REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
PublicaçãoOficialdaSociedadeBrasileiradeAnestesiologiawww.sba.com.br
SCIENTIFIC
ARTICLE
Comparison
of
the
effects
of
sugammadex
and
neostigmine
on
postoperative
nausea
and
vomiting
夽
Özgür
Ya˘
gan
a,∗,
Nilay
Tas
¸
a,
Tu˘
gc
¸e
Mutlu
a,
Volkan
Hancı
baOrduUniversity,SchoolofMedicine,DepartmentofAnesthesiology,Ordu,Turkey
bDokuzEylulUniversity,SchoolofMedicine,DepartmentofAnesthesiology,Alsancak,Izmir,Turkey
Received18February2015;accepted17August2015
Availableonline19March2016
KEYWORDS
Sugammadex; Neostigmine; Postoperative; Nausea; Vomiting
Abstract
Backgroundandobjectives: The aimofourstudy istocompare theeffectsofsugammadex andneostigmine,usedforneuromuscularblockageantagonism,onpostoperativenauseaand vomiting(PONV).
Methods:Ourstudywascompletedwith98ASAI-IIriskpatientsundergoingendotracheal intu-bationundergeneralanesthesia.Attheendofthesurgerypatientswererandomlydividedinto twogroupsgiven2mgkg−1sugammadex(GroupS)or50gkg−1neostigmineplus0.2mgkg−1 atropine(GroupN).Monitoringandrecordingtimesweresetas1hourpostoperativeandfrom 1---6,6---12,and12---24hours.Theanti-emeticamountsadministeredwererecorded.
Results:In the firsthourpostoperative 13 patients inGroupN (27%)and 4inGroupS (8%) wereobservedtohavenauseaand/orvomitingandthedifferencewasstatisticallysignificant (p=0.0016).Duringthe24hoursofmonitoringtherewasnosignificantdifferenceinthe inci-denceandseverityofPONV(p>0.05),howeverthenumberofpatientsgivenondansetronfor PONVtreatmentinGroupNwasstatisticallysignificantlyhigherthanthenumberinGroupS (16inGroupN,6inGroupS,p<0.011).
Conclusions: Attheendofourstudycomparingneostigminewithsugammadexfor neuromus-cularblockageantagonism,wefounduseofsugammadexhadlowerincidenceofPONVinthe postoperative1sthourandlessanti-emeticusein24hoursofmonitoring.
©2016SociedadeBrasileiradeAnestesiologia.Publishedby ElsevierEditoraLtda.Thisisan openaccessarticleundertheCCBY-NC-NDlicense( http://creativecommons.org/licenses/by-nc-nd/4.0/).
夽 ThisstudywascarriedoutatOrduUniversityEducationandTrainingHospital. ∗Correspondingauthor.
E-mail:ozguryagan@hotmail.com(Ö.Ya˘gan).
http://dx.doi.org/10.1016/j.bjane.2015.08.003
PALAVRAS-CHAVE
Sugammadex; Neostigmina; Pós-operatório; Náusea; Vômito
Comparac¸ãodosefeitosdesugamadexeneostigminaemnáuseaevômito nopós-operatório
Resumo
Justificativaeobjetivos: Oobjetivodenossoestudofoicompararosefeitosdesugamadexe neostigmina,usadosparaoantagonismodobloqueioneuromuscularemnáuseaevômitono pós-operatório(NVPO).
Métodos: Oestudofoiconcluídocom98pacientesderiscoASAI-II,submetidosàintubac¸ão traquealsobanestesiageral.Aofinaldacirurgia,ospacientesforamaleatoriamentedivididos emdoisgruposquereceberam2mgkg−1desugamadex(GrupoA)ou50gkg−1deneostigmina mais0,2mgkg−1deatropina(GrupoN).Ostemposdemonitorac¸ãoeregistroforamdefinidos como1horadepós-operatórioede1-6,6-12e12-24horas.Asquantidadesadministradasde antieméticosforamregistradas.
