www.jped.com.br
ORIGINAL
ARTICLE
Clinical
and
laboratory
description
of
a
series
of
cases
of
acute
viral
myositis
夽
,
夽夽
Silvana
Paula
Cardin,
Joelma
Gonc
¸alves
Martin,
Claudia
Saad-Magalhães
∗DepartmentofPediatrics,FaculdadedeMedicinadeBotucatu,UniversidadeEstadualPaulista(UNESP),Botucatu,SP,Brazil
Received5June2014;accepted12November2014 Availableonline26June2015
KEYWORDS
Influenza; Acutemyositis; Creatine phosphokinase
Abstract
Objective: Describetheclinicalandlaboratoryprofile,follow-up,andoutcomeofaseriesof casesofacuteviralmyositis.
Method: A retrospective analysis of suspected cases under observation in the emergency departmentwasperformed,includingoutpatientfollow-upwiththerecordingofrespiratory infectionandmusculoskeletalsymptoms,measurementofmuscleenzymes,creatine phosphoki-nase(CPK),lactatedehydrogenase(LDH),transaminases(ASTandALT),bloodcount,C-reactive protein, anderythrocyte sedimentation rate inthe acutephase andduring follow-up until normalization.
Results: Between2000and2009, 42suspectedcaseswereidentifiedand35 (27boys)were included.Themedianagewas7yearsandthediagnosiswasreportedin89%inthefirst emer-gencyvisit.Theobservedrespiratorysymptomswerecough(31%),rhinorrhea(23%),andfever (63%),withameandurationof4.3days.Musculoskeletalsymptomswerelocalizedpaininthe calves(80%),limitedambulation(57%),gaitabnormality (40%),andmuscleweaknessinthe lowerlimbs(71%), withameandurationof3.6days.There wassignificant increaseinCPK enzymes(5507±9180U/L),LDH(827±598U/L),andAST(199±245U/L),withatendencyto leukopenia(4590±1420)leukocytes/mm3.Thecomplete recoveryoflaboratoryparameters wasobservedin30days(median),andlaboratoryandclinicalrecurrencewasdocumentedin onecaseafter10months.
Conclusion: Typicalsymptomswithincreasedmuscleenzymesafterdiagnosisofinfluenzaand self-limited courseof thedisease were the cluesto the diagnosis. The increase inmuscle
夽 Pleasecitethisarticleas:CardinSP,MartinJG,Saad-MagalhãesC.Clinicalandlaboratorydescriptionofaseriesofcasesofacuteviral
myositis.JPediatr(RioJ).2015;91:442---47.
夽夽
StudyconductedattheDepartmentofPediatrics,FaculdadedeMedicinadeBotucatu,UniversidadeEstadualPaulista(UNESP),Botucatu,
SP,Brazil.
∗Correspondingauthor.
E-mail:claudi@fmb.unesp.br(C.Saad-Magalhães).
http://dx.doi.org/10.1016/j.jped.2014.11.008
enzymesindicatetransientmyotropicactivityrelatedtoseasonalinfluenza,whichshouldbe considered, regardlessoftheviral identification,possibly associatedwith influenzavirus or otherrespiratoryviruses.
©2015SociedadeBrasileiradePediatria.PublishedbyElsevierEditoraLtda.Allrightsreserved.
PALAVRAS-CHAVE
Influenza; Miositeaguda; Creatina-fosfoquinase
Descric¸ãoclínico-laboratorialdeumasériedecasosdeMiositeAgudaViral
Resumo
Objetivo: Descreveroperfilclínico-laboratorial,acompanhamentoedesfechodeumasériede casosdeMiositeAgudaViral.
Método: Foi conduzida uma análise retrospectiva de casos suspeitos, em observac¸ão em unidade deemergência,eseguimento ambulatorialcomoregistrode sintomasdeinfecc¸ão respiratória,sintomasmúsculo-esqueléticos,determinac¸ãodeenzimasmusculares, creatina-fosfoquinase (CPK), desidrogenase lática (DHL), transaminases (AST e ALT), hemograma, proteína Creativa evelocidadede hemossedimentac¸ão,nafase agudaeacompanhamento, atéanormalizac¸ão.
