REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
OfficialPublicationoftheBrazilianSocietyofAnesthesiologywww.sba.com.br
SCIENTIFIC
ARTICLE
The
impact
of
different
antiepileptic
drugs
on
the
sedation
of
children
during
magnetic
resonance
imaging
Isil
Davarci
a,∗,
Murat
Karcioglu
a,
Kasim
Tuzcu
a,
Fatmagul
Basarslan
b,
Ramazan
Davran
c,
Erhan
Yengil
d,
Cahide
Yilmaz
b,
Selim
Turhanoglu
aaDepartmentofAnesthesiology,FacultyofMedicine,MustafaKemalUniversity,Hatay,Turkey bDepartmentofPediatry,FacultyofMedicine,MustafaKemalUniversity,Hatay,Turkey cDepartmentofRadiology,FacultyofMedicine,MustafaKemalUniversity,Hatay,Turkey dDepartmentofFamilyMedicine,FacultyofMedicine,MustafaKemalUniversity,Hatay,Turkey
Received16September2013;accepted31October2013
Availableonline11December2013
KEYWORDS
Epilepsy; Pediatric; Antiepileptics; Sedation; MRI
Abstract
Backgroundandobjectives: Theinduction andinhibitionofcytochrome P450isoenzymes by antiepilepticdrugsleadtochangesintheclearanceofanestheticdrugseliminatedviahepatic metabolism.Weinvestigatedthedurationofthesedationandadditionalanestheticneeds dur-ingmagneticresonanceimaginginepilepticchildrenreceivingantiepilepticdrugsthatcause eitherenzymeinductionorinhibition.
Methods:In American Society of Anesthesiology I---II, 120 children aged 3---10 years were included. Group 1: children using antiepileptic drugs that cause cytochrome P450 enzyme induction;Group2:thoseusingantiepilepticdrugsthatcauseinhibition;andGroup3:those thatdidnotuseantiepilepticdrugs.Sedationwasinducedwiththeuseof0.05mgkg−1
mida-zolamand1mgkg−1 propofol.Anadditional0.05mgkg−1ofmidazolamandrescuepropofol
(0.5mgkg−1)wereadministeredandrepeatedtomaintainsedation.Thedurationofsedation
andtheadditionalsedationneededwerecompared.
Results:The durationoftheinitialdosewas significantlyshorterinGroup Icompared with groupsIIandIII(p=0.001,p=0.003,respectively).ItwassignificantlylongerinGroupII com-paredwithgroupsIandIII(p=0.001,p=0.029,respectively).Theadditionalmidazolamneeded foradequatesedationwasincreasedinGroupIwhencomparedwithgroupsIIandIII(p=0.010,
p=0.001,respectively).Inaddition,therescuepropofoldosewassignificantlyhigheronlyin GroupIwhencomparedwithGroupIII(p=0.002).
Conclusion:Inepilepticchildren,theresponsevariabilitytotheinitialsedativeagentsduring themagnetic resonanceimaging procedureresultingfromtheinhibitionorinductionofthe cytochromeP450isoenzymesbytheantiepilepticdrugsmandatedthetitrationofanesthetic agents.
©2013SociedadeBrasileiradeAnestesiologia.PublishedbyElsevier EditoraLtda.Allrights reserved.
∗Correspondingauthor.
E-mail:isildavarci@gmail.com(I.Davarci).
PALAVRAS-CHAVE
Epilepsia; Pediátrica; Antiepilépticos; Sedac¸ão; RM
Impactodediferentesmedicamentosantiepilépticosnasedac¸ãodecrianc¸asdurante aressonânciamagnética
Resumo
Justificativaeobjetivos: A induc¸ão e a inibic¸ão das isoenzimas do citocromo P450 pelos medicamentosantiepilépticoslevamaalterac¸õesnadepurac¸ãodemedicamentosanestésicos eliminadospelometabolismohepático.Investigamosadurac¸ãodasedac¸ãoeanecessidade adi-cionaldeanestésicosdurantearessonânciamagnéticaemcrianc¸asepilépticasquereceberam antiepilépticosquecausamainduc¸ãoouainibic¸ãodeenzimas.