Resultados: Naprimeirahoradepós-operatório,13pacientesdoGrupoN(27%)e4doGrupo S (8%) apresentaram náusea e/ou vômito e a diferenc¸a foi estatisticamente significativa (p=0,0016).Nãohouve diferenc¸asignificativanaincidência egravidadedeNVPO (p>0,05) duranteas24horasdemonitorac¸ão,porémonúmerodepacientesquerecebeuondansetron paraotratamentodeNVPOnoGrupoNfoiestatísticaesignificativamentemaiorqueonúmero depacientesnoGrupoS(16e6,respectivamente,p<0,011).
Conclusões:Aofinaldoestudoquandocomparamosneostigminacomsugamadexparao antag-onismodobloqueioneuromusculardescobrimosquesugamadexapresentoumenorincidência deNVPOnaprimeirahoradepós-operatórioeconsumomenordeantieméticoem24horasde monitorac¸ão.
©2016SociedadeBrasileiradeAnestesiologia.PublicadoporElsevierEditoraLtda.Este ´eum artigoOpen Accesssobumalicenc¸aCCBY-NC-ND( http://creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
Postoperative nausea and vomiting (PONV) has been one ofthemostimportantproblemsofanesthesiathroughthe years.Kapur1describedPONVasthe‘‘BigLittleProblem’’ in 1991.While Watcha2 touchedonKapur’s definition, he summarized hisownviews of PONVasthe ‘‘Big Big Prob-lem’’. PONV is one of most common complications after generalanesthesiathatmaycauseincreasedmorbidityand prolonged hospital stay.3 Duration of anesthesia, type of surgery, postoperative analgesia with opioids, as well as patientrelatedfactorssuchasage,gender,smokinghabits and previous history of PONV and of motion sickness are knownasriskfactorsfordevelopingPONV.3---5
Neuromuscularblockermedicationsareanecessarypart ofgeneralanesthesia.Additionallyattheendofthesurgical procedurethemajority oftimestheresidual neuromuscu-larblockisreversedwithacetylcholineesteraseinhibitors.6 Cholinesteraseinhibitorshavebeenimplicatedinthe devel-opment of PONV as a result of their potent muscarinic effects upon the gastrointestinal tract and the vomiting center in the brain.7 Neostigmine, used at the end of surgeryforresidualneuromuscularblock,isassociatedwith increasedthe riskof PONV, especiallywhen usedin large doses(>2.5mg).7Somepreviousstudieshaverecommended avoiding the use of acetyl choline esterase inhibitors to reducepostoperativevomiting.8
Sugammadexis a ␥ cyclodextrin agent that selectively
bindssteroidalneuromuscularblockerssuchasrocuronium. Bymakingcomplexeswithrocuroniumincirculationandat
neuromuscularjunction,itenablestheexcretionofthedrug in the urine without metabolization.9 Sugammadex gives risetosafe andrapidreversal of neuromuscularblockade inducedbyrocuronium.10,11Sugammadexisknownasasafe drugwithoutanyknownserioussideeffects.Thecommon side effects of sugammadex areminimal cough, oral dis-comfort, hypersensitivity, temporary QT prolongation and temporary(<30min)activatedpartialthromboplastintime prolongation.12 The studies onthe effectsofsugammadex onPONVareverylimited.13
Thehypothesisofourstudyisthatuseofsugammadexto antagonizetheeffectsofneuromuscularblockeragentswill reducepostoperativenauseaandvomitingwhencompared withneostigmine. Withthe aim of testing thishypothesis weaimedtocomparetheeffectsof2mgkg−1sugammadex
and 50gkg−1 neostigmineonthe incidenceof PONV. We
defined the major outcome as presence of PONV at the postoperativeonehourperiodandnumberofpatientswho wereneededondansetronforsymptomatictreatmentduring 24hourspostoperativeperiod.
Method
Declaration of Helsinki. Written informed consent was obtainedfromallpatientsparticipatinginthestudy.
