REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
Publicação Oficial da Sociedade Brasileira de Anestesiologiawww.sba.com.br
SCIENTIFIC
ARTICLE
Effects
of
carbon
dioxide
insufflation
on
regional
cerebral
oxygenation
during
laparoscopic
surgery
in
children:
a
prospective
study
Ayca
Tas
Tuna
a,∗,
Ibrahim
Akkoyun
b,
Sevtap
Darcin
c,
Onur
Palabiyik
daSakaryaUniversity,FacultyofMedicine,DepartmentofAnesthesiology,Sakarya,Turkey
bKonyaTrainingandResearchHospital,DepartmentofPediatricSurgery,Konya,Turkey
cDrFarukSukanMaternityandChildHospital,DepartmentofAnesthesiology,Konya,Turkey
dSakaryaUniversity,TrainingandResearchHospital,DepartmentofAnesthesiology,Sakarya,Turkey
Received10September2014;accepted28October2014
Availableonline12May2015
KEYWORDS Pediatricanesthesia; Carbondioxide insufflation; Regionalcerebral oxygen;
Laparoscopy
Abstract
Backgroundandobjectives: Laparoscopic surgery has become a popular surgical tool when comparedtotraditionalopensurgery.Therearelimiteddataonpediatricpatientsregarding whetherpneumoperitoneumaffectscerebraloxygenationalthoughend-tidalCO2concentration
remainsnormal.Therefore,thisstudywasdesignedtoevaluatethechangesofcerebraloxygen saturationusingnear-infraredspectroscopeduringlaparoscopicsurgeryinchildren.
Methods:Thestudycomprisedfortychildrenwhowerescheduledforlaparoscopic(GroupL,
n=20)oropen(GroupO,n=20)appendectomy.Hemodynamicvariables,rightandleftregional cerebraloxygensaturation(RrSO2andLrSO2),fraction ofinspired oxygen, end-tidalcarbon
dioxidepressure(PETCO2),peakinspiratorypressure(Ppeak),respiratoryminutevolume,
inspi-ratoryandend-tidalconcentrationsofsevofluraneandbodytemperaturewererecorded.All parameterswererecordedafteranesthesiainductionandbeforestartofsurgery(T0,baseline), 15minafterstartofsurgery(T1),30minafterstartofsurgery(T2),45minafterstartofsurgery (T3),60minafterstartofsurgery(T4)andendofthesurgery(T5).
Results:TherewereprogressivedecreasesinbothRrSO2andLrSO2levelsinbothgroups,which
were notstatisticallysignificantatT1,T2,T3,T4.The RrSO2levelsofGroupL atT5were
significantlylowerthanthatofGroupO.OnepatientinGroupLhadanrSO2value<80%ofthe
baselinevalue.
Conclusions: Carbondioxide insufflationduringpneumoperitoneuminpediatricpatientsmay notaffectcerebraloxygenationunderlaparoscopicsurgery.
© 2015SociedadeBrasileirade Anestesiologia.Publishedby ElsevierEditoraLtda.Allrights reserved.
∗Correspondingauthor.
E-mail:aycatas@yahoo.com(A.T.Tuna).
http://dx.doi.org/10.1016/j.bjane.2014.10.004
PALAVRAS-CHAVE Anestesiapediátrica; Insuflac¸ãodedióxido decarbono;
Oxigêniocerebral regional;
Laparoscopia
Efeitosdainsuflac¸ãodedióxidodecarbonosobreaoxigenac¸ãocerebralregional durantecirurgialaparoscópicaemcrianc¸as:umestudoprospectivo
Resumo
Justificativaeobjetivos: Acirurgialaparoscópicasetornouumaferramentacirúrgicapopular emcomparac¸ãocomacirurgiaabertatradicional.Hápoucosdadossobrepacientespediátricos noqueserefereaopneumoperitônioafetaraoxigenac¸ãocerebralenquantoaconcentrac¸ãode CO2aofinaldaexpirac¸ãocontinuanormal.Portanto,esteestudotevecomoobjetivoavaliaras
alterac¸õesdasaturac¸ãodeoxigêniocerebralusandoespectroscopiadeinfravermelhopróximo durantecirurgialaparoscópicaemcrianc¸as.
