SOCIEDADE BRASILEIRA DE ORTOPEDIA E TRAUMATOLOGIA
w w w . r b o . o r g . b r
Original
Article
Functional
evaluation
of
repairs
to
circumferential
labral
lesions
of
the
glenoid
–
Case
series
夽
Alexandre
Tadeu
do
Nascimento
∗,
Gustavo
Kogake
Claudio
HospitalOrthoservice,GrupodeOmbroeCotovelo,SãoJosédosCampos,SP,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received15September2015 Accepted20October2015 Availableonline9August2016
Keywords:
Jointcapsule Jointinstability Shoulderjoint Arthroscopy Retrospectivestudies
a
b
s
t
r
a
c
t
Objective:Toevaluatetheclinicalresultsamongpatientsundergoingarthroscopicrepairof
circumferentiallabrallesions.
Methods:Thiswasaretrospectivestudyon10patientswhounderwentarthroscopicrepair
tocircumferentiallabrallesionsoftheshoulder,betweenSeptember2012andSeptember 2015.ThepatientswereevaluatedbymeansoftheCarter-Rowescore,DASHscore,UCLA score,visualanalogscale(VAS)forpainandShort-Form36(SF36).Theaverageageatsurgery was29.6years.Themeanfollow-upwas27.44months(range:12–41.3).
Results:The meanscorewas16 pointsforDASH;32 pointsforUCLA,amongwhichsix
patients(60%)hadexcellentresults,three(30%)goodandone(10%)poor;1.8pointsfor VAS,amongwhichninepatients(90%)hadminorpainandone(10%)moderatepain;79.47 forSF-36;and92.5forCarter-Rowe,amongwhichninepatients(90%)hadexcellentresults andone(10%)good.Jointdegenerationwaspresentinonecase(10%),ofgrade1.Wedid notobserveanysignificantcomplications,exceptforgrade1glenohumeralarthrosis,which onepatientdevelopedaftertheoperation.
Conclusion: Arthroscopicrepairofcircumferentiallabrallesionsoftheshoulderthroughuse
ofabsorbableanchorsiseffective,withimprovementsinallscoresapplied,anditpresents lowcomplicationrates.Casesassociatedwithglenohumeraldislocationhavelower long-termresidualpain.
©2016SociedadeBrasileiradeOrtopediaeTraumatologia.PublishedbyElsevierEditora Ltda.ThisisanopenaccessarticleundertheCCBY-NC-NDlicense(http:// creativecommons.org/licenses/by-nc-nd/4.0/).
Avaliac¸ão
funcional
do
reparo
de
lesões
labrais
circunferenciais
da
glenoide
–
Série
de
casos
Palavras-chave:
Cápsulaarticular Instabilidadearticular Articulac¸ãodoombro
r
e
s
u
m
o
Objetivo:Avaliarosresultadosclínicosdospacientessubmetidosareparoartroscópicode
lesãolabralcircunferencial.
Métodos:Estudoretrospectivode10pacientessubmetidosaoreparoartroscópicodelesão
labralcircunferencial doombrodesetembrode 2012asetembrode2015.Ospacientes
夽
WorkconductedattheHospitalOrthoservice,GrupodeOmbroeCotovelo,SãoJosédosCampos,SP,Brazil.
∗ Correspondingauthor.
E-mail:dr.nascimento@icloud.com(A.T.Nascimento). http://dx.doi.org/10.1016/j.rboe.2016.08.005
residualemlongoprazo.
©2016SociedadeBrasileiradeOrtopediaeTraumatologia.PublicadoporElsevier EditoraLtda.Este ´eumartigoOpenAccesssobumalicenc¸aCCBY-NC-ND(http:// creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
Labral lesions and glenohumeral instability are common injuries in populations of athletes and blue-collar work-ers. Anterior labral lesions (Bankart) were first described byPerthes1 and Bankart.2 Superior labrallesionswere first
describedbyAndrewsetal.3inapopulationofthrowing
ath-letes. Snyder et al.4 later classified SLAP lesions into four
categories;5%outof2375lesionswererankedascomplex,i.e., thoselesionscouldnotbeclassifiedasthetypes/associated typesdescribed.TheassociationbetweenBankartlesionsand SLAP lesions is well known; arthroscopic repair has been associatedwithgood results,5–8 but the treatmentofother
combinationsoflabrallesionshasrarelybeendescribed. Withtheadvancementofarthroscopy,thecombinationof labrallesions that appearasa circumferential detachment oftheentireglenoid labrumhas beenacknowledged. Pow-elletal.9classifiedthisinjuryasapan-labralSLAPlesionor
typeIX.LoandBurkhartdescribedtriplelabrallesions (ante-rior,posterior,andSLAPtypeII)inaretrospectivereviewof sevenpatients.Twoofthesevenpatientshadcircumferential detachmentofthelabrum.Alltheseinjurieswere repaired arthroscopicallywithfixationanchors,withnocasesof insta-bilityrecurrence.10
This study aimed to report a series of ten patients, presentingscorestoevaluatethefunctionaloutcomeof treat-mentofcircumferentiallabrallesions.