Exclusion criteria were including neurosurgery, laparo-scopic,oncologic,gynecologic,breast,strabismusandmid ear surgery, history of drug and alcohol abuse, body massindex(BMI)>30kgm−2,useofanalgesics,sedativeor
antiemeticdrugswithin24hoursbeforesurgery,psychiatric and neurological disorders, allergy or contraindication of studydrugs.Additionallypatientswithmorethantwohours surgerytimewerealsoexcluded.
Nopreanaestheticmedicationwasadministered.Inthe operatingroom, patients were monitored with ECG, non-invasive arterialpressure, peripheralO2 saturation(SpO2)
andend-tidalCO2levels(Mindray,BeneViewT8,Shenzhen,
PR China). An intravenous line of 10mLkg−1 ringers
lac-tate solutionwasinfusedvia 20G venous cannulathrough the dorsum of the nondominant hand. Using a computer generated sequence of numbers and a sealed envelope technique, patientswere randomly dividedinto 2groups: patients who received neostigmine/atropine combination (GroupN,n=50)orsugammadex(GroupS,n=50)for rever-sal ofneuromuscular blockade.Neuromuscularmonitoring wascarriedoutusingTOFWatchSX® (OrganonLtd.,Dublin,
Ireland)acceleromyography,withskinelectrodeslocatedat theulnarnervetracefor contractionsofadductorpollicis muscle.
Before the operations to assess the PONV risks of patients, the simplified Apfel scoring system was used: (gender: male:0, female:1)+(history of PONV or motion sickness: no:0, yes:1)+(smoking status: no:0, yes:1)+(anticipated use of postoperative opioids: no:0, yes:1).14 Patients witha score of two weregiven 4mg iv dexamethasone (Deksamet 8mg/2mL, Osel ˙Ilac¸, Beykoz, ˙Istanbul) before induction, while patients witha scoreof 3 and above were additionally given 4mg iv ondansetron (Ondaren4mg/2mL,Vem ˙Ilac¸,Mecidiyeköy, ˙Istanbul)atthe endofsurgery.15
Generalanesthesiawasinducedbyiv1gkg−1fentanyl
and 2.5mgkg−1 propofol. With the loss of consciousness
(loss of eyelash reflex), iv 0.6mgkg−1 rocuronium was
applied. Orotracheal intubation was performed when no responsewasyieldedwithTrain ofFour(TOF) stimulation of TOF-Guard. Afterintubation the patientwas mechani-callyventilatedinthecontrolledmodewheretheend-tidal CO2 pressure was kept between 35 and 40mmHg.
Anes-thesia wasmaintained with 2% sevoflurane in 50% O2/air
mixture and 0.2---0.7gkg−1min−1 iv remifentanil
infu-sion.Additionalivbolusof0.1---0.2mgkg−1rocuroniumwas
administeredduring surgical procedure providedthatTOF ratiotobe10% orlower. Noneuromuscularblockeragent was used if the remaining time to the end of surgery waslessthan30minutes.Atthe endofthesurgery, anes-theticdrugadministrationwasceasedandthepatientwas manually ventilated with 100% oxygen. According to the randomization schedule,antagonization of neuromuscular blockadewas providedwithintravenousadministrationof 0.05mgkg−1neostigmineand0.02mgkg−1atropineforthe
patients in Group N and 2mgkg−1 sugammadex for the
patientsinGroupSwhenreappearanceofthesecondtwitch (T2)on the TOF.The patients were extubated after aspi-ration of oropharyngeal secretions withthe 90% recovery ofTOFvalue.Additionalivadministrationof0.025mgkg−1
neostigmine and 0.01mgkg−1 atropine in Group N and
2mgkg−1 sugammadexin Group S wasplanned in case of
need(shouldtheTOFvaluestayunder90%after5minutes). In all patients iv 1 gr paracetamol (Parol 10mgmL−1,
Atabay, Kadıköy, ˙Istanbul) infusion was administered for postoperativeanalgesiaatend ofthesurgery andevery8 hoursin firstpostoperativeday. Painwasassessedusinga visual analog scale (VAS) from1 to10. Intravenous 50mg dexketoprofen (Arveles 50mg/2mL, Ufsa ˙Ilac¸, Topkapı, ˙Istanbul) wasgivenonwhen VAS score>4. Administration ofiv1mgkg−1tramadol(Contramal50mgmL−1,A˙I,Sarıyer,
˙Istanbul)forpostoperativeanalgesiawereplannedasrescue agents.
