w w w . r e u m a t o l o g i a . c o m . b r
REVISTA
BRASILEIRA
DE
REUMATOLOGIA
Original
article
Which
is
the
best
cutoff
of
body
mass
index
to
identify
obesity
in
female
patients
with
rheumatoid
arthritis?
A
study
using
dual
energy
X
-ray
absorptiometry
body
composition
Maria
Fernanda
B.
Resende
Guimarães
a,∗,
Maria
Raquel
da
Costa
Pinto
a,
Renata
G.
Santos
Couto
Raid
b,
Marcus
Vinícius
Melo
de
Andrade
c,
Adriana
Maria
Kakehasi
a,daUniversidadeFederaldeMinasGerais(UFMG),HospitaldasClínicas,Servic¸odeReumatologia,BeloHorizonte,MG,Brazil
bUniversidadeFederaldeMinasGerais(UFMG),FaculdadedeTecnologiaemRadiologia,BeloHorizonte,MG,Brazil
cUniversidadeFederaldeMinasGerais(UFMG),FaculdadedeMedicina,DepartamentodeClínicaMédica,BeloHorizonte,MG,Brazil
dUniversidadeFederaldeMinasGerais(UFMG),FaculdadedeMedicina,DepartamentodoAparelhoLocomotor,BeloHorizonte,MG,
Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received12March2015 Accepted16September2015 Availableonline10March2016
Keywords:
Rheumatoidarthritis Obesity
Bonedensitometry Bodycomposition Bodymassindex
a
b
s
t
r
a
c
t
Introduction:Standardanthropometricmeasuresusedtodiagnoseobesityinthegeneral
populationmaynothavethesameperformanceinpatientswithrheumatoidarthritis.
Objective:Todeterminecutoffpointsforbodymassindex(BMI)andwaistcircumference
(WC)fordetectingobesityinwomenwithrheumatoidarthritis(RA)bycomparingthese standard anthropometricmeasuresto a dual-energyX-rayabsorptiometry (DXA)-based obesitycriterion.
Patientsandmethod:AdultfemalepatientswithmorethansixmonthsofdiagnosisofRA
underwentclinicalevaluation,withanthropometricmeasuresandbodycompositionwith DXA.
Results:Eightytwopatientswereincluded,meanage55±10.7years.Thediagnosisofobesity
inthesamplewasabout31.7%byBMI,86.6%byWCand59.8%byDXA.ConsideringDXA asgoldenstandard,cutoffpointswereidentifiedforanthropometricmeasurestobetter approximateDXAestimatesofpercentbodyfat:forBMIvalue≥25kg/m2wasthebestfor definitionofobesityinfemalepatientswithRA,withsensitivityof80%andspecificityof 60%.ForWC,with80%ofsensitivityand35%ofspecificity,thebestvaluetodetectobesity was86cm.
∗ Correspondingauthor.
E-mail:mfbresende@yahoo.com.br(M.F.Guimarães). http://dx.doi.org/10.1016/j.rbre.2016.02.008
Conclusion: Alargepercentageofpatientswereobese.Thetraditionalcutoffpointsusedfor obesitywerenotsuitableforoursample.ForthisfemalepopulationwithestablishedRA, BMIcutoffpointof25kg/m2 andWCcutoffpointof86cmwerethemostappropriateto detectobesity.
©2016ElsevierEditoraLtda.ThisisanopenaccessarticleundertheCCBY-NC-NDlicense (http://creativecommons.org/licenses/by-nc-nd/4.0/).
Qual
o
melhor
ponto
de
corte
de
índice
de
massa
corporal
para
diagnosticar
a
obesidade
em
mulheres
com
artrite
reumatoide?
Um
estudo
que
usa
a
composic¸ão
corporal
pela
absorciometria
com
raios
X
de
dupla
energia
Palavras-chave:
Artritereumatoide Obesidade
Densitometriaóssea Composic¸ãocorporal Índicedemassacorporal
r
e
s
u
m
o
Introduc¸ão: Medidasantropométricasuniversalmenteusadasparadiagnosticarobesidade
napopulac¸ãogeralpodemnãoapresentaramesmaperformanceempacientescomartrite reumatoide.