Métodos: Foramincluídasnoestudo120crianc¸as,estadofísicoASAI-II,entre3-10anos.Grupo 1:emusodeantiepilépticosquecausamainduc¸ãodeenzimasdocitocromoP450;Grupo2: emusodeantiepilépticosquecausamainibic¸ãodeenzimasdocitocromoP450;eGrupo3:que nãousavamantiepilépticos.Asedac¸ãofoiinduzidacommidazolam(0,05mgkg−1)epropofol
(1mgkg−1).Umadicionalde0,05mgkg−1demidazolameresgatecom0,5mgkg−1depropofol
foramadministradoserepetidosparamanterasedac¸ão.A durac¸ãodasedac¸ãoeasedac¸ão adicionalnecessáriaforamcomparadas.
Resultados: Adurac¸ãodadoseinicialfoisignificativamentemenornoGrupoIemcomparac¸ão comosgruposIIeIII(p=0,001,p=0,003,respectivamente)esignificativamentemaiornoGrupo IIemcomparac¸ãocomosgruposIeIII(p=0,001,p=0,029,respectivamente).Anecessidade demidazolamadicionalparasedac¸ãoadequadafoimaiornoGrupoIemcomparac¸ãocomos gruposIIeIII(p=0,010,p=0,001,respectivamente).Alémdisso,adosederesgatedepropofol foisignificativamentemaiorapenasnoGrupoIemcomparac¸ãocomoGrupoIII(p=0,002).
Conclusão:Emcrianc¸asepilépticas,avariabilidadedarespostaaosagentessedativosiniciais durantearessonânciamagnética,resultantedainibic¸ãoouinduc¸ãodasisoenzimasdocitocromo P450pelosmedicamentosantiepiléticos,exigiuatitulac¸ãodosagentesanestésicos.
©2013SociedadeBrasileira deAnestesiologia.PublicadoporElsevierEditoraLtda.Todosos direitosreservados.
Introduction
Epilepsyisthemostcommonchronicneurologicaldisorder amongchildrenandischaracterizedbyparoxysmalattacks.1
Magneticresonanceimaging(MRI)is agenerallypreferred imagingmodalityinthemanagementofepilepticchildren.2
InMRIprocedures,theselectionofanestheticagentswith anticonvulsantactivityaswellasdruginteractionsbetween antiepilepticdrugs(AEDs)andanestheticsareintegral com-ponentsoftheanestheticplanforpatientswithepilepsy.3,4
The induction andinhibition ofcytochrome P450 (CYP-450) in liver metabolism comprise the most important mechanisminpharmacokineticdruginteractionsregarding AEDs.4 Commonly used AEDs, such as phenytoin,
carba-mazepine,primidoneandphenobarbitalinduceseveralCPY isoenzymes(CYP1A2,CYP2C9,CYP2C19andCYP3A4)aswell as UDP-glucuronyl transferase (UGT) and epoxide hydro-lases;onthecontrary,valproicacidis themostimportant inhibitorof theenzymes(CYP2A6,CYP2B6andCYP2C9)in drugmetabolism.3,5
It has been demonstrated that these isoenzymes are involvedinthemetabolisminover50%ofanestheticagents. Midazolam,oneofthemostwidelyusedanestheticagents withanticonvulsantactivity inMRIprocedures,is metabo-lizedbyCYP3A4/CYP3A5,whereaspropofolismetabolized byCYP2C9,CYP2B6andUGTs.Thus,thealterationsinthe distributionandclearanceresultingfromthesimultaneous useofanestheticsthatsharethesamemetabolicpathways withAEDswillchangethedurationofsedationandthe seda-tionlevelneeded.6---8
In thepresent study, we aimedtoinvestigate whether therewasadifferenceintermsoftheadequatedurationof sedation,theadditionalsedative agentusedorneeded to rescuesedativeagentsamongepilepticchildrenusingAEDs thatcauseeitherenzymeinduction orinhibition, orthose thatdidnotuseAEDsundermidazolam-propofolanesthesia duringMRI.
Materials
and
methods
This study was approved by the Ethics Committee of theInstitutional HumanResearch Boardof MustafaKemal University. Overall, 120 children with epilepsy (American Society of Anesthesiology (ASA) I, II; aged 3---10 years) undergoingcranialMRIwithsedationwereincludedinthis prospectiveclinicaltrial.
Epileptic children were classified into three groups as follows:Group1,childrenusingagentsthatcauseCYP-450 induction(n=30);Group2,childrenusingagentsthatcause CYP-450inhibition(n=30);andGroup3,thosenotreceiving AEDs(n=60).