Thepatientsweremonitoredandassessedfor24hours; hourlyforthefirst6hours,every2hoursinthe6---12hours intervaland,subsequently,every4hours.Theywereasked specifically about pain, nausea, vomiting and other side effect.Inallpatients,nauseaandvomitingwereassessed by the same researcher (NT) using a four point verbal descriptivescale as described in previous studies: 0=not nauseated,1=nauseated,notvomiting,2=nauseated,one totwoepisodesofvomiting,3=nauseated,morethantwo episodesofvomitingduringtheobservationperiod).16
Inthepresenceof continuingnausea(>5min)oractive vomiting,iv4mgondansetronwasadministered,ifnotgiven asprophylactic.Ifondansetronwaspreviouslyadministered themedicationwasnotgivenagainwithin6hoursbut meto-clopramide0.2mgkg−1wasgiveninstead.
Patientcharacteristics, typeofsurgery, amountof opi-oidconsumptionanddurationofanesthesiawererecorded. Complicationsafterthesurgery suchasheadache,cough, respiratory depression, hypertension, bradycardia, sore throat,gastrointestinalsystemcomplaintswerealsonoted. HRbelow50pulsemin−1wasconsideredasbradycardiaand
managed with 0.5mg iv atropine. MAP above 125mmHg wasconsideredashypertension andmanaged with0.1mg ivnitroglycerin.
Poweranalysis
Inaprevious study,16 theincidenceof PONVwasreported as30%withthesameneostigminedoseasourstudywhileit was11%withplacebo.Accordingtoanevaluationbasedon athisstudy,44patientsineachgroupwouldberequiredin ordertodetect20%changewith80%powerand5% signifi-cance(˛=0.05,ˇ=0.80)intwowaysignificantinteractions (Minitab13.1Inc.,StateCollege,PA,USA).Weplannedto include100patientsinthisstudytoallowfordropouts.
Statisticalanalysis
Table1 Patientsandclinicalcharacteristics. GroupN
n=48
GroupS n=50
p
Age(yr) 40.8±11.2 40.3±13.3 NS Weight(kg) 73±9.2 71±10.5 NS BMI(kgm−2) 23.9±3.5 22.8±3.6 NS
Gender(F/M) 18/30 16/34 NS
ASAI/II 37/11 36/14 NS
Apfelscore 0/1/2/3(n)
14/20/14/0 16/19/15/0 NS
Surgerytime (min)
49.9±22.3 54.7±22.0 NS
Remifentanil consumption (g)
624±196 681±186 NS
NS,notsignificant;BMI,Bodymassindex;F/M,female/male; ASA,AmericanSocietyofAnesthesiologist.
Dataarepresentedasmean±SDorfrequencies.
sideeffects.Avalueofp<0.05wasacceptedasstatistically significant.
Results
The study included two groups with 50 patients in each group.TwopatientsinGroupNwereexcludedfromthestudy astheirsurgerieslastedmorethan2hours.Thedemographic datainbothgroupsweresimilar(Table1).Therewasno sig-nificantdifferencebetweenthepatientsintermsofPONV risk scores, surgical durations and consumed remifentanil amounts(Table1).InGroupN,24patients(50%)underwent head and neck surgery, 13 (27%) had urology, 4 (8%) had orthopedic and 7 patients (15%) hadgeneral surgery pro-cedures.InGroupS, 29patients(58%) hadheadandneck surgery,11 (22%)hadurology,5(10%) hadorthopedicand 5patients(10%)hadgeneralsurgeryprocedures.Therewas nostatisticallysignificantdifferencebetweenthegroupsin termsoftypeofsurgeryundergone(p>0.05).
