REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
OfficialPublicationoftheBrazilianSocietyofAnesthesiologywww.sba.com.br
SCIENTIFIC
ARTICLE
Comparison
of
metaraminol,
phenylephrine
and
ephedrine
in
prophylaxis
and
treatment
of
hypotension
in
cesarean
section
under
spinal
anesthesia
Fábio
Farias
de
Aragão
a,b,∗,
Pedro
Wanderley
de
Aragão
b,
Carlos
Alberto
de
Souza
Martins
a,b,
Natalino
Salgado
Filho
b,
Elizabeth
de
Souza
Barcelos
Barroqueiro
baSociedadeBrasileiradeAnestesiologia,Brazil
bUniversidadeFederaldoMaranhão(UFMA),SãoLuís,MA,Brazil
Received28June2013;accepted25July2013 Availableonline2July2014
KEYWORDS
Anesthesia; Cesareansection; Spinalanesthesia; Hypotension; Vasoconstrictor agents
Abstract Maternalhypotensionisacommoncomplicationafterspinalanesthesiaforcesarean
section,withdeleteriouseffectsonthefetusandmother.Amongthestrategiesaimedat min-imizingtheeffectsofhypotension,vasopressoradministrationisthemostefficient.Theaim ofthisstudywas tocomparetheefficacy ofphenylephrine,metaraminol, andephedrine in the prevention andtreatment of hypotensionafter spinal anesthesia for cesarean section. Ninetypregnantwomen,notinlabor,undergoingcesareansectionwererandomizedintothree groupstoreceiveabolusfollowedbycontinuousinfusionofvasopressorasfollows: phenyle-phrinegroup(50g+50g/min);metaraminolgroup(0.25mg+0.25mg/min);ephedrinegroup (4mg+4mg/min).Infusiondosewasdoubledwhensystolicbloodpressuredecreasedto80%of baselineandaboluswasgivenwhensystolicbloodpressuredecreasedbelow80%.Theinfusion dosewasdividedinhalfwhensystolicbloodpressureincreasedto120%andwasstoppedwhen itbecamehigher.Theincidenceofhypotension,nauseaandvomiting,reactivehypertension, bradycardia,tachycardia,Apgarscores,andarterialcordbloodgaseswereassessedatthe1st and5thminutes.
Therewasnodifferenceintheincidenceofhypotension,bradycardia,reactivehypertension, infusiondiscontinuation,atropineadministrationorApgarscores.Rescueboluseswerehigher only intheephedrine groupcompared tometaraminol group.The incidenceofnausea and vomitingandfetalacidosisweregreaterintheephedrinegroup.Thethreedrugswereeffective inpreventinghypotension;however,fetaleffectsweremorefrequentintheephedrinegroup, althoughtransient.
© 2014SociedadeBrasileirade Anestesiologia.Publishedby ElsevierEditoraLtda.Allrights reserved.
∗Correspondingauthor.
E-mail:fabio.aragao30@gmail.com(F.F.deAragão). http://dx.doi.org/10.1016/j.bjane.2013.07.014
PALAVRAS-CHAVE
Anestesia; Cesariana; Raquianestesia; Hipotensão; Agentes
vasoconstritores
Avaliac¸ãocomparativaentremetaraminol,fenilefrinaeefedrinanaprofilaxiaeno tratamentodahipotensãoemcesarianassobraquianestesia
Resumo Hipotensão materna é uma complicac¸ão comum após raquianestesia em cirurgia
cesariana,trazendoefeitosdeletériosparaofetoeamãe.Entreasestratégiascomoobjetivo deminimizarosefeitosdahipotensão,aadministrac¸ãodevasopressoreséamaiseficiente. Oobjetivo deste estudo foi comparara eficáciada fenilefrina, metaraminol e efedrinana prevenc¸ão etratamento dehipotensão após raquianestesia em cirurgia cesariana.Noventa gestantesquenãoestavam emtrabalhodepartosubmetidas àcesarianaeletivaforam ran-domizadasemtrêsgruposparareceberumbolus,seguidodeinfusãocontínuadevasopressor daseguinteforma:GrupoFenilefrina(50g+50g/min);GrupoMetaraminol(0,25mg+0,25 mg/min);GrupoEfedrina(4mg+4mg/min).Adosedainfusãofoidobradaquandoapressão arterialsistólica(PAS)decresceuaté80%dosvaloresbasaiseumbolusfoidadoquandoaPAS decresceupara valoresabaixo de80%.A dosedainfusãofoidivididaaomeioquandoaPAS aumentouaté120%efoiinterrompidaquandomaiselevada.Foramanalisadasasincidências dehipotensão,náuseasevômitos,hipertensãoreativa,bradicardia,taquicardiaeescoresde Apgarnoprimeiroequintominutosegasesdesanguearterialdocordãoumbilical.
Não houve diferenc¸as nas incidências de hipotensão, bradicardia, hipertensão reativa, interrupc¸ãoda infusão,administrac¸ão deatropinaouescores deApgar.A administrac¸ãode
bolusderesgateforamsuperioresapenasnoGrupoEfedrinaemcomparac¸ãocomMetaraminol. A incidência de náuseas evômitos e acidosefetal foramsuperiores noGrupo Efedrina. Os trêsfármacosforameficazesnaprevenc¸ãodehipotensão,masrepercussõesfetaisforammais frequentesnoGrupoEfedrina,emboratransitórias.
©2014SociedadeBrasileiradeAnestesiologia.PublicadoporElsevierEditoraLtda.Todosos direitosreservados.
