www.jped.com.br
ORIGINAL
ARTICLE
Accuracy
of
chest
radiography
for
positioning
of
the
umbilical
venous
catheter
夽
,
夽夽
,
夽夽夽
Adriana
F.M.
Guimarães
a,b,∗,
Aline
A.C.G.
de
Souza
b,
Maria
Cândida
F.
Bouzada
c,
Zilda
M.A.
Meira
a,caUniversidadeFederaldeMinasGerais(UFMG),HospitaldasClínicas,BeloHorizonte,MG,Brazil bFundac¸ãoHospitalardoEstadodeMinasGerais(FHEMIG),SantaEfigênia,MG,Brazil
cUniversidadeFederaldeMinasGerais(UFMG),DepartamentodePediatria,BeloHorizonte,MG,Brazil
Received24March2016;accepted18May2016 Availableonline15July2016
KEYWORDS
Newborn; Umbilicalveins; Centralvenous catheter;
Chestradiography; Echocardiography
Abstract
Objectives: To evaluate the accuracy of the simultaneous analysis of three radiographic anatomicallandmarks---diaphragm,cardiacsilhouette,andvertebralbodies---indetermining thepositionoftheumbilicalvenouscatheterdistalendusingechocardiographyasareference standard.
Methods: Thiswas a cross-sectional, observationalstudy,with the prospective inclusionof datafromallneonatesborninapublicreferencehospital,betweenApril2012andSeptember 2013,submittedtoumbilicalvenouscatheterinsertionaspartoftheirmedicalcare.The posi-tionofthecatheterdistalend,determinedbythesimultaneousanalysisofthreeradiographic anatomicallandmarks,wascomparedwiththeanatomicalpositionobtainedby echocardiogra-phy;sensitivity,specificity,positivepredictivevalue,negativepredictivevalue,andaccuracy werecalculated.
Results: Ofthe162newbornsassessedbyechocardiography,only44(27.16%)hadthecatheter inoptimalposition,inthethoracicportionoftheinferiorvenacavaoratthejunctionofthe inferiorvenacavawiththerightatrium. Thecatheterswerelocatedintheleft atriumand interatrialseptumin54(33.33%)newborns,intherightatriumin26(16.05%),intra-hepatic in37(22.84%),andintra-aorticin-onenewborn(0.62%).Thesensitivity,specificityand accu-racyoftheradiographytodetectthecatheterinthetargetareawere56%,71%,and67.28%, respectively.
夽
Pleasecitethisarticleas:GuimarãesAF,SouzaAA,BouzadaMC,MeiraZM.Accuracyofchestradiographyforpositioningoftheumbilical venouscatheter.JPediatr(RioJ).2017;93:172---8.
夽夽
StudyconductedatthePostgraduatePrograminHealthSciences,ChildandAdolescentHealthArea,FaculdadedeMedicina, Universi-dadeFederaldeMinasGerais(UFMG),BeloHorizonte,MG,Brazil.
夽夽夽
PartofAdrianaFurlettiMachadoGuimarães’Master’sDegreeDissertation.
∗Correspondingauthor.
E-mail:adriana.furletti@hotmail.com(A.F.Guimarães).
http://dx.doi.org/10.1016/j.jped.2016.05.004
0021-7557/©2016SociedadeBrasileiradePediatria.PublishedbyElsevierEditoraLtda.ThisisanopenaccessarticleundertheCCBY-NC-ND
Conclusion: Anteroposterior radiography ofthechest alone isnotable to safely definethe umbilicalvenouscatheterposition.Echocardiographyallowsdirectvisualizationofthecatheter tipinrelationtovascularstructuresand,wheneverpossible,shouldbeconsideredtoidentify thelocationoftheumbilicalvenouscatheter.
©2016SociedadeBrasileiradePediatria.PublishedbyElsevierEditoraLtda.Thisisanopen accessarticleundertheCCBY-NC-NDlicense(http://creativecommons.org/licenses/by-nc-nd/
4.0/).
