REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
Official Publication of the Brazilian Society of Anesthesiologywww.sba.com.br
SCIENTIFIC
ARTICLE
Intraoperative
esmolol
infusion
reduces
postoperative
analgesic
consumption
and
anaesthetic
use
during
septorhinoplasty:
a
randomized
trial
Nalan
Celebi,
Elif
A.
Cizmeci
∗,
Ozgur
Canbay
DepartmentofAnaesthesiologyandReanimation,HacettepeUniversityFacultyofMedicine,Ankara,Turkey
Received17August2013;accepted31October2013 Availableonline2February2014
KEYWORDS
Analgesia; Bispectralindex; Esmolol;
Morphine
Abstract
Backgroundandobjectives: Esmololisknowntohavenoanalgesicactivityandnoanaesthetic
properties;however,itcouldpotentiatethereductioninanaestheticrequirementsandreduce
postoperativeanalgesicuse.Theobjectiveofthisstudyistoevaluatetheeffectofintravenous
esmololinfusiononintraoperativeandpostoperativeanalgesicconsumptionsaswellasitseffect
ondepthofanaesthesia.
Methods:Thisrandomized-controlleddoubleblindstudywasconductedinatertiarycare
hospi-talbetweenMarchandJune2010.Sixtypatientsundergoingseptorhinoplastywererandomized
intotwogroups.Historyofallergytodrugsusedinthestudy,ischaemicheartdisease,heart
block,bronchialasthma,hepaticorrenaldysfunction,obesityandahistoryofchronicuseof
analgesic or-blockerswereconsideredcause forexclusionfrom thestudy.Thirtypatients
receivedesmololandremifentanil(esmololgroup)and30patientsreceivednormalsalineand
remifentanil(control group)asan intravenousinfusionduring theprocedure.Meanarterial
pressure,heartrate,andbispectralindexvalueswererecordedevery10min.Total
remifen-tanilconsumption,visualanaloguescalescores,timetofirstanalgesiaandtotalpostoperative
morphineconsumptionwererecorded.
Results:Thetotalremifentanilconsumption,visualanaloguescalescoresat0,20and60min,
totalmorphineconsumption,timetofirstanalgesiaandthenumberofpatientswhoneededan
intravenousmorphinewerelowerintheesmololgroup.
Conclusions: Intravenous infusion of esmolol reduced the intraoperative and postoperative
analgesicconsumption,reducedvisualanaloguescalescoresintheearlypostoperativeperiod
andprolongedthetimetofirstanalgesia;howeveritdidnotinfluencethedepthofanaesthesia.
© 2014SociedadeBrasileirade Anestesiologia.Publishedby ElsevierEditoraLtda.Allrights
reserved.
∗Correspondingauthor.
E-mail:elifcizmeci@hotmail.com(E.A.Cizmeci).
0104-0014/$–seefrontmatter©2014SociedadeBrasileiradeAnestesiologia.PublishedbyElsevierEditoraLtda.Allrightsreserved.
PALAVRAS-CHAVE
Analgesia; Índicebispectral; Esmolol;
Morfina
Infusãointraoperatóriadeesmololreduzoconsumopós-operatóriodeanalgésicose ousodeanestésicoduranteaseptorrinoplastia:estudorandômico
Resumo
Justificativaeobjetivos: esmololéconhecidopornãoteratividadeanalgésicaepropriedades
anestésicas;porém,podepotenciarareduc¸ãodanecessidadedeanestésicosereduzirouso
deanalgésicosnopós-operatório.Oobjetivodesteestudofoiavaliaroefeitodainfusãode
esmololporviaintravenosasobreoconsumodeanalgésicoduranteosperíodosintraoperatório
epós-operatório,bemcomoseuefeitosobreaprofundidadedaanestesia.