Introduction
Maternalhypotensionafter spinal anesthesiafor cesarean sectionsisacommoncomplicationandmayoccurinupto 80%ofcases.1 Ifnottreatedpromptly,it cancause
unde-siredeffectsonthemotherandfetus.2Theeffectsthatmost
commonlyaffectmothersarenauseaandvomiting,although moreseriouscomplicationssuchascirculatorycollapseand cardiacarrestmayoccuriftreatmentisnotpromptand effi-cient.Inthefetus,placentalhypoperfusionmaycausefetal distress, resultingin fetalacidosis, increasedbase excess andlowApgarvalues.3
Severalstrategieshavebeenusedtopreventorminimize hypotension, such as infusion of intravenous fluids, uter-inedisplacementtotheleftandelasticcompressionofthe lowerlimbs.However,thesemeasuresalonearegenerally noteffective.Theuseofvasopressorsisrequired.4
The optimal vasopressor should offset the progressive effectsof ascending sympatheticblockade, whichis diffi-culttoachievebecausethe␣-and-adrenergicactivities canvaryindependently duringblockade installation.Still, changesinsympatheticactivitymaybeorgan-specific (inhi-bition of cardiac fibers), region-specific(inhibition in the lower body and increased activity in the upper body) or systemic (inhibition of catecholamine release from the adrenal medulla). The most commonly used vasopressors (phenylephrine,metaraminol,andephedrine)have primar-ily systemic effects and may have undesirable effects on organs,vascularbedsorfetus.5
Ephedrine is a non-catecholamine sympathomimetic agent that stimulates the ␣- and -adrenergic receptors bydirectandindirectaction.Itbecamethevasopressorof
choicefortreatmentandprophylaxisofhypotensionaftera studywithsheepinthe70Ys,whichshowedminimalchanges
inuterinebloodflowafteradministration,whiledrugswith predominant␣-agonisteffectcausedasignificantreduction intheflow.6
However, the supremacy of ephedrine as a vasopres-sorof choiceincesarean sectionsbegantobequestioned afteritsassociationwithfetalacidosisandlowervaluesof baseexcesscomparedtovasopressorswithpredominant␣ -agonist effect. This fact is explicable because ephedrine crosses the uteroplacental barrier, acts directly on the fetus, andincreasesitsmetabolismthrough2-adrenergic receptors.7 The administrationof ephedrine for cesarean
sections,besidescausingfetalacidosis,alsobecame asso-ciatedwiththe highestincidenceof maternal nauseaand vomiting.8
The aim of this study was to compare the efficacy of phenylephrine, metaraminol and ephedrine for the prevention and treatment of maternal hypotension dur-ingcesareansection,evaluatevasopressortherapy-related adverseeffects,andstudyfetalchangesthroughApgarscore andumbilicalcordarterialandvenousbloodgases.
Methodology
andonedayand40weeksandsixdays,undergoingelective cesareandeliveryinaprivatematernityhospitalofSãoLuís (MA).
Sample
The primary outcome wasthe umbilical arterypH, which servedasthebasisforsample calculation.Withdatafrom previous studies, it was calculated that a sample of 26 pregnantwomen per groupwould have 90% powerwith a significancelevelof5%todetectadifferenceof0.05units intheumbilicalarterypHbetweengroups.However,inorder tominimizepossiblelosses,theinclusionwasscheduledfor 30pregnantwomenineachgroup.
Inclusion,non-inclusionandexclusioncriteria
Pregnant women between 39 weeks and one day and 40 weeksandsixdaysofgestationalage,undergoingelective cesarean delivery,physical statusASA I(American Society ofAnesthesiologists’classification),withasinglegestation and between 20 and 34 years old were included in the study,asthisagegroupisindifferenttomaternalandfetal complications.9
It is well documented that pregnant women over 35 years of age are more likely to have premature rup-tureofmembranes,placentapraevia,gestationaldiabetes and preeclampsia, in additionto a higherchance of hav-ingchronicdiseases, suchassystemichypertension10;and
pregnantwomenunder20yearsofagehaveahigherriskof fetaldeath.11
Non-inclusion criteria were pregnant women refusal, comorbidities, fetal abnormalities, contraindication for spinalanesthesiaandahistoryofhypersensitivitytodrugs usedinthestudy.
Exclusion criteria were volume of collected umbilical cordbloodinsufficienttodeterminebloodgasesand anes-theticblockfailure.
Treatmentgroups
Pregnantwomenwererandomlydividedintothreegroups: metaraminol(GroupM);phenylephrine(GroupP);ephedrine (GroupE).Themethodusedwasthedrawingofsequential sealedenvelopescontainingnumberspreviouslygenerated by computer. Bothpregnant women and anesthesiologists who participated in the surgeries were blinded to group allocation.
Preparationofvasopressors
Asecondanesthetist,whodidnotattendthesurgery, pre-paredthevasopressoragents.Thesolutionswereprepared inasyringeof20mLasfollows:
• GroupP:phenylephrine100g/mL; • GroupM:metaraminol0.5mg/mL; • GroupE:ephedrine8mg/mL.
Anesthetictechnique
Patientsweremonitoredwithcontinuous electrocardiogra-phy,noninvasive blood pressure and pulse oximetry, with InfinityDeltamonitor(DrägerwerkAG&Co.KGaA,2009).
Venipuncturewithan18GJelcowasperformedandthen patientswereplacedsupine,withuterinedisplacementto theleftforafewminutes.Then,bloodpressurewas mea-sured three times at 3-min intervals and the arithmetic average of the values was calculated, which was consid-eredthebasalpressureofpregnantwomenandrecordedon thedatacollectionform.Then,withthepatientinsitting position,spinalanesthesiawasperformedwith27Gneedle (Whitacre)betweenthethirdandfourthlumbarvertebrae. Patientsreceived10mgof0.5%hyperbaricbupivacaine com-binedwith100gofmorphine,atarateof1mLevery15s.12
Immediatelyaftertheblockade,concomitanthydration of Ringer’slactate(10mLkg---1)wasstarted.13
After blockade, the measurement of pregnant women systolic blood pressure (SBP) was recorded every minute ondata collectionformup to fetus extraction. The level ofsensoryblockwasassessedwiththepinpricktestevery minuteafterthepuncture,untilitreachedthedermatome level of the fifth thoracic nerve root (T5). The beginning ofsurgerywasthenauthorized.Thetimefromblockadeto skinincision,uterineincision,andextractionoffetuswere recorded.12
Protocolforadministrationofvasopressors
Immediatelyafterblockade,thepatientsreceivedabolus of 0.5mL of the solution, which corresponded to 50g of phenylephrine, 250g of metaraminol, and 4mg of ephedrine, followed by subsequent doses of continuous intravenousinfusionwithasyringepump(SamtronicSaúde Technologia,model670),programmedfor aninfusionrate of30mL/h,sothatallpatientsreceivedthedosespreviously established:
• GroupP:phenylephrine50g/min---1;14
• GroupM:Metaraminol250g/min---1;15
• GroupE:ephedrine4mgg/min---1.16
Althoughinfusion withfixedrates iseasier toperform, varyinginfusionrateswereusedaccordingtotheSBPvalues, inordertoenablegreatereffectivenessincontrollingblood pressure.17 Thus, therate of infusion of vasopressors was
adjustedaccordingtotheprotocolasshowninTable1.