PALAVRAS-CHAVE
Recém-nascido; Veiasumbilicais; Cateterismovenoso central;
Radiografiatorácica; Ecocardiografia
Acuráciadaradiografiadetóraxparaoposicionamentodocatetervenosoumbilical
Resumo
Objetivos: Avaliaraacuráciadaanálisesimultâneadostrêsmarcosanatômicosradiográficos ---diafragma,silhuetacardíacaecorposvertebrais,nadeterminac¸ãodaposic¸ãodaextremidade distaldocatetervenosoumbilical,utilizandoecocardiografiacomopadrãodereferência.
Métodos: Estudotransversal,observacional,cominclusãoprospectiva dedadosdetodosos neonatosnascidosemumamaternidadepúblicadereferência,entreabrilde2012esetembro de2013,submetidosàinserc¸ãodecatetervenosoumbilicalcomopartedoatendimentoclínico. Aposic¸ãodaextremidadedistaldocateter,determinadapelaanálisesimultâneadostrêsmarcos anatômicosradiográficos,foicomparadacomaposic¸ãoanatômicaobtidapelaecocardiografiae sensibilidade,especificidade,valorpreditivopositivo,valorpreditivonegativoeacuráciaforam calculados.
Resultados: Dos 162 recém-nascidos avaliados por ecocardiografia, somente 44 (27,16%) estavamcomocateteremposic¸ãoótima,naporc¸ãotorácicadaveiacavainferiorounajunc¸ão da veiacava inferiorcomoátriodireito.Oscateteres foramlocalizadosnoátrio esquerdo e septo interatrial em 54 (33,33%), no átrio direito em 26 (16,05%),intra-hepático em 37 (22,84%)enaaortaemumrecém-nascido(0,62%).Asensibilidade,especificidadeeacurácia daradiografiaparadetectarcateternazonaalvofoide56%,71%e67,28%,respectivamente.
Conclusão: Aradiografiaanteroposteriordetóraxisoladanãoécapazdedefinircomseguranc¸a aposic¸ãodocatetervenosoumbilical.Aecocardiografiapermiteavisibilizac¸ãodiretadaponta docateteremrelac¸ãoàsestruturasvascularese,semprequepossível,deveserconsiderada paralocalizac¸ãodocatetervenosoumbilical.
©2016SociedadeBrasileiradePediatria.PublicadoporElsevierEditoraLtda.Este ´eumartigo OpenAccesssobumalicenc¸aCCBY-NC-ND(http://creativecommons.org/licenses/by-nc-nd/4.
0/).
Introduction
Thecareofincreasinglyyoungerprematureinfantsisa con-stantchallengefortheclinicalteam.Aneffectivevascular accessthat is assafeaspossible is of utmostimportance when caring for these children. The use of the umbili-cal vein, first reported in 1947 by Diamond,1 constitutes a fast and easy option to obtain access to the systemic circulation.2---6
There are several complications resulting from the use of the umbilical venous catheter (UVC), including cardiac arrhythmia, infection, intracardiac and portal venous system thrombosis, embolism, myocardial per-foration, pericardial and pleural effusion, pulmonary infarction and hemorrhage, hepatic erosion and necrosis, and portal hypertension.2,5,7---10 The incidence of reported complications ranges from 20% to 35%, especially if the catheterispoorlypositioned,9asitisessentialtoensurethe correctpositioningofthecatheterinthethoracicportionof theinferiorvenacava(IVC)oratthejunctionoftheIVCwith therightatrium(RA).2,5,7,11---13
The catheter position is routinely assessed by antero-posterior chest radiograph, using the cardiac silhouette,
the diaphragm, and the vertebral bodies as anatomi-cal landmarks.2,4,7,9,11---14 The catheter should be at the diaphragmlevelorslightlyabove,4orbetweenthevertebral bodiesT8andT9,12 or atthecavoatrialjunctionobtained byextrapolatingthe curveof theRA medialborderup to itsintersectionwiththeIVCorwiththerightborderofthe vertebralbodies.9 However, various studies usingimaging methodssuchasultrasoundandechocardiographyto eval-uatetheUVCpositionhavedemonstratedthelowaccuracy ofradiographicanatomicallandmarks.2,4,7,9,12,14