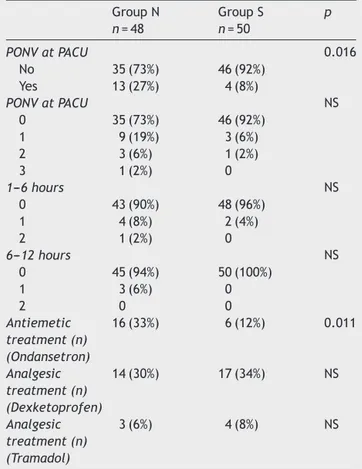
Inthepostanesthesiacareunit(PACU)during1hour post-operative monitoring,13 patients in Group N(27%) and4 patientsinGroup S(8%)hadnauseaand/or vomiting.The ratewashigherbyastatisticallysignificantdegreeinGroup N(p=0.016). In the later 24 hour monitoring, there was nostatisticallysignificant differenceobserved inthe inci-denceandseverityofPONVbetween thegroups(p>0.05,
Table2).Howeverthenumberofpatientsgivenondansetron inGroupNwassignificantlyhigh(16patientsinGroupN,6in GroupS,p=0.011).Thepostoperativeanalgesictreatments inbothgroupsweresimilar(Table2).Therewasno signifi-cantdifferencebetweenthegroupsintermsofsideeffects (Table3).
Discussion
In our study comparing the effects of sugammadex and neostigmine,usedtoantagonizetheeffectsof neuromus-cularblockeragents,onincidenceofpostoperativenausea and vomiting, less PONV was observed in the first hour postoperative with the use of sugammadex compared to
Table2 Incidenceandseverity ofPONV andantiemetic andanalgesictreatmentingroups.
GroupN n=48
GroupS n=50
p
PONVatPACU 0.016
No 35(73%) 46(92%)
Yes 13(27%) 4(8%)
PONVatPACU NS
0 35(73%) 46(92%)
1 9(19%) 3(6%)
2 3(6%) 1(2%)
3 1(2%) 0
1---6hours NS
0 43(90%) 48(96%)
1 4(8%) 2(4%)
2 1(2%) 0
6---12hours NS
0 45(94%) 50(100%)
1 3(6%) 0
2 0 0
Antiemetic treatment(n) (Ondansetron)
16(33%) 6(12%) 0.011
Analgesic treatment(n) (Dexketoprofen)
14(30%) 17(34%) NS
Analgesic treatment(n) (Tramadol)
3(6%) 4(8%) NS
Dataarepresentedasfrequencies.PONV,Postoperativenausea andvomiting;PACU,Postanestheticcareunit.PONVwas evalu-atedasfollows:0=notnauseated,1=nauseated,notvomiting, 2=nauseated,onetotwoepisodesofvomiting,3=nauseated, morethantwoepisodesofvomiting.
Table3 Postoperativesideeffects. GroupN n=48
GroupS n=50
p
Headache 4(8%) 2(4%) NS
Hypertension 2(4%) 3(6%) NS
Bradycardia 2(4%) 0 NS
Coughing 2(4%) 0 NS
Shivering 0 1(2%) NS
Sorethroat 1(2%) 0 NS
Respiratorydepression 2(4%) 0 NS
Dataarepresentedasfrequencies.
neostigmine.Ourcasesadministeredsugammadexhada sig-nificantreductionintheamountofanti-emeticsusedinthe first24hourspostoperativecomparedwithcases adminis-teredneostigmine.