Resultados: Entre2000e2009,42casossuspeitosforamidentificadose35(27meninos)foram incluídos.Amedianadeidadefoi7anoseodiagnósticorelatadoem89%,naprimeiravisita deemergência.Ossintomasrespiratóriosobservadosforam:tosse(31%),coriza(23%),efebre (63%)comdurac¸ãomediade4,3dias.Ossintomasmúsculo-esqueléticosforam:dorlocalizada naspanturrilhas(80%),deambulac¸ãolimitada(57%),marchaanormal(40%),fraquezamuscular nosmembrosinferiores(71%),comdurac¸ãomédiade3,6dias.Observou-seelevac¸ãoimportante dasenzimasCPK(5507±9180)U/l,DHL(827±598)U/leAST(199±245)U/l,etendênciaa leucopenia(4590±1420)leucócitos/mm3.Arecuperac¸ãocompletedosparâmetros laboratori-aisfoiobservadaem30dias(mediana)earecaídaclínicaelaboratorialemumcasoapós10 meses.
Conclusão: OssintomastípicoscomenzimasmusculareselevadasapósdiagnósticodeInfluenza eocursoauto-limitadoforamosindíciosparaodiagnóstico.Aelevac¸ãodeenzimasmusculares indicamaatividademiotrópicatransitóriarelacionadaàinfluenzasazonalquedeveser con-siderada,àdespeitodaidentificac¸ãoviral,possivelmenteassociadacomovírusInfluenzaou outrosvírusrespiratórios.
©2015SociedadeBrasileiradePediatria.PublicadoporElsevierEditoraLtda.Todososdireitos reservados.
Introduction
Acuteviralmyositisisasyndromecharacterizedby muscu-loskeletal impairmentafter upperairwaydisorders,which leadstotemporarylimitedambulationinchildrenandis pre-dominantinboys.Itmanifestsasmusclepainandlower-limb weakness, especially in the calves and thighs.1---4 Its
inci-denceisunknown,butitisconsideredrareandisdescribed mainlyduringinfluenzaoutbreaks.5Thepreceding
respira-torysymptomsarecommon,includingfever,malaise,cough, odynophagia,headache,andrhinorrhea.
Musculoskeletalsignsandsymptoms---althoughtransient and often self-limited --- require emergency care, are of concerntoparents,andcausesomediagnosticdifficulties, especiallyregardinglimitedambulation.
There are literature reports of isolated cases, small series,or epidemicoutbreaks.2,6---12 Researchonits
patho-genesisisstilllimited.Theearlyrecognitionofthedisease mayimproveemergencycareandconservativetreatment. Theobjectivewastoexploreanddescribetheclinicaland laboratorypresentationandoutcomeofaseriesofcasesof acuteviralmyositis.
Methods
symptomsandcomplications, aswellasthe identification of respiratory symptoms, musculoskeletal symptoms, and recurrencewereidentifiedinoutpatientvisits.Possible dif-ferentialdiagnoses considered duringthe emergencycare wererecordedintheprotocol.
The laboratory tests were requested by the attending physician according to the clinical suspicion or diagnos-tic referral in the emergency room and consisted of the following:measurementofmuscleenzymes,creatine phos-phokinase(CPK)anditsisoenzyme,CK-MBfraction(CK-MB), lactatedehydrogenase(LDH),aspartatetransaminase(AST), andalanineaminotransferase(ALT),performedinthe rou-tinehospitallaboratory,usingacolorimetricenzymeassay withresultsexpressedinunitsperliter(U/L).Bloodcount andurinalysiswereperformedbyroutinemethods,aswell aserythrocyte sedimentation rate(Westergreen method), withresults expressed in mm/h,while C-reactive protein wasmeasured by an automated nephelometric assayand resultswereexpressedinmg/dL.