Ithasbeenobserved,whenperformingechocardiograms andespeciallyinprematureinfantsasignificantnumberof cathetersplacedintheleftatrium(LA),eventhough they wereconsidered tobe in the ideal positionat the radio-graphicanalysis. Catheterspoorly positionedinthe LA,is associatedwiththrombusformation.7
weightand gestationalagewithcatheterpositioning.The echocardiographic imagewasconsidered asthereference standard,asinpreviousstudies.2,7,14
Methods
This was a cross-sectional, observational study, with the prospectiveinclusionof datafromallnewborns submitted to UVC insertion, regardless of birth weight and gesta-tionalage, born in a publicreference hospitalfrom April 2012 to September 2013. Newborns with malformations that altered the heart and/or liver position, critically-ill neonates and withno other indication for echocardiogra-phy,and thosewith a chest radiography to be compared with echocardiography with a time interval greater than 36hwereexcludedfromthestudy.Thesampleconsistedof newbornswhomettheeligibilitycriteriaduringthestudy period.
ThestudyprotocolwasapprovedbytheResearchEthics Committee of Fundac¸ão Hospitalar do Estado de Minas Gerais,opinionNo.597196-0,CAAE08220212.7.3001.5119, andsubsequentlyapprovedbytheResearchEthics Commit-teeof UniversidadeFederal deMinas Gerais, opinion No. 205460,CAAE08220212.7.0000.5149toobtaintheMaster’s DegreeinHealthSciences.Informed consentwasobtained fromtheparentsorlegalguardiansofallparticipants.
The variables of interest, namely birth weight, gesta-tionalage,gestationalageclassificationinrelationtobirth weight,clinicaldiagnosis,andcatheterrepositioningafter chestradiographanalysiswerecollectedfromthehospital medicalrecords.
The umbilical catheters were inserted by the medical teamaccordingtostandardtechniques forcatheter inser-tion,usingknownbodyreferencestoestimatethelength, such as the shoulder-umbilicus length graph and regres-sionequationbasedonbirthweight.2Afterinsertion,chest radiographyintheanteroposteriorviewwasrequestedand based on the interpretation made by the neonatologist, theUVCwaspulledback,whennecessary.Repeated radio-graphic images were obtained every time the catheter positionwaschanged.
AftertheUVCpositionwasconsideredappropriatebythe neonatologist, a two-dimensionalechocardiographic study wasperformedby oneof theresearchers,without knowl-edgeof the radiographic assessment of thecatheter. The tests were performed using a portable ultrasound device (LogicE,GeneralElectricHealthcare®,USA)equippedwith
a microconvex transducer of 4---10MHz and the images wereobtained in the subcostal, apical four-chamber,and parasternallong- andshort-axis views. Asmall volumeof salinesolution(0.5mL)wasinjected throughthecatheter ascontrastmedium,todeterminetheexactpositionofthe tip.Thepositionofthetipwasconsideredadequateifitwas identifiedinthetarget area---thoracic portionofthe IVC orIVC/RAjunction---andtheUVCwaspulledunderdirect visualization, when echocardiographic assessment showed anintracardiacpositioning.
All chest radiographies were analyzed by a radiologist of theinstitution, whowas unaware of theevaluation by thepediatrician andalsothelocationofUVCbythe echo-cardiography.Thechestradiographiesselectedforanalysis
werethoseperformedat thenearesttemporalrelationto theechocardiographicstudy.
Catheterpositionwassimultaneouslyestimatedby ana-lyzingthetipprojectionin relationtothediaphragm, the vertebralbodies,andtheheartsilhouette.
The collected data analysis was performed using the program Epi Info 7.1.1.3. (Epi Info, CDC, USA). Initially, a descriptiveanalysis ofdatawasperformed byanalyzing measuresofcentraltendencyanddispersionofcontinuous variables.
