Arq Neuropsiquiat r 2002;60(4):906-908
DIFFUSION-WEIGHTED SEQUENCE ON M RI FOR THE
DIAGNOSIS OF CREUTZFELDT-JAKOB DISEASE
Edgard Pereira
1ABSTRACT – Creut zfeldt -Jakob disease (CJD) is a progressive and fat al dement ing illness caused by a virus like agent called prion. Currently, the definitive diagnosis can only be made through brain biopsy. Given its potential t ransmissibilit y, it is paramount t o have noninvasive and reliable means t o det ect t he disease. The present case report s on a 63 year-old man w it h biopsy proven CJD, and evaluat es t he dependabilit y of diffusion-w eight ed M RI in t his condit ion, st ressing t he import ance of t his part icular sequence t o it s diagnosis.
KEY WORDS: prion disease, dement ia, magnet ic resonance imaging, diffusion-w eight ed sequence.
Ressonância magnética por difusão no diagnóstico da doença de Creutzfeldt-Jakob
RESUM O – A doença de Creut zfeldt -Jakob (DCJ) é enfermidade demencial progressiva e fat al, causada por um agent e semelhant e a virus chamado prion. At ualment e, o diagnóst ico definit ivo só pode ser feit o at ravés de biópsia cerebral. Devido ao seu pot encial de t ransmissão, a det ecção da doença por meios não invasivos e confiáveis é de ext rema import ância. O present e relat o se refere ao caso descreve um homem de 63 anos com DCJ comprovada por biópsia, e avalia a confiabilidade da ressonância magnét ica com t écnica de difusão nessa condição, enfat izando a import ância dessa sequência para o diagnóst ico da doença.
PALAVRAS-CHAVE: doença priônica, demência, ressonância magnét ica.
Present ed at t he 24t h Annual M eet ing of t he American Societ y of Neuroimaging, Las Vegas, NV, January 24-27, 2001. Depart ment of Radiology, Universit y of Louisville Hospit al: 1Assist ant Professor of Radiology, Neurology and Neurological Surgery.
Received 1 M arch 2002, received in final form 13 July 2002. Accept ed 24 July 2002.
Edgard Pereira, M D - 530 Sout h Jackson St reet - Louisville, Kent ucky 40202 - USA.
Creut zfeldt -Jakob disease (CJD) is a t ransmissible illness caused by a prot ein called prion. The disease present s as a rapid progressive ment al det eriorat ion and memory loss associat ed w it h visual and cere-bellar dysfunction. Other signs include abnormal mo-vements, particularly myoclonus, pyramidal signs and seizures. These f eat ures overlap t hose of ot her disorders and make t he diagnosis difficult . EEG and 14-3-3 protein analysis in the CSF are used to support t he clinical suspicion of t he disease, but t hey have neit her high sensit ivit y nor specificit y t o guarant ee an accurat e diagnosis. The confirmat ion of CJD pre-sence st ill depends on brain t issue examinat ion. Ho-w ever, brain biopsy in t hese pat ient s is associat ed w it h 20% mort alit y1. Thus, t here is an urgent need for a reliable and easily reproducible diagnost ic t est t o avoid missing t reat able condit ions t hat may mimic CJD. Report s addressing t he use of convent ional M RI sequences have been published2-5 but t hey also failed to demonstrate abnormality in a large number of cases. M ore recently, diffusion-w eighted imaging (DWI) has opened a new possibility for the diagnosis of CJD.
In t his report , a review of t he DWI findings in a biopsy proven case support s t his M RI sequence as an essent ial t ool for t he diagnosis of t his condit ion.
CASE
Arq Neuropsiquiat r 2002;60(4) 907
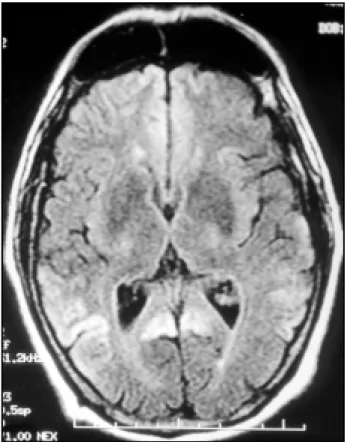
ESR w as 4, ANA and hepat it is t it ers w ere negat ive. RPR w as non react ive. B12 and t hyroid funct ion t est s w ere normal. CSF demonst rat ed a normal cell count , prot ein and glucose, and t he 14-3-3 β isoform w as not det ect ed. Viral cult ures of CSF w ere negat ive. EEG, as w ell as CT of t he brain, w as normal. M RI of t he brain w as performed using a 1.5-T scanner. The fluid at t enuat ed inversion reco-very (FLAIR) images show ed areas of mild increased signal in t he front al, t emporopariet al and occipit al cort ex bila-t erally (Fig 1). The diffusion-w eighbila-t ed imaging (DWI) de-monst rat ed more accurat ely large areas of increased signal in t he front al, t emporopariet al and occipit al lobes (Fig 2). The cent rum semiovale, basal ganglia, and brainst em w ere spared. The cortical sulci, fissures and cisterns w ere normal. M RI repeat ed t w o w eeks lat er did not show int erval changes. The adjacent w hit e mat t er w as spared. M icros-copic examinat ion of t he cort ex specimen obt ained t hro-ugh open brain biopsy demonst rat ed neuronal loss and ast rocyt ic gliosis w it h ext ensive spongiform changes com-pat ible w it h prion disease. Immunohist ochemical st ain for proteinase resistant prion protein w as negative. The patient died 2 mont hs aft er t he diagnosis.