Material
and
methods
BetweenSeptember 2012and September2015,tenpatients underwent arthroscopictreatment ofcircumferentiallabral lesions and were operated inthe Orthoservice Hospital in SãoJosédosCampos(SP)byasinglesurgeon.The distribu-tionaccordingtoageandactivitywithprobableassociation withthediseaseisshowninTable1.Allpatientsweremale. Thestudy included patients withoneor moreepisodes of anteriorshoulderdislocationorsymptomsandexamination compatible with hidden instability or higher labral lesion
Table1–Patients’clinicaldata.
Patient Age Activity
1 52 Blue-collarworker
2 26 Athlete
3 41 Blue-collarworker
4 29 Athlete
5 18 Athlete
6 31 Athlete
7 32 Blue-collarworker
8 20 Athlete
9 18 Athlete
10 35 Blue-collarworker
Mean 30.2
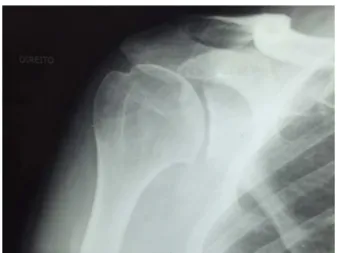
aftermagneticresonanceimaging(MRI,Fig.1).Theminimum follow-up wasdefinedasoneyear.Exclusioncriteriainthe selectionofpatients comprisedcasesoftraumatic disloca-tionassociatedwithnerveandvascularinjuries,traumacases relatedtofracturesatothersitesoftheshouldergirdle, Hill-Sachslesioninvolvingmorethan25%ofhumeralhead,and Bankartlesioninvolvingmorethan25%oftheglenoid.
Fig.2–Circumferentiallabrallesion.
Preoperativeperiod
Preoperatively,allpatientsunderwentclinicalevaluationfor thediagnosisandclassificationofshoulderinstability, func-tion,andpain,usingtheRowe,DASH,UCLA,VAS,andSF-36 scores.Patientsunderwent preoperativeMRI,but thelabral lesionwas detectedpreoperatively inonlythreeoftheten cases.Intheothercases,indicationforsurgerywastorepair justonelabralsegment,butacircumferentiallabrallesionwas evidencedintraoperatively.
Surgicaltechnique
Thesurgicalprocedurewasdonewiththepatientunder gen-eralanesthesiaandbrachialplexusblockade,positionedinthe lateraldecubituspositionoppositetotheinjuredshoulder.
On the surgical table, vertical and longitudinaltraction were applied;limb wasmaintained atabout 60 degrees of abductionand15degreesofflexionthroughfixedlongitudinal andverticaltraction,using5kgweights.
Theanterior,anterolateral,andposteriorportalswereused intherepair;thearthroscopewaspositionedinthe anterolat-eralportal.Forallcases,completeinspectionofthejointwas madetoevaluateassociatedlesionsandtoconfirmthatthe lesionwasindeedcircumferential(Fig.2).Afterproper prepa-rationoftheglenoid,thelesionswererepairedprimarilyinthe posteriorregionwiththreeanchors.Then,theupperregion wasrepaired withone anchorand the anterior with three anchors;atotalofsevenanchors(allabsorbable)wereused
toachieveacompleterepairofthelesion(Fig.3).Whena rota-torcuffwasassociated,itwasproperly repairedtoheal all injuries(onecase).
Postoperativeperiod
Patientsremainedundercontinuousimmobilizationinasling forfourweeks,afterwhichtherehabilitationprocessstarted. Physical therapy was initially indicated only for range of motiongain;onlywhenthiswascompletedwasthe muscle-strengtheningphaseinitiated.
Clinicalevaluation
Allstudypatientshadaminimumpostoperativefollow-upof 12months.Allpatientsweremale;ninerightshouldersand oneleftshoulderwereoperated.
Questionnaireswereappliedtopatientsintheroutine pre-operative assessmentand postoperatively atthree and six months,andatoneyear,twoyears,andthreeyearsincases withcompletefollow-up.
Operative results were quantified through the Carter-Rowe,11DASH,UCLA,VAS,andSF-36scores.