A comparative analysis of continuous variables, mean gestationalage, andmeanbirth weightwiththe needfor UVCrepositioningwasperformedusinganalysisofvariance (ANOVA),accordingtoBartlett’stest.
ThepositionofthedistalendoftheUVC,determinedby simultaneousanalysisofthreeradiographicanatomical land-marksperformed bythe radiologist,wascomparedtothe anatomicalpositionobtainedbyechocardiography.Basedon thesedata,sensitivity,specificity,positivepredictivevalue (PPV), negative predictive value (NPV), and radiographic examinationaccuracywerecalculated.
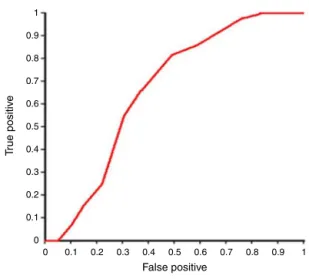
Areceiveroperatingcharacteristic(ROC)curvewas con-structedtoevaluatetheperformanceofthevertebrallevel methodinpredictingtheUVCposition.Theareaunderthe ROCcurvewithaconfidenceintervalwasalsodetermined, usingtheclassificationproposedbyHosmerandLemeshow (2000), in which an area between 0.7 and0.8 represents anacceptablediscriminatorycapacity,between0.8and0.9 an excellentdiscrimination,andabove0.9an exceptional discrimination.
Thestatisticalsignificancelevelwassetatp<0.05,with aconfidenceinterval(CI)of95%.
Results
One hundred and sixty-eight venous umbilical catheters were assessedin 167 newborns. Six evaluationswere lost due topoorqualityof the radiographicexamination, pre-venting adequate analysis. A total of 162 infants were evaluated, with gestational ages ranging from 23 to 41 weeks (32.19±4.23) and birth weight of 405 to 4630g (1809.05±897.46). Most had adequate weight for gesta-tionalage (86.42%).The most commonclinical diagnoses, which determined their admission to the neonatal inten-sive care unit,were prematurity (75.93%)and respiratory distresssyndrome(12.96%).
The catheters were positioned correctly in the target areainonly 44(27.16%)newborns, asdocumentedby the echocardiography.Theywerelocatedintheleftatriumand interatrial septum in 54 (33.33%) cases, in the RA in 26 (16.05%)cases,intra-hepaticin37(22.84%)cases,and intra-aorticinonenewborn(0.62%).
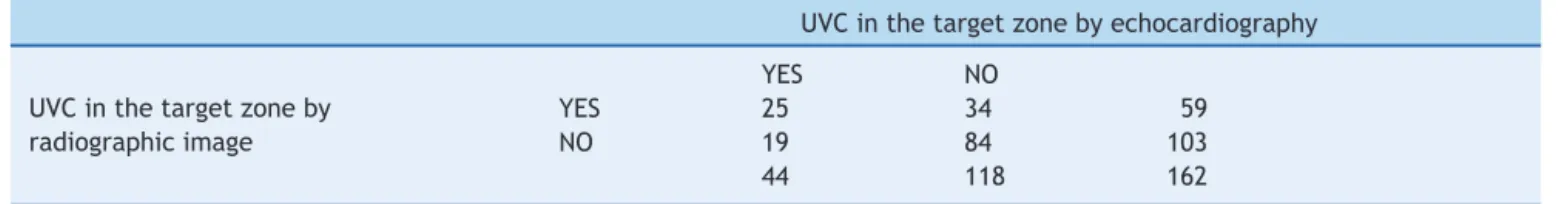
Table1 AssessmentoftheanteroposteriorchestX-raycapacityindetectingawell-positionedumbilicalvenouscatheterwhen comparedwithechocardiography.
UVCinthetargetzonebyechocardiography
YES NO
UVCinthetargetzoneby radiographicimage
YES 25 34 59
NO 19 84 103
44 118 162
UVC,umbilicalvenouscatheter.
