REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
OfficialPublicationoftheBrazilianSocietyofAnesthesiologywww.sba.com.br
SCIENTIFIC
ARTICLE
Preanesthetic
assessment
data
do
not
influence
the
time
for
tracheal
intubation
with
Airtraq
TM
video
laryngoscope
in
obese
patients
夽
Dante
Ranieri
Jr.
a,∗,
Fabio
Riefel
Zinelli
a,
Adecir
Geraldo
Neubauer
a,
Andre
P.
Schneider
a,
Paulo
do
Nascimento
Jr.
baDepartmentofAnesthesioloy,HospitaldoCorac¸ãodeBalneárioCamboriu,BalneárioCamboriu,SC,Brazil
bDepartmentofAnesthesioloy,FalcudadedeMedicianadeBotucatu(FMB-Unesp),SãoPaulo,SC,Brazil
Received27October2012;accepted21November2012 Availableonline7March2014
KEYWORDS
Obesity; Intubation; Laryngoscopy; AirtraqTM
Abstract
Purpose:thisstudyinvestigatedtheinfluenceofanatomicalpredictorsondifficultlaryngoscopy andorotrachealintubationinobesepatients bycomparingMacintosh andAirtraqTM laryngo-scopes.
Methods:from132bariatricsurgerypatients(bodymassindex≥35kgm−1),cervicalperimeter, sternomentaldistance,interincisordistance,andMallampatiscorewererecorded.Thepatients wererandomizedinto twogroups accordingtowhetheraMacintosh (n=64)oranAirtraqTM (n=68)laryngoscopewasusedfortrachealintubation.Timerequiredforintubationwasthefirst outcome.Cormack---Lehanescore,numberofintubationattempts,theMacintoshbladeused, anyneedforexternaltrachealcompressionortheuseofgumelasticbougiewererecorded. Intubationfailureandstrategiesadoptedwerealsoregistered.
Results:intubation failed in two patients in the Macintosh laryngoscope group, and these patients were included as worst cases scenario. The intubation times were 36.9+22.8s and13.7+3.1s fortheMacintosh andAirtraqTM laryngoscope groups(p<0.01),respectively. Cormack---LehanescoreswerealsolowerfortheAirtraqTMgroup.OnepatientintheMacintosh groupwithintubationfailurewasquicklyintubatedwiththeAirtraqTM.Cervicalcircumference (p<0.01)andinterincisordistance(p<0.05)influencedthetimerequiredforintubationinthe MacintoshgroupbutnotintheAirtraqTMgroup.
Conclusion:inobesepatientsdespiteincreasedneckcircumferenceandlimitedmouthopening, theAirtraqTMlaryngoscopeaffordsfastertrachealintubationthantheMacintoshlaryngoscope, anditmayserveasanalternativewhenconventionallaryngoscopyfails.
©2014SociedadeBrasileiradeAnestesiologia.PublishedbyElsevier EditoraLtda.Allrights reserved.
夽 StudyconductedattheDepartmentofAnesthesiology,HospitaldoCorac¸ãodeBalneárioCamboriu,BalneárioCamboriu,SC,Brazil. ∗Correspondingauthor.
E-mail:deranieri@terra.com.br(D.RanieriJr.).
0104-0014/$–seefrontmatter©2014SociedadeBrasileiradeAnestesiologia.PublishedbyElsevierEditoraLtda.Allrightsreserved.
Airtraq anddifficultairwaypredictorsinobesepatients 191
Introduction
Difficultiesin airwaymanagement area concernin obese
patients.1,2Anatomicalcharacteristicssuchascervicaland
occipitalfataccumulation,tonguesize,airwaynarrowing,
limitedneckextension,andlimitedmouthopeningare
fac-torsthat maketrachealintubation moredifficultin obese
patientsthaninthosewithalowerbodymassindex.3,4These
factorshavebeendesignedtopredictdifficultlaryngoscopy
andintubation.
Several devices can beused tofacilitate intubation in
patients withconditions suchasobesity.AirtraqTM (Prodol
Medic; Biscay, Spain) is a disposable video laryngoscope
designed to provide vocal cord visualization without the
needtoalignthemouthandpharynxwiththetrachealaxis,
and has been in clinical use since 2006.5 In several
stud-ies, AirtraqTM has proven to be better than conventional
laryngoscopesforpatientswithcertainconditions,including
obesity.6---8
The difficult airway anatomical predictors are useful
when the Macintoshlaryngoscope is used; however, when
videolaryngoscopyisemployedthesepredictorsare
uncer-tain. Thus, the aim of this study was to investigate the
influenceofdemographicdataandanatomical
characteris-ticsofobesepatientsinairwaymanagementbycomparing
the Macintosh laryngoscope and AirtraqTM video
laryngo-scope.
