BrazJOtorhinolaryngol.2017;83(4):490---493
www.bjorl.org
Brazilian
Journal
of
OTORHINOLARYNGOLOGY
CASE
REPORT
Maxillary
sinus
hemangioma:
usefulness
of
embolization
according
to
classification
夽
Hemangioma
de
seio
maxilar:
utilidade
da
embolizac
¸ão
de
acordo
com
a
classificac
¸ão
Hisashi
Hasegawa
a,
Hiroumi
Matsuzaki
a,∗,
Tohru
Furusaka
a,
Takeshi
Oshima
a,
Shinobu
Masuda
b,
Toshiyuki
Unno
c,
Osamu
Abe
caNihonUniversitySchoolofMedicine,DepartmentofOtorhinolaryngology,HeadandNeckSurgery,Tokyo,Japan bNihonUniversitySchoolofMedicine,DepartmentofPathology,Tokyo,Japan
cNihonUniversitySchoolofMedicine,DepartmentofRadiology,Tokyo,Japan
Received19June2015;accepted12September2015 Availableonline17December2015
Introduction
Hemangiomainthenoseandnasalsinusesisrare,1
particu-larlyinthemaxillarysinus.2Differentiationofhemangioma
frommalignanttumorsisimportant,becausebothmaybe
accompanied by bone destruction. With regard to giant
hemangioma,thistype hasarich bloodsupply,and
surgi-caltreatmentrequiresparticular careduetothehighrisk
ofmassivebleedingandobstructedfieldofview.Although
maxillarysinushemangiomahasbeensporadicallyreported,
few reports have described cases of this type diagnosed
accordingtothe1996classificationoftheInternational
Soci-etyfortheStudyofVascularAnomalies(ISSVA)andtreated
witharterialembolization.
Here,we reportthree casesof massive sinonasal
hea-mangiomathatwereresectedafterarterialembolization.
夽
Pleasecitethisarticleas:HasegawaH,MatsuzakiH,Furusaka T,OshimaT,MasudaS,UnnoT,etal.Maxillarysinushemangioma: usefulnessofembolizationaccordingtoclassification.BrazJ Otorhi-nolaryngol.2017;83:490---3.
∗Correspondingauthor.
E-mail:matuzaki.hiroumi@nihon-u.ac.jp(H.Matsuzaki). PeerReviewundertheresponsibilityofAssociac¸aoBrasileirade OtorrinolaringologiaeCirurgiaCervico-Facial.
Case
report
AnoverviewofthethreecasesisshowninTable1.
Case1
A 43-year-old man presented with recurrent right nasal
bleeding and nasal obstruction for six months. Mucosal
swellingwasobservedfromthemaxillarysinustothenasal
septumintherightinferiorandmiddlenasalmeatuses.Sinus
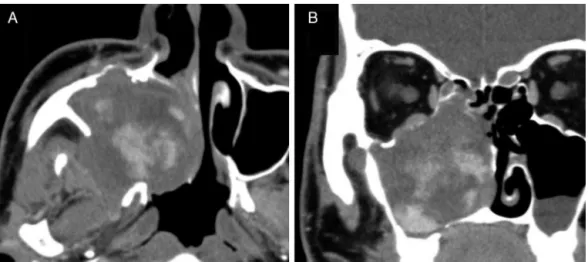
computed tomography (CT) revealed a soft tissuedensity
shadow, with a contrast-enhanced interior in a scattered
and graduallyincreasing pattern (Fig. 1). Nocalcification
was observed. Gadolinium contrast magnetic resonance
imaging (MRI) showed that the inside of the mass was
markedlycontrast-enhanced, suggesting a vasculartumor.
Sphenopalatine arteriographyshowed tumor staining with
a collection of thin, meandering arteries extending from
theposteriorsuperioralveolararteryanddescending
pala-tineartery.Thetumor,whichwascontrast-enhancedduring
the arterial phase,was a slow-flow vascular lesion, from
which the contrast medium was partially washed out in
thelatephase,andwasdiagnosedasvenousmalformation
http://dx.doi.org/10.1016/j.bjorl.2015.09.002
Maxillarysinushemangioma:usefulnessofembolizationaccordingtoclassification 491
Table1 Anoverviewofthethreecases.
Case 1 2 3
Agegender 41y.o.male 43y.o.female 74y.o.male
Preoperatedbiopsy Hematoma Necroticpolypoid Nasalmucosa
Origin Lateralwall Upperwall Unknown
Artery Posteriorsuperioralveolar
descendingpalatine
Infraorbitaldorsalnasal Sphenopalatinedeeptemporal
Embolicdevice Microcoilandgelatinsponge Microcoilandgelatinsponge Microcoilandgelatinsponge
Technique ESSandWatsuji---Denker
operation
ESSandWatsuji---Denkeroperation ESSandWatsuji---Denker operation
ISSVAclassification Lowflowvenousmalformation Lowflowvenousmalformation Lowflowvenousmalformation
Bleeding(g) 60 30 100
Diagnosis Sinusoidalhemangioma Cavernoushemangioma Cavernoushemangioma
according to the ISSVA classification. Both arteries were embolized. Threedays later,the patientunderwent com-bined surgery with an endoscopic procedure and the Watsuji---Denker operation. Intraoperative blood loss was
30mL. Sinusoidal hemangioma, a variant of cavernous hemangioma, was diagnosed by histopathology (Fig. 2A).