T8
T9
T10
RA
a
b
d
c
AO
LA
LA AO
RA Liver
UVC RVOT
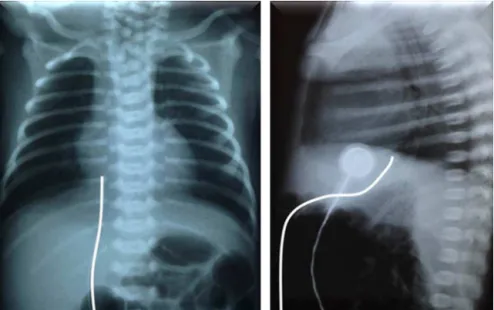
Figure1 Anteroposteriorchest X-rayshowing theumbilical venouscatheterinT9,just abovethediaphragmand cavoatrial junction,interpretedaswellpositioned(a)andcorrespondingechocardiographicimage(b)demonstratingthedistalendofthe catheterinthe leftatrium, after crossing theinteratrial septum(*).In another newborn,theradiographic imageshowed the catheterbetweenT9andT10,belowthediaphragmandcavoatrialjunction,suggestingitispositionedintheliver(c),butitsend wascorrectlyidentifiedintheinferiorvenacavajunctionwiththerightatriumbytheechocardiography(d).LA,leftatrium;RA, rightatrium;AOaorta;UVC,umbilicalvenouscatheter;RVOT,rightventricularoutflowtract.
area by the radiograph, 19 were visualized at the target zoneontheechocardiography(NPVof81.55%).Thisresults in a sensitivity of 56% and specificity of 71% for radio-graphs in the evaluation of UVC target area positioning (Table1).
Fig. 1 shows two examples of discordance between assessmentsofUVCpositionbyanteroposteriorchest radio-graphyandthecorrespondingechocardiographicimage.The
1
0.9
0.8
0.7
0.6
0.5
0.4
0.3
0.2
0.1
0
0 0.1 0.2 0.3 0.4 0.5
False positive
Area under the ROC curve = 0.6615947 (0.5779026 – 0.7452869)
T
rue positiv
e
0.6 0.7 0.8 0.9 1
Figure2 ROCcurve to assessthe performanceofthe ver-tebrallevelmethodinpredictingthepositionoftheumbilical venouscatheter.
Sixty-eight(41.98%)catheters,considered tobe intrac-ardiac, were pulled back by neonatologists before the echocardiography was performed, requiring more than one radiographic image. Of these 68 pulled catheters, 14 (20.59%) were visualized in the liver through the echocardiographyand were removed. A lower mean ges-tationalage(30.77±4.38vs.33.21±3.82weeks,p<0.01, ANOVA)and a lower meanbirth weight(1566.29±924.73
vs. 1984.67±839.06g, p<0.01, ANOVA) were statistically significantriskfactorsforpoorUVCpositioning,aftera pre-liminaryassessmentofthechestradiography.
Althoughsalinecontrastwasinjectedintoallcatheters, itwasusefulinonly56(34.57%)casestodeterminetheexact positionofthetip,moreoftenwhenthetipwasintheductus venosusorhepaticvessels(36patients).Intheothercases, theechocardiographic image alone wasenough toclearly identifythecatheterlocation.
The mean time intervalbetween the radiographic and echocardiographicstudies was14h (ranging from5min to 31h).
Discussion
Radiographic control for UVC position assessment was introduced by Peckand Lowman15 in 1967, and the tech-nique remains the most often used.2,4,9,11,16 After the 1980s, various studies that evaluated the catheter by ultrasonography5,9,12,17 or echocardiography2,4,7,14 showed thatthechestanteroposteriorradiographyaloneisnot capa-bleofensuringareliableUVCpositioning.