Métodos: esteestudorandômico,controladoeduplo-cegofoiconduzidoemumhospital
ter-ciário entre marc¸o e junho de 2010. Foram randomicamente divididos em dois grupos 60
pacientes programados para serem submetidos à septorrinoplastia. História de alergia aos
medicamentosusadosnoestudo,isquemiacardíaca,bloqueiocardíaco,asmabrônquica,
insufi-ciênciahepáticaourenal,obesidadeehistóriadeusocrônicodeanalgésicosou-bloqueadores
foram os critérios de exclusão. Trinta pacientes receberam esmolol e remifentanil (grupo
esmolol) e30 receberamsorofisiológicoeremifentanil(grupocontrole) viaperfusão
intra-venosa. Pressão arterial média, frequência cardíaca e valores do índice bispectral foram
registradosacada10minutos.Consumototalderemifentanil,escoresdaescalavisual
analóg-ica, tempo para a primeira analgesia econsumo total de morfina nopós-operatório foram
registrados.
Resultados: oconsumototalderemifentanil,osescoresdaescalavisualanalógicanos
minu-tos0,20e60,oconsumototaldemorfina,otempoparaaprimeiraanalgesiaeonúmerode
pacientesqueprecisaramdemorfinaintravenosaforammenoresnogrupoesmolol.
Conclusões:esmolol em infusão intravenosa reduziu o consumo de analgésicos tanto no
intraoperatórioquantonopós-operatório,reduziuosescoresdaescalaanalógicavisualno
pós-operatórioimediatoeprolongouotempoparaaprimeiraanalgesia;contudo,nãoinfluenciou
aprofundidadedaanestesia.
©2014SociedadeBrasileiradeAnestesiologia.PublicadoporElsevierEditoraLtda.Todosos
direitosreservados.
Introduction
Esmololisanultra-short-acting,cardioselective1-receptor antagonist.Itiseffectiveinbluntingadrenergicresponsesto perioperativestimuli,includingtrachealintubation,1
intra-operativeeventscausedbydecreasinganaestheticdepth,2
and tracheal extubation.3 Esmolol is known to have no
analgesicactivityandnoanaestheticproperties.4However,
previousstudieshaveshownthatesmololcouldpotentiate thereductioninanaestheticrequirementsduringpropofol,5
or volatile-based anaesthesia.6 In a previous study it was
suggestedthatesmololinfusionreducedtheintraoperative use of fentanyl, decreased haemodynamic responses and reducedpostoperativemorphineconsumption.7Esmololalso
decreasednociceptioninavarietyofexperimentalsettings, suggesting the potential to decrease the intraoperative anaesthetic requirements.8 In animals esmolol provided
analgesia and a reduction of cardiovascular responses to painin the absenceof anaesthesia.9 Howeverthe roleof
esmololinpainmodulationremainstobeestablished. This prospective, randomized, double-blind, placebo controlledstudywasdesignedtoassesstheeffectof peri-operativeesmololuponanalgesicconsumptionanddepthof anaesthesiainpatientsundergoingseptorhinoplastysurgery.
Methods
Patients
After approval by the Institutional Ethics Committee, patients’ written informed consents were obtained. The studytookplaceinatertiaryhospitalbetweenMarchand June2010.PatientsofAmericanSocietyofAnesthesiologists (ASA)physicalstatusI---II,ages18---65 yearsoldand under-goingseptorhinoplastywereenrolledinthisstudy.Patients wereselectedrandomlybyusingcomputer-generated ran-dom numbers and divided into two groups (esmolol vs. control).Exclusioncriteriaincluded allergichistorytoany of the drugs used in the study, ischaemic heart disease, heart block, bronchial asthma, hepatic or renal dysfunc-tion and obesity (body mass index≥30) and a history of
Anaesthesia
Allpatientswereinformedaboutthevisualanaloguescale (VAS; 0=no pain, 10=worst imaginable pain), the verbal ratingscale (VRS; 0=nopain,1=weak pain,2=moderate pain,3=severepain,4=excruciatingpain)andthe patient-controlledIVanalgesiadevicebeforesurgery.Patientswere not premedicated beforesurgery. All patients were mon-itored withbispectral index (BIS) in additionto standard monitorization.
