www.bjorl.org
Brazilian
Journal
of
OTORHINOLARYNGOLOGY
ORIGINAL
ARTICLE
Tracheostomy
in
children:
a
ten-year
experience
from
a
tertiary
center
in
southern
Brazil
夽
,
夽夽
Cláudia
Schweiger
a,∗,
Denise
Manica
a,
Carolina
Fischer
Becker
a,
Larissa
Santos
Perez
Abreu
a,
Michelle
Manzini
a,
Leo
Sekine
b,
Gabriel
Kuhl
a,caHospitaldeClínicasdePortoAlegre,Servic¸odeOtorrinolaringologia,PortoAlegre,RS,Brazil
bUniversidadeFederaldoRioGrandedoSul(UFRGS),ProgramadePós-graduac¸ãoemEpidemiologia,PortoAlegre,RS,Brazil cUniversidadeFederaldoRioGrandedoSul(UFRGS),DepartamentodeOftalmologiaeOtorrinolaringologia,PortoAlegre,RS,
Brazil
Received27May2016;accepted10August2016 Availableonline24August2016
KEYWORDS
Tracheostomy; Child;
Epidemiology
Abstract
Introduction:Childrenmayrequiretracheostomyduetomanydifferenthealthconditions.Over thelast40years,indicationsoftracheostomyhaveendorsedsubstantialmodifications.
Objective: ToevaluatepediatricpatientswarrantedtracheostomyatourHospital,inregardto theirindications,associatedcomorbidities,complicationsanddecannulationrates.
Methods:Retrospective study concerning patients under 18 years of age undergoing tra-cheostomyinatertiaryhealthcarecenter,fromJanuary2006toNovember2015.
Results:123childrenrequiredatracheostomyafterENTevaluationduringthestudyperiod. Aproportionof63%wasmale,and56%wasunderoneyearofage.Glossoptosiswasthemost commonindication(30%),followedbysubglotticstenosis(16%)andpharyngomalacia(11%).The mortalityratewas31%.Bytheendofthisreview,35children(28.4%)hadbeendecannulated, andthefewerthenumberofcomorbidities,thegreaterthedecannulationrate(0.77±0.84vs. 1.7±1.00comorbidities;p<0.001).
Conclusion: Tracheostomyinchildrenisarelativelyfrequent procedureatourhospital.The mostcommonindicationsareglossoptosisandsubglotticstenosis.A highmortalityratewas found,potentiallysubstantiatedbythehighnumberofcriticalcarepatientswithchronic neu-rologicalconditionsinthiscohort.Ourdecannulationrateisslightlybelowotherseries,probably becauseofthegreateramountofpatientswithcomorbidities.
© 2016 Associac¸˜ao Brasileira de Otorrinolaringologia e Cirurgia C´ervico-Facial. Published by Elsevier Editora Ltda. This is an open access article under the CC BY license (http:// creativecommons.org/licenses/by/4.0/).
夽 Pleasecitethisarticleas:SchweigerC,ManicaD,BeckerCF,AbreuLS,ManziniM,SekineL,etal.Tracheostomyinchildren:aten-year
experiencefromatertiarycenterinsouthernBrazil.BrazJOtorhinolaryngol.2017;83:627---32.
夽夽ThisstudywasperformedintheOtolaryngologyUnitofHospitaldeClínicasdePortoAlegre.
∗Correspondingauthor.
E-mail:causch@hotmail.com(C.Schweiger).
PeerReviewundertheresponsibilityofAssociac¸ãoBrasileiradeOtorrinolaringologiaeCirurgiaCérvico-Facial.
http://dx.doi.org/10.1016/j.bjorl.2016.08.002
PALAVRAS-CHAVE
Traqueostomia; Crianc¸a; Epidemiologia
Traqueostomiaemcrianc¸as:umaexperiênciadedezanosemumcentroterciáriodo
suldoBrasil
Resumo
Introduc¸ão:Ascrianc¸aspodemnecessitardetraqueostomiadevidoadiferentesproblemasde saúde.Aolongodosúltimos40anos,asindicac¸õesdetraqueostomiapassarampormudanc¸as substanciais.