32%andvomitingby47%to11%intheneostigmine-atropine group.Dingetal.18 studiedlaparoscopictuballigationand foundsignificantlymorePONVinthePACUwhenneostigmine wascomparedwithplacebo aftermivacurium, 65%versus 25%respectively.Meta-analysesdemonstratethathigh-dose neostigmine(>2.5mg)isassociatedwithincreasedPONVand thatreducingthedosecandecreasePONVrisk.7,19
However,theclinicalimportanceofneostigmine’seffects onPONVhasbeenquestioned.Theresultsofameta-analysis studyincluding15studies,foundtheevidencethat neostig-mine increased the risk of PONV to be insufficient.20 A studyresearchingtheeffectsofneostigmineonPONVafter abdominalhysterectomyoperationsleftonegroupto spon-taneouslyrecoverfromneuromuscularblockageinducedby mivacurium while the other group was antagonized with 2mgneostigmine.Theydidnotfindasignificantdifference betweenthegroupsintermsofbothnauseaandvomiting.In conclusiontheystatedthattheuseofneostigminefor neu-romuscularblockantagonismdidnotincreasetheincidence orseverityofPONV.21Ithasbeenreportedthat neuromuscu-larblockantagonismwith2mgneostigmineinlaparoscopic gynecological operationsdid notcause an increase in the incidence of PONV.22 The noticeable point in these two studies is the amount of neostigmine used. It has been determinedthatuseofneostigmineindosesabove2.5mg increasestheriskofPONV.7,15-17
A study by Lovstad et al.16 compared the effect of 50gkg−1 dose of neostigmine with a placebo group on
PONVin womenafterlaparoscopicgynecologyoperations. Attheendofsurgeryallpatientsweregiveniv0.05mgkg−1
ondansetron. In the first 6 hours they found the nau-sea rate in the neostigmine group was 30%, while in the placebogroupthis ratewas11%. Thenecessity forrescue anti-emetic medication (metoclopramide 0.2mgkg−1 and
droperidol0.025mgkg−1)was28%intheneostigminegroup
and7%intheplacebogroup.Theyreportedthatboththese differences were statistically significant. The researchers didnotfindasignificantdifferenceinvomitingratesinthe first6hours.Monitoringfrom6to24hours,theso-calledlate period,observednosignificant differenceineithernausea orvomiting.Inconclusionthisstudyreportedthathighdose neostigmineforneuromuscularblockageantagonismcaused an increasein theriskof nauseainthefirst 6hoursafter surgery for women undergoinglaparoscopic surgery, even withondansetronprophylaxis.Thedoseofneostigmineused inthisstudy,whentheweightofthepatientsinthestudyis takenintoaccount,isabovethe2.5mgdosestatedtocause anincreasedriskofPONV.
Thestudiesassessingtheeffectonpostoperativenausea andvomitingwhensugammadexandneostigmineareused toreversetheeffectofneuromuscularblockeragentsare verylimited.According tothe resultsof astudy assessing postoperative results of neuromuscular blockage antago-nism and including 1440 patients (772 sugammadex, 212 neostigmine,510noreversal),theincidenceofPONVinthe PACUwasfoundtobesignificantlyhighintheneostigmine groupcomparedtothesugammadexgroup(21.5%vs.13.6%,
p<0.05). The researchers did not determine any signifi-cantdifferencebetweenthesugammadexandno-reversal groups.Inastudywhichreportedtheuseofintraoperative anti-emeticswasmorefrequentintheneostigminegroup, theyemphasizedthatthecauseofincreasedriskof PONV
inthesugammadexgroupwasurgentsurgeryand abdomi-nalsurgicalprocedures.Whentheresearchersassessedthe resultsofthestudytheystatedthatthecostincreasecaused byuseofsugammadexwasoff-setbythereductionin inci-denceofPONV.23
A study by Koyuncu et al.13 compared the effects of 70gkg−1neostigmineand2mgkg−1sugammadexonPONV
whenusedfor neuromuscularblockage antagonismin 100 patients undergoing extremity surgery. In the study with inductionofanesthesiausingpropofol,fentanyland rocuro-niumwhilemaintenanceuseddesfluraneandnitrousoxide withoxygen, 0.5mgkg−1 iv meperidine wasadministered