DISCUSSION
CJD is t he most common t ransmissible spongi-form encephalopat hy in humans, w it h a w orldw ide incidence of 0.5 t o 1.0 cases per million per year1. From 1979 t o 1998, 4751 cases of CJD w ere report ed in t he Unit ed St at es, w it h an annual age-adjust ed deat h rat e ranging f rom 0.78 in 1980 t o 1.13 in 19976. The transmissible agent, a proteinase-resistant prot ein (PrP or prion), exist s in t w o isoforms. One (α) is a normal const it uent of t he human cell mem-brane, encoded by a gene in t he chromosome 20. The ot her (β) is found in scrapie and in CJD. The hu-man disease can be sporadic (80-90% of CJD cases), infect ious, or genet ic7. Familial cases occur as a con-sequence of mut at ion in t he PrP gene, w hich t here-fore are bot h herit able and t ransmissible. Iat rogenic disease result s from use of cont aminat ed st ereot at ic brain electrodes, transplanting corneas or dura mater f ro m af f ect ed in d ivid u als o r ad m in ist rat io n o f infect ed grow t h hormone ext ract . Alt hough measu-res t o reduce t he iat rogenic form have been imple-ment ed, t he occurrence of a new variant (nvCJD) ac-quired from exposure t o bovine spongiform ence-phalopat hy, may spaw n donor groups w hose t issue and blood could be used in complet e ignorance of t heir pot ent ial infect ivit y8.
The clinical diagnosis of CJD may be suggest ed in a middle age pat ient w it h progressive dement ia, myoclonus, and cerebellar signs. How ever, t his t riad overlaps ot her dement ial disorders9, or it may not be manifest ed as in t he present case. The clinical
Fig 2. Axial DWI (TR/TE 9999/92.6), approximat ely at t he same level as t he previous image, depict s unequivocal hyperint ense signal in t he front al, t emporal and occipit al cort ices bilat erally. The basal ganglia and t halamus are spared.
908 Arq Neuropsiquiat r 2002;60(4)
diagnosis, t heref ore, relies on f ew unpredict able tests. The classical EEG findings of periodic complexes of spikes or slow act ivit y at int ervals of 0.5 t o 2.0 seconds may or not be seen in t he lat e st age of t he disease, and it s occurrence is not pat ognomonic for CJD, being associat ed w it h ot her ent it ies easily mis-t aken for mis-t his disorder. M oreover, EEG changes are not charact erist ic of t he nvCJD10. Det ect ion of 14-3-3 prot eins in t he CSF, considered t o be t he most relia-ble diagnost ic t ool, w it h a sensit ivit y of 94% and specificit y of 84%11, w as t hought t o be false posit ive only for diseases easily dist inguished from CJD such as subarachnoid hemorrhage or inflammat ory CNS disorders. It is now know n to have misleading results, eit her being falsely posit ive in pat ient s w it h disorders resembling CJD, such as front ot emporal dement ial and Alzheimer disease, or falsely negat ive in some t ypical aut opsy proven sporadic CJD, in a large num-b er of genet ic CJD, and in m any p at ient s w it h nvCJD12,13. CT is of no help in t he diagnosis, show ing no abnormalit ies (80%) or nonspecific at rophy14. Ex-t ensive liEx-t eraEx-t ure now exisEx-t s describing M RI findings in pat ient s w it h CJD. These nonspecific abnormalit ies include symmet ric bilat eral increased signal int ensit y in t he basal ganglia and t halami on T2- and prot on densit y w eight ed images, w it h normal signal on T1-w eight ed images. HoT1-w ever, convent ional sequences seem not t o be very sensit ive for CJD, since no major changes could be ident ified in 21% of pat ient s in a st udy of 29 pat ient s5 w it h sporadic disease. Equally, no specific M RI changes w ere observed in a series of 33 p at ien t s w it h iat ro g en ic CJD15. In ad d it io n , adjacent CSF signal may obscure cort ical abnorma-lit ies on convent ional M RI sequences, making t his diagnost ic t ool almost useless in t he so-called occi-pit al (Haidenhain) variant . The use of FLAIR images may circumvent somew hat this problem in detecting cortical abnormalities16, and the k-space reordered by inversion time at each slice position sequence may even improve the conventional FLAIR in this particular17. On the other hand, DWI has been show n to increase the M RI resolution and yields better demonstration of the abnorm al f indings in pat ient s w it h CJD18-20. Such abnormalities w ere also found to correlate w ith those areas of dist urbed met abolism by PET and SPECT scans20. The physicochem ical basis f or dif f usion abnormalities in this disease is unclear, but perhaps the compartmentalization of w ater w ithin the vacuoles may rest rict t he diffusion of it s molecules and be responsible for the high signal observed on DWI.
