REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
PublicaçãoOficialdaSociedadeBrasileiradeAnestesiologiawww.sba.com.br
SCIENTIFIC
ARTICLE
Influence
of
perfusion
status
on
central
and
mixed
venous
oxygen
saturation
in
septic
patients
Simone
Harumi
Goto
∗,
Bruno
Franco
Mazza,
Flávio
Geraldo
Resende
Freitas,
Flávia
Ribeiro
Machado
UniversidadeFederaldeSãoPaulo,EscolaPaulistadeMedicina,HospitalUniversitário,SãoPaulo,SP,Brazil
Received30May2016;accepted21March2017 Availableonline8August2017
KEYWORDS Sepsis;
Venousoxygen
saturation;
Mixedoxygen
saturation
Abstract
Backgroundandobjectives: Although thereiscontroversy regardingthe role ofvenous oxy-gensaturationintheinitialresuscitationofsepticpatientswithhypoperfusionthesemarkers arestillwidelyused.Thisstudyaimedtoevaluatethecorrelationandconcordancebetween central(SvcO2)andmixed(SvO2)oxygensaturationinsepticshockpatientswithorwithout
hypoperfusioninadditiontotheimpactofthesedifferencesinpatientconduction.
Methods:Patients with septic shock were monitored with pulmonary artery catheter and the following subgroups of hypoperfusion were analyzed: 1) lactate>28mg.dL−1; 2) base
excess≤−5mmol.L−1;3) venoarterial CO
2 gradient>6mmHg; 4) SvO2<65%;5) SvcO2<70%;
6)lactate>28mg.dL−1andSvO
2<70%;7)lactate>28mg.dL−1andSvcO2<75%.
Results:Seventy-sevensamplesfrom24patientswereincluded. Therewasonlyamoderate correlationbetweenSvO2andSvcO2(r=0.72,p=0.0001)andtherewasnogoodconcordance
betweenthesevariables(7.35%biasand95%concordancelimitsof−3.0%to17.7%).Subgroup analysis according tothe presence ofhypoperfusion showed nodifferences inconcordance between variables.Therewasdiscordanceregardingclinicalmanagementin13.8%(n=9)of thecases.
Conclusions: ThereisamoderatecorrelationbetweenSvO2andSvcO2;however,the
concord-ancebetween themisinadequate.Itwasnotpossibletodemonstratethatthepresenceof hypoperfusion alters theconcordancebetween SvO2 andSvcO2.The useofSvO2 instead of
SvcO2mayleadtochangesinclinicalmanagementinasmallbutclinicallyrelevantportionof
patients.
©2017SociedadeBrasileiradeAnestesiologia.Publishedby ElsevierEditoraLtda.Thisisan openaccessarticleundertheCCBY-NC-NDlicense( http://creativecommons.org/licenses/by-nc-nd/4.0/).
∗Correspondingauthor.
E-mail:goto.simone@gmail.com(S.H.Goto). http://dx.doi.org/10.1016/j.bjane.2017.03.002
PALAVRAS-CHAVE Sepse;
Saturac¸ãovenosade
oxigênio;
Saturac¸ãomistade
oxigênio
Influênciadostatusperfusionalnassaturac¸õesvenosasdeoxigêniocentralemista
empacientessépticos
Resumo
Justificativaeobjetivos: Emborahajacontrovérsiassobreopapeldassaturac¸õesvenosasde oxigênionaressuscitac¸ãoinicialdopacientesépticocomhipoperfusão,essesmarcadoressão aindabastante usados.Esteestudoprocurouavaliaracorrelac¸ãoeaconcordânciaentreas saturac¸õesvenosascentral(SvcO2)emista(SvO2)deoxigênioempacientescomchoqueséptico,
napresenc¸aounãodehipoperfusão,alémdoimpactodessasdiferenc¸asnaconduc¸ãoclínica dopaciente.
Métodos: Foramincluídospacientescomchoquesépticomonitoradoscomcateterdeartéria pulmonar e analisados os seguintes subgrupos de hipoperfusão: 1) Lactato>28mg.dL−1; 2)
Excesso debases≤-5mmoL.L−1;3)Gradientevenoarterial deCO
2>6mmHg; 4)SvO2<65%;
5)SvcO2<70%;6)Lactato>28mg.dL−1eSvO2<70%;7)Lactato>28mg.dL−1eSvcO2<75%. Resultados: Foramincluídas70amostrasde24pacientes.Houveapenascorrelac¸ãomoderada entreSvO2eSvcO2(r=0,72;p=0,0001)enãohouveboaconcordânciaentreessasvariáveis(viés
de7,35%elimitesdeconcordânciade95%de-3,0%-17,7%).Aanálisedossubgruposdeacordo comapresenc¸adehipoperfusãonãomostroudiferenc¸asnaconcordânciaentreasvariáveis. Houvediscordâncianacondutaclínicaem13,8%doscasos(n=9).