The day before the MRI, all patients were assessed by an anesthesiologist, including history of current dis-ease,medicalhistoryandphysicalexamination.Allparents were informed of the fasting periods allowed under the AmericanSocietyofAnesthesiologistsPreprocedureFasting Guidelines.9,10
tonsilhypertrophy,thosewithgastroesophagealrefluxorfull stomach,obesechildren,thosewithsleep-apnea,andthose withabnormalrenal function testsor a historyof allergy againstagents used in the study or a history of difficulty in previous MRI procedures were excluded. Children with accompanying diseases such as cerebral palsy or mental-motorretardationwerenotexcludedfromthestudy.
Before the procedure, written informed consent was obtainedfromparents.Demographic datasuchasweight, ageandgender,ASAstatus,historyofepilepsy,antiepileptic medicationandaccompanyingdiseaseswererecorded.Inall patients,0.5mgkg−1midazolamwasgivenorallybymixing
itintoaparticle-freefruitjuicefor premedication 30min beforethe intravenous catheter placement, and patients weretakenintotheMRIroomwhentheParentalSeparation Anxiety Scale reached 1---2.11,12 The time from
premedi-cationwithoral midazolamtoarrivalintheMRIroomwas referredtoasthetimeofreadinessfortheprocedure (seda-tionready).In both groups, 0.05mgkg−1 midazolam (i.v.)
wasgiven asthe primarysedative, followed by 1mgkg−1
propofolfor30s.Thesedationlevelwasassessed through-outtheimagingprocedurewiththeUniversityofMichigan Sedation Scale (UMSS)13 and it was considered adequate
whenpatientscouldbeawakenedonlybysignificant physi-calstimulus.Thetimetoarriveatasufficientsedationlevel (UMSS=3)wasreferredtoastheinductiontime.Toprevent thepainof thepropofolinjection,0.25mgmL−1 lidocaine
wasaddedtothesamesyringe.14
Whensedationandimmobilizationcouldnotbeachieved during the imaging procedure, a midazolam dose was titratedby0.05mgkg−1 increments(maximum increment:
1mgandmaximumtotaldose:0.1mgkg−1),andapropofol
bolusof0.25---0.5mgkg−1wasgivenasarescuedosewhen
midazolamtitrationfailed.The durationbetween the ini-tialdoseandtheadditionalsedationneededwasdefinedas UMSS<3andmovementofpatientcausingtorepeated imag-ingprocedure. Discomfort or inevitable movement of the childrenresultedinthecancellationoftheimagingdespite thefactthatsedationwasconsideredasinadequate seda-tion.
The heart rate and peripheral oxygen saturation were monitoredduringtheprocedure(MILLENNIA3155MVS,USA) andrecordedat5-minintervals.Non-invasivebloodpressure measurementswereonlyperformedbeforeandattheend oftheprocedureasitcouldcauseawakeningduetomuff.9
Clinically,hypotensionwasdefinedasa20%ormore reduc-tioninsystolicarterypressurecomparedwiththebaseline value.14
Allchildrenwereprotectedfromnoiseduringthe proce-dureandsupplementedwith2mLmin−1O
2viaafacemask
inordertomaintainspontaneousrespiration.Intervention decisionsweremadein casesofSpO2<94%, apnea lasting
20s(apnea),adecreaseintheheartratebymorethan20% comparedtothebaselinevalue(bradycardia)and arrhyth-mias. Airwaysupportmaneuverswere performed incases ofairwayobstructionandhypoxia,includingtactile stimu-lus,chinlifting,airwayplacementandbag-maskventilation afterthediscontinuationoftheMRI.14Inaddition,adverse
eventsoccurringduringinduction,MRIandbeforedischarge wererecorded,includingnausea,vomiting,apnea,cough, hiccup,irritability, agitation,allergicreaction and aspira-tion.