Table1 Vasopressorinfusionrates.
SBPvalues(%) Approach
Above120% InfusiondiscontinuationuntilSBPreturn to<120%
100and120% Reductionofinfusionrateto15mL/h Around100% Maintenanceofinfusionrateat30mL/h 80and100% Increaseofinfusionrateto60mL/h Below80% Solutionbolusof1mL(rescuedose)and
Reactive hypertensionaftertheuseof vasopressorwas definedasSBP20%greaterthanthebaselinevalueand,ifit occurred,itwastreatedwithinfusiondiscontinuationuntil bloodpressurereachedvalueslowerthan120%ofbaseline, andtheinfusionwasrestarted.Whenpatienthadmorethan twoepisodesofreactivehypertension,infusionwas perma-nentlydiscontinued(whichwasrecorded),andsubsequent episodesofhypotensionweretreatedwithbolusinfusionof thesolution(1mL).Bradycardiawasconsideredwhenheart ratevalueswerelowerthan50beatsperminuteand,when accompaniedbyhypotension,itwastreatedwithatropine (0.5mg).Tachycardiawasconsideredataheartrategreater than100beatsperminute.12Valueslessthan100%of
base-lineSBPwereconsideredhypotension.
Evaluationofpregnantwoman
MaternalSBPwererecordedeveryminuteondatacollection form.Episodes of hypotension, hypertension, tachycardia and bradycardia, need for rescue doses of vasopressor, infusiondiscontinuation,andatropineadministrationuntil birthwererecorded.Episodesofnauseaandvomitingwere alsorecorded untilthe end of cesarean section and, ifit occurred,itwastreatedwith4mgintravenousondansetron.
Newbornevaluation
Arterialbloodsampleswerecollectedfromthefetal umbil-icalcordimmediatelyafterbirth,andduringtheclamp,the surgeon was requested to withdraw a fragment of about 10cm long for arterial puncture. At the operating room, analysisofblood gas,lactate,andglucosewasperformed using a portable gas analysis device (Epoc, Epocal Inc., Ottawa,Canada). An umbilical pH less than 7.2 was con-sideredfetalacidosis.18
Newborns were evaluated by an assistant pediatrician whoassessed theApgar score at the 1stand 5thminutes ofbirth,andalowApgar wasconsideredwhen thevalues assignedwerelessthan7.
Thenewborndestinationwasalsoevaluated,ifhewas takentotheneonatalintensivecare unit,ifhewasunder observationintheneonatalresuscitationroomortakento theapartment.
Statisticalanalysis
The results were statistically analyzed with the software BioEstat5.3.Numericalvariableswerecomparedamongthe threegroupsusingtheKruskal---Wallistest followedbythe Mann---Whitney test. Categorical variables were compared amongthethreegroupsusingthechi-squaretest followed byFisher’sexacttest.Resultswereconsideredstatistically significantwhenp<0.05.
Results
Amongthethreegroups,allpregnantwomenwereover20 andunder35yearsofage,gestationalagebetween39weeks andonedayand40weeksandsixdaysand,untilbirth,they receivedthesameamountoffluids.
Oneofthepregnantwomenwhoreceivedephedrinewas excludedduetoinsufficientvolumeofbloodcollectedfrom theumbilicalcord.
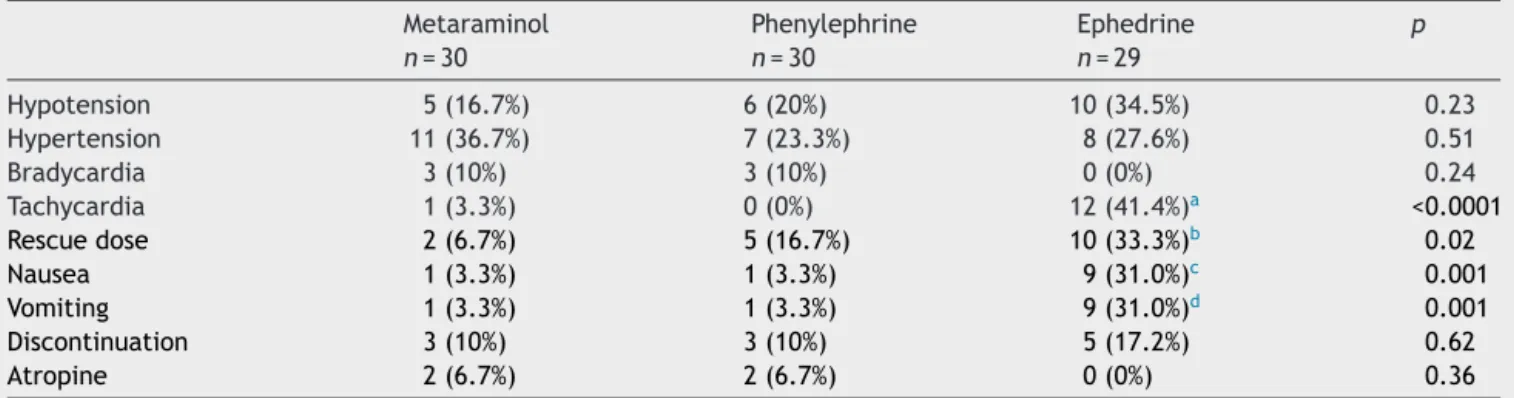
Pregnantwomenevaluationshowednosignificant differ-ence regarding theincidence of hypotensionin the three groups,aswellasincidenceofreactivehypertension,need forinfusiondiscontinuation,andbradycardia.Regarding res-cuedoseadministration,therewasnostatisticaldifference betweengroupsMandE,althoughhigherinGroupE,which wasnotobservedinGroupP.Theincidenceoftachycardia, nauseaandvomitingwashigherinGroupE(Table2).