Conclusões:Existecorrelac¸ãomoderadaentreSvO2eSvcO2,entretantoaconcordânciaentre
elaséinadequada.Nãofoipossíveldemonstrarqueapresenc¸adehipoperfusãoalteraa con-cordânciaentreaentreSvO2eSvcO2.OusodaSvO2emvezdaSvcO2podelevaraalterac¸ões
nacondutaclínicanumaparcelapequena,porémclinicamenterelevante,dospacientes. ©2017SociedadeBrasileiradeAnestesiologia.PublicadoporElsevierEditoraLtda.Este ´eum artigoOpen Accesssobumalicenc¸aCCBY-NC-ND( http://creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
Sepsis is defined as an infection followed by systemic manifestationsresultingfromthehost’sdeleterious inflam-matoryresponse.Itaffectsmillionsofpeopleworldwideand hasahighmortalityraterangingfrom20%to80%.1---5Rivers etal.usedcentralvenousoxygensaturation(SvcO2)asone
of the componentsof early goal-directed therapy (EGDT) andshowedasignificantmortalityreductioninpatientswho mettheproposedgoals.6 Subsequently,other studiesthat involved a greater number of patients did not reproduce these results and suggested that there wasno benefit in theimprovementguidedbythisvariable.7---9However,these studieswereperformedinplaceswithhigh-qualityprimary care,resultinginlowmortalityrateinthecontrolgroups, arealityquite differentfromthatfound incountrieswith limitedresources.10,11Itshouldalsobeconsideredthat pre-randomizationinterventionsresultedinanalreadyimproved SvcO2inmostpatientsincluded.Theimpactofinterventions
for SvcO2 normalization in patients who persisted at low
valuesprior torandomizationwasnotassessed. Moreover, enhancementbasedon classicalEGDT wasnotassociated withincreasedadverse events. Forall thesereasons, the SepsisSurvivalCampaignhaschosentomaintaintheSvcO2
measurementasoneofthepossibletherapeutictargetsin patientswithinitialsignsofhypoperfusion.12
SvcO2 measurement is quicker, easier, and involves
lowercostsandrisksthanmixedvenoussaturation(SvO2),
whichrequirestheinsertionofapulmonaryarterycatheter (PAC), a more invasive device whose usefulness remains
questionable.Furthermore,thereisnoconsensusregarding the behavior of these oxygenation variables. Some argue that SvcO2 and SvO2, although numerically different, are
related,have similartrends duringpatientevolution, and bothareclinicallyuseful.
SvcO2differsfromSvO2byreflectingtheoxygencontent
in blood after its consumption by the upper limbs and cephalic segment, as it is measured through the blood collected from the superior vena cava. SvO2, in its turn,
indicates the blood oxygen contentafter this gas extrac-tionthroughoutthebody,includingtheheart.13 Ifthereis splanchnic hypoperfusion,thereis anincrease inthe rate ofoxygenextractioninthisregion;sothat,intheory,SvcO2
andSvO2wouldbeevenmoredisparate.Thus,theprimary
objectiveofthisstudywastoevaluateifthereis correla-tionandagreementbetweenthevaluesofSvcO2andSvO2in
patientswithseveresepsisorsepticshockandwhetherthe presenceofhypoperfusionalterstherelationshipsbetween thesetwovariables.The secondaryobjectivewasto eval-uatetheimpactofusingthesetwovariablesintheclinical managementofthepatient.
Methods
Patientsolderthan18yearswithsepticshock lessthan 48h after vasopressor initiation and monitored with PAC (Vigilance®, Edwards Lifesciences, Irvine, CA, USA) were included in the study. Sepsis was defined according to the consensus conference of the Society of Critical Care MedicineandtheAmericanCollegeofChestPhysician14and septicshock wasdefinedashypotensionrefractoryto vol-umereplacementinneedofvasopressors.Exclusioncriteria weregestation,hemoglobinlessthan7.0g.dL−1,hepatic
cir-rhosis,tricuspidvalvulopathy,pulmonaryvalvulopathy,and knownintracardiacshunts.
Demographic data, comorbidities, general character-istics of sepsis, the severity of the Acute Physiological and Chronic Health Evaluation (Apache II) scores, and the Sequential Organ Failure Assessment (Sofa) were recorded.
Blood sampleswere simultaneously collected from the pulmonary artery (distal lumen of PAC), superior vena cava (central venous catheter), and invasive blood pres-surecatheter.Arterialbloodlactatewasmeasured.Inorder toavoidcontaminationwithliquidsinfusedintocatheters, 5mL were aspirated from their lumen before collecting eachsample.Uptofourmeasurementswereperformedper patientwithaminimumintervalof6hbetweeneachsample collection.PACandcentralvenous catheterwereinserted throughtheinternalorsubclavianjugularveinandtheir cor-rectplacementwereconfirmedbythepulmonaryarteryand right atrium curvesand chestX-ray. Inaddition, hemody-namic andtissueperfusion parameters,hematimetry, and useanddoseofvasoactivedrugswererecordedatthetime ofsamplecollection.