Métodos: Oestudorecrutouquarentacrianc¸asprogramadasparaapendicectomialaparoscópica (GrupoL,n=20)ouaberta(GrupoA,n=20).Variáveishemodinâmicas,saturac¸ãodeoxigênio cerebralregional direitae esquerda(RrSO2 e LrSO2), frac¸ão inspiradade oxigênio,pressão
expiratóriafinaldedióxidodecarbono(PETCO2),picodepressãoinspiratória(Ppico),volume
minutorespiratório,concentrac¸õesdesevofluranoinspiradoeexpiradoetemperaturacorporal foramregistados.Todososparâmetrosforamregistadosapósainduc¸ãodaanestesiaeantesdo iníciodacirurgia(T0,basal),15minutosapósoiníciodacirurgia(T1),30minutosapósoinício dacirurgia(T2),45minutosapósoiníciodacirurgia(T3),60minapósoiníciodacirurgia(T4) enofinaldacirurgia(T5).
Resultados: Houvediminuic¸ãoprogressivaemambososníveisdeRrSO2eLrSO2nosdoisgrupos, masnãofoiestatisticamentesignificativaemT1,T2,T3,T4.OsníveisdeRrSO2doGrupoLem T5foramsignificativamentemenoresqueosdoGrupoA.UmpacientedoGrupoLapresentou umvalorrSO2<80%dovalorbasal.
Conclusões:A insuflac¸ão de dióxido de carbono durante o pneumoperitônio em pacientes pediátricospodenãoafetaraoxigenac¸ãocerebralemcirurgialaparoscópica.
©2015SociedadeBrasileiradeAnestesiologia.PublicadoporElsevierEditoraLtda.Todosos direitosreservados.
Introduction
Laparoscopicsurgeryhasbecomeapopularsurgicaltooldue toitslessinvasivenature,therebyprovidingamorerapid recoverywithashorterhospitalstay,decreased postopera-tivepainandimprovedcosmeticoutcomewhencompared totraditionalopensurgery.1,2Thesuccessfulapplicationof
laparoscopictechniquesinadultshasledtotheirincreasing useinpediatricsurgery.3,4Aninvestigationinadultpatients
hasshown that although relatively uncommon, significant
changes in cerebral oxygenation occur in some patients
during CO2 insufflation for laparoscopic surgery.5 There
are limited data on pediatric patients regarding whether
pneumoperitoneumaffects cerebral oxygenation although
end-tidalCO2concentrationremainsnormal.
Ourhypothesiswasthatcerebraloxygensaturationwould
decreasein pediatricpatients duringlaparoscopic surgery
becauseofpneumoperitoneumandCO2absorption.
There-fore,this study wasdesigned to evaluate the changes of
cerebraloxygensaturationusingnear-infraredspectroscope
(NIRS)duringlaparoscopicsurgeryinchildren.
Methods
Afterreceivingapprovalfromtheethicscommitteeofthe
KırıkkaleUniversity,fortychildrenwithASAphysicalstatus
Iwhowerescheduled forlaparoscopic(GroupL,n=20)or
open(GroupO,n=20)appendectomysurgerywereenrolled
in this prospective study. Written informed consent was
obtainedfromallthepatients’parentsbeforethesurgery.
Exclusioncriteriawereasfollows:patientswhose parents
did not give consent,ASA II and above, age ≥18 and ≤2
years.