Objetivos: Determinarpontosdecortedoíndicedemassacorporal(IMC)eda
circunfer-ência decintura(CC) paradetecc¸ãodeobesidadeemmulherescomartritereumatoide (AR)pormeiodacomparac¸ãodessasmedidasantropométricashabituaiscomosíndices deadiposidadeobtidospeladensitometriaósseaporduplaemissãoderaiosX(DXA).
Pacientesemétodo: MulheresadultascommaisdeseismesesdediagnósticodeARforam
submetidas a avaliac¸ãoclínica commedidas antropométricase à DXAcomexame da composic¸ãocorporal.
Resultados: Foramincluídas82pacientes,médiade55±10,7anos.Odiagnósticode
obesi-dadenaamostrafoide31,7%peloIMC,86,6%pelacircunferênciadecinturae59,8%pela DXA.ConsiderandoaDXAopadrão-ouro,ovalordeIMCacimade25kg/m2foiomais ade-quadoparadefinic¸ãodeobesidadenaspacientescomAR,apresentousensibilidadede80% eespecificidadede60%.Damesmaforma,paraaCC,com80%desensibilidadeede35%de especificidade,ovalorencontradofoide86cmparasedetectaraobesidade.
Conclusão: Foi elevado o porcentual de pacientes obesas. Os pontos de corte
tradi-cionalmenteusadosparaobesidadenãoforamadequadosparanossaamostra.Paraessa populac¸ãodepacientesfemininascomdiagnósticodeAR,opontodecortede25kg/m2para IMCede86cmparaCCfoiomaisadequadoparadefinirobesidade.
©2016ElsevierEditoraLtda.Este ´eumartigoOpenAccesssobumalicenc¸aCC BY-NC-ND(http://creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
Obesityand rheumatoid arthritis(RA) havebeen shown to berelatedindifferentways.Thefirstconditionseemstobe relatedtoanincreasedriskofdevelopmentofthesecond dis-ease.Recentmeta-analysisthatincluded11studiesshowed thatobesesubjectswithBMI≥30kg/m2hadahigherrelative riskfordevelopingRA.1
Inpatientswiththeestablisheddisease,theinflammatory processisableofalteringbodycomposition,leadingtoobesity withincreasedabdominalfat andlossofleanbody mass.2
Thisdecreaseinleanbodymass,alongwiththeincreaseinfat massandincentralobesity,mayberelatedtotheincreased cardiovascularmorbidityandalsowithfunctionaldecline.3
In cases of RA, the occurrence of body fat accumu-lation without a significant increase in body weight is a condition known as rheumatoid cachexia,4,5 whose
esti-mated prevalence ranges from 10 to 67%.6 In a setting
of chronic inflammation, high levels of cytokines cause
metabolicchanges,whichcanresultinthealterationsabove mentioned.7,8
Moreover,accordingtotheUSCenterofDiseaseControl (CDC),9theprevalenceofobesityinpatientswithrheumatoid
arthritisis54%higherthaninRA-freeindividuals.A multicen-terstudyfoundaprevalenceof18%ofobesityinapopulation withRA,10whileanotherstudyfoundaprevalenceof31%.11
EpidemiologicaldataconsideredRAasanindependentrisk factorforcardiovasculardisease(CVD),andoneofthemain causes ofdeathinpatientswiththat disease.12–14 A
meta-analysisof24studiesofpatientswithRAshowedanincrease of 50% in the risk ofdeath from cardiovascular causes in general.15
Obesity can contribute to increasing the risk of CVD developmentaswellasoftypeIIdiabetesmellitus(DMII), dyslipidemia,andhypertension(HBP).16,17
negatively influence the course of the disease, functional capacity ofpatients, as well as disease activity.18,20 Obese
patientsarenot-sogoodrespondentstotheuseofanti-TNF agents,andarelesslikelytoachieveremissionwiththeuse ofthese drugs.21 Onestudyfoundadecreased responseto
treatmentwithacombinationofsyntheticdisease-modifying anti-rheumaticdrugsinpatientswithhighBMIs.22
Obesity, definedas an increase infat insufficient level tocauseadversehealthconsequences,isusuallydiagnosed byanthropometricmeasurementsofbodymassindex(BMI), which is calculated as weightin kilograms divided bythe squareofheightinmeters(kg/m2),andofwaistcircumference (WC).23
BMIiseasy to performand agood indicator ofobesity, but does not have an accurate correlation with body fat. Thisindicator is notable to distinguishbetween fat mass andleanmass,anddonotnecessarilyreflectsthe distribu-tionofbodyfat.24Identifyingfatdistributionisimportantin
theevaluationofoverweightand obesity,asvisceral (intra-abdominal)fatisariskfactorforCVD,regardlessoftotalbody fat.Individualswiththe same BMImayhavedifferent lev-elsofvisceralfatmass;andthisrelationshipbetweenweight andheightmay notbeabletoreflectthosebody composi-tionchanges oftenfoundinpatientswithRA.8 For agiven