Samples were immediately sent to laboratory for processing.Forarterial andvenous blood gasand arterial lactate examination, a microtechnique was usedin a gas analyzer (ABL 700 Radiometer, Copenhagen, Dinamarca). Blood gases with hyperoxia, with partial arterial oxygen pressure(PaO2)greaterthan150mmHgwereexcluded.
Toevaluatetheclinicalagreement,thesame investiga-tor assessed the hemodynamic and respiratory data sets, the diagnoses and vasoactive drug dosages, and defined whetherany approachtoward hemodynamic improvement wouldbenecessary.ConsideringthatSvcO2wasthe
param-eter validated by Rivers in his study,8 the percentage of timesinwhichtheuseofSvO2generateddifferentclinical
approacheswasevaluated.
Moreover,weoptedtoanalyzeasubgroup inwhichthe presenceofhyperlactatemiaandchangesinvenous satura-tionwere jointly evaluated. Patientswithlactategreater than 28mg.dL−1 associated withSvO
2<70%or SvcO2<75%
wereincludedinthissubgroup.Theselimitsweredefinedin ordertoexcludecasesofhyperlactatemiasecondarytolow oxygen usedue tocytopathichypoxemia or hyperflow.As the concomitant use of adrenaline could compromise the assessment of the presence of hyperlactatemia, patients taking this medication were included in this group only if SvO2 or SvcO2 were below 65% or 70%, respectively. To
define other groups considered as being under hypoper-fusion,thefollowinglimitswereused:lactate>28mg.dL−1
orbaseexcess(BE)lessthan5mmol.L−1orCO
2venoarterial
gradient(deltaCO2)greaterthan6mmHgor SvO2<65%or
SvcO2<70%.Patientswerealsoclassifiedaccordingtotheir
cardiacindex,usingasreference3.5L.min−1.m−2.
Statisticalanalysis
Inorder tocalculate thesample we sought to determine the existence of a correlation between two quantitative variables,withtwo-tailedtest,0.05significancelevel,and 0.80testpower.Itwasconsideredasanoptionalhypothesis theexistenceof correlationwithr=0.8 andnull hypothe-sisasnocorrelationwithr=0.4.Thecalculatedsamplesize was44.CalculationswereperformedusingtheSTPLAN soft-wareversion 4.1 for correlation tests of one-sample with normalapproximation.Consideringthepossibleasymptotic distributionofthevariableandthepossibilityofanalyzing subgroupsaccordingtothepresenceorabsenceof hypoper-fusion,thesamplewasrecalculatedin65pairs.
The continuous variables distributionpattern was ana-lyzed using the Kolmogorov-Smirnov test, with normal distribution presented as mean and standard deviation andnon-normaldistribution asmedianand 25thand75th percentile.Categorical variableswerepresented asa per-centage.Mann---Whitney test or Student’s t-test was used to compare the continuous variables, according to their distribution.The correlation between paired samples was assessedusingSpearman’scorrelationtestandconcordance usingtheBland---Altmantest,wherethe95%limitsof agree-ment represent the bias (mean absolute difference)±2 standarddeviations.Clinicalagreementwasreportedonly inadescriptiveway.
Inalltests,ap-value<0.05wasconsideredstatistically significant.Statisticalanalysiswasperformedusingthe Sta-tisticalPackageforSocialSciences(SPSS)version19.0and thesoftwareGraphPadPrismversion5.0.
Results
Twenty-fourpatientswereincluded,or70pairedblood sam-ples.Fivesampleswereexcludedduetohyperoxia,threeof themfromthesamepatient,whowereexcludedfromthe study.Patientcharacteristicsandsamplecollectiontimeare available(Table1).In 61samples(93.8%)the patientwas takennoradrenaline;in 26 samples(40%) thepatient was takenadrenaline; and in 15 samples(23.1%), the patient wastakendobutamine.
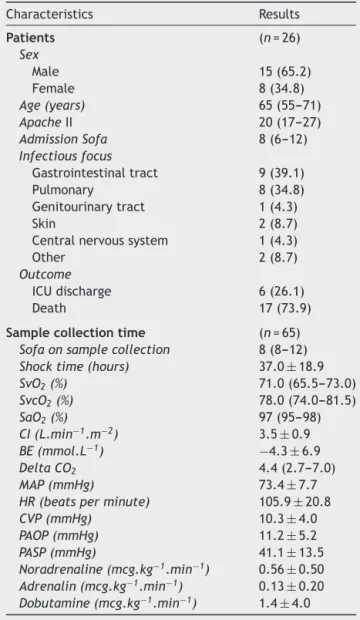
The Bland---Altman test in allpatients showed nogood agreementbetween SvO2 andSvcO2,with 7.35% biasand
LC 95%: −3.0% to 17.7% (Fig. 1). There was a moderate correlationbetweenthesevariables(r=0.72;p=0.0001).