Patientsintheesmololgroupreceivedaloadingdoseof esmolol(0.5mgkg−1in30mLnormalsaline)followedbyan infusionofesmolol(0.05mgkg−1min−1)whilepatientsinthe controlgroupreceivedthesamevolumeofnormalsalinefor loadingdoseandcontinuousinfusion.
General anaesthesia was induced in all patients with propofol (2.5mgkg−1) and a mixture of oxygen and air (50---50%). After induction, an infusion of remifentanil (0.05---0.5gkg−1min−1)wasstartedinbothgroups. Vecuro-niumbromide (0.1mgkg−1) was administeredto maintain musclerelaxationandfortrachealintubation.Sevoflurane atanend-tidalconcentrationof2MACinair/oxygenmixture was used for the maintenance of anaesthesia. To deter-mine the depth of anaesthesia, BIS monitoring was used in addition toautonomic or somatic signs and changesin meanarterialpressure(MAP)orheartrate(HR).ABISvalue between 40 and 60 was targeted since it was accepted as an adequate level of anaesthesia at which recall was prohibited.10
The depthofanaesthesiawasassessed.(1)Anincrease in MAP and HRof more than 20% from baselinefor more than 1min; (2) autonomic signs (e.g. mydriasis, flushing, lacrimation);(3)somaticsigns(e.g.purposefuleye move-ments,grimacing,swallowing); and (4) BISvaluesgreater than 60 were considered as inadequate depth of anaes-thesia.The remifentanildosewastitratedtoincrease the depthofanaesthesiainthepresenceofatleastoneofthese signs.Datawererecorded1minbeforeinduction, immedi-ately afterinduction, 1, 3 and5min after intubation and at10minintervalsduringsurgery.Duringsurgery,the qual-ityofthesurgicalfieldwasevaluatedevery10min bythe samesurgeon,whowasblindedtothestudy,usingan eval-uationscalefor bleedingofthesurgicalfield(Table1).At thecompletionofsurgery,allinfusionswerediscontinued.
Table1 Evaluationscaleforbleedingofsurgicalfield.
0Nobleeding
1Slightbleeding---nosuctioningofbloodrequired
2Slightbleeding---occasionalsuctioningrequired.Surgical
fieldnotthreatened
3Slightbleeding---frequentsuctioningrequired.Bleeding
threatenssurgicalfieldafewsecondaftersuction
removed
4Moderatebleeding---frequentsuctioningrequired.
Bleedingthreatenssurgicalfielddirectlyaftersuction
removed
5Severebleeding---constantsuctioningrequired.Bleeding
appearsfasterthancanberemovedbysuction.Surgical
fieldseverelythreatenedandsurgeryimpossible
Theneuromuscularblockwasantagonizedwithneostigmine (0.05mgkg−1) and atropine (0.01mgkg−1). The times to emergencefromanaesthesia(extubation,eyeopeningand responsetosimpleverbalstimuli),durationofsurgeryand totalremifentanil consumption were recorded. An anaes-thetistwhowasblindedtothestudygroupsconductedthe entirecourseofanaesthesia.Intraoperativebradycardiaand hypotensionweredefinedasaHRlowerthan45beats/min andaMAPvaluelessthan50mmHg, respectively.Patients experiencingbradycardiaorhypotensionweretreatedwith atropine(0.5mg)orintermittentephedrine(5mg).
Blindingwasachievedbyrequestingananaesthetistwho wasnotinvolvedinthestudytopreparetheinfusion solu-tionsforeachpatientaccordingtothecomputer-generated randomnumbersandgroupsdeterminedatthebeginningof the study.The solutions were labelledwith the patients’ names only. The patient name, number and the solution preparedwererecordedbythisanaesthetist.Thesolutions werethengiventotheanaesthetistadministeringthe anaes-thesia.
