REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
PublicaçãoOficialdaSociedadeBrasileiradeAnestesiologiawww.sba.com.br
SCIENTIFIC
ARTICLE
Effect
of
equipotent
doses
of
bupivacaine
and
ropivacaine
in
high-fat
diet
fed
neonatal
rodent
model
Ying-Dong
Lian
a,
Zong-Xiang
Chen
a,
Kang-Ru
Zhu
b,
Shu-Yin
Sun
a,
Li-Ping
Zhu
b,∗aJiningNo.1People’sHospital,DepartmentofEmergency,Jining,China bJiningNo.1People’sHospital,DepartmentofPediatrics,Jining,China
Received2April2015;accepted17August2015 Availableonline20April2016
KEYWORDS
Bupivacaine; Ropivacaine; Intrathecal anesthesia; Spinaltoxicity; Obesity
Abstract
Objectives: Theincreaseintheprevalenceofobesitypresentsasignificanthealthandeconomic problem.Obesityhasbeenreportedtobeamajorcontributortovarietyofchronicdiseases. Childhoodobesityhasbeenrisingoverthepastdecadesleading tovariouscomplicationsin health.Millionsofinfantsandchildrenundergosurgeryeveryyearonvarioushealthgrounds. Thepresentinvestigationwasundertakentoevaluatetheeffectofspinalanesthesiaof equipo-tentdosesofropivacaineandbupivacaineonover-weightneonatalrats.
Methods:The Sprague-Dawley rat pups were overfed on high fat diet to induce obesity.
Behavioralassessmentsforsensoryandmotorblockadewasmadebyevaluatingthermaland mechanicalwithdrawallatenciesatvarioustimeintervalsfollowingintrathecalinjectionsof bupivacaine (5.0mg·kg−1) andropivacaine (7.5mg·kg−1)in P14 rats. Spinal tissuewas
ana-lyzedfor apoptosisbydeterminationofactivatedcaspase-3usingmonoclonalanti-activated caspase-3andFluoro-JadeCstaining.Long-termspinalfunctioninP30ratpupswasevaluated.
Results:ExposuretointrathecalanesthesiainP14increasedthermalandmechanicallatencies andwasobservedtoincreaseapoptosisaspresentedby increaseinactivatedcaspase-3and Fluro-Jade Cpositive cells. Significantalterations inspinal function were observed inhigh fatdiet-fedpupsasagainstnon-obesecontrolpupsthatwereonstandarddiet.Bupivacaine producedmorepronouncedapoptoticeffectsonP14pups;ropivacainehoweverproducedlong lastingeffectsasevidencedinmotorfunctiontestsatP30.
Conclusion: Ropivacaineandbupivacaineinducedspinaltoxicitythatwasmorepronouncedin over-fedratpupsasagainstnormalcontrols.
©2016SociedadeBrasileiradeAnestesiologia.Publishedby ElsevierEditoraLtda.Thisisan openaccessarticleundertheCCBY-NC-NDlicense( http://creativecommons.org/licenses/by-nc-nd/4.0/).
∗Correspondingauthor.
E-mail:zhuliping278@gmail.com(L.-P.Zhu). http://dx.doi.org/10.1016/j.bjane.2015.08.006
PALAVRAS-CHAVE
Bupivacaína; Ropivacaína; Anestesiaintratecal; Toxicidademedular; Obesidade
Efeitodedosesequipotentesdebupivacaínaeropivacaínaemmodeloderoedor
neonatalalimentadocomdietaricaemgordura
Resumo
Objetivos: Oaumentodaprevalênciadaobesidadeéumproblemasériodesaúdeeeconômico. A obesidade tem sido relatada como um dos principais contribuintes para uma variedade de doenc¸as crônicas. A obesidade infantil tem aumentado nas últimasdécadas, levando a várias complicac¸õesde saúde. Milhõesde bebêsecrianc¸assãosubmetidos àcirurgia todos osanospordiversosmotivosdesaúde.Opresenteestudofoirealizadoparaavaliaroefeitoda raquianestesiacomdosesequipotentesderopivacaínaebupivacaínaemratosrecém-nascidos comsobrepeso.