Astherearenostandardizedcriteriaforthediagnosisof acuteviralmyositis,the protocolwasestablished accord-ingtothesymptomsmostoftendescribedintheliterature, i.e.,painin thelimbs andmuscle weaknessaccompanied byelevatedmuscleenzymes.Casesthatmetthefollowing criteriawereincluded:age<18yearswithclinicalsuspicion confirmedduringoutpatientfollow-up,from2000to2009, withclinicalandlaboratoryassessmentatdiagnosisandat leastonefollow-upvisit.Suspectedcasesthatdidnothave elevatedmuscleenzymeswereexcluded,despitethe symp-tomsof myalgia --- limb painwithself-limitedevolution ---occurringafterrespiratoryinfection.
Variablefrequencywasrecorded,includinggender; pri-marydiagnosis,origin;consultedspecialties;complications; additional requested tests and altered laboratory tests; associated diseases; and the presence of clinical signs, mainlymyalgia,paininthecalves,limitedambulation,and gaitabnormality,suchaswalkingontiptoeandmuscle weak-ness.Theprecedingrespiratorysymptoms,suchassneezing, nasalobstruction,cough,rhinorrhea,fever,headache,sore throat, vomiting, diarrhea, epistaxis, pharyngotonsillitis, anduseofmedicationswerealsorecorded.Theprotocolwas approvedbytheethicscommitteeforinstitutionalresearch onDecember7,2009(No.3409/2009).
Statistical analysis was performed; quantitative data are shown as medians, minimum and maximum values, and means and standard deviations; categorical variables are shown as absolute values and percentages. The fre-quency and the annual distribution of cases are shown asfrequency histogram. The comparisonbetween labora-toryvariablesatclinicalpresentationandduringsymptom resolution(timevariable)wasperformedusing thepaired
t-test, withthesignificance thresholdset at5%(p<0.05). The tests were performed and the charts created using PrismGraphPadv.4.0®(GraphPadSoftwareInc.,California,
USA).
Results
A total of 42 cases with clinical suspicion of acute viral myositiswereidentifiedinemergencycareandoutpatient clinicrecords,fromJuneof2000toDecemberof2009.Of
0 1 2 3 4 5 6 7 8 9
0 1 2 3 4 5 6 7 8
2001 2000
Months
Jan Feb Mar Apr May Jun July Aug Sep Oct Nov Dec Annual incidence
Number of cases
Number of cases
2002 2003 2004 Year
Incidence per month of the year
2005 2006 2007 2008 2009
Figure 1 Frequency and monthly distribution of cases of acuteviralmyositisin2000---2009.
these,35caseswereincluded,27boysand8girls,withone caseofrecurrenceinasecondepisode.
The annual distribution of cases and the frequency accordingtothemonthsoftheyearisshowninFig.1,with a higherfrequency in the monthsof May, June, July,and September,whencomparedtotheothers,correspondingto thecoldermonthsoftheyear.Therewasahigherfrequency ofcasesdiagnosedfrom2004to2006.
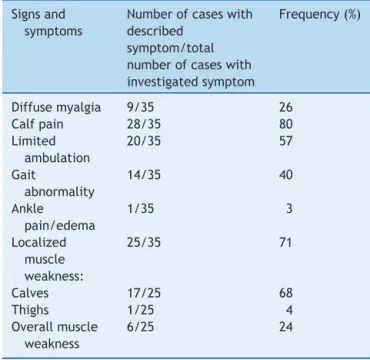
The age of symptom onset ranged from 3.4 to 12.5 years, with a median of 7.5 years. The interval between symptom onset and the first consultation ranged from 1 to 6 days. The duration of respiratory symptoms ranged from 1 to 15 days, with a median of 3.5 days and mean of 4.3±2.8 days. Among the reported symptoms, fever, cough,andrhinorrheawereobservedin63%,31%,and23%, respectively. Table 1 shows the musculoskeletal signs and symptomsdescribedaccordingtothedatacollection proto-col.Neurologicalexaminationwasnormalinallcases.The durationofmuscleweaknessrangedfrom1to8days,with a medianof 2days andmeanof 2.7±1.9days.Symptom resolution ranged from1 to 16 days, witha median of 3 andmeanof3.6±3.3days.One-to-threeconsultationswere performedduringtheacutephaseand48-hhospitalization occurredin4/35(11%).Follow-updurationvariedfrom30 to180days,withamedianof32days.