Clinical evaluation of newborns showed no difference in Apgar scores at the 1st or 5th minute between groups (Table3).OnlyonenewborninGroupEhadApgarscoreless than seven at the 1stminute, associated withfetal acid-osis.However,heshowedclinical improvementandApgar score=9atthe5thminute.Noinfantreceivedresuscitation maneuversorrequiredcareintheintensivecareunit.
Table2 Hemodynamicchangesrelatedtomaternalsympatheticblockandsideeffectssecondarytovasopressortherapyin
pregnantwomenundergoingelectivecesareansectionunderspinalanesthesia. Metaraminol
n=30
Phenylephrine
n=30
Ephedrine
n=29
p
Hypotension 5(16.7%) 6(20%) 10(34.5%) 0.23 Hypertension 11(36.7%) 7(23.3%) 8(27.6%) 0.51 Bradycardia 3(10%) 3(10%) 0(0%) 0.24 Tachycardia 1(3.3%) 0(0%) 12(41.4%)a <0.0001
Rescuedose 2(6.7%) 5(16.7%) 10(33.3%)b 0.02
Nausea 1(3.3%) 1(3.3%) 9(31.0%)c 0.001
Vomiting 1(3.3%) 1(3.3%) 9(31.0%)d 0.001
Discontinuation 3(10%) 3(10%) 5(17.2%) 0.62
Atropine 2(6.7%) 2(6.7%) 0(0%) 0.36
Resultsareexpressedasfrequency(percentage)(chi-square,Fisher).
Table3 ClinicalevaluationofthenewbornthroughtheApgartestatthe1stand5thminutesafterbirthinelectivecesarean sectionsunderspinalanesthesia.
Apgar Metaraminol Phenylephrine Ephedrine p
1stminute 9(7---9) 9(8---9) 9(6---9) 0.7413 5thminute 10(9---10) 10(9---10) 10(9---10) 0.7542
Valuesareexpressedasmedianandinterquartilerange(Kruskal---Wallis).
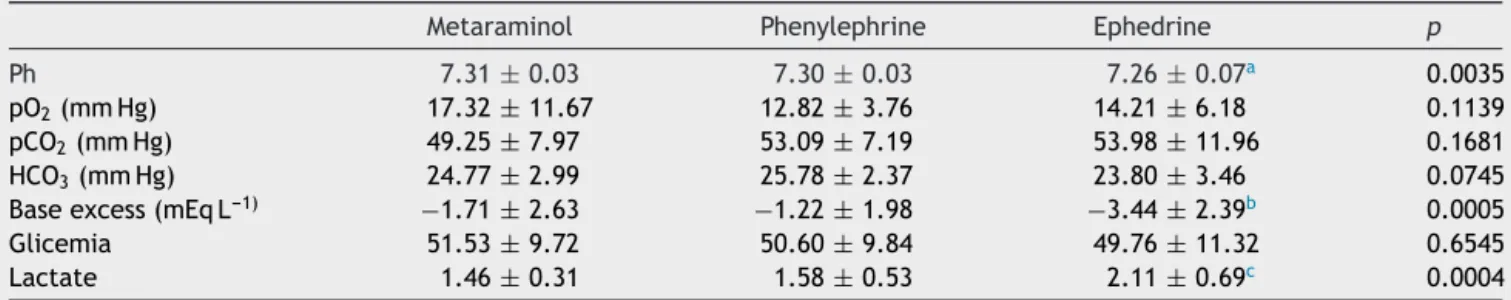
Regardinglaboratory evaluationofnewborns,the aver-age pH was7.31±0.03 in Group M, 7.30±0.03 in Group Pand7.26±0.07 in Group E.In groupE, threenewborns (10.3%) had pH less than 7.20. However, thep-value was significant(p=0.0035).
Considering the mean value of excess base, therewas a significant difference between groups M and P in rela-tiontoE,butnotbetweengroupsMandP.Lactatevalues alsoshowedsignificantdifferencebetweengroupsandwere higherinGroupEcomparedtogroupsMandP.Parameters suchaspO2,pCO2,HCO3,andglucoseshowednostatistical differences(Table4).
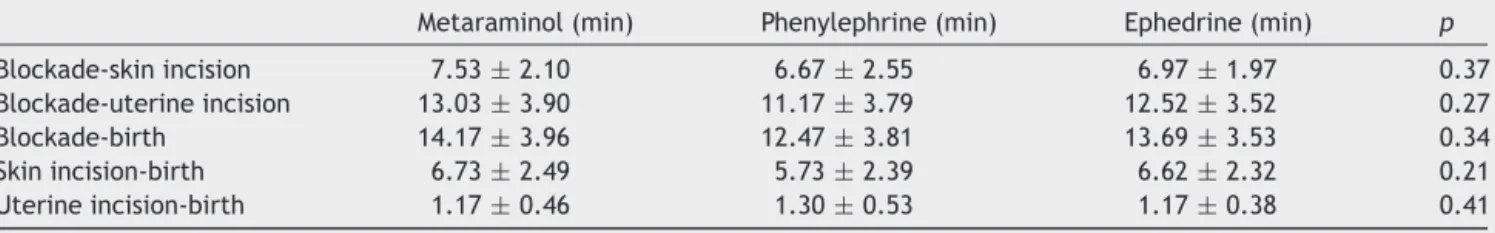
There was no statistical difference between groups regardingthetimeelapsedbetweenblockadeandskin inci-sion,blockadeanduterineincision,andblockadeandbirth (Table5).