Objetivo:Avaliar pacientes pediátricos com traqueostomia no nosso Hospital, no que diz respeitoàssuasindicac¸ões,comorbidadesassociadas,complicac¸õesetaxasdedecanulac¸ão.
Método: Estudo retrospectivo de pacientescom menos de 18 anos de idade submetidos a traqueostomiaemumcentrodesaúdeterciário,dejaneirode2006anovembrode2015.
Resultados: 123crianc¸asprecisaramdeumatraqueostomiaapósavaliac¸ão otorrinolaringológ-icaduranteoperíododoestudo.Dototal,63%eradosexomasculinoe56%menoresdeum ano.Glossoptosefoiaindicac¸ãomaiscomum(30%),seguidaporestenosesubglótica(16%)e faringomalácia(11%).A taxademortalidadefoide31%.Atéofimdesteartigo,35crianc¸as (28,4%)haviamsidodecanuladasequantomenoronúmerodecomorbidades,maiorfoiataxa dedecanulac¸ão(0,77±0,84vs.1,7±1,00comorbidades;p<0,001).
Conclusão:A traqueostomia em crianc¸as é um procedimento relativamente frequente em nossohospital. Asindicac¸ões maiscomunssão glossoptosee estenosesubglótica. Uma alta taxa de mortalidade foi encontrada, potencialmente comprovada peloelevado número de pacientescríticoscomcondic¸õesneurológicascrônicasnessacoorte.Nossataxadedecanulac¸ão estáligeiramenteabaixodeoutrasséries,provavelmenteporcausadamaiorquantidadede pacientescomcomorbidades.
© 2016 Associac¸˜ao Brasileira de Otorrinolaringologia e Cirurgia C´ervico-Facial. Publicado por Elsevier Editora Ltda. Este ´e um artigo Open Access sob uma licenc¸a CC BY (http:// creativecommons.org/licenses/by/4.0/).
Introduction
Tracheostomyisoneoftheoldestandmostcommonly per-formed surgical procedures among critically ill patients. Children require tracheostomy for many different rea-sons,andthosewithachronictracheostomyconstitutean importantsubgroup ofchildren whoareat risk forairway compromise.
Althoughalifesavingsurgery,tracheostomyinchildren ismorechallenging whencomparedtothoseperformedin adults,anditis associatedwithhigher ratesof morbidity andmortality.Overmore,theriskofcomplicationsincreases withageamongpediatricpatients.1,2
Over the last 40 years,there has been a transition in tracheostomyindications.During1970s,themainindication oftracheostomywasupperairwayobstructionsecondaryto anacuteinflammatorydiseasesuchasepiglottitis,croupor laringotracheitis.2Withtheintroductionofvaccinesagainst Haemophilus influenzae and Corynebacterium diphteriae andtheadoptionofroutineuseofendotrachealintubation asan alternative totracheostomy, therewasa declinein suchindications.
Ontheotherhand,theimprovementofsupportcareand therapeuticsinprematureinfantsandchildrenwith congen-italanomaliesincreasedthesurvivalratesofthesechildren, which often required protracted periods of endotracheal intubationandmechanicalventilation.Childrenwith endo-tracheal intubation may need mechanical ventilation for conditionssuch as pulmonary and cardiac malformations, chronicpulmonaryinsufficiency,neurologicaldisordersand
cervical trauma. In the other hand, craniofacial malfor-mations andanatomical/functional changesofthe larynx, suchassubglotticstenosis,tracheomalaciaandtumors,are amongtheobstructivecauses.3
A recent study from a Scotland tertiary center3 found long-term ventilation as the main indication for tra-cheostomy in their series of 111 children and cited some articlesfromUnitedKingdomhospitalswithsimilarfindings. However, a study in New Zealand4 included 122 patients undergoing tracheostomies between 1987 and 2003 and found that the obstruction of upper airway wasthe indi-cation in70% of thepatients.More recently,an American studypublishedinMarch,2013,5whichrevieweddatafrom 158patients,raisedthehypothesisthatindicationsof tra-cheotomy would be changing again, with a reduction of indications for prolonged endotracheal intubation and an increase inthe groupof craniofacialanomalies andupper airwayobstruction.
