rev bras ortop.2016;51(3):370–373
SOCIEDADE BRASILEIRA DE ORTOPEDIA E TRAUMATOLOGIA
w w w . r b o . o r g . b r
Case
report
Solid
variant
of
aneurysmal
bone
cist
on
the
distal
extremity
of
the
radius
in
a
child
夽
Adriano
Jander
Ferreira,
Sebastião
de
Almeida
Leitão,
Murilo
Antônio
Rocha,
Valdênia
das
Grac¸as
Nascimento
∗,
Giovanni
Bessa
Pereira
Lima,
Antonio
Carlos
Oliveira
de
Meneses
UniversidadeFederaldoTriânguloMineiro,Uberaba,MG,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory: Received5April2015 Accepted28May2015 Availableonline30March2016
Keywords:
Aneurysmalbonecysts Bonetumor
Radiusfractures Child
a
b
s
t
r
a
c
t
Thesolidvariantofaneurismalbonecysts(ABC)isconsideredrare.Itoccurswithgreater frequencyinpediatricpatientsandinthetibia,femur,pelvisandhumerus.Wepresenta caseofametaphyseallyticlesiononthedistalextremityoftheradiusinachildwhose radiographwasrequestedafterlow-energytrauma.Thehypothesisofapathologicalbone fracturesecondarytoananeurysmalbonecystwassuggested.Afterbiopsy,thechild under-wentintralesionalexcisionwithoutbonegraftingandthehistopathologicalfindingswere compatiblewiththesolidvariantofaneurysmalbonecyst.
PublishedbyElsevierEditoraLtda.onbehalfofSociedadeBrasileiradeOrtopediae Traumatologia.ThisisanopenaccessarticleundertheCCBY-NC-NDlicense(http:// creativecommons.org/licenses/by-nc-nd/4.0/).
Variante
sólida
do
cisto
ósseo
aneurismático
na
extremidade
distal
do
rádio
em
uma
crianc¸a
Palavras-chave:
Cistosósseosaneurismáticos Neoplasiasósseas
Fraturasdorádio Crianc¸a
r
e
s
u
m
o
Avariantesólidadocistoósseoaneurismático(COA)éconsideradalesãorara,ocorrecom maiorfrequêncianospacientespediátricose nosossos datíbia,fêmur,pelveeúmero. Apresentamosocasodeumalesãolíticametafisárianaextremidadedistaldorádiode umacrianc¸aemque,aoexameradiográficofeitodevidoaumtraumadebaixaenergia,foi aventadaahipótesedefraturaemumossopatológicosecundáriaaumcistoósseo aneuris-mático.Apósabiópsia,acrianc¸afoisubmetidaaressecc¸ãointralesionalseminterposic¸ão deenxertoeoexamehistopatológicofoicondizentecomavariantesólidadocistoósseo aneurismático.
PublicadoporElsevierEditoraLtda.emnomedeSociedadeBrasileiradeOrtopediae Traumatologia.Este ´eumartigoOpenAccesssobumalicenc¸aCCBY-NC-ND(http:// creativecommons.org/licenses/by-nc-nd/4.0/).
夽
StudycarriedoutattheServiceofOrthopedicsandTraumatology;HospitaldeClínicas;UniversidadeFederaldoTriânguloMineiro; Uberaba;MG;Brazil.
∗ Correspondingauthor.
E-mail:vallfmtm@yahoo.com.br(V.d.G.Nascimento). http://dx.doi.org/10.1016/j.rboe.2016.03.002
rev bras ortop.2016;51(3):370–373
371
Introduction
Theaneurysmalbonecyst (ABC)isanexpansile pseudotu-morlesionofunknownetiology,usuallyfoundinthetibia, femur,pelvisandhumerus.1ThesolidvariantoftheABCwas describedin1983bySanerkinetal.2duetohistological pre-dominanceofsolidmaterialintheaneurysmalbonecyst.It isconsideredrare,accountingfor3.4–7.5%ofallABCs, occur-ringmorecommonlyinpediatricpatients.3Painisthemost commonsymptom,followedbymildedemathatcanprecede thedefinitivediagnosisinupto12months.3Radiographyand CTscanimagesdiscloseanexpansileosteolyticlesion indis-tinguishablefromtheABC.4
Thesolidvariantofaneurysmalbonecystischaracterized byfibroblastproliferationwithoutanycellornuclear pleomor-phism,giantcellssimilartoosteoclastsrichareas,aneurysmal sinusoids,differentiatedosteoclastswithosteoidproduction and occasional foci of degenerated calcifying fibromyxoid tissue.2
Thedifferentialdiagnosesincludesimplebonecyst, repar-ativegiantcellgranuloma,hyperparathyroidismbrowntumor, giantcelltumorandmalignantprimarytumorssuchas chon-drosarcoma,osteosarcomaandEwing’ssarcoma.5
Inthisreportwepresentthecaseofapatientwiththesolid variantofaneurysmalbonecystdiagnosedafterfractureof thedistalextremityoftheradius, secondarytolow-energy trauma.