Although previous reports have demonstrated the great er sensit ivit y of DWI as compared t o rout ine
M RI sequences, all hist ologically confirmed CJD have also show n t ypical changes in t he EEG and/or a posi-t ive 14-3-3 proposi-t ein immunoassay in posi-t he CSF. The ma-jorit y of t hem w ere also remarkable for high signal in t he basal ganglia bilat erally on DWI. The present case, how ever, w as unique in t hat bot h EEG and CSF analysis have show n normal result s, and DWI ab-normalit ies w ere rest rict ed t o t he cerebral cort ex.
In conclusion, findings on DWI increase t he diag-nost ic accuracy in CJD and may be t he most cons-picuous abnormalit ies seen in t his disease. DWI also might guide t he st ereot at ic biopsy t o an area of in-creased pat hological act ivit y t o maximize it s efficacy and safeness. M oreover, it s short scanning t ime en-sures few art ifact s, especially in pat ient s w it h myo-clonus. Thus, this report substantiates the DWI fea-tures in CJD and adds further support to its role as the sequence of choice for the diagnosis of this condition, particularly w hen other auxiliary tests are negative.
REFERENCES
1. Brown P. Transmissible spongiform encephalopaties. In Bradley WG, Daroff RB, Fenichel GM, et al. (Eds). Neurology in clinical practice. Boston: Butterworth-Heinemann, 2000:1423-1430.
2. Esmonde TF, Will RG. Magnetic resonance imaging in Creutzfeldt-Jakob disease. Ann Neurol 1992;31:230-231.
3. Falcone S, Quencer RM, Bowen B, et al. Creutzfeldt-Jakob disease: focal symmetrical cortical involvement demonstrated by MR imaging. AJNR 1992;13:403-406.
4. Barboriak DP, Provenzale JM, Boyko OB. MR diagnosis of Creutzfeldt-Jakob disease: significance of high signal intensity in the basal ganglia. AJR 1994;162:137-140.
5. Finkenstaedt M, Szudra A, Zerr I, et al. MR imaging of Creutzfeldt-Jakob disease. Radiology 1996;199:793-798.
6. Gibbons RV, Holman RC, Belay ED, et al. Creutzfeldt-Jacok disease in the United States: 1979-1998. JAMA 2000;284:2322-2323.
7. Jubelt B. Prion diseases. In Row land LP (Ed). Merritt’ s neurology. Philadelphia: Lippincott Williams & Wilkins, 2000:206-211. 8. Brown P, Preece M, Brandel JP, et al. Iatrogenic Creutzfeldt disease at
the millennium. Neurology 2000;55:1075-1081.
9. Haik S, Brandel JP, Sazdovitch V, et al. Dementia with Lewy bodies in a neuropathologic series of suspected Creutzfeldt-Jakob disease. Neurology 2000;55:1401-1404.
10. Zeidler M, Stewart GE, Barraclough CR, et al. New variant Creutzfeldt-Jakob disease: neurological and diagnostic tests. Lancet 1997;350:903-907. 11. Zerr I, Pocchiari M, Collins S, et al. Analysis of EEG and CSF 14-3-3
p ro teins as aid s to the d iagno sis o f Creutzfeld t-Jako b d isease. Neurology 2000;55:811-815.
12. Chapman T, McKeel DW, Morris JC. Misleading results with the 14-3-3 assay for the diagnosis of Creutzfeldt-Jakob disease. Neurology 2000;55:1396-1397. 13. Burkhard PR, Sanchez JC, Landis T, et al. CSF detection of the 14-3-3 protein
in unselected patients with dementia. Neurology 2001;56:1528-1533. 14. Galvez S, Cartier L. Computed tomography findings in 15 cases of
Creutzfeldt-Jakob disease w ith histological verification. J Neurol Neurosurg Psychiatry 1984;47:1244-1246.
15. Billette de Villemeur T, Deslys JP, Gelot A. Clinical and pathological aspects of iatrogenic Creutzfeldt-Jakob disease. In Court L, Dodet B (Eds). Transmissible subacute spongiform encephalopathies: prion diseases. Paris: Elsevier, 1997:537-545.
16. Vrancken A FJE, Frijns CJM, Ramos LMP. FLA IR MRI in sporadic Creutzfeldt-Jakob disease. Neurology 2000;55:147-148.
17. Herlihy AH, Hajnal JV, Curati WL, et al. Reduction of CSF and blood flow artifacts on FLAIR images of the brain with k-space reordered by inversion time at each slice position (KRISP). AJNR 2001;22:896-904. 18. Bahn MM, Parchi P. Abnormal diffusion-weighted magnetic resonance
images in Creutzfeldt-Jakob disease. Arch Neurol 1999;56:577-583. 19. Demaerel P, Heiner L, Robberecht W, et al. Diffusion-weighted MRI in
sporadic Creutzfeldt-Jakob disease. Neurology 1999;52:205-208. 20. Na DL, Suh CK, Choi SH, et al. Diffusion-weighted magnetic resonance