Thus,ourobjectiveistoevaluatechildrenwhowarranted tracheostomyatourHospital,inregardtotheirindications, associatedcomorbidities,complicationsanddecannulation rates.
Methods
0 0-2 months
2-4 months
4-6 months
6-8 months
8-10 months
10-12 months
12-24 months
24-36 months
36-48 months
48-60 months
5-8 years
8-12 years
12-15 years
15-18 years 5
10 12
33
14
3
5 5
2 9
2 9
7
8 8
6 15
20 25
Numbers of patients
30 35
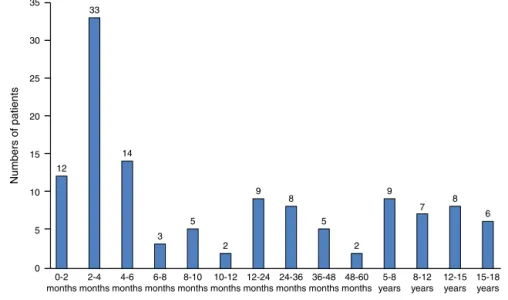
Figure1 Distributionofpatientsinregardtotheirage.
Patients’ fileswere reviewed withrespect to the follow-ing variables: demographics,comorbidities, indication for procedure,complicationsrelatedtothetracheostomyand decannulation.
Surgeries were performed by resident doctors under consultant supervision. All patients were under general anesthesiaduringprocedureandwereadmittedtothe pedi-atricintensivecareunitaftersurgery.Astandardprocedure techniquewasapplied,withhorizontalskin incisionanda verticalincisionin thetrachea.Two parallelsutures were placedoneachsideofthetrachealincision.Thesuturesin thetracheawereremovedoneweeklater.
TheprotocolofthestudywasapprovedbytheResearch andEthicsCommitteeofourHospital(n◦14-0650).
Data are shown in median (interquartile range) or mean±StandardDeviation.Mann---WhitneyUtestwasused forstatisticalanalysiswhenappropriate.
Results
Patientdemographics
Between January 2006 and November 2015, 146 chil-dren evaluatedby the ENTUnit required atracheostomy. Datawasavailable from123patients.Seventy-eight(63%) patients were male. Almost half of them had their tra-cheostomyperformedundersixmonthsofage(48%)and69 patients(56%)wereunderoneyearofageatthetimeofthe procedure.Themedianageoftracheostomywas7months, withagerangingfrom8daysto17years(Fig.1).
A median of 12 (interquartile range: 10---14.25) tra-cheostomies was performed each year. The number of proceduresperyearremainedstableoverthestudyperiod (Fig.2).
Indications
Glossoptosis wasthe most common indication (30%), fol-lowed by subglottic stenosis (16%) and pharyngomalacia
0
2006 2007 2008 2009 2010 2011 2012 2015
(jan-nov) 2014 2013 2
4 6 8 10 12
Number of tr
acheostomies
14 16
18 18
7 13
11 11
14 14
15
10 10
Figure2 Numberoftracheostomiesperformedperyear.
(11%). Other causes included laryngomalacia, prolonged intubation,acute lesionsof the larynxleading to extuba-tionfailure, vocal foldpalsy andlaryngeal papillomatosis (Table1).Somechildrenhadmorethanoneindicationfor tracheostomy.
Upper airway obstruction was the indication for tra-cheostomyin102patients(83%),concerningdisorderslike glossoptosis, subglottic and glottic stenosis, pharyngoma-lacia, laryngomalacia, vocal fold palsy, acute lesions of the larynx leading to extubation failure (post-intubation laryngitis), craniofacial abnormalities and airway tumors. Pulmonarytoilet,intubationfailureandlong-term ventila-tionwerenon-obstructivecausesfortracheostomy.
Twenty-onepatients(17%)hadtheirtracheostomyplaced aftersurgical failure.Supraglottoplastywasnotsuccessful in five patients, and osteomandibular distraction as well asresectionofpapillomatosislesionscouldnotrevertthe obstructioninfourpatientseachone(Table2).
Comorbidities
Table1 Indicationsfortracheostomy.