Postoperativemanagementandevaluations
Allpatients were transferred tothe postanaesthesia care unit(PACU)aftersurgeryandobservedfor3h.Painintensity wasevaluatedusingbothVASandVRS.Patients,whoseVAS scoreswere≥3atanytime,receivedanIVmorphineinfusion
(0.1mg/kgofloadingdose,1mgondemand,5minof lock-outtime)byaPCA device. VASandVRS scores,morphine consumption,timetofirstanalgesiaand sideeffectssuch assedation, nausea,vomiting, andrespiratory depression wererecordedattheindicatedtimeintervals.Thesedation levelwasrecordedaccordingtoafour-pointscale(0=awake andalert,1=mildlysedated,easytoarouse,2=moderately sedated but can be aroused, 3=deeply sedated, difficult toarouse).Vomitingwastreated withmetoclopramide IV (10mg). Respiratory depression was defined asa ventila-toryfrequencyoflessthan8perminute.TheAldretescore wasevaluatedtodeterminethetimetodischargefromthe PACU.Attheendof3h,patientswithanAldretescoreof≥9
weredischargedfromthePACUafterbeingdirectedtotake perioral(P.O)naproxensodiumforanalgesia,ifneeded.At thetimeofdischarge,allpatientswereaskedtwoquestions: (1)whatwasthelastthingyourememberafterenteringthe operatingroom?and(2) doyou recallanything fromyour operation?;todetermineiftheyrecalledanyintraoperative events.Timetodischargefromthehospitalwasrecorded. Theanaesthetistwhoobservedthepatientsduringsurgery alsoobserved thepatientsinthe PACU.Bothpatientsand observerswereblindwithrespecttotreatmentgroups.On the second day after surgery, patients were interviewed bytelephonetoevaluate thepainintensity and analgesic requirementafterdischarge.
Statisticalanalysis
Table2 Patientandsurgicalcharacteristics.
Controlgroup(n=30) Esmololgroup(n=30) p-Value
Age(yr) 29.1(9.5) 27.4(7.9) 0.445
Gender(F/M) 19/11 21/9 0.584
Weight(kg) 61.8(11.8) 60.7(8.7) 0.691
Height(cm) 169(8.9) 167(6.6) 0.328
ASA(I/II) 27/3 29/1 0.612
Durationofsurgery(min) 109(35.1) 97(27.8) 0.148
Durationofanaesthesia(min) 126.6(36.9) 111(29) 0.093
TRemifentanilused(mg) 1.6(1.3) 0.8(0.5) 0.004a
Theemergencetimes(min)
Extubation 4.5(2.3) 5.3(2) 0.568
Openingeyes 5.3(2.4) 6(2.1) 0.602
Responsetoorders 6(2.4) 6.3(2) 0.856
Valuesaremean(SD)ornumber.
ap<0.05;statisticallysignificant.
presented asmedian and standard deviation. The ordinal variableswerepresented asmedian (inter-quartilerange) andcategoricalvariableswerepresentedaspercentage(%). ThemeanvaluesofgroupswerecomparedusingStudent’s tor Mann---WhitneyUtests.RepeatedSAP,DAP,MAP, SpO2 andHRvalueswerecomparedusingtheBonferroni multi-plecomparisonstestwithinthegroupsandbetweengroups. Variance analysis was used for repeated measurements. Becauserepeatedvariablesshowedsignificantchange,the measurement time causing this change was determined forcategoricalcomparisonsusingChi-squaredandFisher’s exacttests.TheMann---WhitneyUtestwasusedtocompare nonparametricvariables.Statisticalsignificancewassetat p<0.05.
Results
All 60 patients enrolled in the study were evaluated for statistical analysis and all the analyses were performed according tothe original groups. Allpatients were evalu-ated for the analgesic andanaesthetic effects of esmolol andnopatientswereexcludedafterrandomization.Patient characteristics,durationofsurgeryandanaesthesia, quan-tity of remifentanil used, the emergence times from the endofanaesthesiaforthetwogroupsareshowninTable2. Remifentanilusedduringanaesthesiawassignificantlylower in the esmolol group (p=0.004). There were no differ-encesinpatientcharacteristics,durationofanaesthesiaand surgeryandtheemergencetimesfromtheendof anaesthe-siabetweentwogroups.