In 1995, Greenberg et al.12 demonstrated that 90% of catheterspositionedbetweenT8andT9and100%ofthose at T9 were correctly positioned in the IVC/RA junction. However, other studies have identified a poor correla-tion between the thoracic level and echocardiographic orultrasonographiclocation.2,9,13 Cathetersthat are well-positioned in the target area may be located in a wide range of vertebral bodies, from T6 to T112 or even at T4.13 The present study also showed a lower capacity of
thevertebralbodymethodtodifferentiatebetween well-positionedcathetersandpoorlypositionedones(areaunder theROCcurveof0.66).
Accordingtothecase-controlstudycarriedoutbyRaval etal.,7thedetectionofapoorlypositionedUVCintheleft atriumthrougharadiographshowedasensitivity,specificity, andaccuracyof45%,87%,and66%,respectively.These find-ingsaresimilartothosefoundbyAdesetal.2(32%,89%,and 63%,respectively). Micheletal.13 evaluatedthe radiogra-phycapacitytodeterminetheadequatepositioningofthe UVCandconcludedthatitwasinefficientindeterminingthe cathetertip position(sensitivity 66% andspecificity 63%). Inthepresentstudy,theradiographyaccuracyindetecting a well-positionedcatheterwas67%,i.e., themethodwas notabletoidentifymalpositionatapproximately33%ofthe time.
In 2014, Hoellering et al.9 recommended that, if the assessmentoftheUVCbyultrasonographyisnotavailable, thepositionshouldbedeterminedbythecardiacsilhouette method. This method, unlikethe vertebralbody method, wasabletoaccuratelypredictcatheterposition;however,it waslocatedinthetargetareainonly35(18%)of200 assess-ments.Inthisstudy,thecatheterswerefound adequately positioned in the target area in 27% of the assessments, as documented by echocardiography, evenwhen simulta-neouslyanalyzingthevertebralbody,cardiacsilhouette,and diaphragmmethods.
A high need for UVC repositioning after radiographic controlwasidentified(41.98%),significantlyhigherin new-bornswithlowermeangestationalageandlowermeanbirth weight,similartothefindingsofHaraborandSoraisham.16 Micheletal.13 foundan accuracyofthechestradiography todefineUVCpositionthatwassignificantlyhigherin new-bornswithlowbirthweight.However,thestudywascarried outwithadifferentreferencestandard(jointinterpretation of the resultsof radiography andultrasonography), which does notallow foran adequate comparativeanalysiswith thepresentstudy.
Catheters identified by radiographic assessment as intracardiac may be in the appropriate position, as sug-gested by Ades et al.2 If unnecessarily pulled back, they will be displaced into the liver, as documented by echo-cardiography in 14 (20%) assessed infants. This resulted in loss of venous access, increased patient handling, and exposuretoradiation.Flemingdescribedthesame:‘‘Every cathetermanipulationhasariskofvesseltrauma,infection, orthrombosis’’.17
In1969,Baker etal.18 were thefirsttoemphasize the importance of using lateral radiographic projections. The lastportionoftheductusvenosusrunsinthesagittalplane and,therefore,itisonlycorrectlyvisualizedinalateral pro-jection,andpoorpositioningcanbeeasilyidentified.5,11,19,20 TheUVCappearsinthefrontalprojectionasastraightline orslightlycurvedtotheright;atthelateralprojection,itis seenanteriorlycrossingtheliverandasanS-shapedcurve beforeitreachestheheart5,18---23(Fig.3).Thelateral projec-tionincreasesthechestradiographyaccuracyinpredicting the UVClocation;ontheother hand, itresults in greater exposureofthenewborntoradiation.
Figure3 Trajectoryoftheumbilicalvenouscatheterinchestradiographyattheanteroposterior(left)andlateral(right)views.
Thecatheterimageprojectedondifferentanatomical land-marksundergoeschangesaccordingtothedegreeofimage distortion,lungaeration,andthenewborn’sposition.24,25As thecatheterisinsertedintotheumbilicalveinandblindly advancedtothepredeterminedlength,thealignmentand correct use of the central radius cannot be guaranteed. Given the short length of the target area9 and the chil-dren’ssmallsizes,particularlythosewhorequireumbilical access,asmallrotationorinclinationandcatheterexposure tothedivergingradiusesmayresultinimageswith signif-icantlydifferent findings, which donot accurately reflect theirposition.