Indications N◦ofpatients(%)
Glossoptosis 37(30)
Subglotticstenosis 20(16)
Pharyngomalacia 14(11)
Prolongedventilation 13(10)
Laryngomalacia 13(10)
Acutelesionsofthelarynxleading toextubationfailure
10(8)
Vocalfoldpalsy 5(4)
Intubationfailure 5(4)
Laryngealpapillomatosis 4(3)
Glotticstenosis 4(3)
Maxillaryhipoplasia 4(3)
Linfangioma 2(1)
Mucopolissacaridosis 1(0.8)
Hemangioma 1(0.8)
Laryngealcleft 1(0.8)
Laryngitis 1(0.8)
Pulmonarytoilet 1(0.8)
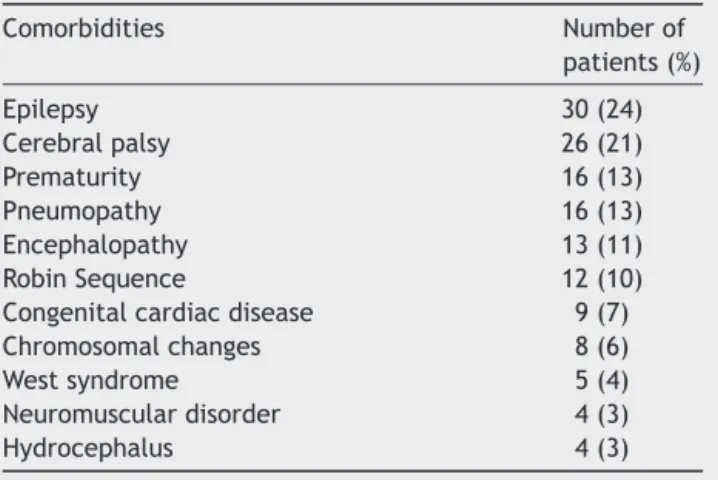
morecomorbidities.Only20patientshadnoparallelhealth conditions.
Nearly41% presented neurological conditions(cerebral palsy, encephalopathy, epilepsy, neuromuscular disorders) and27patientshadsomesyndromicdisorderthatincluded Treacher-Collins syndromeand Downsyndrome. The main comorbiditiespresented by the 103 children in the series arelisted onTable 3. Besides neurological andsyndromic conditions,comorbiditiesalsoincludedprematurity,cardiac congenitaldiseaseandlungdisease.
Complications
Complications were divided into perioperative, and early and late postoperative (Table 4). Perioperative complications were definedas thoseoccurring during the surgical procedure or immediately after. Those occurring duringthefirstpostoperativeweek wereconsidered early complications, and late complications were defined as thoseoccurringafterthefirstweek.
Perioperative complications occurred in ten children (8.1%) and included six cases of pneumothorax, three patients with subcutaneous emphysema and two children
Table2 Tracheostomyaftersurgicalfailure.
Surgicalprocedure Numberof
patients(%)
Supraglotoplasty 5(4)
Osteomandibulardistraction 4(3)
Excisionofpapillomatosis 4(3)
BalloondilatationforSGS 4(3)
Laryngotracheoplasty 1(0.8)
Uvulopalatoplasty 1(0.8)
LaserprocedureforSGS 1(0.8)
Treatmentofairwayacutelesions 1(0.8)
Table3 Comorbiditiesfoundinthisseries.
Comorbidities Numberof
patients(%)
Epilepsy 30(24)
Cerebralpalsy 26(21)
Prematurity 16(13)
Pneumopathy 16(13)
Encephalopathy 13(11)
RobinSequence 12(10)
Congenitalcardiacdisease 9(7)
Chromosomalchanges 8(6)
Westsyndrome 5(4)
Neuromusculardisorder 4(3)
Hydrocephalus 4(3)
withpneumomediastium. Therewasnoepisode of signifi-cantbleeding.Onedeathoccurredduringtheprocedure,in achildwithOtopalatodigitalsyndrome.Thecauseofdeath wasimpossibilityofventilationduetopulmonaryproblems. Earlypostoperativebleeding,accidentaldecannulation, woundinfectionandfalsetractofthecannulaoccurredin sevenpatients.