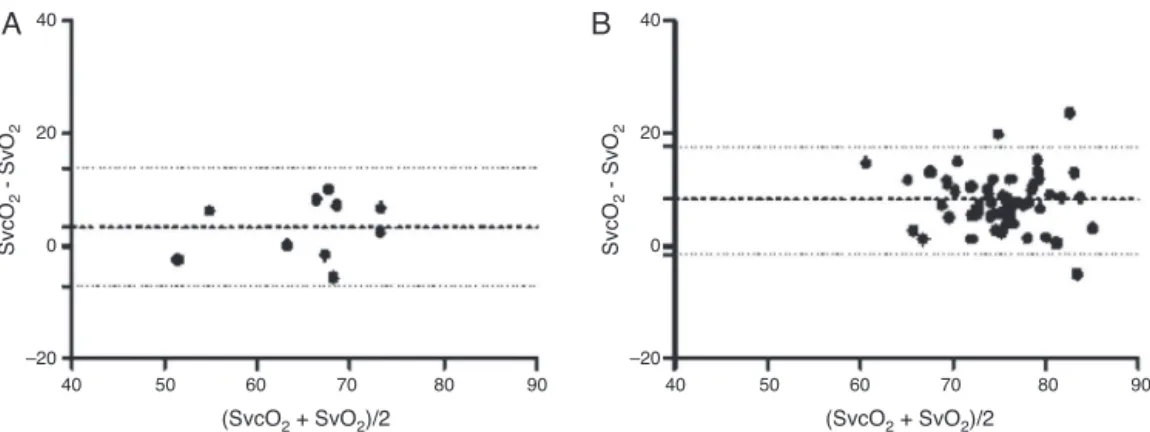
Only10samples(15.4%)metthehypoperfusioncriterion; thatis,thepresenceofnormalorlowSvO2and/orSvO2
asso-ciatedwithhyperlactatemia---inonlyfourofthesesituations both venous saturations were below the established lim-its.There was no good agreement amongthem because, although therewas a smallbias, the limitsof agreement werewide(3.15%,LC95%:−7.25%to13.76%)(Fig.2).
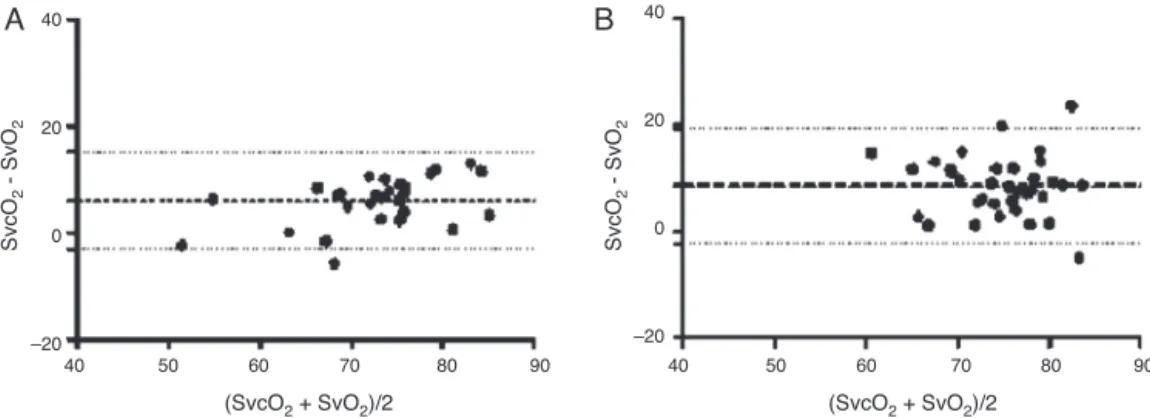
SvcO2<70% was found in only eight samples, whereas
SvO2<65%occurredin12ofthem.Bland---Altmantestalso
did not show good agreement between these variables inboth situations (Figs. 3and 4).There were 20samples (30.8%)withawideneddeltaCO2(>6mmHg)and29samples
(44.6%) withBE<−5.0mmol.L−1. The Bland---Altman
anal-ysis alsoshowed low agreement between SvO2 and SvcO2
Table1 Generalcharacteristicsofpatientsanddataatthe samplecollectiontime.