valueofBMI,body fatmay differ,andthereis evidenceof higher percentages of body fat in patients with RAversus
controls.25
Dual-energyX-rayabsorptiometry(DXA)isamoreaccurate method than BMI measurement to assess body composi-tion, both in young and in older subjects; this method is sensitivetosmall changes inbody composition.26–28 In RA
patients, theassessmentofbody compositionby DXAwas abnormal,withadecreaseinleanbodymassandanincrease offatmass,especially inpatientswithinnormalrange for BMI.29,30
Theaimofthisstudyistoevaluatethecorrelationbetween conventional anthropometric measurements (BMI and WC) and total fat percentage and adiposity indexes obtained throughbody composition byDXA.Another objective is to identifytheneedof,anddetermine,newcutoffpointsforBMI andWCforobesitydetectioninwomenwithRA.
Patients
and
methods
Female patients with rheumatoid arthritis defined accord-ing totheAmerican CollegeofRheumatology (ACR)198731
ortoACR/EULAR201032classificationcriteria,withover six
monthsofsymptoms,andagedover18yearsoldwere con-secutivelyinvitedtoparticipateinthisstudy.Patients with otherconnectivetissuediseases(overlapsyndromes),except forsecondarySjögren’ssyndrome;withpresenceofa pace-maker,implanteddefibrillator,andorthopedicprosthesis,or any metallic object (pins, screws)from orthopedic surgery wereexcluded fromthis study,due tointerferenceinbody compositionexaminationbyDXA.Beforeperformingany pro-cedure,allparticipantssignedainformedconsentform(FICF) previously approved by the Research Ethics Committee of UFMG.
Allpatientsunderwentclinicalevaluation,whichincluded swollen/painful joint counts. Information related to the disease,diagnosticcriteria,clinicaland laboratory manifes-tations, the presence of extra-articular manifestations, comorbidities, and current and previous treatments, was obtained from an interview and by medical record review.
Anthropometric measurements and bone densitometry withbodycompositionwereperformedonthesame assess-ment day. The participants were weighed barefooted and withoutheavyclothingonaFilizolascale(1–200kg,withan errormarginof50g)intendedexclusivelyforweighing peo-ple.Thesubject’sheightwasmeasuredwiththestadiometer coupledtothesameFilizolascale.TheBMIcalculationwas performedaccordingtotheformula:BMI=weight(kg)/height (m2).
The following BMI ranges were adopted: normal, BMI=18.5–24.9kg/m2; overweight, BMI=25–29.9kg/m2; and obesity,BMI≥30kg/m2,asrecommendedbytheWorld HealthOrganization.33
WCwas performedusingaplastictapemeasure,which wasappliedmidwaybetweenthelowestribandtheiliaccrest withthesubjectstanding,andrepresentedthehorizontal dis-tancearoundtheabdomen.Presenceofabdominalorcentral obesity was considered in women whose waist circumfer-ence≥80cm.34
Wealso calculatedthe conicityindex, whichis another waytoestimateabdominalobesity.Thisindexwasdeveloped fromageometricratiomodel,andwascalculatedusingthe patient’swaistcircumference,weightandheightthroughthe followingformula:35
waistcircumference(cm)
0.109×
weight(kg)height(m)
Body composition was measured byDXA (Discovery W Hologic densitometer [Bedford, MA, USA], v. 3.3.0), and the results were always interpreted by the same trained researcher.Themeasurementswereperformedwiththe sub-jectsupine,afterremovingallmetalfittings,andlastedsix minutes. We used Bray GA’s definition of obesity by DXA, that considers the patient’s gender and age group. In this definition,thepercentageoffatconsideredrepresentativeof obesityvariesfrom39to43%inwomen,accordingtotheirage group.36
Statistical
analysis
The descriptive analysis was performed using mean and standarddeviationforcontinuousvariablesandpercentages forbinaryvariables.Anthropometricvariableswerecorrelated (Spearmanmethod)tototalfatpercentageobservedwithDXA. Theoptimalcutoffpointsofanthropometricvariableswere determinedusingROCcurves,andwiththefindingofpoints thatdeterminedpresetsensitivitiesof80%and90%for detec-tionofobesitydiagnosedwithDXA.