In24months offollow-up conductedeverythreemonths,
however,wehaveyettorecognizerecurrence.
Figure1 EnhancedCTinCase1.Axial(A)andcoronal(B)images.Astrong,spreading,andgraduallyincreasingcontrasteffect isseenduringthearterialphase.
492 HasegawaHetal.
Figure3 Gadolinium-enhancedMRIofCase2.Axial(A)andcoronal(B)images.Aheterogeneouslyenhancedvasculartumorwas suspected.
Case2
A 41-year-old woman presented with recurrent leftnasal
bleedingandnasalobstructionfor amonth.Her left
com-monnasalmeatuswasfilledwithedematousmucosa.Sinus
CT revealed a soft tissue density shadow occupying the
leftmaxillarysinus,ethmoidsinus,frontalsinus,andnasal
cavity, with a bone defect on the medial wall of the
left maxillary sinus. In addition, CT showed a soft
tis-sue density shadow including blood retention that filled
theleftmaxillary sinus. The medialwall of the maxillary
sinus showed destruction and was increasingly
contrast-enhanced. A 30mm heterogeneously enhanced vascular
tumor wassuspected, based ongadolinium-enhanced MRI
(Fig.3). Facialarteriographyshowed tumor staining from
theinfraorbitalarteryontheupperwalloftheleftmaxillary
sinus,andthearterywasembolized. Inaddition,the
dor-salnasalarterywasembolized.Thetumorwasaslow-flow
vascular lesion, and venous malformation was diagnosed
according to the ISSVA classification. Four dayslater, the
patient underwent combined surgery with an endoscopic
procedureandtheWatsuji---Denkeroperation,andtheentire
lesionwasextracted.Intraoperativeblood losswas30mL.
The postoperative pathological diagnosis was cavernous
hemangioma. In 18 months of follow-up conducted every
three months, however, we have yet to recognize
recur-rence.
Case3
A 74-year-old man presented with right nasal bleeding
andnasal obstruction. Two yearsbefore, the patienthad
experienced right nasal bleeding lasting a few hours.
Myelodysplastic syndrome was diagnosed. An edematous
polyp occupying the right common nasal meatus was
observed. Sinus CT showed a soft tissue density shadow
occupying the right maxillary sinus, ethmoid sinus, and
frontal sinus to the left nasal cavity, with bone
destruc-tiononthemedialwalloftherightmaxillarysinus.Contrast
CTshowedalobulatedtumorouslesionthatwasgradually
contrast-enhancedfromthemaxillarysinustothecommon
nasalmeatus,aswellasmicrovasculardevelopmentinthe
tumor.Gadolinium-enhancedMRIshowedaheterogeneously
enhancedlesion,raisingsuspicionofavasculartumor.Tissue
biopsyshowedonlynasalmucosa.Externalcarotid
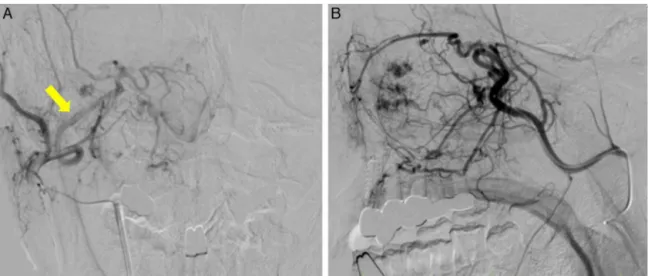
arteriog-raphyshowedtumor staininginthe areacorrespondingto
theentirerightmaxillarysinus.Sphenopalatine
arteriogra-physhowedthattheinfraorbitalartery,descendingpalatine
artery,andanumberofsmallmedial/lateralposteriornasal
brancheswereinvolved asfeeders.The maintrunk ofthe
sphenopalatinearteryand branchesof thedeeptemporal
arterywereembolized(Fig.4).Thetumorwasaslow-flow
vascular lesion diagnosedas venousmalformation
accord-ingtotheISSVAclassification.Fourdayslater,thepatient
underwentcombinedsurgerywithanendoscopicprocedure
andtheWatsuji---Denkeroperation,andtheentirelesionwas
extracted.Intraoperativebloodlosswas100mL.The
post-operativepathologicaldiagnosiswascavernoushemangioma
(Fig.2B).In18monthsoffollow-upconductedeverythree
months,however,wehaveyettorecognizerecurrence.