Discussion
The vasopressor doses administered in this study were appropriateforthepreventionandtreatment ofmaternal hypotension. Currently, it is known that the three vaso-pressors are considered equally effective for preventing hypotensionduringelectivecesareansections.3,15,19
Whenphenylephrineisadministeredbycontinuous infu-sion,theincidenceofhypotensionvariesbetween13%and 23%.17 Allenetal.14 comparedfixedinfusionsof25,50,75
and100g/minofphenylephrineandreportedbetter hemo-dynamic stability when doses of 25 and 50g/min were used.The incidence of hypotensionin thisstudy was20% andsatisfactoryhemodynamiccontrolwasobtainedwiththe variableinfusionstartedwith50g/min.
In a study by NganKee etal.,15 in which metaraminol
wasadministeredasabolus of0.5mgfollowed by contin-uousinfusionof0.25mg/min,theincidenceofhypotension
was35%,which is higherthan that obtained inthis study (16.7%). Although the initial infusion doses in both stud-iesweresimilar,thedifferenceobservedprobablyoccurred becausethedosesadministeredinthisstudyvaried accord-ingtobloodpressuremeasurements,whichpromotesbetter hemodynamiccontrol.17
Regardingephedrine,thisstudyobservedhypotensionin 34.5%ofcases,whereasin thestudyby Carvalhoetal.,20
theincidence was45%. Note that both the work byNgan Keeetal.15 and Carvalhoetal. usedprior administration
ofcrystalloid,an approachprovenineffective. Becausein thisstudyfluidswereconcomitantlyadministeredwiththe blockade,thismayexplainthedifferenceinresults.
Ontheotherhand,Bhardwajetal.21inastudycomparing
thethreevasopressorsusedinthepresent study, adminis-teredbolus followed by continuous infusion and reported incidence of hypotension in Group M (14.8%) and Group P(12.5%), results closest tothis study. As for ephedrine, hypotensionoccurredin23%ofthecases.
Toavoiddistortionsintheresults,allpatientsreceiveda volumeof10mL/kgofRinger’ssolutionuntilchilddelivery, asconcomitant hydration (cohydration). Banerjee etal.22
consideredrationaltostarttherapidinfusionofcrystalloid, suchasRinger’ssolution,concurrentlywiththeanesthetic block,ascrystalloids improvesystolicvolumeandcardiac outputonlytransiently,anditisconsideredacheaperoption thancolloids,withlessrisk ofcomplications(anaphylaxis, coagulationdisorders).23
Incasesofreactivehypertensionandvasopressorinfusion discontinuation,theresultsmatchthoseoftheliterature,19
i.e.,therewerenosignificantdifferencesamongthethree groups.Regardingtheincidenceofbradycardia,althoughit wassimilarinthethreegroups,theresultsareoppositeto thestudies byVeeseretal.,which reportedlowerrisk of bradycardiainpregnantwomenreceivingephedrine.
Table4 Laboratoryevaluationofthenewbornperformedwithsamplecollectionofumbilicalcordarterialbloodfor
measure-mentofglucose,lactate,andbloodgasesduringelectivecesareansectionunderspinalanesthesia.
Metaraminol Phenylephrine Ephedrine p
Ph 7.31±0.03 7.30±0.03 7.26±0.07a 0.0035
pO2(mmHg) 17.32±11.67 12.82±3.76 14.21±6.18 0.1139
pCO2(mmHg) 49.25±7.97 53.09±7.19 53.98±11.96 0.1681
HCO3(mmHg) 24.77±2.99 25.78±2.37 23.80±3.46 0.0745
Baseexcess(mEqL---1) −1.71±2.63 −1.22±1.98 −3.44±2.39b 0.0005
Glicemia 51.53±9.72 50.60±9.84 49.76±11.32 0.6545
Lactate 1.46±0.31 1.58±0.53 2.11±0.69c 0.0004
Valuesareexpressedasmeanandstandarddeviation(Kruskal---Wallis,Mann---Whitney).
Table5 Intraoperativevariables.
Metaraminol(min) Phenylephrine(min) Ephedrine(min) p
Blockade-skinincision 7.53±2.10 6.67±2.55 6.97±1.97 0.37 Blockade-uterineincision 13.03±3.90 11.17±3.79 12.52±3.52 0.27 Blockade-birth 14.17±3.96 12.47±3.81 13.69±3.53 0.34 Skinincision-birth 6.73±2.49 5.73±2.39 6.62±2.32 0.21 Uterineincision-birth 1.17±0.46 1.30±0.53 1.17±0.38 0.41
Valuesareexpressedasmeanandstandarddeviation(Kruskal---Wallis).
An interesting observation was that pregnant women treated withmetaraminol hadless need for rescue doses than those who received ephedrine. The same was not observed with phenylephrine. This probably occurred becausemetaraminolincreasesthesystemicvascular resis-tance(afterload),recruits splanchnicblood,andincreases the venous return (preload), besides presenting positive inotropicactivity,unlikephenylephrine,whichactsbasically onlyintheafterload.24
The incidence of tachycardia was higher in Group E than in other groups, which was expectedbecause when ephedrine is used to prevent hypotension during surgery underspinalanesthesia,itcausesanincreaseofcardiac out-putat the expense ofincreased heart rate.On the other hand, it is known that ␣-agonist drugs, such as phenyle-phrineandmetaraminol, maycause reflexbradycardia to the increased peripheral vascular resistance.25 However,
therewerenodifferencesbetweengroupsintheincidence ofbradycardia,whichmaybeduetotheadministrationof adequatedosesofmetaraminolandphenylephrine.