Table1 Descriptionofmusculoskeletalsymptomsat pre-sentationinaseriesofcasesofacuteviralmyositis.
Signsand symptoms
Numberofcaseswith described
symptom/total numberofcaseswith investigatedsymptom
Frequency(%)
Diffusemyalgia 9/35 26
Calfpain 28/35 80
Limited ambulation
20/35 57
Gait
abnormality
14/35 40
Ankle pain/edema
1/35 3
Localized muscle weakness:
25/35 71
Calves 17/25 68
Thighs 1/25 4
Overallmuscle weakness
6/25 24
pharyngotonsillitis.Antibioticuserangedfrom5to15days, withamedianof10daysandmeanof10.6±3.3days.
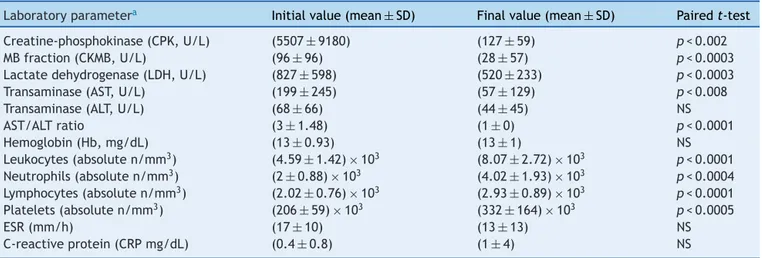
Laboratory test alterations are shown in Table 2. The resolutiontimeuntilnormalizationofmuscleenzymesand bloodcountparameters,aswellaserythrocyte sedimenta-tionrate(ESR)andC-reactiveprotein(CRP)levels,varied from30to180(medianof32)days.
Only three (9%) urinalysis tests were indicated, with abnormalresultsinoneofthetests,whichshowed protein-uriaof2+,butnoneindicatedmyoglobinuria.Serologytests were performed, including toxoplasmosis IgM+/negative mononucleosis/CytomegalovirusIgG+inasinglecase.Inthis case, the initial diagnosis was unspecified limb pain. No imagingorelectromyographytestswereindicated.
The normalization of laboratory parameters, muscle enzymes(CPK,CK-MB,LDH,ASTandALT)andthedecrease in AST/ALT ratio are shown in Table 2. A significant differencewas observed at the paired t-test, when com-paring initial and resolution values for CPK (p<0.002), CK-MB(p<0.0003),LDH(p<0.006)andAST(p<0.008),and AST/ALTratio(p<0.0001),butthedifferencewasnot sig-nificantforALT.
Thenormalizationofbloodcountparametersandacute phasereactants,showninTable2,alsoindicatedstatistical difference between the initial and resolution parameters for the absolute count of leukocytes (p<0.0001), neu-trophils(p<0.0004),lymphocytes(p<0.0001),andplatelets (p<0.005),buttherewasnosignificantdifferencebetween baseline and resolution parameters for hemoglobin, C-reactiveprotein,andESR.