Duringa UVCstudyusing ultrasonography,Fleming and Kim17observedameanofcathetermigrationtotheheartof 5.4mm (max18mm)withlower-limbmovement.This dis-tancebecomesvery relevantwhen considering the target zone length of4---11mm (median6mm), accordingto the studybyHoelleringetal.,9andmayexplainthelowaccuracy oftheanteroposteriorchestradiograph.
Duringrepositioningunderdirectvisualizationofpoorly positionedcatheters,itwasobservedwithinterestthat sim-plyremovingthefixing bandagewassometimesenoughto placeitinanacceptableposition.Thatis,asimplepressure onthefixing bandagecanleadtoan inadvertentlydeeper catheterpositioning.
After the UVC insertion, it is important to ensure its correct positioning in order to prevent potentially fatalcomplications.Complicationswerenotsystematically assessed in this study. However, threecases of thrombus were identified, two intracardiac and one at the IVC/RA junction,twoliverlacerationswithfluidoverflowintothe hepatic parenchyma, and two pericardial effusions. The lesionsspontaneouslyregressedaftertheUVCwithdrawal, exceptforoneintracardiacthrombusthatshowed progres-siveincreasein size,forwhichthechildwastreatedwith enoxaparin.
Themajorlimitationofthisstudywasthemeantimeof 14h(range5minto31h)betweentheradiographyandthe echocardiography, which cannot guarantee the constancy of catheter positioning. Hoellering et al.9 described that
cathetermigrationafterafewhoursisnotunusualin clini-calpractice,butthedisplacementisverifiedthroughserial chestradiographies.However,radiographicimagesobtained with different exposure settings and with the patient in different positions may result in catheter tip projections at different locations. During this study, the authors re-evaluatedthreeinfantswithsuspectedcathetermigration, whichwasnotconfirmedbyechocardiography.Therefore,to quantitatethedegreeofUVCmigration,itwouldbe neces-sarytocarryoutprospectivestudiesusingimagingmethods thatallowadirectvisualizationofthetip,suchasultrasound orechocardiography.
The authors conclude that the anteroposterior chest radiography, a method routinely used to assess catheter positioning,isnotreliableinidentifyingtheexact anatomi-callocationofthedistalendoftheUVC.Echocardiography allowsdirectvisualizationofthecathetertipinrelationto vascular structures,reduceshandling of the newbornand exposureofthenewbornandmedicalstafftoradiationand, more importantly, prevents the complications associated withapoorly-positionedcatheter,andshouldthereforebe consideredasareferencestandardforlocationoftheUVC. Afteratrainingprotocolinechocardiographyorfunctional ultrasound,insertionoftheUVCwithdirectvisualizationis moreadequateandcanbeperformedbytheneonatologist inchargeoftheprocedure.4
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.DiamondLK.Erythroblastosisfoetalisorhaemolyticdiseaseof thenewborn.ProcRSocMed.1947;40:546---50.
3.FigueiredoIJr,LimaGM.Oconhecimentodeneonatologistas relativoatécnicasdeposicionamentodecateteresumbilicais. Pediatria(SãoPaulo).2004;26:85---9.
4.Pulickal AS, Charlagorla PK, Tume SC, Chhabra M, Narula P, NadrooAM.Superiorityoftargetedneonatalechocardiography for umbilical venouscathetertip localization:accuracy ofa clinicianperformancemodel.JPerinatol.2013;33:950---3.
5.SimanovskyN, Ofek-ShlomaiN, RozovskyK,Ergaz-ShaltielZ, HillerN,Bar-OzB.Umbilicalvenouscatheterposition: evalua-tionbyultrasound.EurRadiol.2011;21:1882---6.