Latepostoperativecomplicationsoccurredin38patients (31%).Twenty-threepatientspresentedwithstomaland/or supra-stomal granulomas adjacent to the tracheostomy. Some of the granulomas were excised and others were treatedwithchemicalablation.Cannulaobstructionbyplug ofsecretion,lateaccidentaldecannulation,papillomatosis extensiontothetracheaandtrachealstenosisalsooccurred.
Lengthoftracheostomystayanddecannulation
Timebetweentracheostomyanddecannulationrangedfrom less thanonemonth to7years(median of5 months).Six patients requiredsurgical closureof thetracheostomy. By
Table4 Complications.
Complications N◦ofpatients(%)a
Perioperative 10(8) Pneumothorax 6 Subcutaneousemphysema 3 Pneumomediastinum 2
Death 1
Earlypostoperative 7(6) Falsetractofthecannula 4 Accidentaldecannulation 3 Woundinfection 2 Latepostoperative 38(31) Stomaland/orsupra-stomal
granulomas
23
Accidentaldecannulation 7 Cannulaobstruction 5 Papillomatosisextensionto
thetrachea
2
Trachealstenosis 2
45
40
35
75%
25%
No comorbidity One comorbidities Two comorbidities Three or more comorbidities 27%
73%
11% 89%
10% 90% 30
25
Number of patients
20
15
10
5
0
Decannulated Not decannulated
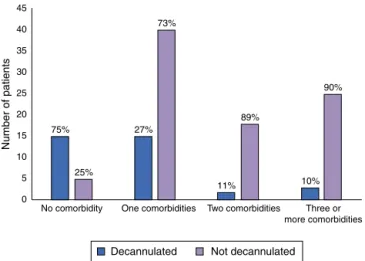
Figure3 Associationbetween thenumberofcomorbidities anddecannulationrates.
theendofthisreview,35childrenfromthiscohorthadbeen decannulated(28%).
The decannulation protocol of our institution includes cannula downsizing and its occlusion after specific treat-ment of the airway pathology. A laryngoscopy is always performedpriortothecannuladownsizing,inorderto con-firmthepatencyoftheairway.
Themajorityofdecannulatedchildrenhadno comorbidi-tiesoronlyonecomorbidity,correspondingto86%ofcases. Subglotticstenosiswasthemainindicationoftracheostomy inthedecannulatedchildren(15patients).
Analyzing the association between comorbidities and decannulationrates,onecannoticethatthefewerthe num-ber ofcomorbidities, the greater thedecannulation rates (0.77±0.84 comorbidities vs. 1.7±1.00 comorbidities in decannulatedvs.non-decannulatedpatients,respectively; p<0.001).DataareshowninFig.3.
Mortality
Thirty-eight (31%) children died during study period, and sepsis wasthecause infourteen. Acuterespiratory insuf-ficiencycausedthedeathineightchildren;pneumoniaand clinical complications in another 11 patients. There were apparentlynodeathscausedbyaccidentaldecannulationor cannulaobstruction.However,wewereunabletoidentifya deathcauseinsixchildren.
Discussion
Incomparisonwithadultpopulation,whereindicationsseem toremain thesame overthe years,studies recentlyhave shownahistoricaltransitioninindicationsfortracheostomy in children.In developedcountries,acute epiglottitisand laryngotracheobronchitisnolongerrepresentanindication fortracheostomy,duetotheuseoftheendotracheal intu-bationinthesecases,besidesHaemophilusinfluenzatype Bvaccineforepiglottitis.3Inthiscohort,onlyonechildstill had a tracheostomy for acute inflammation of the upper airway(lupuslaryngitis).
The commonest indications for pediatric tracheostomy are prolonged ventilation studies and obstruction of the
upperairway.Inarecentstudywith111childrenpublished by a Scotlandtertiary center,3 32% of patients had their tracheostomyindicatedforlong-termventilation,followed by craniofacial abnormality causing airway obstruction in 18%ofchildrenandsubglottic stenosisin 14%.Their num-bers are similar to those of United Kingdom hospitals.6,7 Douglas et al. attributed this to the elevated number of patientswithsignificant medicallyproblemssurvivinglong term,asaresultoftheimprovementinneonatalintensive care.