In this study,despite effective blood pressurecontrol, therewasarelationshipbetweentheuseofephedrineand theincidenceofnauseaandvomiting.Leeetal.,2ina
sys-tematicreview onthe use of ephedrine,found that even underbloodpressurecontrolincesareansectionstherewere differencesbetween theephedrine groupand thecontrol group (without vasopressor) regarding the occurrence of nauseaandvomiting.
Ngan Keeet al.,26 in a study comparinginfusions with
varying combinations of ephedrine and phenylephrine for maintenanceofbloodpressureduringelectivecesarean sec-tion,foundthatthehighertheproportionofephedrineand the lower the proportion of phenylephrine, the hemody-namiccontrolwasmoredifficult,fetalacid-baseprofileless favorable,andincidenceofnauseaandvomitinghigher.
It is knownthat intraoperative nauseaandvomiting in cesarean sections may be prevented through hypotension controlandimprovingtheuseofneuraxialandintravenous opioids,whichimprovestheanestheticblockquality, mini-mizessurgicalstimulation,andreducestheuseofuterotonic drugs.Whereasallpregnantwomen inthisstudyreceived the same dose of opioids and uterotonic drugs, as well asadequate levels of anesthetic blockade, the increased incidence of nausea and vomiting caused by ephedrine is probably due to an effect of the drug itself, besides indicating that the etiology of nausea and vomiting is multifactorial.27
Some studies have reported a lower incidenceof nau-sea,vomiting,andmaternalhypotensionwhenvasopressors areadministeredbycontinuousinfusion.Therefore,inthis
study,the administration of bolus followed by continuous infusionwaschosen.6,17,28However,itisknownthat
continu-ousinfusionofvasopressorsisassociatedwithhigherdosesin ordertomaintainbloodpressureclosetobaselinevalues.29
Thevasopressorofchoicewithbetterprofilefor hemo-dynamic control of pregnant women in cesarean sections is still largely debatable, by the observation that during theanestheticblockinstallationthereisareductionin sys-temicvascularresistance,associatedwithincreasedcardiac output, which is mediatedby increasedheart rate. Thus, bradycardia caused by the administration of ␣-agonists resultsindecreasedmaternalcardiacoutput,leadingsome anesthesiologiststobasetheirchoiceonthemother’sheart rate.30
Dyeretal.,inastudyevaluatingpregnantwomen under-going cesarean section under spinal anesthesia through minimally invasive cardiac output monitors (LiDDCO and BioZ) who received ephedrine or phenylephrine, showed that, after spinal anesthesia, the pregnant women had a marked decrease in systemic vascular resistance, with a compensatory increase in cardiac output, and concluded that low doses of phenylephrine are able to restore the systemicvascularresistanceandcardiacoutputtobaseline values.31
Auleretal.32 whoalsoassessedmaternal hemodynamic
changesthroughminimallyinvasivemonitoringofpregnant womenundergoingcesareansection underspinal anesthe-siaandwhoreceivedmetaraminoltocontrolbloodpressure, reportedadecreaseinsystolicvolume,offsetbyincreased heartrate,butdidnotobservesignificantchangesinmean arterialpressureandsystemicvascularresistance,and spec-ulatedthat these results occurred becauseof more rapid and effective correctionof mean arterial pressureby the administrationofmetaraminol.
Althoughthehemodynamiccontrolwassatisfactorywith thethreevasopressors, alimitationof thestudy wasthat the doses administered were extracted from other stud-ies without equipotent ratio, as there are no studies in literaturecomparingequipotentdosesofvasopressors stud-ied.Still, measurement of maternal pressurewasusedat intervalsofoneminute,whichbesidesbeinguncomfortable for the mother may hinderblood pressure measurement, as sometimes it takes more than a minute to measure blood pressure. Cooperet al.33 in a study evaluating the
Regardingfetalprognosis,althoughthechosen vasopres-sordosesweresuitableformaternalhypotensioncontrolin the threegroups, the newborns of motherswho received ephedrineshowedpHvaluesandbaseexcesslowerthanthe othergroups.
Fetal acidosis, assessed through umbilical cord blood pH and base excess, is considered a marker of neona-tal prognosis. Although some studies report that only severely acidotic fetuses (pH<7), after an acute intra-partumevent,haveahigherriskofmortalityandmorbidity (hypoxic-ischemic encephalopathy, intraventricular hem-orrhage, cerebral palsy), a recent meta-analysis showed that when acidosis was defined as pH<7.20, a four- and two-fold increase occurred in mortality and morbidity, respectively.34
According to Magalhães et al.18 who used the value
of 7.20tocharacterize fetalacidosis inelective cesarean sections,inwhichpatientsreceivedephedrineor phenyle-phrine,therewerenocasesoffetalacidosis.Inthiswork, fetalacidosiswasobservedinonlythreenewbornsofGroup E;however,p-valuewasnotsignificant.Despitethe occur-renceoffetalacidosisinthethreecasesmentionedabove, therewerenoclinicalconsequencesinanyofthem,asall newbornhadApgarscores>8atthe5thminuteanddidnot requireresuscitationmaneuversortransfertotheintensive careunit.
Baseexcesscomparisonshowednodifferencesbetween theMandPgroupscomparedtoGroupE.Thevalueswere lowerinthelatter.However,despitethedifferences,these valuesarewithinnormallimits.35
From fetal standpoint, no doubt that phenylephrine and metaraminolare associated withhigher valuesof pH and base excessin umbilical cordblood that were higher thanthoseofephedrine,2,15,36whichwereconfirmedinthe
present study,reason for which the use of ephedrine for hypotension management in obstetric anesthesiais being questionedasafirst-choicevasopressor.Thus,onecan pre-dict that the administration of high doses of ephedrine, especially in situations of fetal compromise, should be avoided.15,37
Fetalchangescausedbyephedrinearerelatedtothefact thatitrapidlycrossestheuteroplacentalbarrier,stimulates fetal-adrenergicreceptors,andincreasesfetalmetabolic demand.This canbeseenby theincreasein lactate, glu-cose, and catecholamines in umbilical cord blood. In the presentstudy,whenthemotherreceivedphenylephrine,the lactatevaluesinumbilicalcordbloodwerehigherthanwhen themotherreceivedephedrineandmetaraminol.However, regardingglycemia,therewerenodifferencesbetweenthe threegroups,incontrasttotheresultsofNganKeeetal.38
Fetal metabolic response to vasopressor administered in the mother may depend on the fetal2-adrenoceptor genotype and further complicate the understanding of the relationship between ephedrine administration and lower pH values. Fetal homozygosity for the ADRB2 gene p.Arg16 seemstobemore resistanttoephedrine-induced acidemia.39
On theotherhand,arecentstudybyBhardwajetal.21
showed no differences between the M, E, and P groups regardingpH ofumbilical cordbloodandbase excess val-ues. This difference probablyoccurred due tothe use of smallerdosesofephedrine.