Métodos: AscriasderatosSprague-Dawleyforamalimentadasemexcessocomdietaricaem gorduraparainduzirobesidade.Avaliac¸õescomportamentaisparabloqueiosensorialemotor foramfeitasatravésdaavaliac¸ão daslatênciasderetiradatérmicase mecânicasem vários intervalosde tempoapósinjec¸ões porviaintratecaldebupivacaína(5,0mg·kg−1)e
ropiva-caína(7,5mg·kg−1)emratosP14.Tecidomedularfoianalisadoparaapoptosepordeterminac¸ão
dacaspase-3ativada,usandoanticorpomonoclonalanti-caspase3ativadaeecolorac¸ãocom Fluoro-JadeC.Afunc¸ãodacolunavertebralalongoprazoemfilhotesderatosP30foiavaliada.
Resultados: A exposic¸ão à anestesia intratecal em P14 aumentou as latências térmicas e mecânicaseobservamosaumentodaapoptose,comoapresentadopeloaumentodacaspase-3 ativadaecélulaspositivasparaFluro-JadeC.Alterac¸õessignificativasdafunc¸ãodacoluna ver-tebral foramobservadasem filhotes alimentadoscomdieta ricaem gorduraversus filhotes controles não-obesos em dieta padrão. Bupivacaína produziu efeitos apoptóticos mais pro-nunciados sobreosfilhotes P14;ropivacaína,entretanto, produziuefeitos duradouros como evidenciadonostestesdefunc¸ãomotoraemP30.
Conclusão:Ropivacaínaebupivacaínainduziramtoxicidademedularmaispronunciadanos fil-hotesderatossobrealimentadosquenoscontrolesnormais.
©2016SociedadeBrasileiradeAnestesiologia.PublicadoporElsevierEditoraLtda.Este ´eum artigoOpen Accesssobumalicenc¸aCCBY-NC-ND( http://creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
Childhoodobesityisoneof themostseriouspublichealth challenges of the 21st century. The prevalence of child-hood obesity has increased at an alarming rate. Obesity affectsaround1.5billionpeoplearoundtheglobetoday1,2
ofwhich200millionarechildren.3Obeseandover-weight
childrenhavehigherchancesofdevelopingobesity-related complications.4,5
Obesity has also been reported to be associated with severalsurgicalpathologies.6 Thephysiological changesin
obesitymarkedlyaffectdistribution,binding,and elimina-tion of anesthetic drugs7---9 and severe adverse reactions
couldpossiblyresultifdrugdosingisbasedonlyontheactual bodyweightofthepatient.
Regional anesthesiaas combinedspinal---epidural anes-thesia or integratedepidural andlight general anesthesia are often employed in obese patients to lessen the risks related to airway control and postoperative respiratory depressionsthatareinducedbygeneralanestheticsor opi-oidsusedintreatmentofpain.10
Bupivacaineisusedasalocalanestheticthatisemployed innerveblock,epidural,andintrathecalanesthesiaandis oftenadministeredtocontrolpainbefore,duringandafter spinalsurgery.11Althoughextensivelyusedinpaincontrol,
bupivacaine has been reported to be cardiotoxic, neuro-toxic,andisthemostmyotoxicofthelocalanesthetics.12
Ropivacaine,anaminoamidederivativeisalocalanesthetic drugthat isstructurallyrelatedtomepivacaineand bupi-vacaine,andhastherapeuticpropertiessimilartothoseof bupivacaine but associated withless motor blockade and toxicity.13Inclinicalstudies,ropivacaineappearstobe
suit-ableforbothepiduralandregionalanesthesia.14Thepresent
study wasundertakentostudy theeffects of bupivacaine andropivacaineinover-weight/obeseneonatalrats.
Materials
and
methods
Animals
obesitybyreducinglittersizeto3pupsperlitter(small lit-ter,SL)onP6,while normallitters (NL)wereculledto10 pupsperlitter.ThepupsofSLwereprovidedaccesstohigh fat dietfromP6tillP21.Highfat dietwaspreparedwith butter,milkpowder,wheatflourandsugarinequal propor-tionseach.Theratswerefedwithhighfatdietat4g/day alongwithstandardratchow.TheanimalsofbothSL(n=36) andNL(n=36)weremonitoredcarefully.OnP14,therats weregrouped separatelyfor experiments. The NL control pups(NLC)receivednoanesthesiaandwerefedonnormal standarddietandSLcontrolpups(SLC)receivedno anesthe-siabutwerefedonhighfatdiet.ThetreatmentgroupsNL andSLpupswereinducedwithintrathecalbupivacaine(NLB andSLB)andropivacaine(NLRandSLR)onP14.OnP14,the bodyweightsofNL pupswere23---28gandthatofSLpups werebetween26and34g.