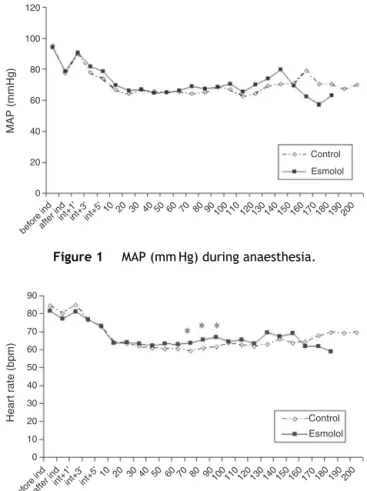
TheMAPduringanaesthesiaisshowninFig.1.Therewas nosignificantdifferencebetweentwogroupswithregardto MAPduringanaesthesia.TheMAPshowedfluctuationsfrom baselinevalueinbothgroups.
TheHRduringanaesthesiaisshowninFig.2.TheHRat 70th,80thand90thminutesafterintubationwashigherin theesmololgroup(p=0.035,p=0.027andp=0.017, respec-tively).The HRwasgenerallyhigherduring surgeryinthe esmololgroupbutitwasnotstatisticallysignificant.TheHR showedfluctuationsfrombaselinevalueinbothgroups.
The BISvaluesareshown inFig.3. Therewereno sig-nificantdifferencesbetweentwogroupswithregardtoBIS
values during anaesthesia. There were also nosignificant differencesfromthebaselinevalueinbothgroups.
VASandVRSscoresareshown inFigs.4and5, respec-tively. The VASand VRSscores were significantlylower in theesmolol groupat1and20minand1h after anaesthe-sia (p=0.001,p=0.034 andp=0.016, respectivelyfor VAS scores; p=0.033, p=0.016 and p=0.022, respectively for VRSscores).
120
100
80
60
MAP (mmHg) 40
20
before indafter ind int+1
' int+3
' int+5
'
10 20 30 40 50 60 70 80 90 100110 120130 140 150 160 170 180 190 200 0
Control Esmolol
Figure1 MAP(mmHg)duringanaesthesia.
90 80
70 60
Hear
t r
a
te (bpm)
50 40
30 20
10
before indafter ind int+1
' int+3
' int+5
'
10 20 30 40 50 60 70 80 90 100 110 120130 140 150 160 170 180 190 200 0
Control Esmolol
Figure2 HR(beatsmin−1)duringanaesthesia.*p<0.05;
100
80
60
Bispectr
al inde
x
40
20
0
before indafter ind int+1
' int+3
' int+5
'
10 20 30 40 50 60 70 80 90 100 110 120130 140 150 160 170 180 190 200 Control Esmolol
Figure3 BISvaluesduringanaesthesia.
0 2 4 6
48h 24h 12h 3h 2h 1h 20' 0'
VAS scores
Control Esmolol ∗
∗
∗
Figure4 VASscores inthe postoperative period. *p<0.05; statisticallysignificant.
TimetofirstanalgesiaanddischargefromPACU,Aldrete scores, quantityand percentageof IVmorphineand anal-gesicusedafterdischargeandtheincidenceofsideeffects inboth groups areshownin Table3.Timetofirst analge-siawassignificantlylongerintheesmololgroup(p=0.001). Totalmorphineconsumptionandthenumberofpatientswho received IV morphine were significantly lower in esmolol group(p=0.011andp=0.005,respectively).
0 1 2 3
48h 24h 12h 3h 2h 1h 20' 0'
VRS scores
∗ ∗
∗
Control Esmolol
Figure5 VRS scoresinthe postoperative period.*p<0.05; statisticallysignificant.
Discussion
In this study we found that esmolol shows a postopera-tiveanalgesiceffectwhenadministeredintraoperativelyin septorhinoplastypatients.Esmolol reducedthe postopera-tiveVASandVRSscores,togetherwithelongatingthetime tofirstanalgesia andreducingboth thetotalIVmorphine consumption and the number of patients who needed morphine. Also, the amount of remifentanil used during anaesthesiawassignificantlylowerintheesmololgroup.