None of the infants in this study had low Apgar score (lessthan 7)at the5thminute. Itis knownthat episodes ofhypotensionduringelectivecesareansectionsarenota cause of clinically significant fetal changes when treated promptly.In asystematicreviewbyVeeseretal.19,which
included20 studieswitha totalof 1069newborns, it was demonstratedthatonly onenewbornhadApgarscoreless than7inthe5thminute.
In order to minimize the occurrence of fetal acidosis, inadditiontotheapproachesalreadydescribedhere,itis knownthatthetimeelapsedbetweentheskinincisionand birth, and between uterine incision and birth, is directly relatedtofetalacidosis.This hasencouragedsurgeons to reducethedurationofsurgeries.40
Inthisstudy,thedurationofsurgeryinallstudygroups waslowerthanthatreportedintheliterature,whichmay beareasonable explanationfor thefavorableoutcome of newborns, evenin caseswhere fetal acidosisoccurred. A study by Maayan-Metzgeret al. showed that infants born towomenwhohad aninterval ofmore thantwominutes between uterotomia and birth had a higher incidence of feedingproblemsandprolongedhospitalization.41
Currently,vasopressorswithpredominantlyalpha-agonist effects are considered drugs of choice for preventing maternal hypotension, nausea and vomiting during spinal anesthesiaforelective cesareansections.Although itsuse isassociatedwithreducedheartrateandcardiacoutput,it isclinicallyinsignificantinlow-riskpregnanciesandelective cesareansections.
Ourresultsshowthatinelectivecesareansectionsunder spinal anesthesiahypotension can be controlled withany ofthevasopressorsstudied,astherewerenoclinically sig-nificantmaternalorfetalchanges,whichshows thatstrict control of blood pressure is an important condition for maternalandfetalwell-being. However,metaraminoland phenylephrinehadadvantagesoverephedrine,especiallyin theincidenceofnauseaandvomiting.Repercussionsof vaso-pressortherapyinemergencycesareansectionsandhighrisk pregnanciesarestillamatterofmuchdiscussion.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.Macarthur A, Riley ET. Obstetric anesthesia controversies: vasopressorchoiceforpostspinalhypotensionduringcesarean delivery.IntAnesthesiolClin.2007;45:115---32.
2.LeeA,NganKeeWD,GinT.Aquantitative,systematicreviewof randomizedcontrolledtrialsofephedrineversusphenylephrine forthemanagementofhypotensionduringspinalanesthesiafor cesareandelivery.AnesthAnalg.2002;94:920---6.
3.Cyna AM,Andrew M, Emmett RS,et al. Techniques for pre-venting hypotension during spinal anaesthesia for caesarean section; 2010 (Review). Available from: http://onlinelibrary. wiley.com/o/cochrane/clsysrev/articles/CD002251/pdffs.html [accessed7.11.10].
5.CooperDW.Cesareandeliveryvasopressormanagement.Curr OpinAnesthesiol.2012;25:300---8.
6.RalstonDH,ShniderSM,DelorimierAA.Effectsofequipotent ephedrine, metaraminol,mephentermine, and methoxamine on uterine blood flow in the pregnant ewe. Anesthesiology. 1974;40:354---70.
7.ClyburnP.Spinalanaesthesiaforcaesareansection:timefor re-appraisal?Anaesthesia.2005;60:633---5.
8.CooperDW,CarpenterM,MowbrayP,etal.Fetalandmaternal effectsofphenylephrineandephedrineduringspinalanesthesia formcesareandelivery.Anesthesiology.2002;97:1589---90. 9.MontanS. Increasedriskintheelderlyparturient.Curr Opin
ObstetGynecol.2007;19:110---2.
10.EzraY,McParlandP,FarineD.Highdeliveryinterventionrates innulliparouswomenoverage35.EurJObstetGynecolReprod Biol.1995;62:203---7.
11.Vienne CM,Creveuil C,DreyfusM.Does young maternalage increasetheriskofadverseobstetric,fetalandneonatal out-comes: a cohort study. Eur J Obstet Gynecol Reprod Biol. 2009;147:151---6.
12.Neves JFNP, Monteiro GA, Almeida JR, et al. Utilizac¸ão da fenilefrinaparacontroledapressãoarterialemcesarianas ele-tivas:doseterapêuticaversusprofilática.RevBrasAnestesiol. 2010;60:391---8.
13.Cardoso MSC, Santos MM, Yamaguchi ET, et al. Expansão volêmicaem raquianestesia para cesariana:comorealizá-la? RevBrasAnestesiol.2004;54:13---9.
14.Allen TK, George RB, White WD, et al. A double-blind, placebo-controlledtrialoffourfixedrateinfusionregimensof phenylephrineforhemodynamicsupportduringspinal anesthe-siaforcesareandelivery.AnesthAnalg.2010;111:1221---9. 15.Ngan KeeWD,LauTK,KhawKS.Comparisonofmetaraminol
andephedrineinfusionsformaintainingarterialpressureduring spinalanesthesiaforelectivecesareansection.Anesthesiology. 2001;95:307---13.