Characteristics Results
Patients (n=26)
Sex
Male 15(65.2)
Female 8(34.8)
Age(years) 65(55---71)
ApacheII 20(17---27)
AdmissionSofa 8(6---12)
Infectiousfocus
Gastrointestinaltract 9(39.1) Pulmonary 8(34.8) Genitourinarytract 1(4.3)
Skin 2(8.7)
Centralnervoussystem 1(4.3)
Other 2(8.7)
Outcome
ICUdischarge 6(26.1) Death 17(73.9)
Samplecollectiontime (n=65)
Sofaonsamplecollection 8(8---12)
Shocktime(hours) 37.0±18.9
SvO2(%) 71.0(65.5---73.0)
SvcO2(%) 78.0(74.0---81.5)
SaO2(%) 97(95---98)
CI(L.min−1.m−2) 3.5±0.9
BE(mmol.L−1) −4.3±6.9
DeltaCO2 4.4(2.7---7.0)
MAP(mmHg) 73.4±7.7
HR(beatsperminute) 105.9±20.8
CVP(mmHg) 10.3±4.0
PAOP(mmHg) 11.2±5.2
PASP(mmHg) 41.1±13.5
Noradrenaline(mcg.kg−1.min−1) 0.56±0.50
Adrenalin(mcg.kg−1.min−1) 0.13±0.20
Dobutamine(mcg.kg−1.min−1) 1.4±4.0
ApacheII,acutephysiologyandchronichealthevaluation;BE,
excessofbases;HR,heartrate;CI,cardiacindex;MAP,mean
arterialpressure; PAOP,pulmonary arteryocclusive pressure;
PASP,pulmonary arterysystolicpressure;CVP,central venous
pressure; SaO2, arterial oxygen saturation; Sofa, sequential
organfailureassessment;SvcO2,centralvenousoxygen
satura-tion;SvO2,mixedvenousoxygensaturation;ICU,intensivecare
unit.
Resultsarepresentedasnumber(percentage),mean±standard
deviationormedian25%---75%.
samples(44.6%).TheBland---Altmantestanalysisofgroups
with or without hyperlactatemia revealed inadequate
agreementbetweenmixedand centralvenous saturations
inbothsituations(Fig.5).
Regarding CI, 29 samples (44.6%) presented with high values, higher than 3.5L.min−1.m−2, with an inadequate
agreementbetween saturationsin both CI conditions.All subgroupanalysisresultsaresummarizedinTable2.
Regarding the clinical approachassessment, there was disagreement as to the need for intervention in nine situations (13.8%) when SvO2 or SvcO2 was informed to
the investigator, in addition to the other hemodynamic
40
20
0
–20
40 50 60 70 80 90
(SvcO2 + SvO2)/2
SvcO
2
- SvO
2
Figure1 Concordanceanalysisbetweencentralvenous
sat-uration(SvcO2)andmixedvenoussaturation(SvO2)inglobal
sample.Datashow 7.35%biasand95%limitsofagreementof 3.0%---17.7%.
and respiratory parameters. Considering SvcO2 as a gold
standardandapredictorornotfortreatment,thetreatment basedonSvO2wouldhave beenexcessivein sixsituations
becauseSvcO2wasalreadyimproved.Intwosituationsthe
presence of elevated SvcO2 would have led to a
reduc-tion of medication intake, which did not occur when the observerwasbasedonSvO2.Inasinglesituation(1.5%)the
patient wouldno longer betreated onthe basis of SvO2,
whentheapproachshouldhavebeenconsideredinviewof SvcO2<70%.
Discussion
InthisstudytherewasnogoodagreementbetweenSvcO2
andSvO2,regardless of thepresence orabsenceof tissue
hypoperfusion,characterizedbyhyperlactatemia,reduced venous saturation, metabolic acidosis withBE fall or CO2
delta ratio enlargement. Therewas disagreementin clin-ical management in a small, though clinically significant, portionofthecases(13.8%)whenusingaSvcO2<70%asgold
standard.
The use of venous saturation as a therapeutic target in criticallyill patientshasbeen the subjectofnumerous studies.InitialanalyzesbasedonSvO2obtainedthrough
pul-monaryarterycatheterfailedtodemonstratethat itsuse resulted inreducedmorbidity andmortality.15---17 However, the use of this parameter was delayed by these studies, whichmayhaveimpaired theabilitytocorrectlyevaluate itsvalidityasaresuscitationtarget.Basedoncurrent knowl-edgeweknowthatthehemodynamiccareandimprovement ofthesepatientsshouldbeperformedearly.18
Thefirststudytovalidatetheuseofvenoussaturations asatherapeutictargetwasconductedbyRiversetal.6This study wascriticized for several reasons, amongthem the findingofverylowlevelsofSvcO2nolongerreproducedin
othercaseseries,andamortalityrateinthecontrolgroup higherthaninotherstudies.Subsequently,another random-izedstudyshowedareductioninmortalitywiththestrategy described byRivers.19 Despitethesecontroversiesa SvcO
2
40
20
0
–20
A
B
40 50 60 70 80 90
(SvcO2 + SvO2)/2
SvcO
2
- SvO
2
40
20
0
–20
40 50 60 70 80 90
(SvcO2 + SvO2)/2
SvcO
2
- SvO
2
Figure2 Analysisofagreementbetweenmixed(SvO2)andcentral(SvO2)venoussaturationsinsubgroupsofSvcO2and/orSvO2
andlactatejointanalysis.(A)LowSvcO2and/orSvO2associatedwithhyperlactatemia.Bias:3.15%andLC95%:−7.25%to13.76%.