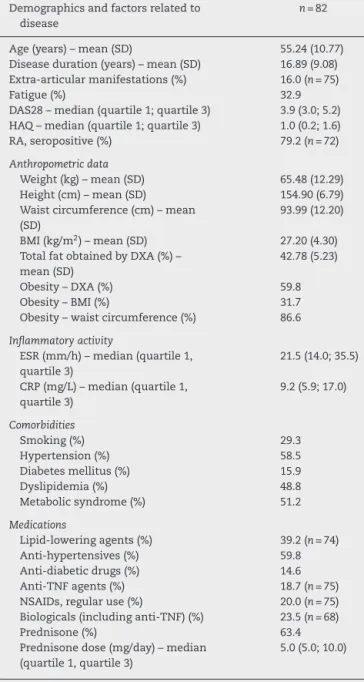
Table1–Demographicandclinicalcharacteristicsof studypopulation.
Demographicsandfactorsrelatedto disease
n=82
Age(years)–mean(SD) 55.24(10.77)
Diseaseduration(years)–mean(SD) 16.89(9.08)
Extra-articularmanifestations(%) 16.0(n=75)
Fatigue(%) 32.9
DAS28–median(quartile1;quartile3) 3.9(3.0;5.2)
HAQ–median(quartile1;quartile3) 1.0(0.2;1.6)
RA,seropositive(%) 79.2(n=72)
Anthropometricdata
Weight(kg)–mean(SD) 65.48(12.29)
Height(cm)–mean(SD) 154.90(6.79)
Waistcircumference(cm)–mean
(SD)
93.99(12.20)
BMI(kg/m2)–mean(SD) 27.20(4.30)
TotalfatobtainedbyDXA(%)–
mean(SD)
42.78(5.23)
Obesity–DXA(%) 59.8
Obesity–BMI(%) 31.7
Obesity–waistcircumference(%) 86.6
Inflammatoryactivity
ESR(mm/h)–median(quartile1, quartile3)
21.5(14.0;35.5)
CRP(mg/L)–median(quartile1, quartile3)
9.2(5.9;17.0)
Comorbidities
Smoking(%) 29.3
Hypertension(%) 58.5
Diabetesmellitus(%) 15.9
Dyslipidemia(%) 48.8
Metabolicsyndrome(%) 51.2
Medications
Lipid-loweringagents(%) 39.2(n=74)
Anti-hypertensives(%) 59.8
Anti-diabeticdrugs(%) 14.6
Anti-TNFagents(%) 18.7(n=75)
NSAIDs,regularuse(%) 20.0(n=75)
Biologicals(includinganti-TNF)(%) 23.5(n=68)
Prednisone(%) 63.4
Prednisonedose(mg/day)–median
(quartile1,quartile3)
5.0(5.0;10.0)
DAS28, Disease Activity Score; HAQ, Health Assessment
Ques-tionnaire;RA,rheumatoidarthritis;BMI,bodymassindex;DXA,
dual-energyX-rayabsorptiometry;ESR,erythrocytesedimentation
rate; TNF, tumor necrosis factor; NSAIDs, nonsteroidal
anti-inflammatorydrug.
Standarddeviationinparenthesesforcontinuousvariables.
Ethics
ThisstudywasapprovedbytheResearchEthicsCommitteeof UniversidadeFederaldeMinasGerais(UFMG)onJanuary10, 2012,withanaddendumandFICFapprovedonFebruary20, 2013.
Results
Eighty-twowomenwithmeanage55±10.7yearsandmean diseasedurationof16±9.08years,wereincludedinthisstudy.
Table2–Spearmancorrelationbetweenanthropometric measurementsforwaistcircumferenceandbodymass indexandtotalfatpercentageobtainedbyDXA.
Women (n=82)
Waistcircumference(cm) 0.482+
BMI(kg/m2) 0.510*
+ p<0.05. ∗ p<0.001.