Clinical
case
Atwo-year-oldgirlwasbroughttotheemergencyroomwith wristpainfortwodaysafterfallingontheground,according tothefamily.Parentsdeniedepisodesoffever.
Physical examination showed pain on palpation of the distal right radius, edema, limitation in passive rotation andflexion–extensionmovementsofthewristduetopain, absenceofjointstiffnessandinflammatorysigns.
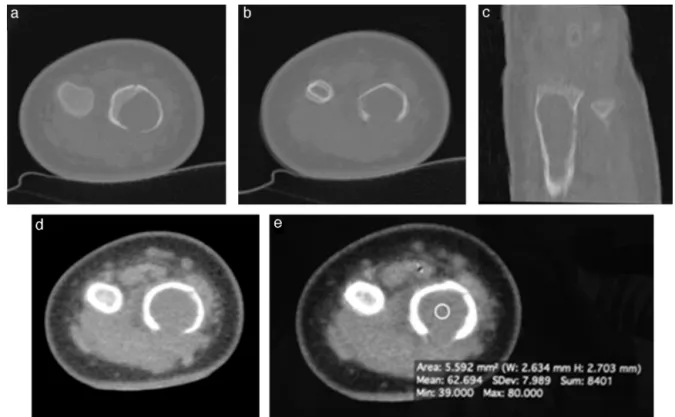
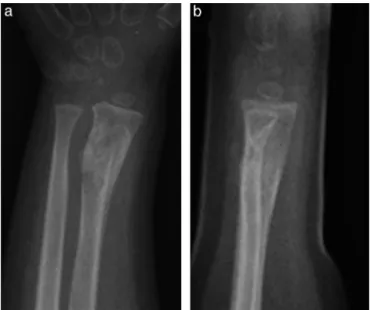
Plainanteroposteriorandlateralradiographsweretaken (Fig.1),anddisclosedthepresenceoflyticmetaphyseallesion, respectingthelimitsofthedistalradialphysis,predominantly homogeneous,withcorticalthinningassociatedwithdorsal andvolarcorticaldiscontinuityofthedistalextremityofthe radius.Aftertheinitialevaluation,aCTscanwasrequested (Fig. 2) and demonstrated more clearly the characteristics ofthelesion.Bonescintigraphyshowedamonostoticlesion withfocalincreaseduptake.Thereafter,itwassuggestedthe hypothesisofdistal radiusfracture ina pathologicalbone, probablyhavinganABCasprimarylesion,withdifferential diagnoses suchasunicameral bonecyst and telangiectatic osteosarcoma.
Thechildunderwent lesionbiopsythatshowedabsence of neoplasia, but without definitive diagnosis. We opted forsurgicaltreatmentwithintralesionalexcision(curettage) associatedwithadjuvantelectrocauterizationwithout inter-positionofbonegrafts and/orbonecement. Theharvested materialwassentforhistopathologyand,aftersurgicalwound closure,thechildwasimmobilizedwithantebrachiopalmar plastercastkeptforsixweeks.
Fig.1–Anteroposterior(a)andlateral(b)radiographic viewsshowingthelyticlesionindistalradialmetaphysis.
Histopathologyshowedsparsemultinucleatedgiantcells, intermingled with partially calcified trabecular immature bone; absence ofnecrosis, mitotic figures and aneurysmal spaces;andnoevidenceofsimplebonecyst.The histopatho-logicalaspectwassuspiciousofsolidaneurysmalbonecyst, despitetheabsenceofaneurysmalvascularspacesasseenon themicroscopeimages(Fig.3).
After eight weeks new radiographs were taken (Fig. 4). Onthefourthpostoperativemonth,newradiographsshowed reactive marginal sclerosis, distancing ofthe initial lesion fromthedistalradialphysisandcorticalthickening– mod-ificationsconsistentwithinactivelesion(Fig.5).