The time intervalbetween measurementsat presenta-tionandresolutionwasvariable(67±78)days.Recurrence occurredin onecase,withtwodistinctepisodes,thefirst at 8.3 years and the second at 9.1 years. Only the first episodewasconsideredintheanalysis.Theinitialdiagnosis wasacuteviralmyositisinboth.Theclinicalcharacteristics
of thefirst and second episodes were myalgia, calf pain, limited ambulation, gait abnormality, and localized mus-cle weakness in the lower limbs. Symptom duration was 3days inthe first and5 daysin the second episode. The laboratory profile was similar when the first and second episodeswerecompared,withbothprecededbyrespiratory symptoms.
In this series, the time of musculoskeletal symptom resolutionrangedfrom1to16days.Therewereother man-ifestations,whichwererecordedin20%ofcases,including diagnoses of sinusitis, pneumonia, and transient hip syn-ovitis.Thedifferentialandexclusiondiagnosesrecordedin theemergencyroomduetolimitedambulationwere: non-specific synovitis, hip synovitis, Guillain---Barre syndrome, primaryneuromusculardisease,anddermatomyositis.
Discussion
Thisseriesshowedahighernumberofcasesofacuteviral myositisbetween2004and2006,withanannualdistribution in the cold months, withno other apparent explanation. There was a 3:1 predominance in the male gender and most cases were treated first in the emergency depart-ment,whichindicatesitsimpactonchildren’shealth.The recognition of respiratory manifestations associated with musculoskeletal symptoms led to the clinical suspicion, subsequently confirmed by the marked elevation in mus-cle enzymes,especially CPK, in addition to other muscle enzymessuchasLDHandAST;however,aldolase,another enzymewithmuscleinflammationspecificity,wasnot avail-able.
Inadditiontotheprecedingrespiratorysymptoms indi-catingacommonhematologicalresponsetoviralinfections, pronetotransient leukopenia,as well asnonspecific and subtle changes of acute phase reaction, the suspected diagnosis was confirmed by self-limited musculoskeletal symptoms, by serial measurement of muscle enzymes in casesofcalfpainandrefusal towalkorgaitimpairment, inassociationwithinfluenzasymptoms.
The influenza virus and other respiratory viruses can causeacuteandself-limitedfebrileillness,occurringin out-breaks, frequently in the winter. A variety of associated complicationsareknown,includingrespiratoryones,suchas primaryviralpneumoniawithorwithoutsecondarybacterial infections, laryngitis, bronchitis, and bronchiolitis. Non-respiratory complications, such as myositis, myocarditis, asepticmeningitis,andencephalitis,occurlessfrequently.12
The frequency of acuteviral myositis is proportionally higherintypeBinfluenza,withmaleindividualsmoreoften affectedthanfemales.5Myositismayalsobecausedby
bac-terial,fungal, and parasitic infections.13 Other infectious
Table2 Laboratoryparametersatpresentationandatfollow-upofacuteviralmyositis.
Laboratoryparametera Initialvalue(mean±SD) Finalvalue(mean±SD) Pairedt-test Creatine-phosphokinase(CPK,U/L) (5507±9180) (127±59) p<0.002
MBfraction(CKMB,U/L) (96±96) (28±57) p<0.0003
Lactatedehydrogenase(LDH,U/L) (827±598) (520±233) p<0.0003
Transaminase(AST,U/L) (199±245) (57±129) p<0.008
Transaminase(ALT,U/L) (68±66) (44±45) NS
AST/ALTratio (3±1.48) (1±0) p<0.0001
Hemoglobin(Hb,mg/dL) (13±0.93) (13±1) NS
Leukocytes(absoluten/mm3) (4.59±1.42)×103 (8.07±2.72)×103 p<0.0001 Neutrophils(absoluten/mm3) (2±0.88)×103 (4.02±1.93)×103 p<0.0004 Lymphocytes(absoluten/mm3) (2.02
±0.76)×103 (2.93
±0.89)×103 p<0.0001 Platelets(absoluten/mm3) (206±59)×103 (332±164)×103 p<0.0005
ESR(mm/h) (17±10) (13±13) NS
C-reactiveprotein(CRPmg/dL) (0.4±0.8) (1±4) NS
NS,non-significant.
aReferencevalues:CPK:0---80U/L,CKMB:0---6U/L,LDH:313---618U/L,AST:17---37U/L,ALT:30---65U/L,ESR<20mm/h,CRP<1mg/dL.