Previous studies focused on the effect of -blocker usage upon anaesthesia and postoperative pain manage-menthavesuggestedthat-antagonistsreduceanaesthetic requirements during anaesthesia5 and inhalation
anaes-theticminimumalveolarconcentration(MAC),6andimprove
earlypostoperativerecovery.11
Thespecificmechanismbywhich-blockadepotentiates the analgesic effect of an opioid remains controver-sial. Inhibitory G protein-coupled receptor agonists act upon postsynaptic inhibition via G protein-coupled potas-sium channels or via the pre-synaptic inhibition of
Table3 Patients’datainpostoperativeperiod.
Controlgroup(n=30) Esmololgroup(n=30) p-Value
Timetofirstanalgesia(min) 43.8(60.8) 108(81.6) 0.001a
Morphineused(mg) 12.9(8.7) 7.1(8.4) 0.011a
Morphineusage(%) 86.7 53.3 0.005a
Timetodischarge(min) 202.8(38) 189.5(11.5) 0.071
Aldretescore(9/10) 4/26 3/27 0.688
Analgesicathome(tablets) 3.6(2.5) 2.6(2.2) 0.92
Analgesicathome(%) 80 73.3 0.542
Sideeffects
Nausea 8 6 0.542
Vomiting 4 4 1.000
Sedationscores(0/1) 4/26 2/28 0.389
Valuesaremean(SD)ornumber.
neurotransmitterreleasethroughtheregulationof voltage-gated Ca2+ channels; such a pathway underlies the nociceptiveeffectofclonidine.12Hagelukenandcolleagues
demonstrated that -adrenergic antagonists activated G-proteins in isolatedcell membranesand it wassuggested thatthiswasthemechanismofcentralanalgesia.13
Esmolol has been postulated to reduce anaesthetic requirementsviaadirectantinociceptivepropertyina vari-ety of experimental studies, suggesting the potential to decreasetheintraoperativeanaestheticrequirements.8,14In
animalsesmololprovidedanalgesiaandreductionof cardio-vascularresponsestopainintheabsenceofanaesthesia.9
Anothermechanismthatmaysignificantlycontributeto theanaesthetic-sparinginvolvesdecreasedexcitatory stim-ulationofcentralnervoussystemeffectorsitesofhypnosis and somatic response. In this case, peripheral interrup-tionof-adrenergicautonomicpathwaysdecreasesafferent inputandanaestheticrequirements.15Theclinicalutilityof
thiseffectwasdemonstratedbyZauggetal.11inastudywith
elderly surgical patients undergoing non-cardiac surgery. Pre- and postoperative atenolol and high dose intraoper-ative atenolol decreased requirements for intraoperative fentanylandpostoperativemorphine.Chiaetal.7suggested
thatperioperativeesmololadministrationreducedthe intra-operativeuseofisofluraneandfentanylaswellasreducing morphineconsumptionfor3dayspostoperativelyinpatients undergoingabdominaltotalhysterectomy.
Several studies have suggested that sympatholytic drugs may be alternative to opioids in treating acute intraoperative haemodynamic responses. It was reported that in elderly patients undergoing noncardiac surgery, perioperative -blockade with atenolol improved haemodynamic stability, reduced the opioid analgesic requirementand contributedto afaster early recovery.11
In a previous study, it was suggested that perioperative
-antagonistadministrationwasanalternativeto remifen-tanilin maintaining intraoperative stable haemodynamics withsimilar side effects.16 This was also the case in our
study,with nostatistically significant differencebetween groupswithrespecttointraoperativeHRandMAP, demon-stratingthatesmololsuccessfullyreplacedaroleclassically performedbyremifentanil.
Some studies suggested that administration of esmolol attenuated the cardiovascular response to perioperative stimuli.Milleretal.1suggestedthatabolusdoseofesmolol
combinedwithalowdoseofnarcoticresultedineffective controlofhaemodynamicresponsetotrachealintubation. Indifferentstudies,itwasdemonstratedthatasinglebolus doseofesmololeffectivelyattenuatedHRandsystolicblood pressureincreasesproducedby laryngoscopyandtracheal intubation.17,18
Similar to these studies, esmolol attenuated haemodynamic responses to perioperative stimuli such astracheal intubation, incision and extubation and there were no differences between groups in our study with respecttohaemodynamicresponses.