Discussion
Thesolidvariantofaneurysmalbonecystandreparativegiant cellgranulomawereprimarilydescribedincraniofacialbones andsmalltubularbonesofthehandandfoot.2Theyare con-sideredreactiveandnon-neoplasiclesions,althoughtheycan leadtomisdiagnosisofgiantcelltumor,hyperparathyroidism browntumorandosteosarcoma(usuallyfibroblasticor low-gradevariant).6
372
rev bras ortop.2016;51(3):370–373Fig.2–CTscanshowingtheexpansilelyticlesionandassociatedfractureintheaxialviews(aandb);andthemetaphyseal lesionlengthinthecoronalview(c).Intheaxialview(dande)withsofttissuewindow,attenuationofsofttissueswithin theintraosseouslesionthatmayrepresentasolidcomponentorthickfluidcontentcanbeobserved.
Althoughnotspecific, the detectionoffluid levelbyCT scanand/ormagneticresonanceimagingsuggeststhe diag-nosis of ABC.7 The presence of solid material inside the intraosseouslesionwasidentifiedbytheauthorsbythe analy-sisoftheCTscansofttissuewindow,althoughthediagnostic
confirmationofthesolidvariantofaneurysmalbonecystwas achievedonlythroughthehistopathologicalanalysis,withthe followingpathologistdescription:‘histopathologicalaspectis suspiciousofsolidaneurysmalbonecyst,despitetheabsence of aneurysmalvascular spaces.Immature cancellous bone
rev bras ortop.2016;51(3):370–373
373
Fig.4–Anteroposterior(a)andlateralview(b)radiographs atsixpostoperativeweeksshowingfracturehealing.
Fig.5–Anteroposterior(a)andlateralview(b)radiographs fourpostoperativemonthsshowinginactivelesioninthe distalradialextremity.
withmyxoidinterstitialtissueischaracteristicofbone frac-turecallus’.
Recentreportsofthesolidvariantofaneurysmalbonecyst includethehamateboneasreportedbyMavrogenisetal.,8the
cervicalspinebyKarampalisetal.3andthetibiabyTakechi etal.9Consideringthescarcityofreportsintheliteratureon thediagnosisofasolidvariantoftheABCinthedistalradius inachild,weconsideredrelevantreportingthiscase.
Treatment recommendations for ABC include curettage associated withbone grafting. Considering the high recur-rence rates these lesions have when treated with simple curettage only, many surgeons use adjuvant phenol or ethanol.
Inthepresentcase,consideringtheinitialhypothesisof aneurysmalbonecystandduetotheproximitytothedistal radialphysis,wechosetheintralesionalcurettageassociated with adjuvant electrocauterizationwithout graft interposi-tion.Satisfactoryevolutionwasobservedduringfollowup,as shownbythepresentimageswithmarginalsclerosis forma-tion,distancingofthelesionfromthedistalradialphysisand corticalthickening,consistentwithlesioninactivity.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1.MankinHJ,HornicekFJ,Ortiz-CruzE,VillafuerteJ,Gebhardt MC.Aneurysmalbonecyst:areviewof150patients.JClin Oncol.2005;23(27):6756–62.
2.SanerkinNG,MottMG,RoylanceJ.Anunusualintraosseous lesionwithfibroblastic,osteoclastic,osteoblastic,aneurysmal andfibromyxoidelements.Solidvariantofaneurysmalbone cyst.Cancer.1983;51(12):2278–86.
3.KarampalisC,LenthallR,BoszczykB.Solidvariantof aneurysmalbonecystonthecervicalspineofachild:case report,differentialdiagnosisandtreatmentrationale.Eur SpineJ.2013;22(3):523–31.
4.Al-ShamyG,RelyeaK,AdesinaA,WhiteheadWE,CurryDJ, LuerssenTG,etal.Solidvariantofaneurysmalbonecystofthe thoracicspine:acasereport.JMedCaseRep.2011;5:261. 5.GarciaJ,BianchiS.Diagnosticimagingoftumorsofthehand
andwrist.EurRadiol.2001;11(8):1470–82.
6.BertoniF,BacchiniP,CapannaR,RuggieriP,BiaginiR,Ferruzzi A,etal.Solidvariantofaneurysmalbonecyst.Cancer. 1993;71(3):729–34.
7.SullivanRJ,MeyerJS,DormansJP,DavidsonRS.Diagnosing aneurysmalandunicameralbonecystswithmagnetic resonanceimaging.ClinOrthopRelatRes.1999;(366):186–90. 8.MavrogenisAF,SkarpidiE,PapagelopoulosPJ.Solidvariantof
aneurysmalbonecystofthehamate.MusculoskeletSurg. 2010;94(3):145–50.