Results
In the clinical evaluation with the DASH, UCLA, VAS, and Carter-Rowescores,ameanpostoperativescoreof16points wasobservedfortheDASHscore;32pointsfortheUCLAscore
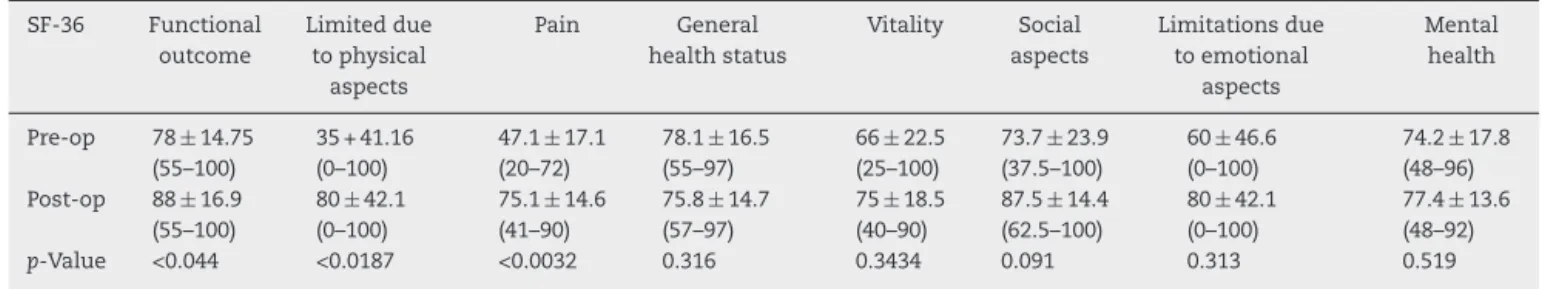
SF-36 Functional outcome Limiteddue tophysical aspects Pain General healthstatus Vitality Social aspects Limitationsdue toemotional aspects Mental health
Pre-op 78±14.75 (55–100)
35+41.16 (0–100)
47.1±17.1 (20–72)
78.1±16.5 (55–97)
66±22.5 (25–100)
73.7±23.9 (37.5–100)
60±46.6 (0–100)
74.2±17.8 (48–96) Post-op 88±16.9
(55–100)
80±42.1 (0–100)
75.1±14.6 (41–90)
75.8±14.7 (57–97)
75±18.5 (40–90)
87.5±14.4 (62.5–100)
80±42.1 (0–100)
77.4±13.6 (48–92)
p-Value <0.044 <0.0187 <0.0032 0.316 0.3434 0.091 0.313 0.519
a Valuesarepresentedasmeanandstandarddeviation;therangeisshowninparentheses.
Table4–Comparisonofresultsbetweenthegroupofathletes(withepisodesofdislocation)withthegroupofblue-collar workers(withepisodesofdislocation).a
UCLA DashH Rowe VAS
Athletes 34.16±0.7
(33–35)
4.44±3.5 (0.83–10.83)
95±5.4 (90–100)
0.5±0.5 (0–1) Blue-collar
workers
28.75±6.8 (19–34)
31.14±32.8 (7.5–77.5)
88.75±10.3 (75–100)
3.7±2.2 (2–7)
0.211 0.201 0.326217 0.058
a Valuesarepresentedasmeanandstandarddeviation;therangeisshowninparentheses.
Table5–ComparisonofSF-36resultsbetweenthegroupofathletes(withepisodesofdislocation)withthegroupof blue-collarworkers(withepisodesofdislocation).a
Functional outcome Limiteddue tophysical aspects Pain General healthstatus Vitality Social aspects Limitationsdue toemotional aspects Mental health
Athletes 96.7±4.08 (90–100)
100±0 (100)
83.3±5.16 (74–90)
85±11.3 (67–97)
80±10.4 (60–90)
95.83±10.2 (75–100)
100±0(100) 85.6±4.45 (80–92) Blue-collar
workers
75±19.5 (55–100)
50±57.7 (0–100)
62.75±15.5 (41–74)
62±4.08 (57–67)
60±23.09 (40–80)
75±10.2 (62.5–87.5)
50±57.7 (0–100)
65±13.6 (48–76)
p-Value 0.056 0.09 0.03 0.001 0.09 0.008 0.09 0.02
a Valuesarepresentedasmeanandstandarddeviation;therangeisshowninparentheses.