6.VerheijGH,tePasAB,WitloxRS,Smits-WintjensVE,Walther FJ, Lopriore E. Pooraccuracy ofmethods currently usedto determine umbilical catheter insertionlength. Int JPediatr. 2010;2010:873167.
7.RavalNC,GonzalezE,BhatAM,PearlmanSA,StefanoJL. Umbil-icalvenouscatheters:evaluationofradiographstodetermine positionandassociatedcomplicationsofmalpositioned umbili-calvenouscatheters.AmJPerinatol.1995;12:201---4.
8.SymanskyMR,FoxHA.Umbilicalvesselcatheterization: indica-tions,managementandevaluationofthetechnique.JPediatr. 1972;80:820---6.
9.HoelleringAB,KoortsPJ,CartwrightDW,DaviesMW. Determina-tionofumbilicalvenouscathetertippositionwithradiograph. PediatrCritCareMed.2014;15:56---61.
10.Bentlin MR, Rugolo LM, Ferrari LS, on behalf of the Brazil-ian NeonatalResearchNetwork(RedeBrasileira dePesquisas Neonatais).Practicesrelatedtolate-onsetsepsisinvery low-birthweightpreterminfants.JPediatr(RioJ).2015;91:168---74.
11.El-MaadawySM,El-AtawiKM,ElhalikMS.Roleofbedside ultra-soundindeterminingthepositionofumbilicalvenouscatheters. JClinNeonatol.2015;4:173---7.
12.GreenbergM,MovahedH,PetersonB,BejarR.Placementof umbilicalvenouscatheterswithuseofbedsidereal-time ultra-sonography.JPediatr.1995;126:633---5.
13.MichelF,Brevaut-MalatyV,PasqualiR,ThomachotL,VialetR, HassidS,etal.ComparisonofultrasoundandX-rayin determin-ingthepositionofumbilicalvenouscatheters.Resuscitation. 2012;83:705---9.
14.GeorgeL,WaldmanJD,Cohen ML,SegallML,KirkpatrickSE, Turner SW, et al. Umbilical vascular catheters: localization bytwo-dimensional echocardio/aortography. Pediatr Cardiol. 1982;2:237---43.
15.PeckDR, Lowman RM.Roentgen aspectsof umbilical vascu-larcatheterization inthenewborn.Theproblem ofcatheter placement.Radiology.1967;89:874---7.
16.Harabor A, Soraisham A. Rates of intracardiac umbilical venous catheter placement in neonates. J Ultrasound Med. 2014;33:1557---61.
17.FlemingSE,KimJH.Ultrasound-guidedumbilicalcatheter inser-tioninneonates.JPerinatol.2011;31:344---9.
18.BakerDH,BerdonWE,JamesLS.Properlocalizationof umbil-icalarterialandvenouscathetersbylateralroentgenograms. Pediatrics.1969;43:34---9.
19.Narla LD,Hom M, Lofland GK, Moskowitz WB. Evaluation of umbilicalcatheterand tubeplacementinpremature infants. Radiographics.1991;11:849---63.
20.Oestreich AE. Umbilical vein catheterization --- appropri-ate and inappropriate placement. Pediatr Radiol. 2010;40: 1941---9.
21.Schlesinger AE, Braverman RM, DiPietro MA. Pictorial essay. Neonatesandumbilicalvenouscatheters:normalappearance, anomalouspositions,complications,andpotentialaidto diag-nosis.AJRAmJRoentgenol.2003;180:1147---53.
22.SandersCF.Theplacementoftheumbilicalvenouscatheterin thenewbornanditsrelationshiptotheanatomyofthe umbili-calvein,ductusvenosusandportalvenoussystem.ClinRadiol. 1978;29:303---8.
23.Rosen MS, Reich SB. Umbilical venous catheterization in thenewborn:identification ofcorrectpositioning.Radiology. 1970;95:335---40.
24.BushongSC.Ciênciaradiológicaparatecnólogos:física,biologia eprotec¸ão.9thed.RiodeJaneiro:Elsevier;2010.p.274---99.