Dataregardingproceduretime,terminationorrepetition oftheMRIprocedure,andadditionalmidazolamorpropofol applicationswererecordedforallpatients.Thedurationof theprocedurewasdefinedasthetimefromtheinitiationof theMRIproceduretoitscompletion,includinginterruptions. When the imaging procedure was completed, children weretransferredtotherecoveryroomwithinthemagnetic resonance (MR)unit andobserved byparents and anurse anesthesiologist. Recovery time was defined as the time fromcompletionoftheMRIproceduretothedischargefrom therecoveryroom(ModifiedAldretescore≥8andComfort Scalescore≥3).14,15Thechildrenwerethentransferredto
thedepartmentofpediatricsandweredischargedaftervital signsandlevelsofconsciousnessreturnedtobaselinevalues. Parents’level ofsatisfactionwith thesedation experi-encewasassessedonthebasisofa4-pointLikertscale(very dissatisfied,somewhatdissatisfied,somewhatsatisfiedand verysatisfied). The qualityof MRsequences wasassessed according to the presence/absence of artifacts resulting frommovement of thepatientby aradiologist blindedto patients and sedation technique via a 3-point scale: (1) excellent,noartifactduetomovement;(2)procedurewas completedwithminormovement;and(3)majormovement andabortedprocedure.16
Inaddition,aphoneinterviewwasconducted24hafter discharge by a blinded anesthesiology resident regarding delayedadverse events,nocturnalenuresis,insomnia,and nightmares.
Statisticalanalysis
SPSSforWindowsversion13.0(StatisticalPackageforSocial Sciences)wasusedforallstatisticalanalyses.Sample size estimateswerebasedonthedurationoftheinitialdose(in minutes).Itwasestimatedthatasamplesizeof21pergroup wouldprovide80%powertodetectaclinicallymeaningful difference of 1.5min when the accepted standard devia-tionwas8.3 andthe˛error was0.05.Standard deviation
wasdeterminedbasedonapilotstudyonepilepticchildren undergoingMRI.
The normal distribution of continuous variables was testedwiththeKolmogorov---Smirnovtest.Chi-squaretests wereusedfor comparisonsbetween categoricalvariables. Kruskal---Wallis and Mann---Whitney U tests were used in the comparisons of continuous variables between groups.
p<0.05wasconsideredsignificantforallstatisticaldata.
Results
Thedatawereobtainedfrom120epilepticchildren,using antiepileptic agents for focal or generalized convulsions, whohadnoMRIscanandreceivedsedationforMRIthatwas performedforinitialdiagnosis orforevaluatingthe remis-sion course aswell as the management of accompanying diseasesduringaperiodof19monthsbetweenSeptember, 2012andApril,2013.
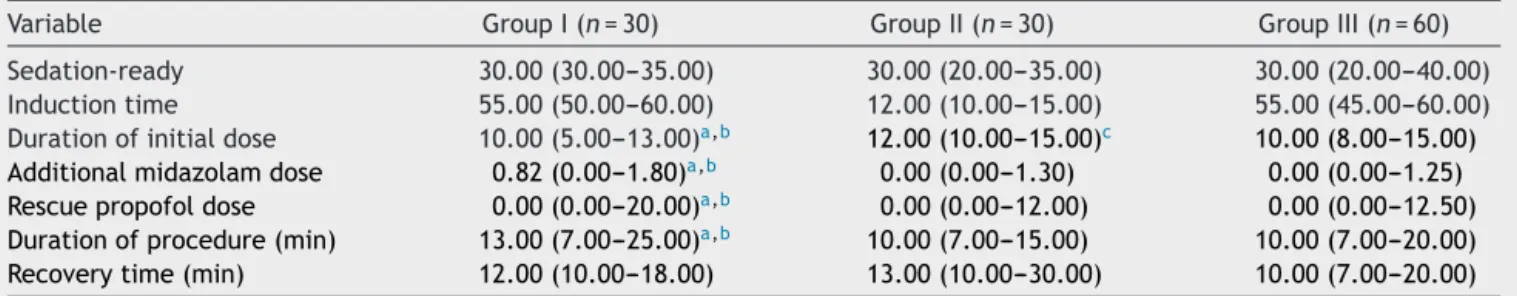
Table1presentsthedemographicdataandthe propor-tionofpatientswiththerateofaccompanyingdiseases in bothgroups.ProceduraldataarepresentedinTable2.
Table1 Patientscharacteristicdata.