(six[60%]excellentresults,three[30%]good,and onepoor [10%]);1.8pointsintheVAS(nine[90%]casesofmildpainand one[10%]caseofmoderatepain);and92.5intheCarter-Rowe score(nine[90%]excellentresults,one[10%]good).Overall SF-36scorewas79.85.Table2presentsthecomparisonbetween thepre-andpost-operativeresults,analyzedwithStudent’s
t-test,andTable3presentstheSF-36results,stratifiedinto its eight areas and analyzed with the t-test. None of the patientshadanewepisodeofglenohumeraldislocation.One patienthadpooroutcomeassociatedwiththedevelopment ofglenohumeralarthrosis.Comparingthefinalresultthrough Student’st-test,theresultswereanalyzedseparatelybased ontheprimarypathology,i.e., thecasesoffrank instability (athletes)were compared withcasesin which, despitethe
signsonphysicalexamination,thepatienthadnohistoryof glenohumeral dislocation (blue-collar workers). Results are describedinTables4and5.Sevenabsorbableanchorswere usedforlabralrepair,withthreeanchorstorepairtheposterior labrum,oneforsuperiorlabrumrepair,andthreeforanterior labrum.Therepairsequencewasalwaysposteriortoanterior; thesuperiorlabrumwasrepairedbetweenthesetwo.Torepair theposteriorlabrum,asmallerdiametercannulawasusedin allcases,anditwasalwaysuseddespitethesmallposterior space.
Tables 2and 3 show the statisticallysignificant results,
Fig.4–Glenohumeralarthritis,Samilsongrade1.
nostatisticallysignificantdifferenceswerethoserelatingto qualityoflifeandemotionalaspects.
Tables4and5presentnon-statisticallysignificantresults,
p>0.05,forthemainfunctionaldifferencesandpainscores (Table4);regardingSF-36(Table5),ofthequestionsthatassess functionandpain,onlythequestiononpainhadsignificant differencebetweenthegroups.Therewasasignificant differ-enceforresultsofqualityoflifeandmentalhealth.
Onepatienthadsubscapularisand supraspinatusinjury associatedwiththelabrallesion.Inthiscase,inadditiontothe repairofthelabralinjury,theaforementionedtendonswere alsorepaired. Patient presentedan equally good outcome, withthefollowingresults: DASH,8.33;UCLA,34;Rowe,90; VAS,2;andSF-36,82.4.Whenassessingthecasesseparately, it wasobservedthat onepatient hada bad outcome,with lowscores(DASH,77.5;UCLA,19;Rowe,75;VAS,7;andSF-36, 47.24),whichwereassociatedwiththedevelopmentof gleno-humeralarthrosispostoperatively(Fig.3).Oneofthepatients isaprofessionalrugbyathleteandwasabletoreturntothe samelevelofperformancewithoutsymptoms.Theother ath-leteswereamateursandwereallabletoreturntothesame levelofactivitypriortotheinjury.Ofthefourblue-collar work-ers,oneisretired,onewasabletoreturntoactivities,andtwo areinadaptedwork,havingfailedtoreturntotheprevious activity(Fig.4).
Discussion
Littlehasbeenwrittenaboutcircumferentiallabrumglenoid injuries.4,7,8,12,13Powelletal.9firstdescribedacircumferential
labrallesionasaSLAPinjurytypeIX.Inaretrospectivestudy, LoandBurkhart10describedpatientswithanteriorBankart,
posteriorBankart,and typeIISLAP associatedlesions.Two oftheinjurieswerecircumferential.Theauthorsnotedthat these lesions represented 2.4% of all labral lesions and believedthattheinjurybeganwithatraumaticevent,with anteriordislocationinabductionandexternalrotation. Poste-riorinstabilityandpan-labrallesionswouldbeanextension of anterior instability.4,8,14 Similarly, in the present series,
sixshouldershad ahistoryofanterior instability.However, incaseswheretherewasno historyofinstability,patients
reportedworking forhourswithequipment thatgenerated vibrationandthusmicrotrauma,withthearminabduction andexternalrotationposition.Circumferentiallabrallesions tendtobemoresymptomatic,evenintheabsenceofarecent episodeofdislocation.Ascircumferential labrallesionsare difficult to diagnose based solely on history and physical examination,the orthopedistshouldhaveahigh suspicion whenexaminingashoulderwithseveralepisodesof disloca-tion,substantialpainintheabsenceofarecentepisode,and provocativemaneuversthatreproducesymptomsbothinthe anterior,posteriorandsuperiorregions.Insuchsituations,a magneticresonancearthrographymayaidanaccurate diag-nosis,sinceinthepresentstudy,eventhougha1.5TMRIwas used,labrallesionswereonlydiagnosedascircumferentialin threeofthetencases.Thepresentsurgicalapproachfollowed thetechniquepublishedbyTokishetal.,15exceptforthefact
thatitbeganbyposteriorrepairratherthanSLAPrepair,as describedearlier.Thereasoningforrepairingallpartsofthe pan-labrallesionisbasedonthefactthatevenifthe instabil-ityisanterior,forexample,damagetootherportionsofthe labrummaycontributetoinstability,pain,andpoorhealing oftherepairedlabralregion.10,15 Neeretal.16described the
associationofsurgicaltreatmentofshoulderdislocationwith thedegenerationofthatjoint.In1983,SamilsonandPrieto17
coinedtheterm“instabilityarthropathy”andradiographically classifiedthatentity.