Adequate depthof anaesthesiaasindicated by theBIS was achieved in a group of elderly patients, using high dose atenolol and a restricted amount of anaesthesia.11
Inparalleltothisstudy despiteremifentanilrequirements beingsignificantlylower,anaesthesiawasstilladequateas indicated by BIS in the esmolol group and no recall was
seen in either of the groups in our study. Also, noxious stimuli during general anaesthesia causes an increase in BISaswellastachycardia,hypertensionandmovement.19,20
Previous studies assessing the effectiveness of esmolol in bluntingthehaemodynamicresponses inducedbytracheal intubationfailedtomonitorelectricalactivityofthebrain. Only a few studies have evaluated the effect of interac-tionbetween-adrenergicantagonistsandanaestheticson BIS.11,16In2001Johansensuggestedthatperioperative
infu-sion of esmolol decreased BIS values and increased burst suppressionratio.21 In2002,Menigauxandcolleagues
sug-gestedthatesmololattenuatedhaemodynamicandsomatic responsestolaryngoscopyandorotrachealintubation,and also prevented BIS arousal reactions in patients anaes-thetizedwithpropofol.22InourstudyesmololpreventedBIS
increasesinresponsetonoxiousstimuliincludingtracheal intubation,incisionandtrachealextubationaswellas blunt-ing haemodynamic responses in relation to these stimuli. Only one patient in both groups demonstratedsignificant tachycardiaandhypertensionassociatedwithanincreasein BIS.The clinicalimportanceofthisfindingisthatesmolol may have thepotential toreplace anaesthetic drugs that are givenfor the sole purposeof blunting haemodynamic responses.
TitrationofanaestheticstoHRandbloodpressure with-outadministrationof-adrenergicantagonistsmayleadto prolonged recovery from anaesthesia as a result of ‘rel-ative overdosing’ with administered anaesthetics and/or analgesics.Fasterrecoveryfromanaesthesiawasreported in patients receivingpropranolol.23 It wasshown that the
extubation time and recovery in the PACU were signifi-cantlyfasterinpatientstreatedwithintra-orperioperative atenolol.11 In contrast to these studies, there were no
differences in extubation time and recovery from anaes-thesia between groups in our study. In these studies the patientswereunderchronic-adrenergicantagonist treat-ment in the preoperative period or high dose atenolol was administered intraoperatively. However none of our patients were receiving -adrenergic antagonists chron-ically and esmolol was not administered in high dose, suggesting arelationshipbetween thechronicityofuse of
-adrenergic antagonists and the time to recovery from anaesthesia.
There aresome limitations to this study.The patients intheesmololgroupreceivedremifentanilasananalgesic during the operation. BIS values were recorded to deter-mine wakefulness of patients. Although BIS values during surgeryweresimilarbetweengroups,analgesiaisa differ-ent concept from anaesthesia. The esmolol administered topatientsmayhavepartiallymaskedtheclassical hyper-tensionandtachycardiaresponsesthatareassociatedwith pain. However, analgesic administration was not omitted in the esmolol group, despite beingconsumed at a lower dose.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.MillerDR,MartineauRJ,WynandsJE,etal.Bolusadministration ofesmololforcontrollingthehaemodynamicresponseto tra-chealintubation:theCanadianmulticentretrial.CanJAnaesth. 1991;38:849---58.
2.GoldJI, SacksDJ, GrosnoffDB, etal. Useofesmolol during anesthesiatotreattachycardiaandhypertension.AnesthAnalg. 1989;68:101---4.
3.FuhrmanTM,EwellCL,PippinWD,et al.Comparison ofthe efficacyofesmolol and alfentanilto attenuatethe hemody-namicresponsetoemergenceand extubation.JClinAnesth. 1992;4:444---7.