Intrathecalinjectionsofbupivacaineand ropivacaine
Withthe animals in aprone position,the spinalsolutions wereinjectedintrathecallyattheL4---L5orL5---L6levelusing a100Lsyringe(26Sgaugeneedle,model801RN;Hamilton
Company,Bonaduz,Switzerland).Intrathecalplacementof theneedletipwasconfirmedbyobservationofatailflick. Aconstantconcentrationofbupivacainewasinjecting vary-ingvolumesscaledtotheratpup’sbodyweightatadose of5.0mg·kg−1 b.wt.Ropivacaineat 7.5mg
·kg−1 b.wt.was
administered.
Behavioralassessmentsforsensoryandmotor blockade
TheP14ratsunderwentbaselinemeasurementofhindpaw thermal withdrawal latencies immediately before spinal injection. Blockade of thermal nociception was assessed usingamodifiedhotplatetestasdescribedpreviously.15,16
Hindpawswereexposedinsequence (leftthenright)toa hotplate(model39Dhotplateanalgesiameter;IITCInc., WoodlandHills,CA,USA)at52◦CforP14.Thetime
(ther-malwithdrawallatency)untiltheratsliftedtheirpawswas measuredwithastopwatch.After12s,thetestedpawwas removedbytheexperimentertoavoidinjurytotheanimal orthedevelopmentofhyperalgesia.Thistestwasrepeated threetimes(witha10spausebetweentests)foreachratat everytimepoint.Thermalwithdrawallatencieswere mea-suredevery10minforatleast40minaftertheintrathecal injection.
Blockadeofmechanicalnociceptionwasassessedbyhind paw withdrawal using von Frey filaments. The von Frey filaments apply logarithmically increasing pressure. Pups werelightlyrestrainedonaflatsurfaceandwellcalibrated von Frey hairsdevice (electronic vonFrey device, Stoelt-ing,WoodDale,IL,USA)thatdeliverincreasingmechanical stimuliwereappliedtothedorsal surfaceof thehindpaw of the pups, five times with one second intervals.17 The
number of evoked withdrawal responses toeach stimulus ofincreasingintensitywasrecordeduntilagivenstimulus evokedfiveresponsesoruntilasuprathresholdcut-off pres-surewasreached.17Mechanicalwithdrawalthresholdswere
recorded at baselineand every 10min for at least 40min
aftertheintrathecal injection anduntilfull recovery was observed.Inboththe thermalandmechanical withdrawal tests,animalswereobservedforthepossibilityofexhibiting motorblockadewithoutsensoryblockadebasedonabsence of lower limb movement accompanied by vocalization or signsofupperbodyescaperesponses.Thiswasnotobserved foranyanimal.
Motorperformanceofthelowerextremitieswasassessed byaqualitativescore.Foreachleg,iftherewasno spon-taneousorevokedmovement,thecontributiontothescore waszero.Iftherewaspartialmovement,thecontribution wasone; andif therewas normal movement, the contri-butiontothescorewastwo. Thus,insummingthevalues for both legs, thescore couldrange fromzero (complete blockade)tofour(normal).
Motorbehavioronpostnatalday30
Motorimpairment was assessed onthe P30 rats that had undergonespinal bupivacaineor ropivacaineinjections on P14.TheseratswereintroducedtoaDualspeciesEconomex Rotarod(ColumbusInstruments,Columbus,OH,USA)using a spindle rotating at 10 rotations per minute.18 Each rat
wastestedthreetimeswith10minintervalsbetweeneach assessment. The maximal latency for each trial was300s beforeremovalfromthespindle.Theaverageofthethree assessmentswasusedfordataanalysis.
Euthanasiaandperfusion
Theanimalswereeuthanizedwithintraperitonealinjection ofsodiumpentobarbital(100mg·kg−1)andperfused
trans-cardiallywithsalinefollowedby 4%paraformaldehyde 6h afterthe treatment periods ended. The spinal anesthesia groupsreceivingbupivacaineorropivocainewereperfused 6hfollowinginitiationoftheanestheticintervention.After gentledissectionofthespinalcord,thetissueswerestored overnightat 4◦C in4% paraformaldehyde and then
trans-ferred to a 30% sucrose solution at 4◦C until sectioning.
The transverse sectionsof lumbosacralspinalcord (7and 14m)werecutusingacryostat,fixedonslidesandstored
at−30◦C.