Table3–SensitivityandspecificityBMI(kg/m2)in obesitydetectiondiagnosedbyDXA.Usualcutoffpoint (BMI=30)andoptimalpointsfound.
Women(n=82)
BMI Specificity Sensibility
30 76% 37%
25 58% 82%
23 36% 92%
ThiscohorthadameanBMIof27.2±4.3kg/m2,ameanwaist
circumferenceof94±12.2cm,andameanconicityindexof 1.33.Thedemographiccharacteristicsandfactorsrelatedto thediseasearelistedinTable1.Theobesityratefoundvaried accordingtodifferentcriteria:31.7%byBMI,86.6%byWC,and 59.8%byDXA.Thecorrelationsbetweenthefollowing clini-calvariableswereevaluated:diseaseduration,DAS28,HAQ, CRP,ESRandcumulativedoseofprednisone,bothwithBMI and withbody fatbyDXA. Noneofthesecorrelations was statisticallysignificant.
Table2showsSpearmancorrelationsbetweentotalfat per-centageobtainedbyDXAandWCandBMI.Onecanperceive thatallcorrelationsobtainedweresignificant(˛=5%)andBMI correlated morestronglywithtotalfatpercentageobtained
byDXAversusbyWC.Thecorrelationbetweenconicityindex
andtotalfatbyDXAwasalsopositive,withstatistical signif-icance(+0.2350withp=0.019);however,thisvaluewaslower thanthatforthecorrelationwithBMI.
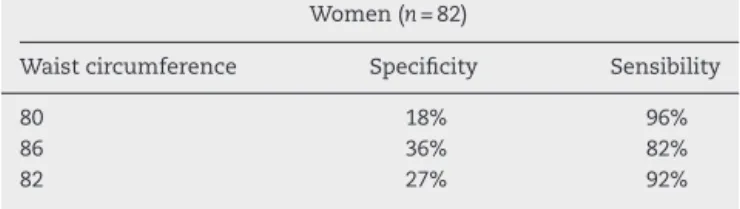
To determine the optimalcutoffpoints ofBMI and WC forobesitydetectioninpatientswithRA,theconstructionof ROCcurvesshowedcutoffvaluespresenting80%and90%of sensitivity. TheROCcurves showthat, forthedesired sen-sitivityvalues,BMIisabetterdiscriminatorofobesitythan WC,thankstoitshigherspecificityforthesamesensitivity values.
Table4–Sensitivityandspecificityofwaist
circumference(cm)inobesitydetectiondiagnosedby DXA.Usualcutoffpoint(80cmforwomen)andoptimal pointsfound.
Women(n=82)
Waistcircumference Specificity Sensibility
80 18% 96%
86 36% 82%
82 27% 92%
Discussion
TheobesityrateinthispopulationofpatientswithRAwas high;aboutonethirdwiththeuseoftheBMIdefinition,60%by DXA,andmorethan80%accordingtoWC.ThestudybyGiles etal.30reportedthat33%ofwomenand36%ofmenwithRA
wereregardedasobesebyBMI,and57%ofthesepatientswere deemedobesebyDXA.Katzetal.havedescribedobesityby BMIin28.4%;ontheotherhand,theseauthorsreached58.2% byDXAinthepopulationstudied.39Inrelationtoobesity
fre-quencybyWC,thevaluefoundwashigherthanthatdescribed intheliterature.24WiththeuseofWC,Katzetal.usedthe
obesitycriterionof88cmforwomen,39,40whereasthepresent
studyusedacutoffpointof80cmbyWC–alevelmorerecently recommendedbytheInternationalDiabetesFederation(IDF) in2006.34
When using DXA asthe gold standard for detection of obesity,werealizethattheprevalenceofthisconditionwas underestimatedbyBMIand overestimatedbyWC.Theuse ofa BMI>30kg/m2 had a sensitivity<40%; and the use of WC>80cm for women showed specificity<20%,clearly an overestimate ofthe number ofobese women in the study group.
One possible explanation for the underestimation seen withtheuseofBMIisthatthisindicatorlackstheabilityto considerthelossofleanbodymassconcomitantlytofatmass gaininindividualswithRA.AsforWC,itmaybethatits rec-ommendedthresholdforwomenisunreasonablylow(80cm), avaluewhichlacksspecificity.
