theadditionoftramadol tolidocainedoesnotreducetourniquetandpostoperativepain duringivregionalanesthesia.CanJAnesth.2002;49:165---8.
15.Sen S, U˘gur B, Aydın ON, et al. The analgesic effect of lornoxicamwhenaddedtolidocainefor intravenousregional anesthesia.BrJAnesth.2006;97:408---13.
16.Armstrong P, Brockway M, Wıldsmıth JAW. Alkalinization of prilocainefor intravenous regional anaesthesia. Anaesthesia. 1990;45:935---7.
17.ReubenSS,DupratKM.Comparisonofwoundinfiltrationwith ketorolacversusintravenousregionalanesthesiawithketorolac forpostoperativeanalgesiafollowingambulatoryhandsurgery. RegAnesth.1996;21:565---8.
18.Deciga-Campos M, Lopez Munoz FJ. Participation of the l-arginine---nitric oxidecyclic GMP-ATP-sensitive K2+ channel cascade in the antinociceptive effect of rofecoxib. Eur J Pharmacol.2004;484:193---9.
19.Dallel R, Voisin D. Towards a pain treatment based on the identificationofthepain-generatingmechanisms?EurNeurol. 2001;45:126---32.
20.JankovicRJ,VisnjicMM,MilicDJ,etal.Doestheadditionof ketorolacanddexamethasonetolidocaineintravenousregional anesthesia improve postoperative analgesia and tourniquet tolerance for ambulatory hand surgery.Minerva Anesthesiol. 2008;74:521---7.
21.Chabel C, Russel LC, Lee R. Tourniquet induced limb ischemia: a neurophysiologic animal model. Anesthesiology. 1990;72:1038---44.
22.Rokyta R, HolecekV, Pekárkova I,et al. Free radicals after painful stimulation are influenced byantioxidants and anal-gesics.NeuroEndocrinolLett.2003;24:304---9.
23.KanbakO,SucuY,Gö˘güs¸N,etal.R˙IVA’daketorolakve tenok-sikamkullanımı.AnesteziDergisi.1996;4:38---41.
24.Steinberg RB, Reuben SS, Gardner G. The dose---response relationship of ketorolac as a component of intravenous regional anesthesia with lidocaine. Anesth Analg. 1998;86: 791---3.