Analysisofactivatedcaspase-3
To assess apoptosis, the spinal tissue obtained from P14 animals 6h following intrathecal injection of anesthesia wasstainedforactivatedcaspase-3. Theslideswere incu-bated for 10min in 3% peroxidase, blocked with 0.3% Triton X-100 and 5% normal goat serum in Tris-buffered saline for 1h at room temperature, followed by incu-bation with rabbit monoclonal anti-activated caspase 3 (1:100;CellSignaling,Danvers,MA,USA)overnightat4◦C.
Biotinylated goat anti-rabbit secondary antibody (Vector Laboratories, Burlingame, CA, USA) wasapplied at 1:250 for 30min at room temperature. The slideswere further incubated with avidin---biotin-peroxidase complex (Vector Laboratories,Burlingame,CA)for30minanddevelopedwith 3,3′-diaminobenzidine(DAB)for8min.Theslideswere
Fluoro-JadeCstaining
Fluoro-Jade C staining was performed in 14m sections
of spinal cord that were obtained 6h following intrathe-calinjections. The staining wasdone usingFluoro-Jade C staining kit (Biosensis, USA) following the manufacturer’s instructions.Fluoro-JadeCimmunfluorescentpositivecells werecountedundertheappropriatewavelengthfluorescent microscopy.
Statisticalanalysis
Dataareexpressedasmean±SDfromatleastsix indepen-dentexperiments.ANOVA(One-wayanalysisofvariance)at
p<0.05wasconsideredstatisticallysignificant.The statis-ticalanalyseswereperformedusingSPSSsoftware(version 17.0).
Results
Animalresponsetothermalstimulus
Hindpawthermalwithdrawallatenciesweredeterminedfor P14(Fig.1B)ratsingroupsreceivingspinalbupivacaineand ropivacaine.Both0.5mg·kg−1bupivacaineand0.75mg
·kg−1
ropivacaine doses produced dense thermal nociceptive blockade at the first measurement at 10min following
20 15 10 5 0 25 20 15 10 5 Ther
mal latency (sec)
Ther
mal latency (sec)
0
Baseline 10 min 20 min
Time post spinal anesthesia
30 min 40 min Baseline 10 min 20 min
Time post spinal anesthesia
30 min 40 min
Control Bupivacaine Ropivacaine
∗
∗
∗
∗
∗
∗
∗
∗
∗
∗
∗
∗
∗
∗
∗
A
B
Figure1 (A)ThermallatencyofP14normallitterratpups fol-lowingspinalanesthesia.(B)ThermallatencyofP14smalllitter ratpupsfollowingspinalanesthesia.Valuesarerepresentedas mean±SD(n=6).*Representsstatisticalsignificanceatp<0.05 comparedagainstcontrolasdeterminedbyANOVA.
Time post spinal anesthesia (min)
Control Bupivacaine Ropivacaine 80 60 40 P a w withdr a w
al threshold (g)
20
0
0 10 20 30 40
Time post spinal anesthesia (min)
0 10 20 30 40
80 60 40 P a w withdr a w
al threshold (g)
20 0
∗
∗
∗
∗
∗
∗
∗
∗ ∗
∗
∗ ∗
∗
∗
∗
∗
A
B
Figure2 (A)PawwithdrawalthresholdofP14normallitter ratpupsfollowingspinalanesthesiadeterminedusingvonFrey filaments.(B)PawwithdrawalthresholdofP14smalllitterrat pupsfollowingspinalanesthesiadeterminedusingvonFrey fila-ments.Valuesarerepresentedasmean±SD(n=6).*Represents statisticalsignificanceatp<0.05compared againstcontrolas determinedbyANOVA.
injection compared to control and remained dense at 20min.Thethermalwithdrawallatenciesremained signifi-cantlygreaterthancontrolvaluesat30minforropivacaine than bupivacaine. However thermal withdrawal latencies remained higher onbupivacaine injection than controlat 30and40min(Fig.1A).Thelatencieswereobservedtobe markedlyhigherintheover-weightpupsadministeredwith bupivacaine or ropivacaine comparedto non-over-fed rat pups.The controlover-weightratpupsexhibitedlatencies higherthannormallittercontrolpups(Fig.1B).
Responsetomechanicalstimulus
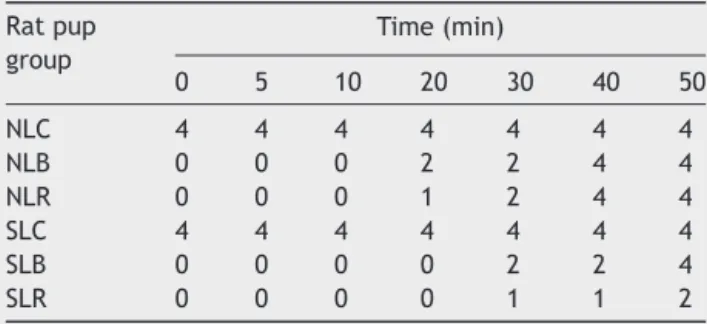
Table1 HindlegmotorresponseofP14ratsafterspinal anesthesia.