16.SaravananS,KocarevM,WilsonRC,etal.Equivalentdoseof ephedrineandphenylephrineinthepreventionofpost-spinal hypotensionincaesareansection.BrJAnaesth.2006;96:95---9. 17.HabbibAS.Areviewoftheimpactofphenylephrine adminis-trationonmaternalhemodynamicsandmaternalandneonatal outcomesinwomenundergoingcesareandeliveryunderspinal anesthesia.AnesthAnalg.2012;114:337---90.
18.MagalhãesE, GovêiaCS, LadeiraLCA,et al. Efedrinaversus fenilefrina:prevenc¸ãodehipotensãoarterialdurante aneste-siaraquídea paracesarianaeefeitossobre o feto.Rev Bras Anestesiol.2009;59:11---20.
19.VeeserM,HofmannT,RothR,etal.Vasopressorsforthe man-agement of hypotension after spinal anesthesia for elective caesarean section. Systematic review and cumulative meta-analysis.ActaAnaesthesiolScand.2012;56:810---6.
20.Carvalho JCA, Cardoso MMSC, Capelli EL, et al. Efedrina profiláticaduranteraquianestesiaparacesariana:estudo dose-respostadaadministrac¸ãoembóluseeminfusãocontínua.Rev BrasAnestesiol.1999;49:309---14.
21.Bhardwaj N, Kajal J, Arora S, et al. A comparison ofthree vasopressor for tight control of maternal blood pressure during cesarean section under spinal anesthesia: effect on maternal and fetal outcome. JAnaesthesiol ClinPharmacol. 2013;29:26---31.
22.Banerjee MD, StoccheRM, AngleP, et al.Preload or coload for spinalanesthesia for electivecesareandelivery: a meta-analysis.CanJAnaesth.2010;57:24---31.
23.Mercier FJ. Cesarean delivery fluid management. Curr Opin Anesthesiol.2012;25:286---91.
24.SiaulysM,YamagushiET.Anestesiaparacesariana.In:SiaulysM, editor.Condutasemanestesiaobstétrica.1sted.RiodeJaneiro: Elsevier;2012.p.41---74.
25.CritchleyLA, StuartJC,Conway F,et al.Hypotensionduring subarachnoidanaesthesia:haemodynamiceffectsofephedrine. BrJAnaesth.1995;74:373---8.
26.NganKeeWD,LeeA, KhawKS,et al.Arandomized double-blindedcomparison ofphenylephrine and ephedrine infusion combinationstomaintainbloodpressureduringspinal anesthe-siaforcesareandelivery:theeffectsonfetalacid-basestatus andhemodynamiccontrol.AnesthAnalg.2008;107:1295---302. 27.BalkiM,CarvalhoJCA.Intraoperativenauseaandvomiting
dur-ingcesareansectionunderregional anaesthesia.IntJObstet Anaesthe.2005;14:230---41.
28.Sia ATH, Tan HS, Sng BL. Closed-loop double-vasopressor automatedsystem to treathypotension duringspinal anaes-thesiaforcaesareansection:apreliminarystudy.Anaesthesia. 2012;67:1348---55.
29.DohertyA, OhashiY,DowneyK,etal.Phenylephrineinfusion versus bolus regimens during cesareandelivery under spinal anesthesia:adouble-blindrandomizedclinicaltrialto assess hemodynamicchanges.AnesthAnalg.2012;115:1343---50. 30.GuptaS.Vasopressorsandtightcontrolofmaternalblood
pres-sureduringcesareandelivery:arockyalliance.JAnaesthesiol ClinPharmacol.2013;29:1---3.
31.Dyer RA, Reed AR, Van Dyk D, et al. Hemodynamic effects of ephedrine, phenylephrine, and the coadministra-tionof phenylephrine withoxytocinduring spinalanesthesia for elective cesarean delivery. Anesthesiology. 2009;111: 753---65.
32.Auler Júnior JOC, Torres MLA, Cardoso MM, et al. Clini-calevaluationoftheflotrac/vigileoTMsystemforcontinuous cardiacoutputmonitoringinpatientsundergoingregional anes-thesia for elective cesarean section: a pilot study. Clinics. 2010;65:793---8.
33.CooperDW,SchofieldL,HyndR,etal.Prospectiveevaluationof systolicarterialpressurecontrolwithaphenylephrineinfusion regimenduringspinalanaesthesiaforcaesareansection.IntJ ObstetAnaesth.2012;21:245---52.
34.MalinGL,MorrisRK,KhanKS.Strengthofassociationbetween umbilicalcordpHandperinatalandlongtermoutcomes: sys-tematicreviewandmeta-analysis.BMJ.2010;340:c1471. 35.Reynolds F, Seed T. Anaesthesia for caesarean section and
neonatal acid---base status: a meta-analysis. Anaesthesia. 2005;60:636---53.
36.LinF,QiuM,DingX,etal.Ephedrineversusphenylephrinefor themanagement ofhypotension duringspinalanesthesia for cesareansection:anupdatedmeta-analysis.CNSNeurosciTher. 2012;18:591---7.
37.DyerRA,BiccardBM.Ephedrineforspinalhypotensionduring electivecaesarean section:thefinal nail inthe coffin?Acta AnaesthesiolScand.2012;56:807---9.
38.NganKeeDW,KhawKS,TanPE, etal.Placentaltransferand fetal metaboliceffects ofphenylephrine and ephedrine dur-ing spinal anesthesia for cesarean delivery. Anesthesiology. 2009;111:506---12.
39.Landau R, Liu S, Blouin J, et al. The effect of maternal and fetal 2-adrenoceptor and nitric oxide synthase geno-typeon vasopressor requirement and fetal acid---base status duringspinalanesthesia for cesareandelivery. AnesthAnalg. 2011;112:1432---40.
40.Ngan Kee DW, Lee A. Multivariate analysis of factors asso-ciated with umbilical arterial pH and standard base excess aftercaesareansectionunderspinalanaesthesia.Anaesthesia. 2003;58:125---30.