IndeterminingthecutoffpointsofBMIand WCforthis femalepopulationwithRA,weemployedsensitivityvaluesof 80and90%,becauseourunderstandingisthatthese anthro-pometricmeasurementsshould beusedto screenpatients withRA;therefore,ahighsensitivityisacriticalfactor.Then, wecomparedourfindings tothose commonlyusedas cut-offpointsofBMIand WC,achieving the newcutoffpoints suggestedintheresults.
Our results suggest the use of a BMI>25kg/m2 as the thresholdforwomen,becausethis valueresultedina sen-sitivityof82%andinaspecificityof58%inthediagnosisof obesity.ForWC,wesuggesttheuseof86cmfordefinitionof obesity,resultingin82%ofsensitivityand36%ofspecificity.
Theresultsfoundinthisstudy areinlinewiththoseof otherauthorswhosuggestreviewingcutoffpointsofBMIand WCinpatientswithRA.Katzetal.proposedacutoffpointfor obesityinwomenof26.1kg/m2forBMIandof83cmforWC.24
Stavropoulos-Kalinoglouetal.suggestedadecreaseof2kg/m2 inBMIforRApatients,inordertoestablishthepresenceof
obesity.4 In this way,oneperceives auniversal acceptance
oftheconceptthatobesityinRApatientsmustbehandled inanearlyandintensivemanner.Lossofmusclemassand fat infiltrationin themuscle, resulting from inflammation, mayexplainthehigherpercentageoffat,despiteaBMIvalue withinthenormalrange.
Onelimitationofourstudyisitssamplesize;thissuggests thattheresultsobtainedarewaitingforexternalvalidation. The non-inclusion of male patients is another important limitation.Itisnoteworthy,however,thattheprevalenceof femalepatientsseemstoconstitutetheabsolutemajorityin RAcohortsinourpopulation.Inthemultinationalcohortof Latin-Americanpatients(GLADAR),theprevalenceoffemale patientswas85%.41Anotheraspecttoconsideristhatinour
studyagroupofpatientswasexcludedforlackingtheabilityto beexaminedbyDXA;thismayhaveleftoutagroupofpatients withcomorbidities,orwithadiseaseofgreaterseverity.
This sample consisted of patients with long disease duration (mean, 16 years) and high prevalence for use of corticosteroids (63.4%). The statistical analysis showed no correlationbetweendiseaseduration orcumulativedoseof corticosteroidswithBMIorwithtotalfatpercentagemeasured byDXA.Inourstudy,itwasfoundthatbodyfatisincreased inagroupoflong-termRApatients,andotherauthorshave demonstratedthatevenpatientswithearlyRAhavetheirtotal fatincreasedwhenmeasuredbyDXAversuscontrols.42
Conclusions
ConsideringDXAasthegoldstandard,thecutoffpoints con-ventionallyusedforobesitythroughanthropometricindexes werenotsuitableforourRApatients.
BMIwasthebestpredictorofobesityinpatientswithRA
versus WC, showinga bettercorrelation withtotal fat
per-centageobtainedbyDXA.BMIvaluesabove25kg/m2suggest alertnesstooptimizethetreatmentbystrengtheningthegoals forsteroiddiscontinuation,tofightagainstsedentarylifestyle, andnutritionalguidance.
Itissuggestedthat thisnewBMIcutoffpointshouldbe adoptedinclinicalpracticewhenapproachingfemalepatients withRA,inordertoidentifythoseoverweightsubjectsandalso topromoteintensiveinterventionsforbettercardiovascular outcomes.
Funding
FundsremainingfromSBR.
Conflict
of
interests
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
reviewanddose–responsemeta-analysis.ArthritisResTher. 2015;17:86.
2. ArshadA,RashidR,BenjaminK.Theeffectofdiseaseactivity onfat-freemassandrestingenergyexpenditureinpatients withrheumatoidarthritisversusnoninflammatory arthropathies/softtissuerheumatism.ModRheumatol. 2007;17:470–5.
3. ElkanAC,EngvallIL,CederholmT,HafströmI.Rheumatoid cachexia,centralobesityandmalnutritioninpatientswith low-activerheumatoidarthritis:feasibilityofanthropometry, mininutritionalassessmentandbodycomposition
techniques.EurJNutr.2009;48:315–22.