Inourseriesofpatients,themostcommonindicationof tracheostomywasupperairwayobstruction,causedby cra-niofacialabnormalitiesandsubglotticstenosis.Themajority of the obstructive causes were glossoptosis, with Robin Sequencefiguringinfirstplaceamongourpatients.
Owzen et al.1 from Turkey and Mahadevan et al.4 from New Zealand also reported that airway obstruction accountedforthemajorityofindicationsoftracheostomy. InOwzen’sseriesof282patients,airwayobstructionmade up72%ofindications.Mahadevanpresentedalargerseries, andalsoshowedthat 70%of the tracheostomiesoccurred becauseofairwayobstruction.
Syndromic patients representeda large numberof our tracheostomizedchildren.Theobstructionusuallyfoundin theseconditions can be associated to craniofacial abnor-malitiesleading toanatomical or functional obstructions, aswellasahypotonicstatus.Anatomicalobstructionscan be seen on imaging examination or rigid laryngotracheal endoscopicevaluation,but functionaldisordersarebetter evaluatedbyflexibleendoscopyoftheairway.Inour hospi-tal,allpediatricpatientswithairwayobstructionsuspicion areevaluatedbyrigidandflexibleairwayendoscopy,which allowus todiagnose conditionsasglossoptosis, pharyngo-malaciaandtracheomalacia.
Ourhospital is a referencecenter in the treatment of PierreRobinSyndromepatients,andthatcouldexplainthe increasednumberofglossoptosisfoundinourpopulation.
Regardingthe16%ofsubglotticstenosisasindicationfor tracheostomy,wehavebeenwitnessingachangeonrecent years,aftertheimplementationofballoondilationfor sub-glotticacutelesions.Recently,thegreatmajorityofchildren evaluatedbecause of acute subglottic obstructive lesions aresubmittedtoendoscopicballoondilation,withexcellent resultsandavoidanceoftracheostomy.Since2009,withthe introduction of balloon dilation, only fourtracheostomies wereperformedbecauseofsubglotticstenosis.
Thirteen patients were tracheostomized because of laryngomalacia.Allofthemhadcomorbiditiesand85%had neurologicaldisorders.Besideslaryngomalacia,allpatients hadparallelindications fortracheostomy,likeglossoptosis andpharyngomalacia.
Four patients required tracheostomy for obstructive recurrent papillomatosis lesions even after cidofovir and bevacizumab therapies, and two presented with tracheal extensionasacomplicationofthetracheostomy.This real-ityis supposedtochangeaftertheimplementationofthe HPVvaccineandcontinuouseducationonprenatalcare.
Analysisofthedemographiccharacteristicsofpatientsin theliteraturerevealedthatthemajorityoftracheostomies were performed in children under one year of age.2,8,9 Ourseriesshowedthesametrend.Thiscouldbeprobably explainedbytheincreasingsurvivalratesamongpremature andsyndromicpatientsandthehigherseverityof obstruc-tiveproblemsatthisage.10
Thetracheostomy-relatedcomplicationsratesinthe lit-erature are around 40%, with numbers ranging from 18% to 56%3,5,11,12 The most common complications are pneu-mothorax, pneumomediastium, stomal and supra-stomal granulomas,cannulaobstruction,falsetractandaccidental decannulation.
In our series, perioperative and early postoperative complicationsrates were low,but stillsignificant (8%and 6%,respectively).Theseratesshowthatthetracheostomy isnotaproceduretobeunderestimatedaboutitsrisksand complications.
Pneumothorax was the most common perioperative complication,andfalsetractwasthemost commonearly postoperativecomplication.On theother hand,late post-operative complications were higher than reported in literature,withthe developmentof stomal and/or supra-stomal granulomas in 23 children. It could probably be explainedbythevariety ofcannulabrands used.Besides, some complications are secondary to poor education on tracheostomy care and low socio-economical conditions, leadingtoaccidentaldecannulationsandcannula obstruc-tion.