Ratpup group
Time(min)
0 5 10 20 30 40 50
NLC 4 4 4 4 4 4 4
NLB 0 0 0 2 2 4 4
NLR 0 0 0 1 2 4 4
SLC 4 4 4 4 4 4 4
SLB 0 0 0 0 2 2 4
SLR 0 0 0 0 1 1 2
Valuesarerepresentedasmean,n=6.
Scoringwas0---4points,basedonthesumofratingsforrightand leftsides.
Thescoreforeachhindleg,0=nomovement,1=partial impair-ment,and2=fullmovement.
NLC,normallittercontrolpups;NLB,normallitterpupsinduced withbupivacaine; NLR,normal litterpupsinducedwith ropi-vacaine;SLC, smalllittercontrolpups;SLB,smalllitterpups inducedwithbupivacaine;SLR,smalllitterpupsinducedwith ropivacaine.
Motorblockscores
Motor block scores are shown in Table 1. Animals that received neither ropivacaine nor bupivacaine showed no signs of motor impairment. Bupivacaine and ropivacaine produceddense motorblockin allanimalsthatrecovered almostcompletelyby40min inallNL animals.Whereasin SL animals that received intrathecal injections presented blocks in SLR and SLB even at 40min. SLR and NLR pups exhibitedmotorblocksmorethanSLBandNLBrespectively at40min(Table1).Controlanimalsthatreceivedno anes-thesia respondedtopinchwithforceps ontheskin of the backwithastartledjerksandexhibitedescapebehaviors. All animals that receivedspinal injections of bupivacaine andropivacaineexhibitednobehavioralresponsetopinch over the skin of the back at lumbar and lower thoracic levels,butshowedslightwithdrawalbehaviorstopinchat upperthoraciclevelsandontheforepawsfollowing10---15 min after injections. Animals of NL and SL groups that receivedeitherbupivacaineorropivacaineexhibitedsimilar responsestopinch.
Motorperformanceinadultratswithpostnatal anestheticexposures
P30 rats that were exposed to intrathecal injections of ropivacaineandbupivacaineat P14weretestedformotor performance using the Rota Rod apparatus. Differences observedbetweenthegroupswerenotsignificantalthough the control group that received neither ropivacaine nor bupivacaineexhibitedhighervaluesthan theothergroups (Fig.3).
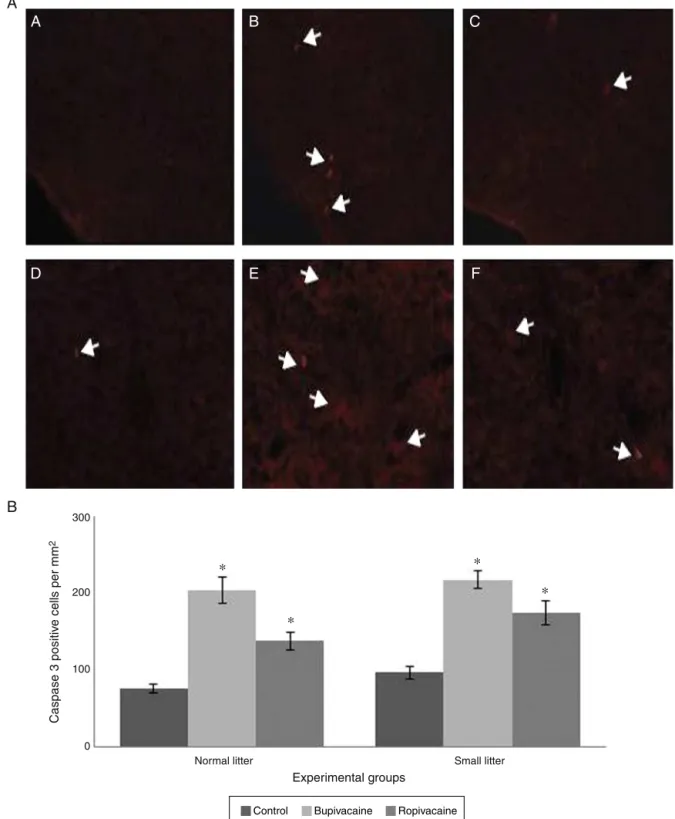
Cleavedcaspase-3andFluoro-JadeCstainingfor apoptoticneurodegeneration
Thenumberofactivatedcaspase-3andFluoro-JadeC pos-itive cells in the lumbar spinal cord of the P14 rat pups
300
200
100
0
Latency to f
all (sec)
Normal litter
Experimental groups
Small litter
Control Bupivacaine Ropivacaine
Figure3 LatencyoffallingofP30ratpupsfollowingspinal anesthesiaonP14.Valuesarerepresentedasmean±SD(n=6).