4. Stavropoulos-KalinoglouA,MetsiosGS,KoutedakisY,Nevill AM,DouglasKM,JamurtasA,etal.Redefiningoverweightand obesityinrheumatoidarthritispatients.AnnRheumDis. 2007;66:1316–21.
5. EngvallIL,ElkanAC,TengstrandB,CederholmT,BrismarK, HafstromI.Cachexiainrheumatoidarthritisisassociated withinflammatoryactivity,physicaldisability,andlow bioavailableinsulin-likegrowthfactor.ScandJRheumatol. 2008;37:321–8.
6. RoubenoffR,RoubenoffRA,WardLM,HollandSM,Hellmann DB.Rheumatoidcachexia:depletionofleanbodymassin rheumatoidarthritis.Possibleassociationwithtumor necrosisfactor.JRheumatol.1992;19:1505–10.
7. Stavropoulos-KalinoglouA,MetsiosGS,KoutedakisY,Kitas GD.Obesityinrheumatoidarthritis.Rheumatology(Oxford). 2011;50:450–62.
8. SummersGD,DeightonCM,RennieMJ,BoothAH.
Rheumatoidcachexia:aclinicalperspective.Rheumatology (Oxford).2008;47:1124–31.
9. LiaoKP,SolomonDH.Traditionalcardiovascularriskfactors, inflammationandcardiovascularriskinrheumatoidarthritis. Rheumatology(Oxford).2013;52:45–52.
10.NaranjoA,SokkaT,DescalzoMA,Calvo-AlénJ,
Hørslev-PetersenK,LuukkainenRK,etal.Cardiovascular diseaseinpatientswithrheumatoidarthritis:resultsfrom theQUEST-RAstudy.ArthritisResTher.2008;10:R30.
11.ArmstrongDJ,McCauslandEM,QuinnAD,WrightGD.Obesity andcardiovascularriskfactorsinrheumatoidarthritis. Rheumatology(Oxford).2006;45:782,authorreply782–783. 12.MeuneC,TouzéE,TrinquartL,AllanoreY.Trendsin
cardiovascularmortalityinpatientswithrheumatoid arthritisover50years:asystematicreviewandmeta-analysis ofcohortstudies.Rheumatology(Oxford).2009;48:1309–13. 13.GabrielSE,CrowsonCS,KremersHM,DoranMF,TuressonC,
O’FallonWM,etal.Survivalinrheumatoidarthritis:a population-basedanalysisoftrendsover40years.Arthritis Rheum.2003;48:54–8.
14.PincusT,CallahanLF,SaleWG,BrooksAL,PayneLE,Vaughn WK.Severefunctionaldeclines,workdisability,andincreased mortalityinseventy-fiverheumatoidarthritispatients studiedovernineyears.ArthritisRheum.1984;27: 864–72.
15.Avi ˜na-ZubietaJA,ChoiHK,SadatsafaviM,EtminanM,Esdaile JM,LacailleD.Riskofcardiovascularmortalityinpatients withrheumatoidarthritis:ameta-analysisofobservational studies.ArthritisRheum.2008;59:1690–7.
16.BlüherM.Adiposetissuedysfunctioninobesity.ExpClin EndocrinolDiabetes.2009;117:241–50.
17.VanGaalLF,MertensIL,DeBlockCE.Mechanismslinking obesitywithcardiovasculardisease.Nature.2006;444: 875–80.
18.AjeganovaS,AnderssonML,HafströmI,GroupBS. Associationofobesitywithworsediseaseseverityin rheumatoidarthritisaswellaswithcomorbidities:a long-termfollowupfromdiseaseonset.ArthritisCareRes (Hoboken).2013;65:78–87.
19.WolfeF,MichaudK.Effectofbodymassindexonmortality andclinicalstatusinrheumatoidarthritis.ArthritisCareRes (Hoboken).2012;64:1471–9.
20.OnuoraS.Rheumatoidarthritis.HowbadisobesityforRA? NatRevRheumatol.2012;8:306.
21.GremeseE,CarlettoA,PadovanM,AtzeniF,RaffeinerB, GiardinaAR,etal.Obesityandreductionoftheresponserate toanti-tumornecrosisfactor␣inrheumatoidarthritis:an
approachtoapersonalizedmedicine.ArthritisCareRes (Hoboken).2013;65:94–100.