GroupI(n=30) GroupII(n=30) GroupIII(n=60) p
Sex
Male(%) 12(40%) 14(46.7%) 22(36.7%) 0.659
Female(%) 18(60%) 16(53.3%) 38(36.3%)
Age(month) 7.0(3.0---10.0) 8.0(3.0---10.0) 5.0(3.0---10.0)a 0.003a
Weight(kg) 22.0(10.0---36.0) 22.5(10.0---35.0) 16.0(10.0---30.0)a 0.001a
ASAI/II 17/13 14/16 27/33 0.567
Rateofaccompanying(%) 11(36.7%) 13(43.3%) 25(41.7%) 0.856
n,numberofcases.
Resultsarepresentedasmedian(min---max)exceptforgender,rateofaccompanyingandASAphysicalstatus(count).
a p<0.05.
Table2 Proceduraldatainthreegroups.
Variable GroupI(n=30) GroupII(n=30) GroupIII(n=60)
Sedation-ready 30.00(30.00---35.00) 30.00(20.00---35.00) 30.00(20.00---40.00)
Inductiontime 55.00(50.00---60.00) 12.00(10.00---15.00) 55.00(45.00---60.00)
Durationofinitialdose 10.00(5.00---13.00)a,b 12.00(10.00---15.00)c 10.00(8.00---15.00)
Additionalmidazolamdose 0.82(0.00---1.80)a,b 0.00(0.00---1.30) 0.00(0.00---1.25)
Rescuepropofoldose 0.00(0.00---20.00)a,b 0.00(0.00---12.00) 0.00(0.00---12.50)
Durationofprocedure(min) 13.00(7.00---25.00)a,b 10.00(7.00---15.00) 10.00(7.00---20.00)
Recoverytime(min) 12.00(10.00---18.00) 13.00(10.00---30.00) 10.00(7.00---20.00)
n,numberofcases.
Statisticallysignificantdifferences(p<0.05)werenotedasfollows:
a GroupIvsGroupII. b GroupIvsGroupIII. c GroupIIvsGroupIII.
The durationofantiepileptic medicationwassimilarin groups I and II (58.06±32.00mg, 59.60±33.50, respec-tively;p>0.05).
Thedurationoftheinitialdosewassignificantlyshorter inGroupIwhencomparedwithgroupsIIandIII(p=0.001and
p=0.003,respectively).ItwassignificantlylongerinGroup IIwhencomparedwithgroupsIandIII(p=0.001andp=0.29, respectively).Theinitialdoseprotocolwithmidazolamand propofolwasadequatetocompletetheMRIprocedurein11 patients (36.7%)in Group I;in 21patients (70%) inGroup II; and in 43 patients (71.7%) in Group III (p=0.03). For theremainingpatients,theneedforadditionalmidazolam for adequate sedation,an additionalmidazolam dose was increasedinGroup Iwhencomparedwithgroups IIandIII (p=0.010,p=0.001andp=0.003,p=0.001, respectively). AlsoitwasnotchangedinGroupIIcomparedwithGroupIII. Inaddition,therescuepropofoldosewassignificantlyhigher onlyinGroupIwhencomparedwithGroupIII(p=0.002).
No significant correlation was detected between the durationoftheantiepilepticmedicationandthedurationof theinitialdoseorthedoseneededforadditionalsedation ingroupsIandII.
The durationof the procedure was similarin groups II and III, while it was significantly higher in Group I when compared with groups II and III (p=0.034 and p=0.004, respectively).
Spontaneousrespirationwasachievedwithouttheneed for ventilation support in all patients. Temporary oxygen
desaturation(<95%)wasobservedinthreepatientsinGroup I(10%)andeachtwopatients(6.6%)inGroupIIandGroup IIIimmediatelyaftertheinitialsedationdose,whichrapidly respondedtotactilestimulus,includingslightneck exten-sionandchinsupport.
Although systolic arterial pressure was decreased to a level of 10% below the baseline value after sedation, hypotensionwasnot observedin anypatient.In addition, none of the patients experienced cardiovascular adverse events,such asbradycardia or arrhythmia duringor after sedation.TherecoverytimesafterMRIweresimilaramong thegroups.
Paradoxical reaction, early or delayed adverse effects werenot observed in any patient and therewas no case inwhichtheMRIprocedurecouldnotbecompleteddueto failureof sedation or a majormovement, and nopatient wasexcludedfromthestudyonthesegrounds.Allparents wereverysatisfiedwiththesedationexperience.No signifi-cantdifferencewasobservedinthequalityofMRsequences amongthegroups(p>0.05).