that received intrathecal injections were observed to be markedly(p<0.05) higherasagainstnormalcontrolpups. Theapoptoticcountswerehigherintheratsreceiving bupi-vacaine than ropivacaine. The counts though higher are notmarkedly different. In SLB, the apoptotic cell counts wereslightly morethan NLB.Similarresults asin bupiva-caineadministrationwereobservedbetween SLRandNLR (Figs.4and5).
Discussion
Anestheticsinduceanunconsciousstatetodevoidpainand awareness,andmillionsofchildreneachyearareexposed toanesthesia as a part of their medical care. Neverthe-less, thesafety of anesthesia in pediatric population is a matterofconcernandprevious retrospectivestudieshave reported a correlation between anesthesia exposure and learningdisabilities.19,20 Inaddition,variousanimalmodels
haveshownthatearlyanestheticexposureresultsin signif-icantlong-termbehavioraldeficits.21---23
Bupivacaine is a commonly used anesthetic for pain control in low back pain and spinal surgery. Bupivacaine binds to the intracellular sodium ions and blocks sodium influx into nerve cells which prevents depolarization.
300
200
100
0
Normal litter
Fluro-J
ade C positiv
e cells per
mm
2
Experimental groups Small litter
Control Bupivacaine Ropivacaine
∗
∗
∗
∗
A
B
C
D
B
A
300
200
100
0
Caspase 3 positiv
e cells per mm
2
Normal litter
Experimental groups
Small litter
E
F
Control Bupivacaine Ropivacaine
∗
∗
∗
∗
Figure5 Caspase-3positive cellsinthespinalcord sectionsofP14 ratpupsfollowing spinalanesthesia.Spinalcordsections revealingcaspase-3positivecells.(A)Spinalsectionofnormallittercontrolpups;(B)spinalsectionofnormallitterpupsinduced withbupivacaine;(C)spinalsectionofnormallitterpupsinducedwithropivacaine;(D)spinalsectionofsmalllittercontrolpups;(E) spinalsectionofsmalllitterpupsinducedwithbupivacaine;(F)spinalsectionofsmalllitterpupsinducedwithropivacaine.Number ofcaspase-3positivecellsinspinalcordsections.Valuesarerepresentedasmean±SD(n=6).*Representsstatisticalsignificance atp<0.05comparedagainstrespectivecontrolsasdeterminedbyANOVA.
In addition, bupivacaine is also a potent uncoupler of mitochondrialoxidativephosphorylationandthereforemay induceapoptosis.24Indeed,aprevious studydemonstrated
that a fraction of cell death caused by bupivacaine is
via apoptosis, although the main mechanism is through necrosis.25Ropivacaineisalong-actingregionalanesthetic
1monthto15yearsregardlessoftherouteof administra-tion. The overall incidence of adverse events associated withropivacaineappeared tobe low,withnauseaand/or vomitingoccurringmostfrequently.26
One of the important properties of a long-acting local anestheticistoreversiblyinhibitthenerveimpulses,thus causingaprolongedsensoryormotorblockadeappropriate foranesthesiaindifferenttypesofsurgeries.27Theresultsof
theassessmentofsensoryandmotorblocksinratpups fol-lowingintrathecalanesthesiaofropivacaineorbupivacaine suggeststhatropivacaineinducedsensoryandmotorblocks foralongerdurationthanbupivacaine.Weightofthe ani-malwasfoundtoinfluencethedegreeofsensoryandmotor blocksaswell. The over-fed mildlyobeserat pups exhib-itedhigherthermalandmechanicallatenciesasagainstthe normallyfedratspupsinducedwithintrathecalinjections. Howevertheinfluenceofweightwasobservednottoeffect onthemotor performanceof therats at P30.The results oftherotarodexperimentssuggestnosignificantvariations ontheperformanceoftheratsbetweenthevariousgroups. The thermalandmechanical latencieswere alsoobserved tofadeawayby40---50minafterinjections.