attheendofsurgeryforpostoperativeanalgesia.Theydid notadministerintraoperativeanti-emeticmedication.PONV wastreated with4mgondansetron iv and ifit continued 10mg metoclopramide iv. When the findings of the study areevaluated,thoughtherewasnodifferenceinanesthesia durationsandApfelscoresofpatients,theystatedthatthe nauseaandvomitingscoresinthePACUwerestatistically sig-nificantlylowerinthesugammadexgroup.Howeverduring 24hourspostoperativenauseaandvomitingwasobservedin 60%ofthesugammadexgroupand58%oftheneostigmine groupandtheyreportedtherewasnosignificantdifference. Inconclusioncomparingsugammadexwithneostigminethey determinedthat therewasa slightand temporary reduc-tionintheincidenceofPONV.Theydidnotfindapositive effectofthereturnofgastrointestinalfunctionsand ambu-lation.TheresearcherslinkedtheirhighratesofPONV,when comparedtotheliterature,totheuseofnitrousoxidefor anesthesiamaintenanceandtheuseofopioidsfor postop-erativeanalgesia.13
The results of our study are similar to the study by Koyuncuetal.13 in identifying alower PONVincidence in the1sthourofmonitoringinPACUwithsugammadex. How-everinthe24hourmonitoringperiod,thestudybyKoyuncu etal. had differentand higher results than in the litera-ture andour study.In our study duringthe postoperative 1---6hours the nausea and vomiting incidence was 10% in GroupNand4% inGroupS, whilebetween6and24hours itwas found tobe6% in Group N and0% in Group S. We believethebasicreasonforthedifferencesfromtheresults ofKoyuncuetal.isthatinsituationswithApfelscoreof2 andaboveweadministeredantiemeticmedication.Another importantreasonmaybetheamountofneostigmineused. Koyuncuetal.used70gkg−1 intheirstudy.In ourstudy
thedoseofneostigminewas50gkg−1,whichissimilarto
manystudiesintheliterature.7,16,20Whenthemeanweights areconsidered,themeanamountofneostigmineusedper patientinourstudywas3.65mg,whilethiswas5.25mgin thestudybyKoyuncuetal.Otherpossiblereasonsmaybe listedasdifferencesinanestheticmethod(wedidnotuse N2Oformaintenanceormeperidineforpostoperative
anal-gesia)andourshorterdurationofsurgery(about30minutes shorter).Ithasbeendeterminedthattheincreaseinsurgical durationmayincreasetheincidenceofPONV(each30min increaseindurationincreasesPONVriskby60%,sothata baselineriskof10%isincreasedby16%after30min).10
anti-emeticmedicationadministrationinthePACUforthe sugammadexgroup.
Themostimportantlimitationofourstudyisthatthough we didnot include surgeries knowntobe risk factors for PONV,itwasnotcompletedwithasingletypeofsurgery.
Inconclusion,thisstudyshowsthatneostigminereversal in increased PONV at PACU and use of antiemetic rescue medicationduringthepostoperative24 hours.Interms of PONV,theuseofsugammadexfor neuromuscularblockage antagonismmay beabetter choicefor patientswithhigh riskorwherethissituationisundesirable.
Clinical
trial
registration
NCT02286752.
Ethics
committee
approval
Ethicscommitteeapprovalwasreceivedforthisstudyfrom EthicsCommitteeofOndokuzMayısUniversity(2014/779).
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.Kapur PA. The big ‘‘little problem’’. Anesth Analg. 1991;73:243---5.
2.Watcha MF, White PF. Postoperative nausea and vomi-ting.Itsetiology,treatment,and prevention.Anesthesiology. 1992;77:162---84.
3.KennyGN.Riskfactorsforpostoperativenauseaandvomiting. Anaesthesia.1994;49:6---10.
4.ApfelCC,GreimCA,HaubitzI,etal.Ariskscoretopredictthe probabilityofpostoperativevomitinginadults.Acta Anaesthe-siolScand.1998;42:495---501.
5.ApfelCC,GreimCA,HaubitzI,etal.Thediscriminatingpowerof ariskscoreforpostoperativevomitinginadultsundergoing var-ioustypesofsurgery.ActaAnaesthesiolScand.1998;42:502---9. 6.FigueredoE,CanosaL.Prophylacticondansetronfor postopera-tiveemesis.Meta-analysisofitseffectivenessinpatientswith previous history of postoperativenausea and vomiting.Acta AnaesthesiolScand.1999;43:637---44.