Discussion
oftheinitialdoseofmidazolam-propofolwasshorterin chil-drenusingAEDsthatcauseenzymeinduction,whileitwas prolongedinchildrenusingAEDsthatcauseenzyme inhibi-tionandinthosenotusingantiepilepticagents. Moreover, theresultsshowedthatadditionalsedationneedincreased inchildrenusingAEDsthatcauseenzymeinduction,whileit decreasedincasesusingAEDsthatcauseenzymeinhibition. We suggested thatthe variationin theduration of ini-tial doses resulted fromalterations in the metabolism of anestheticagents causedbyantiepilepticagentsthatuses commonmetabolicpathwayswithmidazolamandpropofol. Assuch,clinicalreflectionsontheinducerorinhibitory effectsof AEDsare alsodifferentin sedation procedures. The usage of AEDS that inhibit enzyme induction can shortenthesedationperiodofsedatives,therebyresulting inprolongedproceduraltimesduetofrequentrepetitions. Conversely,AEDswithinhibitoryeffectsmayprolong seda-tionaswellastherecoverytime.Bothsituationscancause dissatisfactioninchildrenandtheirparents,resultingina wasteoftimeandmoney.2,14,17
In our study, there was a need for additional doses; thus,thedurationoftheprocedurewasmarkedlyincreased becauseofsignificantlyshorteneddurationsundertheinitial midazolam-propofoldoseinchildrenusingAEDsthatcause enzymeinduction. Inastudy onepileptic children receiv-ingphenobarbitalmonotherapy,Ekeretal.2reportedthat
resultson theneed for additionalsedation andthe dura-tionofsedationwereinagreementwithourstudy.Similar resultshavebeendemonstratedinanimalmodelsregarding enzymeinduction.18,19
Althoughthedurationoftheinitialdosesof midazolam-propofolwassignificantlyprolongedinchildrenusingAEDs thatcauseenzymeinhibition,thisdidnotresultinproblems oradverseeffects.Also,itdidnotresultinaprolonged dura-tionoftheproceduresincetherewasnorepetitionofthe MRI.
No correlation was detected between the duration of theinitialmidazolam---propofoldoseandtheneedfor addi-tionaldoseswiththedurationofthemedication,including enzymeinducingorinhibitingagents.Theinductionor inhi-bitioncausedbyAEDswasconcentration-dependentandwas notrelatedtothedurationofthemedication.20---23Thus,our
resultsareinagreementwiththeliteratureinthisarea. Althoughthedemographiccharacteristics ofthegroups werelargelysimilar,GroupIIIconsistedofyoungeragesand lowermeanweights.Thisdifferencewasattributedtothe lowermeanageinchildrenwhounderwentevaluationsfor newdiagnosisinGroupIII.
WhilemetabolicinteractionsonspecificCYPisoenzymes mayvarydependingongeneticandenvironmentalfactors, pharmacokineticandpharmacodynamicvariationscanalso beobservedinrelationtoage.CYPandUGTisoenzymesare markedlydifferentiatedduringthematurationofchildren, andreachadultlevelsat2---3yearsofage.21 Wethinkthat
ourresultswerenotaffectedbythischangeinisoenzymes, despitethewideagerangeinourstudy,sincethreeyears ofagewasselectedasthelowerlimitofeligibility.
Acombination ofphenobarbitalor carbamazepine with anestheticagentswithasimilarprofileofactivitymayalso enhance anestheticeffects.1 In ourstudy,midazolam and
propofol were preferred because of the shorter time of actionandtheirassociationwithcomfortablerecovery.24In
addition,themajoradvantageofpropofolwasthelack of paradoxicalreactions.25Inagreementwiththeliterature,no
significant adverse effector complication,including para-doxicalreactions(sedation,agitation,andirritability)was observedinourpatients.
Inconclusion, AEDs have many physiological and phar-macologicaleffectsonanestheticagentsandarethemost importantconstituent ofthepracticeofanesthesia. Anes-thesiologistsshouldbeawareofimportantdruginteractions andunderlyingmechanismsinthesedationofchildrenusing antiepilepticagentsandrequireddosetitrationsshouldbe madebymeticulouslyobservingclinicalresponses.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.MaranhaoMV,GomesEA,deCarvalhoPE.Epilepsyand anesthe-sia.RevBrasAnestesiol.2011;61,124---236232---41,242---54. 2.EkerHE,YalcinCokO,AriboganA,etal.Childrenon
phenobar-bitalmonotherapyrequiresmoresedativesduringMRI.Paediatr Anaesth.2011;21:998---1002.