Previous studies have investigated the effect of obe-sity on spinal anesthesia, but the results have not been consistent.28---35 The observed results differed according
to the baricity of the local anesthetics and also the variable chosen for comparison between obese and non-obesepatients. Studieshave reportedpositivecorrelation betweenobesityandsensoryblocklevel.28---31,35Thusinour
studythechangesinblockadesandapoptosislevelssuggest positive relationship between obesity and sensoryblocks. ThoughtheanimalsoftheSLwerenotdesignatedasobese, thedifferenceinweightbetweentheNLgroupsdidinfluence toacertainextendtheoutcomeoftheblockadesfollowing anesthesia.The equipotentdosesofropivacaineand bupi-vacainepresented variationsin theintensity andduration ofblocksbetweentheSLandNL neverthelessropivacaine didnotcausevastalterationsbetweenthegroups.The neu-rotoxic effects of bupivacaine andropivacaine have been reportedinneonatalrats,inourstudyatP30nosignificant changeswereseenintheperformanceofthepupsofboth SLandNL,suggestingthatthedrugsdidnotcauselong-term alterations.
The neurotoxiceffectoflocalanestheticsonthespinal cordhasbeenstudiedextensivelyinadultrats.Bupivacaine appears not to be toxic to the spinal cord in older rats, althoughgeneralanesthesiahasbeenshowntoinduce apop-toticneurodegenerationintheneonatalratspinalcord.18
Cleavedcaspase-3servesasamarkerforapoptosisinthe detectionofanesthetic-induceddevelopmental neurotoxic-ity. Our observations in neonatal rats have demonstrated thatintrathecalbupivacaineandropivacainehadasimilar morphologicalandapoptoticimpactprofile.Thenumberof apoptoticcellswashigherthan control.Bupivacaine how-everinducedmuchraisedlevelsofcaspase-3positivecells asagainstropivacaine.Theextentofneurodegenerationas measuredbyFluro-JadeCstainingwasalsoinlinewiththe aboveresults.ThenumberofFluro-JadeCpositivecellsin thespinalsectionsoftheP14ratsfollowingspinalanesthesia was markedly higher than control pups. The results sug-gestbupivacaineasmoreneurotoxicthanropivacaineand bodyweightdid/doesinfluencestheextentofneurotoxicity
andapoptosis. Althoughropivacainewasfoundtoproduce long lasting blocks, it induced neuronal toxicity to some extent.
Theobservationsonthedevelopmentalneurotoxicityof anestheticagentsinlaboratoryanimalsquestiontheirsafety in clinical practices with raising over-weight of pediatric population. Further studies could be elaborated on hav-ingthoroughinvestigationsonthemechanismsinvolvedand measurestoreduceundesirablesideeffects.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.Reilly JJ. Obesity in childhood and adolescence: evidence basedclinicalandpublichealthperspectives.PostgradMedJ. 2006;82:429---37.
2.deOnisM,BlossnerM,BorghiE.Globalprevalenceandtrends ofoverweightandobesityamongpreschoolchildren.AmJClin Nutr.2010;92:1257---64.
3.WHO Fact Sheet: childhood overweight and obesity. http://www.who.int/dietphysicalactivity/childhood/en/ [accessed17.03.13].
4.GuoSS,WuW,ChumleaWC,etal.Predictingoverweightand obesityinadulthoodfrombodymassindexvaluesinchildhood andadolescence.AmJClinNutr.2002;76:653---8.
5.NaderPR,O’BrienM,HoutsR,etal.Identifyingriskforobesity inearlychildhood.Pediatrics.2006;118:e594---601.
6.BjorntorpP.Obesity.Lancet.1997;350:423---6.
7.AbernethyDR,GreenblattDJ.Drugdispositioninobesehumans. Anupdate.ClinPharmacokinet.1986;11:199---213.
8.AdamsJP,MurphyPG.Obesityinanaesthesiaandintensivecare. BrJAnaesthesiol.2000;85:91---108.
9.CheymolG.Effectsofobesityonpharmacokineticsimplications fordrugtherapy.ClinPharmacokinet.2000;39:215---31. 10.Kuczkowski KM, Benumof JL. Repeat cesarean section in a
morbidly obese parturient: a new anesthetic option. Acta AnaesthesiolScand.2002;46:753---4.
11.Sice PJ, Chan D, MacIntyre PA. Epidural analgesia after spinal surgery via intervertebral foramen. Br J Anaesth. 2005;94:378---80.