Thechildren’sages,weightsandheightswerenoted.All
patientsweremonitoredbyelectrocardiogram(ECG),
non-invasive blood pressure (BP), heart rate (HR), peripheral
oxygen saturation (SpO2),right andleft regional cerebral
oxygen saturation (RrSO2 and LrSO2), fraction of inspired
oxygen, end-tidal carbon dioxide pressure (PETCO2), peak
inspiratory pressure (Ppeak), respiratory minute volume,
inspiratoryandend-tidalconcentrationsofsevofluraneand
bodytemperaturecontinuouslythroughouttheanesthesia.
InallpatientsforRrSO2andLrSO2measurement,sensors
for cerebral oximeter (NIRS model INVOS 5100;
Somanet-ics,Troy,MI)wereplacedbilaterallyatleast2cmabovethe
eyebrowontherightandleftsidesoftheforehead
accord-ing tothemanufacturer’s instructions beforeinduction of
anesthesia.Cerebraloxygendesaturationwasdefinedasan
rSO2value<80%ofthebaselinevalue.Intheeventofsuch
adecreaseinrSO2,100%oxygenwasadministered.
All children received a standardized anesthetic
tech-nique.Anesthesiawasinducedwithintravenousthiopenthal
(5mgkg---1), remifentanyl (0.2
g/kg/min) and atracuryum
besilat(0.5mg/kg).Whenmaximumneuromuscularblocking
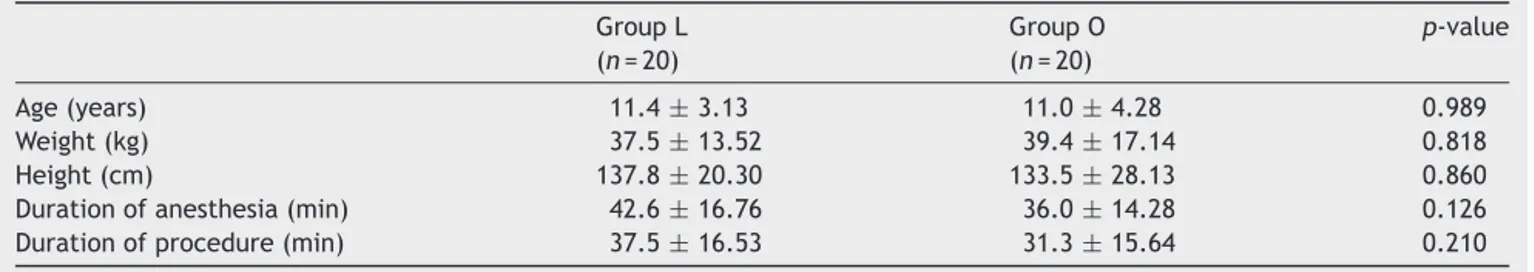
Table1 Demographicandclinicaldataforeachgroup. GroupL (n=20)
GroupO (n=20)
p-value
Age(years) 11.4±3.13 11.0±4.28 0.989 Weight(kg) 37.5±13.52 39.4±17.14 0.818 Height(cm) 137.8±20.30 133.5±28.13 0.860 Durationofanesthesia(min) 42.6±16.76 36.0±14.28 0.126 Durationofprocedure(min) 37.5±16.53 31.3±15.64 0.210
Dataaremean±SDorn.
endotracheal intubation. Anesthesia was maintained with a minimum alveolar anesthetic concentration (MAC) of sevoflurane of 1% and 66% air in oxygen. A remifentanyl infusion (0.05---0.2g/kg/min) was continued to maintain
surgical analgesia. Mechanical ventilation was performed using a pressure-controlled mode (AS3; Datex-Engstroem, Helsinki, Finland). Respiratory rate wasadjusted to keep PETCO2 value between 35 and 45mmHg throughout the
surgery in both groups. In both groups, all patients were arrangedinsupinepositionthroughoutthesurgeryand dur-ing laparoscopic procedures; the abdominal pressure was maintainedat 8---12mmHg.At theend ofthe surgery, the neuromuscular block was reversed with neostigmine and atropine.