Amongtheparasiticinfections,cysticercosis, schistoso-miasis,andtrichinosiscancausesymptomssuchasmyalgia and fever, accompanied by eosinophilia. The diagnosis of muscularinvolvementinthesecasesismostcommonly per-formed by identification of calcified cystson radiographs andthepseudo-hypertrophyofthethighandcalfmusclesin thedisseminatedforms.Theoptimaldiagnosisofacuteviral myositiscanbeattainedbyviralidentification,byserology, orbybiopsy,inthepresenceofnonspecificmusculoskeletal symptoms.
Other investigations,such aselectromyography, havea limitingfactor,i.e.,theinvasivenessofthetechniqueand the cost-benefit ratio, in practice.In spite of the identi-fication failure by serology,6,7 studies have identified the
influenzavirusinmuscletissueofpatientsaffectedbyacute viralmyositis.However,itsetiopathogenicmechanismsare stillunknown. Thereis ahypothesis of muscledamageby immunemechanismor muscletissueinvasionbyviral par-ticles,causingdamagetomusclefibers.Thereisevidence ofviralparticlesisolatedfromcalfmusclesbiopsieswithno specificdegenerativealterationsandmyonecrosis.13Among
thecomplications,rhabdomyolysis,althoughrare,canresult inkidneydamagesecondarytomyoglobinuria.14
Acuteviralmyositisassociatedwithpandemicinfluenza H1N1hasbeenreportedinchildrenandadults,15,16withone
of thecases showing orbital muscle involvement, charac-terizingarareformoforbital myositis15 inan infant.The
recentpandemic,aswellasallhistoricalcyclesofepidemic andseasonalinfluenza,haveindicatedthebenefitsofmass vaccination.
Thepresent studywasconductedduringaperiodwhen vaccinationforseasonalinfluenzahad limitedcoveragein thepublic health care system and documentationof spe-cificvaccination in thisserieswas notdiscriminated. The association betweenthe immunestatus for influenza vac-cination and the risk of acute viral myositis is unknown. Althoughpatientsthatreceivedtheseasonalinfluenza vac-cine could admittedly have a lower risk of respiratory complications (e.g., pneumonia, otitis media), there is no clear demonstration of decrease in other secondary complications.
Amongthelimitationsofthisstudy,thefollowingshould beconsidered:thesmallsizeoftheseries,treatmentata specific hospital,and the retrospective study design. Ide-ally,prospectivepopulationstudieswouldprovidethebest description of acuteviralmyositisincidence.5 The
associ-ationwiththeidentificationofrespiratoryviruses wasnot possible.17,18 Despitetheselimitations,theresultsindicate
somerecommendations,suchasthesystematicevaluation ofchildrenwithlower-limbmyalgiainthepresenceof respi-ratory symptoms and follow-up with serial measurement ofmuscleenzymes,especiallyCPK,consistentwithrecent observations.19
Most children with acute viral myositis are treated in the emergency department,20,21 as the symptoms can
be alarming for parents, with a tendency toward mul-tiple consultations with various specialties and costly investigations.4,11,22Thepediatricianintheemergencycare
service shouldfeel comfortable todischarge the patient, making the differential diagnosis withneuromuscular dis-eases,checking during the follow-upto review symptoms andthe measurementofmuscle enzymesuntil normaliza-tion.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
Acknowledgment
CAPES ---Post-graduate Programin Collective Health, Fac-uldade de Medicina de Botucatu, Universidade Estadual Paulista(UNESP).
References
2.KingBA.Benignacutechildhoodmyositisasacauseoffailure toweightbear.JPaediatrChildHealth.2003;39:378---80.