(B)SvcO2and/ornormalSvO2associatedwithhyperlactatemia.Bias:8.11%andLC95%:−1.6%to17.83%.
40
20
0
–20
A
B
40 50 60 70 80 90
(SvcO2 + SvO2)/2
SvcO
2
- SvO
2
40
20
0
–20
40 50 60 70 80 90
(SvcO2 + SvO2)/2
SvcO
2
- SvO
2
Figure3 Analysisofagreementbetweenmixed(SvO2)andcentral(SvO2)venoussaturationsinsubgroupsofSvcO2.(A)SvcO2<70%.
Bias:1.94%andLC95%:−10.43%to14.31%.(B)SvcO2≥70%.Bias:8.1%andLC95%:−1.18%to17.34%.
40
20
0
–20
A
B
40 50 60 70 80 90
(SvcO2 + SvO2)/2
SvcO
2
- SvO
2
40
20
0
–20
40 50 60 70 80 90
(SvcO2 + SvO2)/2
SvcO
2
- SvO
2
Figure4 Analysisofagreementbetweenmixed(SvO2)andcentral(SvO2)venoussaturationsinSvO2subgroups.(A)SvO2<65%.
Bias:8.83%andLC95%:−3.16%to20.82%.(B)SvO2≥65%.Bias:6.98%andLC95%:−2.93%to16.89%.
Recently, three randomized multicenter studies have shown nodifferencesin mortalityratebetween groupsof patients randomized to conventional treatment (no use of SvcO2) and the goal-guided therapy of Rivers et al.7---9
The limitations of these studies should be kept in mind, as all of them were conducted in high-quality centersin
richcountries,withrelativelylowmortalityrateincontrol groups. This makes it difficult to apply their results in countrieswith limited resources or inadequatequality of care.TheSvcO2meanvaluesatthetimeofrandomization
40
20
0
–20
A
B
40 50 60 70 80 90
(SvcO2 + SvO2)/2
SvcO
2
- SvO
2
40
20
0
–20
40 50 60 70 80 90
(SvcO2 + SvO2)/2
SvcO
2
- SvO
2
Figure5 Analysisof agreement between mixed(SvO2)and central(SvO2)venous saturations inlactate subgroups. (A)
Lac-tate≤28mg.dL−1. Bias: 6.04% and LC 95%: −3.07% to 15.14%. (B): lactate≤28mg.dL−1. Bias: 8.56% and LC 95%: −2.28% to
19.41%.
Table2 Agreementbetweencentralvenoussaturationand mixedvenoussaturationinthevarioussubgroups.
Subgroup Bias(%) 95%limitsof agreement(%)
Global 7.35 −3.00to17.70
Hypoperfusion
Yes 3.15 −7.25to13.76 No 8.11 −1.60to17.83
SvcO2
SvcO2<70% 1.94 −10.43to14.31
SvcO2≥70% 8.10 −1.18to17.34 SvO2
SvO2<65% 8.83 −3.16to20.82
SvO2≥65% 6.98 −2.93to16.89 DeltaCO2
DeltaCO2>6mmHg 7.19 −5.28to19.66
DeltaCO2≤6mmHg 7.43 −1.97to16.83 BE
BE<−5mmol.L−1 7.42 −2.74to17.6
BE≥−5mmol.L−1 5.85 −16.42to28.14 Lactate
Lactate>28mg.dL−1 6.04 −3.07to15.14
Lactate≤28mg.dL−1 8.56 −2.28to19.41 CI
CI≤3.5L.min−1.m−2 7.78 −1.41to16.97
CI>3.5L.min−1.m−2 7.00 −4.30to18.30
BE,baseexcess;CI,cardiacindex;SvcO2,centralvenousoxygen
saturation;SvO2,mixedvenousoxygensaturation.
Resultsarepresentedasnumber(percentage).
indicated that most patients were already adequately
resuscitated,possiblyduetovolumereplacementreceived
prior to randomization.7---9 Furthermore, it is not a study
comparing hemodynamic improvement in patients who persistwithlowsaturationafterinitialresuscitation.Thus, we remain without evidence of the best management in thesesituations:persistwithresuscitation orobservation. Finally,the studies hadtheir samples calculatedwiththe
estimation of mortality rates higher than those actually foundinthestudies.Noneofthestudiesshowedincreased adverseeventsingroupsundergoingEGDT.Thus,theSepsis SurvivalCampaigncontinuestoincludeamongtheoptions forhemodynamic improvementthemeasurementof SvcO2
or SvcO2 as variables that reflect the body supply and
consumptionofoxygen.Therefore,theobjectofourstudy continuestohaverelevanceforthesepatientsmonitoring.