Discussion
Inareportof281casesofhemangioma,55percentoccurred
onthefaceandextracranialhead,and5percentoccurred
on the neck,3 with these lesions only rarely occurring in
thenoseor nasalsinuses.1Ofthosewhichdooccurinthe
noseandnasalsinuses,about80percentoccuronthenasal
septum,inKiesselbach’sareainparticular,and15percent
onthelateralwallofthenasalcavity.Hemangioma
occur-ringinthesinuscavityisevenrarer.Cavernoushemangioma
occursfarlessfrequentlythancapillaryhemangioma,
usu-allydeveloping on turbinate bone andrarely onthe bony
tissueofthemaxillarysinuswall.4
Sinusoidalhemangioma,5,6 diagnosedon histopathology
inCase1,isamarkedlyrarehistologicaltype(Fig.4)which
is relatively unknown amongpathologists. Because only a
few cases of sinusoidal hemangioma have been reported
since the initial description by Calonje and Fletcher in
1991,aclearrecognitionoftheclinicopathological
charac-teristics of thistype willavoid diagnosticpitfalls. Patient
follow-up has revealed no tendency toward either local
recurrenceor metastasis5;however,Ciureaetal.reported
Maxillarysinushemangioma:usefulnessofembolizationaccordingtoclassification 493
Figure4 ExternalcarotidarteriographyofCase3.Frontal(A)andprofile(B)views,showingtumorstaininginthearea corre-spondingtotheentirerightmaxillarysinus.Sphenopalatineartery(arrow).
preoperative CT showed bone destruction. Given the
rar-ityofsinusoidalhemangiomaandthepossibilitythatother
vascular neoplastic lesions might also be present, a high
risk of local recurrenceand metastasis lesions with
simi-lar CTand MRI findings,such ashemangiopericytoma and
hemangiosarcomainthesecases,cannotbedenied.
Hemangioma is commonly diagnosed radiographically,
according to the classification adopted at the 1996 ISSVA
meeting. In the ISSVA classification, conventionally
diag-nosed hemangiomasare divided into vascular tumors and
vascular malformations.8 Vascular malformations,
conven-tionallyclassifiedascavernoushemangiomas,donotregress
spontaneouslyandsometimesrequiretreatmentwhenthey
graduallyincreaseinsize.Theymaybefurthersubdivided
into slow- and fast-flow lesions; fast-flow lesions can be
treatedwithsemipermanentandreliableembolization,such
asviamicrocoils.Knowingtheflow speedhelpsto
deter-minetheembolizationmethodandisausefulreferencefor
intravasculartreatment.
We considered that our surgical method waseffective
on the basis of two criteria: the low rate of
periopera-tivehemorrhageandthereportedsuccessfulpostoperative
management.Wewereable tolimit intraoperative
bleed-ingto60mL,30mL,and100mLforCases1---3,respectively.
Further,postoperativebleedingwassufficientlycontrolled
bytheplacementofgauzetampons.Inapreviousreport,a
patientwhodidnotundergoarterialembolizationrequired
two emergency room visits for the treatment of
postop-erative bleeding.9 Another study reported that massive
sinonasalhemangioma wasabletobe resected
endoscop-ically, albeit with effort, including preoperative arterial
embolizationandanincreaseinsurgicalaccesstothetumor
viatheconstructionofacontrolholeatthecaninefossa.10
For ourthree patients, in contrast, we chose the
combi-nationofanendoscopicprocedureandtheWatsuji---Denker
operation with preoperative arterial embolization, which
facilitatedourinvestigationandcareof thepostoperative
lesion.
Conclusion
Thesethreecaseswerediagnosedasslow-flowvenous
mal-formations, in accordance with the ISSVA classification.
Angiographyandarterialembolizationbothaidedaccurate
diagnosisof the primarysiteand thecontrol of bleeding.
These very rare cases are amenable to relatively
rou-tinetreatmentfollowingcarefulassessmentandaplanned
approach.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.Fu YS,Perzin KH. Non-epithelialtumors of thenasal cavity, paranasalsinuses,andnasopharynx:aclinicopathologicstudy. 3.Cartilaginoustumors(chondroma,chondrosarcoma).Cancer. 1974;34:453---63.
2.BatsakisJG,RiceDH.Thepathologyofheadandnecktumors: vasoformativetumors,part9A.HeadNeckSurg.1981;3:231---9. 3.MacomberW,WangM.Thehemangioma.GP.1953;8:41---9. 4.HellquistHB.Pathologyofthenoseandparanasalsinuses.
But-terworthsEditions;1990.
5.CalonjeE,FletcherCD.Sinusoidalhemangioma.Adistinctive benignvascularneoplasmwithinthegroupofcavernous heman-giomas.AmJSurgPathol.1991;15:1130---5.
6.JammalH,BarakatF,HadiU.Maxillarysinuscavernous heman-gioma:arareentity.ActaOtolaryngol.2004;124:331---3. 7.CiureaM,CiureaR,PopaD,ParvanescuH,MarinescuD,Vrabete
M.Sinusoidalhemangiomaofthearm:casereportandreview ofliterature.RomJMorpholEmbryol.2011;52:915---8. 8.EnjolrasO,WassefM,ChapotR.Coloratlasofvasculartumors
andvascularmalformations.CambridgeUniversityPress;2007. 9.VargasMC,CastilloM.Sinonasalcavernoushaemangioma:acase
report.DentomaxillofacRadiol.2012;41:340---1.