3.AgyemanP, Duppenthaler A, Heininger U,Aebi C. Influenza-associated myositis in children. Infection. 2004;32: 199---203.
4.MujganSonmezF,CakirM,YaylaS,BozC.Benignacute child-hoodmyositis.MedPrincPract.2004;13:227---9.
5.MallS, Buchholz U, Tibussek D,Jurke A, An derHeiden M, DiedrichS, et al.A largeoutbreakofinfluenza B-associated benignacutechildhoodmyositisinGermany,2007/2008.Pediatr InfectDisJ.2011;30:e142---6.
6.CeladeJulianME,MartinPuertoMJ,OteroJR.Acutebenign viralmyositis:neitheretiologicconfirmationnor complemen-taryproofs.AnEspPediatr.1998;49:437---8.
7.Munoz-GarciaM,Valverde-Molina J,Diez-LorenzoP, Camara-Simon M. Acute viral myositis. Is etiologic confirmation necessary?AnEspPediatr.1998;48:333---4.
8.MackayMT,KornbergAJ, ShieldLK, DennettX.Benignacute childhoodmyositis:laboratoryandclinicalfeatures.Neurology. 1999;53:2127---31.
9.MoulinF,MimieuxC,MarcE,GendrelD.Post-influenzaacute myositis.ArchPediatr.2000;7:483s---5s.
10.RajajeeS, EzhilarasiS, RajarajanK. Benignacute childhood myositis.IndJPediatr.2005;72:399---400.
11.Rennie LM, Hallam NF, Beattie TF. Benign acute childhood myositisinanaccidentandemergencysetting.EmergMedJ. 2005;22:686---8.
12.HiteLK,GlezenWP,DemmlerGJ,MunozFM.Medicallyattended pediatricinfluenzaduringtheresurgenceoftheVictorialineage ofinfluenzaBvirus.IntJInfectDis.2007;11:40---7.
13.Crum-CianfloneNF.Bacterial,fungal,parasitic,andviral myosi-tis.ClinMicrobiolRev.2008;21:473---94.
14.WuCT,HuangJL,LinJJ,HsiaSH.Factorsassociatedwith non-traumaticrhabdomyolysisandacuterenalfailureofchildrenin Taiwanpopulation.PediatrEmergCare.2009;25:657---60.
15.GuedjR,DesguerreI,BrassierA,BoddaertN,HubertP,Oualha M.UnusualmuscularinjuryinaninfantwithsevereH1N1 infec-tion.PaediatrNurs.2012;47:51---4.
16.GibsonSB,MajersikJJ,SmithAG,BrombergMB.Threecasesof acutemyositisinadultsfollowinginfluenza-likeillnessduring theH1N1pandemic.JNeuroscRurPract.2013;4:51---4.
17.ThomazelliLM,VieiraS,LealAL,SousaTS,OliveiraDB,Golono MA,etal.Surveillanceofeightrespiratoryvirusesinclinical samplesofpediatricpatientsinsoutheastBrazil.JPediatr(Rio J).2007;83:422---8.
18.BenitesEC,CabriniDP,SilvaAC,SilvaJC,CatalanDT,Berezin EM,et al.Acuterespiratoryviralinfectionsinpediatric can-cer patients undergoing chemotherapy. J Pediatr (Rio J). 2014;90:370---6.
19.Neocleous C,Spanou C,MpampalisE,XatzigeorgiouS, Pavli-douC,PoulosE,etal.Unnecessarydiagnosticinvestigationsin benignacutechildhoodmyositis:acaseseriesreport.ScottMed J.2012;57:182.
20.TippettE,ClarkR.Benignacutechildhoodmyositisfollowing humanparainfluenzavirustype-1 infection.EmergMedAust. 2013;25:248---51.
21.HallG,SchranzCI.Benignacutechildhoodmyositis:ararecause ofabnormalgait.AmJEmergMed.2014;32:193.e1---2.