Although pulmonary artery catheter has been poorly used for being more invasive and due to the difficult interpretation of hemodynamic data,in casesin which it isuseditwouldbeimportanttodefinewhatwouldbethe valuescorrespondingtoSvcO2previouslyvalidatedbyRivers
et al.6 In the guidelines of the Sepsis Survival Campaign, the cut-off pointof 65% isrecommended.18 However,this valuehaslittlesupportintheliterature.Ourresultsarein linewithseveralstudiesshowingpooragreementbetween SvcO2andSvO2.20---22However,itwouldbemoreappropriate
to evaluate these possible differences in patients with signsofhypoperfusion,asitisinthisclinicalsituationthat SvcO2 improvement or non-improvement has relevance.
In our study, agreement between venous saturations is alsoinadequateinhypoperfusionsituations,withlimitsof agreement.
Other authors have suggested a worse agreement between SvcO2 and SvO2 when SvcO2 <60%.22 It is known
thatcirculatoryfailureintheearlystagesofsepsisisrelated tohypovolemia,myocardialpressure,hypercatabolicstate, and abnormal vasoregulation, with a pathological oxygen supplydependencyinthisperiod.Intheory,thepresenceof splanchnichypoperfusionwouldmakeSvcO2andSvO2more
divergentduetoanincreaseintherateofoxygen extrac-tionbytheviscera,measurableinthebloodreturningtothe heartviatheinferiorvenacavaandnotviathesuperiorvena cava. In ourstudy,therewas nodifferencebetween sub-groupsevaluatedaccordingtovenousoxygensaturation.It wasnotpossibletoidentifyarelationshippatternbetween SvcO2andSvO2inanyofthesubgroupswithsignsof
hypo-perfusion.Onehypothesisforourfindingswouldbethefact that abdominal splanchnic hypoperfusion is not primarily responsibleforthereductionofSvO2.Itisbelievedthatthe
main component responsible for a lowerSvO2 value
sinus.20 Thus,thisreductioncouldbetheresultofcardiac outputimpairmentandnotnecessarilyofincreasedvisceral consumption. In myocardial depression low oxygen con-sumptioncouldleadtoarelativeincreaseinSvO2,narrowing
its relationship with SvcO2. However, it was not possible
todemonstrate agreementdifferences in thesubgroup of patients with high or low cardiac output. This analysis is limited both by the fact that therewere nosituations in ourgroupin whichcardiac indexwasreducedinabsolute numbers(below2.5L.min−1.m−2)andbythedifficult
inter-pretationofthecardiacoutputadequacytothebodyneed. Theclinicalagreementanalysisdemonstrateda manage-mentdisagreementin13.8%ofcases,suggestingthattheuse oftheproposed65%limitforSvO2couldtriggertreatment
for hemodynamic parametersupranormalization,although itwasnotpossibletodemonstratethisclearly.Itisknown thathypertreatmentisassociatedwithincreasedmorbidity andmortalitywithexcessiveuseoffluids,dobutamine,and bloodtransfusioninanattempttoincreasecardiacoutput.23 Althoughtherehavebeenfewcasesofinadequate manage-ment in our study,on an individual level thiscould bring harmtothatparticularpatient.
The present study has some strength points. We ana-lyzed a relevant group of patients with septic shock, in whichmanagementstandardizationisnecessaryto eventu-allyreducemorbidity andmortality.We soughttomake a detailedanalysis ofthe perfusional statusand create dif-ferent forms of evaluation based on different laboratory profiles.Inaddition,theanalysiswasnotrestrictedto statis-ticalproceduresofcorrelationandconcordanceevaluation, butrathertotheimpactofusingSvO2or SvcO2inclinical
practice.
This study also hasa number of limitations. First, the smallsamplesizeresultedinalimitednumberofsituations in each of the subgroups evaluated for perfusion status. Second, the patients wereno longer in the first hoursof resuscitation,whichmaylimitthefindingsapplicationinthis clinicalsetting.Inaddition,asaresultofthisinclusion win-dow,most patientswerealready adequatelyresuscitated, whichrestrictedthenumberofpatientsinastateof hypo-perfusion.Third,morethanonesamplewascollectedfrom each patient,whichmay havegenerated biasin interpre-tingtherelationshipsbetweenvenous saturations.Finally, theevaluationofisolatedmeasures,ratherthanthevenous saturationbehaviorinresponsetointerventions,also consti-tutesalimitationinthedefinitionofclinicalbehavior,even ifminimized by thefact thatthe observerhas takeninto accountotherperfusionvariables.