Allparameterswererecordedafteranesthesiainduction andbeforestartofsurgery(T0,baseline),15minafterstart of surgery (T1),30min after start of surgery (T2),45min afterstartofsurgery(T3),60minafterstartofsurgery(T4) andendofthesurgery(T5).Thedurationoftheanesthesia andthesurgerywerealsorecorded.
Statisticalanalysis
Data were analyzed using the IBM SPSS (version 15.0 for Windows)statistical package.Data wereexpressed as mean±standarddeviation(SD)ornwhereappropriate.The Mann---WhitneyUtestwasemployedforthecomparisonof continuousvariablesamonggroups. Ap-value ofless than 0.05wasacceptedasstatisticallysignificant.
Results
The two groups were similarwith respectto their demo-graphicdata(Table1).
The durationofboth theanesthesiaandtheprocedure
werealsocomparablebetweenthegroups(Table1).
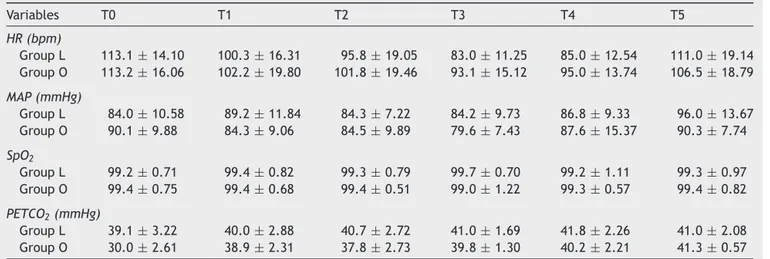
ThehemodynamicparameterssuchasHRmeanarterial
BP, SpO2 and PETCO2 levelswere comparable between the
groups(Table2).
The changein rSO2 isshown inTable3.Althoughthere
wasa progressivedecreasein bothRrSO2andLrSO2levels
inbothgroups,itwasnotstatisticallysignificantatT1,T2, T3,T4 (p>0.05).The RrSO2 levelsofGroup Lat T5 were
significantlylowerthanthatofGroupO(p=0.032).
Only onepatientinGroupLhad anrSO2 value<80%of
thebaselinevalue.
Discussion
Themainfindingofthisstudyis thatCO2insufflation
dur-ingpneumoperitoneuminpediatricpatientsmaynotaffect
cerebraloxygenationunderlaparoscopicsurgery.
Pneumoperitoneumexerts itseffects onorgansystems
primarily via the physical pressure on those systems and
secondlydue tothesystemicabsorptionofcarbondioxide
(thediffusion of CO2 across the peritoneum andinto the
bloodstream).Thephysiologicaleffectsareincreasedwith
decreasingageandweightduetodecreasedmusclebulk,an
increasedperitonealsurfaceareatomassratio,decreased
peritonealthicknessanddecreasedorgan-specificreserve.3
Intra-abdominalpressure(IAP)is acriticaldeterminant
of cardiovascular stability during laparoscopy. Raised IAP
duringpneumoperitoneumdeterminesbradycardiaor
asys-tolebecauseof ahigh levelof vagaltone inchildren.6 To
keepthephysiologicalchangestoaminimum,thelowestIAP
requiredtocarryouttheproceduresafelyisrecommended
aslessthan15mmHginchildren.7 InsufflationwithanIAP
<10mmHg augmentspreload throughthe displacement of
bloodfromthe splanchnicvasculature, while pressures of
>15mmHgimpedesvenousreturn.8Accordingtothese
rec-ommendations,wekeepIAPbetween8and10mmHgduring
laparoscopicsurgery.