3.KofkeWA.Anestheticmanagementofthepatientwithepilepsy orpriorseizures.CurrOpinAnaesthesiol.2010;23:391---9. 4.PerksA,CheemaS,MohanrajR.Anaesthesiaandepilepsy.BrJ
Anaesth.2012;108:562---71.
5.TanL,YuJT,SunYP,etal.Theinfluenceofcytochromeoxidase CYP2A6,CYP2B6, and CYP2C9 polymorphismson theplasma concentrationsofvalproicacidinepilepticpatients.ClinNeurol Neurosurg.2010;112:320---3.
6.Wilfong AA. Monotherapyin childrenand infants.Neurology. 2007;69:S17---22.
7.Anderson GD. Pharmacogenetics and enzyme induc-tion/inhibition properties of antiepileptic drugs. Neurology. 2004;63:S3---8.
8.CohenM,SadhasivamS,VinksAA.Pharmacogeneticsin periop-erativemedicine.CurrOpinAnaesthesiol.2012;25:419---27. 9.AmericanSocietyofAnesthesiologistsTaskForceonSedation
andAnalgesiabyNon-Anesthesiologists.Practiceguidelinesfor sedationand analgesiabynon-anesthesiologists. Anesthesiol-ogy.2002;96:1004---17.
10.Cote CJ, Wilson S. Guidelines for monitoring and manage-ment of pediatric patients during and after sedation for diagnosticandtherapeuticprocedures:anupdate.Pediatrics. 2006;118:2587---602.
11.IsikB,ArslanM,TungaAD,etal.Dexmedetomidinedecreases emergence agitation in pediatric patients after sevoflurane anesthesiawithoutsurgery.PaediatrAnaesth.2006;16:748---53. 12.Weldon BC, Watcha MF, White PF. Oral midazolam in chil-dren: effectof timeand adjunctive therapy. Anesth Analg. 1992;75:51---5.
13.MalviyaS,Voepel-LewisT,TaitAR,etal.Depthofsedationin childrenundergoingcomputed tomography:validityand reli-abilityoftheUniversityofMichiganSedationScale(UMSS).Br JAnaesth.2002;88:241---5.
14.MachataAM,WillschkeH,KabonB,etal.Propofol-based seda-tionregimenfor infantsandchildrenundergoing ambulatory magneticresonanceimaging.BrJAnaesth.2008;101:239---43. 15.AldreteJA.Thepost-anesthesiarecoveryscorerevisited.JClin
Anesth.1995;7:89---91.
17.DemirG,CukurovaZ,ErenG,etal.Theeffectof‘‘multiphase sedation’’inthecourseofcomputedtomographyandmagnetic resonanceimagingonchildren,parentsandanesthesiologists. RevBrasAnestesiol.2012;62:511---9.
18.Matsunaga T, Maruyama M, Harada E, et al. Expression and inductionofCYP3Asinhumanfetalhepatocytes.Biochem Bio-physResCommun.2004;318:428---34.
19.Madan A, Graham RA, Carroll KM, et al. Effects of pro-totypical microsomal enzyme inducers on cytochrome P450 expressioninculturedhumanhepatocytes.DrugMetabDispos. 2003;31:421---31.
20.Perucca E. Clinical implications of hepatic microsomal enzyme induction by antiepileptic drugs. Pharmacol Ther. 1987;33:139---44.
21.PatsalosPN,PeruccaE.Clinicallyimportantdruginteractionsin epilepsy:generalfeaturesandinteractionsbetween antiepilep-ticdrugs.LancetNeurol.2003;2:347---56.
22.Anderson GD. A mechanistic approach to antiepileptic drug interactions.AnnPharmacother.1998;32:554---63.
23.Perucca E,Hedges A, Makki KA, et al. A comparativestudy oftherelative enzymeinducing propertiesofanticonvulsant drugs in epileptic patients. Br J Clin Pharmacol. 1984;18: 401---10.
24.KilbaughTJ,FriessSH,RaghupathiR,etal.Sedationand anal-gesiainchildrenwithdevelopmentaldisabilitiesandneurologic disorders.IntJPediatr.2010:189142.