Inconclusion,thisstudyshowedthatalthoughthereisa moderatecorrelationbetween SvO2andSvcO2,the
agree-ment betweenthem is inadequate.It wasnotpossible to demonstratethatthepresenceofhypoperfusionaltersthe agreement between SvO2 and SvcO2. In addition, theuse
of SvO2 instead of SvcO2 may lead to changes in clinical
management in a small but clinically relevant portion of patients
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.Friedman G,SilvaE, VincentJL. Hasthemortalityofseptic shockchangedwithtime?CritCareMed.1998;26:2078---86. 2.Angus DC,Linde-ZwirbleWT,Lidicker J,et al. Epidemiology
of severe sepsis in the United States: analysis of inci-dence,outcome,andassociatedcostsofcare.CritCareMed. 2001;29:1303---10.
3.MartinGS, ManninoDM, EatonS, etal. Theepidemiologyof sepsisintheUnitedStatesfrom 1979through 2000.NEnglJ Med.2003;348:1546---54.
4.Linde-ZwirbleWT,AngusDC.Severesepsisepidemiology: samp-ling,selection,andsociety.CritCare.2004;8:222---6.
5.DombrovskiyVY,MartinAA,SunderramJ,etal.Rapidincrease inhospitalizationand mortalityratesforseveresepsisinthe UnitedStates:a trendanalysisfrom1993 to2003.Crit Care Med.2007;35:1244---50.
6.RiversE,NguyenB,HavstadS,etal.Earlygoal-directedtherapy inthetreatmentofseveresepsisandsepticshock.NEnglJMed. 2001;345:1368---77.
7.InvestigatorsProCESS,YealyDM,KellumJA,etal.Arandomized trialofprotocol-basedcareforearlysepticshock.NEnglJMed. 2014;370:1683---93.
8.TheARISE InvestigatorsandtheANZICSClinicalTrialsGroup. Goal-directedresuscitationforpatientswithearlysepticshock. NEnglJMed.2014;371:1496---506.
9.MounceyPR,OsbornTM,PowerGS,etal.Protocolised Manage-mentInSepsis(ProMISe):amulticentrerandomisedcontrolled trialoftheclinicaleffectivenessandcost-effectivenessofearly, goal-directed, protocolised resuscitationfor emergingseptic shock.NEnglJMed.2015;372:1301---11.
10.Phua J, Koh Y, DuB, et al. Managementof severesepsis in patients admittedto Asian intensive care units: prospective cohortstudy.BMJ.2011;342:d3245.
11.BealeR, ReinhartK, BrunkhorstFM, etal. Promoting Global ResearchExcellenceinSevereSepsis(PROGRESS):lessonsfrom aninternationalsepsisregistry.Infection.2009;37:222---32. 12.http://www.survivingsepsis.org/Bundles/Pages/default.aspx 13.Marx G, Reinhart K. Venous oximetry. Curr Opin Crit Care.
2006;12:263---8.
14.American College of Chest Physicians/Society of Critical CareMedicineConsensusConferenceCommittee.ACCP/SCCM ConsensusConference:definitionsforsepsisandorganfailure andguidelinesfortheuseofinnovativetherapiesinsepse.Crit CareMed.1992;20:864---74.
15.RichardC,WarszawskiJ,AnguelN,etal.Earlyuseofthe pul-monaryarterycatheterandoutcomesinpatientswithshockand acuterespiratorydistresssyndrome:arandomizedcontrolled trial.JAMA.2003;290:2713---20.
16.WheelerAP,BernardGR,ThompsonBT,etal.,AcuteRespiratory DistressSyndrome(ARDS)ClinicalTrialsNetwork. Pulmonary-arteryversus central venouscatheter toguide treatmentof acutelunginjury.NEnglJMed.2006;354:2213---24.
17.Harvey S, Harrison DA, Singer M, et al., PAC-Man study collaboration. Assessment of the clinical effectiveness of pulmonaryarterycathetersinmanagementofpatientsin inten-sive care (PAC-Man): a randomizedcontrolled trial. Lancet. 2005;366:472---7.
18.DellingerRP,LevyMM,RhodesA,etal.SurvivingSepsis Cam-paign:internationalguidelinesformanagementofseveresepsis andsepticshock:2012.CritCareMed.2013;41:580---637. 19.EarlyGoal-Directed Therapy CollaborativeGroup ofZhejiang
20.Chawla LS, Zia H, Gutierrez G, et al. Lack of equivalence betweencentraland mixedvenousoxygensaturation.Chest. 2004;126:1891---6.
21.VarpulaM,KarlssonS,RuokonenE,etal.Mixedvenousoxygen saturationcannotbeestimatedbycentralvenousoxygen satu-rationinsepticshock.IntensiveCareMed.2006;32:1336---43.
22.VanBeestPA,vanIngenJ,BoermaEC,etal.Noagreementof mixedvenousandcentralvenoussaturationinsepsis, indepen-dentofsepsisorigin.CritCare.2010;14:R219.