Theresultsofthepresentstudy,afterameanof2.5years offollow-up,wereverygood.Allpatientsshowedsignificant improvementinallevaluatedscoresinrelationshiptopain, function,andsensationofinstability,exceptforonepatient whoobservedasmallimprovement.Astatisticallysignificant improvementwasobservedinallscores.Improvementwas morepronouncedincasesrelatedtoinstability(athletes)than incasesinwhichtherewasnofrankinstability(blue-collar workers);nonetheless,despitethistrendofbetterresultsin thatgroup,thedifferenceinmostofthescoreswasnot sta-tisticallysignificant.Thefailurerateinthepresentstudywas 10%(withonecasethatevolvedtoglenohumeralarthrosis, albeitincipient).Authorsbelievethat,inthiscase,thejoint degeneration has occurred due to the surgical treatment, asthispatientdidnothavefrankinstability.Itislikelythat thereisstillsomeinfluencefromworkactivityontheresults presentedbytheblue-collarworkers;theonlyresultthatwas similartoathletesinallscoreswasthatoftheretiredpatient, despitehisage.
The authors also emphasize that circumferential labral lesionsaredifficulttodiagnoseatphysicalexamination;signs ofanteriorinstabilityorSLAP injuryaremoreevident.MRI withoutcontrastwasnotveryhelpfulfortheidentificationof theselesions.Duetothedifficultyofpreoperativediagnosis, thesurgeonmaybesurprisedbythisinjuryduringthe proce-dure;thepatientmaybepositionedinanon-idealpositionfor completerepairoranadequatenumberofanchorsmaynot beavailableforcompleterepairofthelesion.
Conclusion
r
e
f
e
r
e
n
c
e
s
1. PerthesG.Uberoperationenbeihabituellerschulterluxation. DeutscheZChir.1906;85:199–222.
2. BankartA.Thepathologyandtreatmentofrecurrent dislocationoftheshoulderjoint.BrJSurg.1938;26:23–9. 3. AndrewsJR,CarsonWGJr,McLeodWD.Glenoidlabrumtears
relatedtothelongheadofthebiceps.AmJSportsMed. 1985;13(5):337–41.
4. SnyderSJ,KarzelRP,DelPizzoW,FerkelRD,FriedmanMJ. SLAPlesionsoftheshoulder.Arthroscopy.1990;6(4):274–9. 5. BurkhartSS,MorganC.SLAPlesionsintheoverheadathlete.
OrthopClinNorthAm.2001;32(3):431–41.
6. MusgraveDS,RodoskyMW.SLAPlesions:currentconcepts. AmJOrthop(BelleMeadNJ).2001;30(1):29–38.
7. SnyderSJ,BanasMP,KarzelRP.Ananalysisof140injuriesto thesuperiorglenoidlabrum.JShoulderElbowSurg. 1995;4(4):243–8.
12.MaffetMW,GartsmanGM,MoseleyB.Superiorlabrum–biceps tendoncomplexlesionsoftheshoulder.AmJSportsMed. 1995;23(1):93–8.
13.WilliamsRJ3rd,StricklandS,CohenM,AltchekDW,Warren RF.Arthroscopicrepairfortraumaticposteriorshoulder instability.AmJSportsMed.2003;31(2):203–9.
14.TokishJM,KrishnanSG,HawkinsRJ.Clinicalexaminationof theoverheadathlete:thedifferential-directedapproach.In: KrishnanSGH,HawkinsRJ,WarrenRF,editors.Theshoulder andtheoverheadathlete.Philadelphia:LippincottWilliams andWilkins;2004.p.23–49.
15.TokishJM,McBratneyCM,SolomonDJ,LeclereL,DewingCB, ProvencherMT.Arthroscopicrepairofcircumferentiallesions oftheglenoidlabrum.JBoneJointSurgAm.
2009;91(12):2795–802.
16.NeerCS2nd,WatsonKC,StantonFJ.Recentexperiencein totalshoulderreplacement.JBoneJointSurgAm. 1982;64(3):319–37.