Cerebral oximetry has been extensively evaluated in
adultsaswellasinpediatricsurgeryandneonatology.5,9,10
Cerebral oximetry with near-infrared spectroscopy (NIRS)
allows continuous and non-invasive monitoring of rSO2,
which reflects a balance between cerebral oxygen supply
anddemand.11 NIRSquantitatesavenous-weightedratioof
oxygenatedanddeoxygenatedhemoglobinintheregionof
thecerebralcortexunderlyingthesensors,whichareusually
placedontheforehead.12 AnrSO
2value<80%ofthe
base-lineor rSO2 <50%wereassociated withahigherincidence
of cerebral ischemia, postoperative cognitive dysfunction
andlongerhospitalstays.2,11,13Additionally,ifthebaselineis
lowerthan50%,thecriticalthresholdshouldbereducedto
15%.11 Inthepresent study,onepatienthadan rSO
2value
<80%ofthe baselineatthefortiethmin ofsurgeryduring pneumoperitoneum.
There area limitednumber of studies focusingonthe
relationshipbetweenlaparoscopicsurgeryandrSO2in
pedi-atrics. De Waal et al. demonstrated that insufflation of
CO2atlowIAPs(≤8mmHg)inchildrencausesconsiderable
increasesin PETCO2 andarterial CO2 pressure (PaCO2) that
arereflectedinincreasesinrSO2andcerebralbloodvolume,
Table2 Hemodynamicparametresandnumberofcasesforeachgroup.
Variables T0 T1 T2 T3 T4 T5
HR(bpm)
GroupL 113.1±14.10 100.3±16.31 95.8±19.05 83.0±11.25 85.0±12.54 111.0±19.14 GroupO 113.2±16.06 102.2±19.80 101.8±19.46 93.1±15.12 95.0±13.74 106.5±18.79
MAP(mmHg)
GroupL 84.0±10.58 89.2±11.84 84.3±7.22 84.2±9.73 86.8±9.33 96.0±13.67 GroupO 90.1±9.88 84.3±9.06 84.5±9.89 79.6±7.43 87.6±15.37 90.3±7.74
SpO2
GroupL 99.2±0.71 99.4±0.82 99.3±0.79 99.7±0.70 99.2±1.11 99.3±0.97 GroupO 99.4±0.75 99.4±0.68 99.4±0.51 99.0±1.22 99.3±0.57 99.4±0.82
PETCO2(mmHg)
GroupL 39.1±3.22 40.0±2.88 40.7±2.72 41.0±1.69 41.8±2.26 41.0±2.08 GroupO 30.0±2.61 38.9±2.31 37.8±2.73 39.8±1.30 40.2±2.21 41.3±0.57
Dataaremean±SDorn.
To,baseline,afteranesthesiainduction,beforestartofsurgery;T1,15minafterstartofsurgery;T2,30minafterstartofsurgery;T3, 45minafterstartofsurgery;T4,60minafterstartofsurgery;T5,endofthesurgery;HR,heartrate;MAP,meanarterialpressure;SpO2, peripheraloxygensaturation;PETCO2,end-tidalcarbondioxidepressure.
Incontrast,Tsypinetal.reportedanaverageofa3% reduc-tioninregionalcerebraltissuesaturationinchildrenduring gynecological laparoscopic interventions, which was mea-suredbytheCritikonRedOxMonitor2020device.9According
toourresults,wefoundnodifferenceinreductionofrSO2
betweenlaparoscopyandopensurgery.
Thelimitationofthecurrentstudyisthatwedidnot mon-itorPaCO2changesduringCO2insufflation.Itwasreported
thatPETCO2maynotcorrelatewithPaCO2,thereforearterial
blood gas analysis monitoring should be performed
dur-inglonglaparoscopicprocedures.15Becauseoflaparoscopic
appendectomyisaminimalinvasivesurgery,sothatPaCO2
monitorizationmaynotbeappropriateethically.
Inconclusion, the results of the present study showed
thatallpatients,exceptonefromthelaparoscopicgroup,
tolerated CO2 insufflation without significant affects on
cerebral oxygenation.Although cerebral rSO2 changesare
insignificant andthere is no standard care for the use of
NIRS-based cerebral oximetry in pediatric anesthesia, the
INVOScerebraloxymetermaybeahelpfulmonitoringtool
for detecting real-time rSO2 changes during
pneumoperi-toneumwithCO2.
Table3 Changesincerebraloxygenation.