4.AngaranDM,SchultzNJ,TschidaVH.Esmololhydrochloride:an ultrashort-acting,beta-adrenergicblockingagent.ClinPharm. 1986;5:288---303.
5.Johansen JW, Flashion R, Sebel PS. Esmolol reduces anes-theticrequirement for skin incision,during propofol/nitrous oxide/morphineanesthesia.Anesthesiology.1999;91:1674---86.
6.JohansenJW,SchneiderG,WindsorAM,etal.Esmolol potenti-atesreductionofminimalalveolarisofluraneconcentrationby alfentanil.AnesthAnalg.1998;87:671---6.
7.ChiaYY,ChanMH,KoNH,etal.Roleof-blockadein anaesthe-siaandpostoperativepainmanagementafterhysterectomy.Br JAnaesth.2004;93:799---805.
8.DavidsonEM,SzmukP,DoursoutMF,etal.Antinociceptive prop-erties of labetolol in the rat formalin test. Anesthesiology. 1998;89:S1091.
9.DavidsonEM,DoursoutMF,SzmukP,etal.Antinociceptiveand cardiovascularpropertiesofesmololfollowingformalin injec-tioninrats.CanJAnesth.2001;48:59---64.
10.Newfield P, Cottrell JE. Handbook of neuroanaesthesia. Philadelphia:LippincottWilliams&Wilkins;2003.p.39.
11.ZauggM,Tagliente T, LucchinettiE,et al.Beneficial effects from-adrenergicblockadeinelderlypatientsundergoing non-cardiacsurgery.Anesthesiology.1999;93:209---18.
12.MitrovicI,Margeta-MitrovicM,BaderS,etal.Contributionof GIRK2-mediatedpostsynapticsignalingtoopiateand alpha 2-adrenergicanalgesiaandanalgesicsexdifferences.ProcNatl AcadSciUSA.2003;100:271---6.
13.HagelukenA,NaurnbergB,HarhammerR,etal.Lipophilic beta-adrenoreceptorantagonistsare effective directactivatorsof G-proteins.BiochemPharmacol.1994;47:1789---95.
14.Johansen JW, Sebel PS. Possible interaction of esmolol and nitrousoxide.Anesthesiology.1997;87:461---2[letter].
15.VucevicM,PurdyGM,EllisFR.Esmololhydrochloridefor man-agementofthecardiovascularstressresponsetolaryngoscopy andtrachealintubation.BrJAnaesth.1992;68:529---30.
16.Coloma M,ChiuJW, White PF, et al. The use ofesmolol as analternativetoremifentanilduringdesfluraneanesthesiafor fast-tractoutpatientgynecologiclaparoscopicsurgery.Anesth Analg.2001;92:352---7.
17.EbertTJ,BernsteinJS,StoweDF,etal.Attenuationof hemo-dynamicresponsestorapidsequenceinductionandintubation inhealthypatientswithasingledoseofesmolol.JClinAnesth. 1990;2:243---52.
18.ParnassSM,RothenbergDM,KerchbergerJP,etal.Asinglebolus doseofesmololinthepreventionofintubation-induced tachy-cardiaandhypertensioninanambulatorysurgeryunit.JClin Anesth.1990;2:232---7.
19.IselinChavesIA,FlaishonR,SebelPS,etal.Theeffectofthe interaction ofpropofol and alfentanilonrecall,loss of con-sciousnessandbispectralindex.AnesthAnalg.1998;87:949---55.
20.GuignardB,MenigauxC,DuPontX.Theeffectofremifentanilon thebispectralindexchangeandhemodynamicresponsesafter orotrachealintubation.AnesthAnalg.2000;90:161---7.
21.JohansenJW.Esmololpromoteselectroencephalographicburst suppression during propofol/alfentanil anaesthesia. Anest Analg.2001;93:1526---31.
22.MenigauxC,GuignardB,AdamF,etal.Esmololprevents move-mentandattenuatestheBISresponsetoorotrachealintubation. BrJAnaesth.2002;89:857---62.