Decannulation is always the objective of surgeons and families,butthisisnotalwayspossible.Studiesshowthat the decannulation rates vary around 35---75%,1---6 and the highestratesarefoundinstudieswithhigherprevalenceof airwayobstructionwarrantedtracheostomies.Studieswith lowerratesofdecannulationareusuallythosewithahigher numberof neurologicallycompromisedpatients, asinour series.
Ofourdecannulatedpatients,41%hadsubglottic steno-sis and 44% had no comorbidities. This elevated rate of decannulation in children with subglottic stenosis can be explainedbytheuseofballoon dilationsinacute subglot-ticlesionsand successfulopen technique surgeriesin the recentyears.Only16%ofthetracheostomizedpatientswere otherwise healthy (no comorbidities or craniofacial mal-formations) and most of them were decannulated. Robin Sequence, with obstructive glossoptosis and neurological disorderpatientsrepresentarelevantportionofstill non-decannulatedpatients.
The mortality rate of tracheostomized patients is rel-atively high, between 14 and 19%. In our series, it represented 32% of the tracheostomized children. How-ever, most of these deaths were related to underlying comorbiditiesofthesepatientsandnotdirectlytothe pres-enceofthetracheostomy.2,4,11,13,14Theelevatednumberof
critical patients with chronic neurological conditions can alsoexplainourincreasedmortalityrate.Thereweresome deathsathomewithnoidentifiablecause.
Conclusion
Tracheostomyinchildrenisarelativelyfrequentprocedure atourhospital.Thecommonestindicationsareglossoptosis and subglottic stenosis. Our decannulation rateis slightly below other series, probably because of the increased amount of patients withcomorbidities. The perioperative complicationrateislowcomparedtotheliterature.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.Özmen S, Özmen Ö. Pediatric tracheostomies: a 37-year experience in 282 children. Int J Pediatr Otorhinolaryngol. 2009;73:959---61.
2.Annette HC. Pediatric tracheostomies in an Asian Popula-tion:theSingaporeexperience.OtolaryngolHeadNeckSurg. 2005;133:246---50.
3.DouglasCM, Poole-CowleyJ, MorrisseyS, KubbaH, Clement WA,WynneD.Paediatrictracheostomy---a11yearexperience ataScottishpaediatrictertiaryreferralcentre.IntJPediatr Otorhinolaryngol.2015;79:1673---6.
4.MahadevanM,BarberC.Pediatrictracheotomy:17yearreview. IntJPediatrOtorhinolaryngol.2007;71:1829---35.
5.LawrasonA,KavanaghK.Pediatrictracheotomy:areindications changing.IntJPediatrOtorhinolaryngol.2013;77:922---5. 6.CorberttHJ,MannKS,MitraI,JesudasonEC,LostyPD,Clarke
RW.Tracheostomy---ayearexperiencefromaUKpediatric sur-gicalcenter.JPedSurg.2007;42:1251---4.
7.HadfieldPJ,Lloyd-FaulconbridgeRV,AlmeydaJ,AlbertDM, Bai-leyCM.Thechangingindicationsforpaediatrictracheostomy. IntJPediatrOtorhinolaryngol.2003;67:7---10.
8.ButnaruCS,ColreavyMP.Tracheostomyinchildren:evolution inindications.IntJPediatrOtorhinolaryngol.2006;70:115---9. 9.LewisCW,CarronJD.Tracheotomyinpediatricpatients.Arch
OtolaryngolHeadNeckSurg.2003;129:523---9.
10.LiuC,HeffernanC.Indications,hospitalcourse,andcomplexity ofpatientsundergoingtracheostomyatatertiarycarepediatric hospital.OtolaryngolHeadNeckSurg.2014;151:232---9. 11.CarronJD,DerkayCS.Pediatrictracheostomies:changing
indi-cationsandoutcomes.Laryngoscope.2000;110:1099---104. 12.KremerB,Botos-KremerAI.Indications,complications,and
sur-gicaltechniquesfor pediatrictracheostomies---anupdate.J PediatrSurg.2002;37:1556---62.
13.Itamoto CH, Lima BT. Indications and complications of tracheostomy in children. Braz J Otorhinolaryngol. 2010;76:326---31.