Variables GroupL (n=20)
GroupO (n=20)
p-value
RrSO2
To 75.1±9.73 79.4±9.51 NS T1 71.3±11.53 76.2±7.05 NS T2 70.7±9.12 76.0±9.62 NS T3 67.2±7.61 71.8±12.27 NS T4 65.2±8.13 70.0±7.07 NS T5 76.2±9.11 82.5±7.97a 0.03
LrSO2
To 72.9±11.64 79.2±8.52 NS
T1 72.2±10.25 74.1±7.80 NS
T2 70.9±11.62 72.3±8.17 NS
T3 69.1±12.62 68.2±14.3 NS
T4 67.8±12.87 67.7±7.54 NS
T5 76.0±10.97 79.5±6.95 NS
NumberofcasewithrSO2value<80%ofthebaselinevalue(n) 1 0 NS
Dataaremean±SDorn.
Boldp-valueissignificant.RrSO2,rightregionalcerebraloxygensaturation;LrSO2,leftregionalcerebraloxygensaturation;To,baseline,
afteranesthesiainduction,beforestartofsurgery;T1,15minafterstartofsurgery;T2,30minafterstartofsurgery;T3,45minafter startofsurgery;T4,60minafterstartofsurgery;T5,endofthesurgery.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.TruchonR.Anestheticconsiderationsforlaparoscopicsurgery inneonatesandinfants:apracticalreview.BestPractResClin Anaesthesiol.2004;18:343---55.
2.MokaE.Cerebraloximetryandlaparoscopicsurgery.JMinim AccessSurg.2006;2:47---8.
3.Lasersohn L. Anesthetic considerations for pediatric laparoscopy.SAfrJSurg.2011;49:22---6.
4.Huettemann E, Terborg C, Sakka SG, et al. Preserved CO2 reactivityandincreaseinmiddlecerebralarterialbloodflow velocityduringlaparoscopicsurgeryinchildren.AnesthAnalg. 2002;94:255---8.
5.GipsonCL,JohnsonGA,Fisher R,et al.Changes incerebral oximetryduringperitonealinsufflationforlaparoscopic proce-dures.JMinimAccessSurg.2006;2:67---72.
6.GuptaR,SinghS.Challengesinpediatriclaparoscopicsurgeries. IndianJAnesth.2009;53:560---6.
7.NwokomoNJ, Tsang T. Laparoscopy in children and infants. Advanced Laparoscopy Prof. Ali Shamsa. Intech, China. 2011:27---46.
8.TobiasJD.Anesthesiaforminimallyinvasivesurgeryinchildren. BestPractResClinAnaesthesiol.2002;16:115---30.
9.TsypinLE,Mikhel’sonVA,ChusovKP,etal.Centralandcerebral hemodynamicduringgynecological laparoscopicinterventions inchildren.AnesteziolReanimatol.2007;1:30---2.
10.GunaydınB,NasT,BiriA,etal.Effectsofmaternal supplemen-taryoxygen onthenewborn for electivecesareandeliveries underspinalanesthesia.JAnesth.2011;25:363---8.
11.CasatiA,SpreaficoE,PutzuM,etal.Newtechnologyfor nonin-vasivebrainmonitoring:continuouscerebraloximetry.Minerva Anestesiol.2006;72:605---25.
12.KasmanN,BradyK.Cerebraloximetryfor pediatric anesthe-sia:why do intelligentclinicians disagree?PaediatrAnaesth. 2011;21:473---8.
13.ParyEY,KooB-N,MınKT,etal.Theeffectofpneumoperitoneum inthesteepTrendelenburgposition oncerebraloxygenation. ActaAnaesthesiolScand.2009;53:895---9.
14.de WaalEE, de VriesJW, Kruitwagen CL,et al. The effects of low-pressure carbon dioxide pneumoperitoneum on cere-braloxygenationandcerebralbloodvolumeinchildren.Anesth Analg.2002;94:500---5.