12.MorganMM.Clinicalanaesthesiology.4thed.NewYork:Lange MedicalBooks/McGraw-Hill;2006.p.263---75.
13.Markham A, Faulds D. Ropivacaine: a review of its phar-macology and therapeutic use inregional anesthesia.Drugs. 1996;52:429---49.
14.Catterall WA, Mackie K. Local anesthetics. In: Brunton LL, ParkerKL,BlumenthalDK,BuxtonILO,editors.Goodmanand Gilman’sManualofPharmacologyandTherapeutics.NewYork, NY:McGraw-HillMedicalPublishing;2008.p.241---52. 15.HuD,HuR,BerdeCB.Neurologicevaluationofinfantandadult
ratsbeforeand aftersciaticnerveblockade. Anesthesiology. 1997;86:957---65.
16.KohaneD,SankarW,ShubinaM,etal.Sciaticnerveblockadein infant,adolescent,andadultrats:acomparisonofropivacaine withbupivacaine.Anesthesiology.1998;89:1199---208. 17.Walker SM, Howard RF, Keay KA, et al. Developmental age
influencestheeffectofepiduraldexmedetomidineon inflam-matory hyperalgesia in rat pups. Anesthesiology. 2005;102: 1226---34.
19.WilderRT,FlickRP,SprungJ,etal.Earlyexposureto anesthe-siaandlearningdisabilitiesinapopulation-basedbirthcohort. Anesthesiology.2009;110:796---804.
20.FlickRP,KatusicSK,ColliganRC,etal.Cognitiveand behav-ioraloutcomesafterearlyexposuretoanesthesiaandsurgery. Pediatrics.2011;128:e1053---61.
21.Jevtovic-TodorovicV,HartmanRE,IzumiY,etal.Earlyexposure tocommonanestheticagentscauseswidespread neurodegener-ationinthedevelopingratbrainandpersistentlearningdeficits. JNeurosci.2003;23:876---82.
22.BrambrinkAM,EversAS,AvidanMS,etal.Isoflurane-induced neuroapoptosisintheneonatalrhesusmacaquebrain. Anesthe-siology.2010;112:834---41.
23.GentryKR,SteeleLM,SedenskyMM,etal.Earlydevelopmental exposureto volatileanestheticscausesbehavioral defectsin Caenorhabditiselegans.AnesthAnalg.2013;116:185---9. 24.Sun X, Garlid KD. On the mechanism by which bupivacaine
conductsprotonsacrossthemembranesofmitochondriaand liposomes.JBiolChem.1992;267:19147---54.
25.LeeH,SowaG,VoN,etal.Effectofbupivacaineon interver-tebraldisccellviability.SpineJ.2010;10:159---66.
26.BosenbergA, ThomasJ, LopezT, etal. Theefficacyof cau-dalropivacaine1,2and3mg/mlforpostoperativeanalgesiain children.PaediatrAnaesth.2002;12:53---8.
27.HansenTG.Ropivacaine:apharmacologicalreview.ExpertRev Neurother.2004;4:781---91.
28.PitkanenMT.Bodymassandspreadofspinalanesthesiawith bupivacaine.AnesthAnalg.1987;66:127---31.
29.SchniderTW,MintoCF,BruckertH,etal.Population pharma-codynamicmodelingandcovariatedetectionforcentralneural blockade.Anesthesiology.1996;85:502---12.
30.McCullochWJ, Littlewood DG.Influenceofobesity on spinal analgesia with isobaric 0.5% bupivacaine. Br J Anaesth. 1986;58:610---4.
31.TaivainenT, TuominenM,RosenbergPH.Influenceofobesity onthespreadofspinalanalgesiaafterinjectionofplain0.5% bupivacaine at the L3---4 or L4---5 interspace. Br J Anaesth. 1990;64:542---6.
32.BarclayDL,RenegarOJ,NelsonEWJr.Theinfluenceofinferior venacavacompressiononthelevelofspinalanesthesia.AmJ ObstetGynecol.1968;101:792---800.
33.CarvalhoB,Collins J,DroverDR,et al.ED(50)andED(95)of intrathecalbupivacaineinmorbidlyobesepatientsundergoing cesareandelivery.Anesthesiology.2011;114:529---35.
34.Kim WH, Lee JH, Ko JS, et al. The effect of body mass indexonspinalanaesthesiafortotalkneereplacement arthro-plasty:adose---responsestudy.AnaesthIntensiveCare.2012;40: 410---6.