7.TramerMR,Fuchs-BuderT. Omittingreversalof neuromuscu-larblockade:effectonpostoperativenauseaandvomitingand risk of residual paralysis: a systemic review. Br J Anaesth. 1999;82:379---86.
8.Jokela R,KoivurantaM.Tropisetronordroperidolinthe pre-ventionofpostoperativenauseaandvomiting.Acomparative,
randomised, double-blind study in women undergoing laparoscopic cholecystectomy. Acta Anaesthesiol Scand. 1999;43:645---50.
9.de Boer HD, van Egmond J, van de Pol F, et al. Chemical encapsulationofrocuroniumbysyntheticcyclodextrin deriva-tives:reversalofneuromuscularblockinanaesthetizedRhesus monkeys.BrJAnaesth.2006;96:201---6.
10.GijsenberghF,RamaelS,HouwingN,etal.Firsthumanexposure ofOrg25969,anovelagenttoreversetheactionofrocuronium bromide.Anesthesiology.2005;103:695---703.
11.SorgenfreiIF,NorrildK,LarsenPB,etal.Reversalof rocuronium-inducedneuromuscularblockbytheselectiverelaxantbinding agentsugammadex:adose-findingandsafetystudy. Anesthesi-ology.2006;104:667---74.
12.Mirakhur RK. Sugammadex in clinical practice. Anaesthesia. 2009;64:45---54.
13.KoyuncuO, TurhanogluS, Ozbakis,etal. Comparisonof sug-ammadexand conventionalreversalonpostoperativenausea and vomiting: a randomized, blinded trial. J Clin Anesth. 2015;27:51---6.
14.ApfelCC,LaaraE,KoivurantaM,etal.Asimplifiedriskscorefor predictingpostoperativenauseaandvomiting.Anesthesiology. 1999;91:693---700.
15.GanTJ,MeyerTA,ApfelCC,etal.SocietyforAmbulatory Anes-thesiaguidelinesforthemanagementofpostoperativenausea andvomiting.AnesthAnalg.2007;105:1615---28.
16.Løvstad RZ, ThagaardKS, Berner NS, et al. Neostigmine 50 microgkg(-1)withglycopyrrolateincreasespostoperative nau-seainwomenafterlaparoscopicgynaecologicalsurgery.Acta AnaesthesiolScand.2001;45:495---500.
17.King MJ, Milazkiewicz R, Carli F, Deacock AR. Influence of neostigmine on postoperative vomiting. Br J Anaesth. 1988;61:403---6.
18.Ding Y, Fredman B, White PF. Use of mivacurium during laparoscopicsurgery:effectofreversaldrugsonpostoperative recovery.AnesthAnalg.1994;78:450---4.
19.HoKM,IsmailH,LeeKC,etal.Useofintrathecalneostigmine asanadjuncttootherspinalmedicationsinperioperativeand peripartumanalgesia:ameta-analysis.AnaesthIntensiveCare. 2005;33:41---53.
20.ChengCR,SesslerDI,ApfelCC.Doesneostigmineadministration produceaclinicallyimportantincreaseinpostoperativenausea andvomiting?AnesthAnalg.2005;101:1349---55.
21.HovorkaJ,KorttilaK,NelskyläK,etal.Reversalof neuromus-cularblockadewithneostigminehasnoeffectontheincidence orseverityofpostoperativenauseaandvomiting.AnesthAnalg. 1997;85:1359---61.
22.NelskyläK,Yli-HankalaA,SoikkeliA,etal.Neostigminewith glycopyrrolatedoesnotincreasetheincidence orseverityof postoperativenauseaand vomitinginoutpatients undergoing gynaecologicallaparoscopy.BrJAnaesth.1998;81:757---60. 23.LedowskiT, FalkeL, JohnstonF, et al. Retrospective