22.HeimansL,vandenBroekM,leCessieS,SiegerinkB,Riyazi N,HanKH,etal.Associationofhighbodymassindexwith decreasedtreatmentresponsetocombinationtherapyin recent-onsetrheumatoidarthritispatients.ArthritisCareRes (Hoboken).2013;65:1235–42.
23.Gómez-AmbrosiJ,SilvaC,GalofréJC,EscaladaJ,SantosS, MillánD,etal.Bodymassíndexclassificationmissessubjects withincreasedcardiometabolicriskfactorsrelatedto elevatedadiposity.IntJObes(London).2012;36:286–94. 24.KatzPP,YazdanyJ,TrupinL,SchmajukG,MargarettenM,
BartonJ,etal.Sexdifferencesinassessmentofobesityin rheumatoidarthritis.ArthritisCareRes(Hoboken). 2013;65:62–70.
25.DaoH-H.Abnormalbodycompositionphenotypesin Vietnamese’swomenwithearlyrheumatoidarthritis.In:Do Q-T,ed.Rheumatology,2011:1250–1258.
26.HunterHL,NagyTR.Bodycompositioninaseasonalmodelof obesity:longitudinalmeasuresandvalidationofDXA.Obes Res.2002;10:1180–7.
27.MazessRB,BardenHS,BisekJP,HansonJ.Dual-energyX-ray absorptiometryfortotal-bodyandregionalbone-mineraland soft-tissuecomposition.AmJClinNutr.1990;51:1106–12. 28.VisserM,PahorM,TylavskyF,KritchevskySB,CauleyJA,
NewmanAB,etal.One-andtwo-yearchangeinbody compositionasmeasuredbyDXAinapopulation-based cohortofoldermenandwomen.JApplPhysiol.1985 2003;94:2368–74.
29.WesthovensR,NijsJ,TaelmanV,DequekerJ.Body compositioninrheumatoidarthritis.BrJRheumatol. 1997;36:444–8.
30.GilesJT,LingSM,FerrucciL,BartlettSJ,AndersenRE,Towns M,etal.Abnormalbodycompositionphenotypesinolder rheumatoidarthritispatients:associationwithdisease characteristicsandpharmacotherapies.ArthritisRheum. 2008;59:807–15.
31.ArnettFC,EdworthySM,BlochDA,McShaneDJ,FriesJF, CooperNS,etal.TheAmericanRheumatismAssociation 1987revisedcriteriafortheclassificationofrheumatoid arthritis.ArthritisRheum.1988;31:315–24.
32.AletahaD,NeogiT,SilmanAJ,FunovitsJ,FelsonDT,Bingham CO3rd,etal.2010Rheumatoidarthritisclassificationcriteria: anAmericanCollegeofRheumatology/EuropeanLeague AgainstRheumatismcollaborativeinitiative.Arthritis Rheum.2010;62:2569–81.
33.Physicalstatus:theuseandinterpretationofanthropometry. ReportofaWHOExpertCommittee.WorldHealthOrganTech RepSer.1995;854:1–452.
34.AlbertiKG,ZimmetP,ShawJ.Metabolicsyndrome–anew world-widedefinition.AConsensusStatementfromthe InternationalDiabetesFederation.DiabetMed.
2006;23:469–80.
35.ValdezR.Asimplemodel-basedindexofabdominal adiposity.JClinEpidemiol.1991;44:955–6.
36.BrayG.Contemporarydiagnosisandmanagementofobesity andthemetabolicsyndrome.Newtown,PA:Handbooksin HealthCare;2003.
38.SingT,SanderO,BeerenwinkelN,LengauerT.ROCR: visualizingclassifierperformanceinR.Bioinformatics. 2005;21:3940–1.
39.KatzP,YazdanyJ,TrupinL,SchmajukG,MargarettenM, CriswellLA,etal.Genderdifferencesinassessmentofobesity inrheumatoidarthritis.ArthritisCareRes(Hoboken). 2013:62–70.
40.Obesity:preventingandmanagingtheglobalepidemic. ReportofaWHOconsultation.WorldHealthOrganTechRep Ser.2000;894,i–xii,1–253.
41.CardielMH,Pons-EstelBA,SacnunMP,WojdylaD,SauritV, MarcosJC,etal.Treatmentofearlyrheumatoidarthritisina multinationalinceptioncohortofLatinAmericanpatients: theGLADARexperience.JClinRheumatol.2012;18: 327–35.