Materials
and
methods
After receiving approval from the Institutional Research
Ethics Committee, and registering at Australian and New
ZealandClinicalTrials(ANZCT,12610000136000),candidates
aged18---60yearswereinvitedtoparticipateinthisstudy.
Allpatientsprovidedinformedconsentandtheparticipants
wereASA I---III(American Society ofAnesthesiologists) and
hadabodymassindex(BMI)≥35kg/m2.Patientswitha
his-toryofuntreatedgastro-oesophagealreflux,succinylcholine
intolerance, or previous difficult or unfeasible intubation
were excluded. At preanesthetic assessment, Mallampati
score,9 interincisor distance, sternomental distance, and
neckcircumferenceatthelevelofthethyroidcartilagewere
recorded.
The patients were given ranitidine 50mg and
meto-clopramide 10mg intravenously1h beforesurgery. In the
operating room after monitoring and prior to anesthesia
induction,thepatientswererandomlyassigned(withsealed
opaqueenvelopes)tooneof thetwogroups, accordingto
thedevicetobeusedfortrachealintubation:Macintoshor
AirtraqTMlaryngoscope.Patientmonitoringincluded
contin-uouselectrocardiography(EKG),pulseoximetry(SpO2)and
non-invasivebloodpressure.
Thepatientswereplacedintherampedposition,which
began at the lumbar region and progressed to the
sub-scapular and suboccipital areas, to keep the auditory
meatus above the sternal manubrium and the shoulders
according to the description by Collins and colleagues.10
After a 3-min pre-oxygenation, anesthesia was induced
with2.0g/kgfentanyl and2.0mg/kg propofol.Afterthe
corneal---palpebralreflexwaslost,thepatientsweregiven
succinylcholine1.0mg/kg.Thepropofoldosewasadjusted
accordingtocorrectedweight(22height×height).11
Intuba-tionwasperformedatcompletecessationofvisiblemuscle
twitching andwasconfirmed by capnography curve.Then
0.1mg/kg vecuronium was injected, and anesthesia was
maintainedbytheadministrationofsevoflurane(2%---3%)in
amixtureofoxygenandair(FiO2=0.4).
The intubation was performed by four participating
senioranesthesiologistswithmorethan4 yearsof clinical
experiencewithconventional laryngoscopy and AirtraqTM.
Themaximumtimepermittedforintubationwas120s.
Anes-thesiologistsusingtheMacintoshlaryngoscopewerefreeto
choosethebladesize(3,4,or5)andinthecaseoffailure,
anewintubationattempt wasperformed withadifferent
blade size. The regular AirtraqTM (size 3) wasused in all
casesinthisgroup.
Optimizingmaneuverforthelaryngoscopywasthe
Back-ward, Upward, Rightward Pressure (BURP) maneuver.12
Intubation failures were recorded, and the alternative
device could be used. Thus, patients who could not be
intubatedwiththe Macintosh laryngoscope couldbe then
intubated with the AirtraqTM, and vice versa. For cases
whereintubationcouldnotbeperformedwitheitherdevice,
or for cases where facemask ventilation posed difficulty,
a laryngeal mask airway (FastrackTM) or a flexible
bron-choscope could be used. Alternatively, the patient could
be awakened and the surgery rescheduled. For women,
7.5-diameterlubricatedtrachealtubeswereused,and
8.5-diameterwasusedformen.
Timein secondsfromthemomentthe anesthesiologist
pickedupthedevice(MacintoshlaryngoscopeorAirtraqTM)
until cuff inflation was our primary outcome. Other
sec-ondary outcomes were the Cormack---Lehane scores13 as
reportedbytheanesthesiologist;thenumberofintubation
attempts;thenumberoftheMacintoshbladeused;anyneed
forexternaltrachealcompressionbymeansofaBURP
per-formedbyanassistant,ortheuseofagumelasticbougie;
andintubationfailureandthestrategiesadopted.
The number of participants in this study was
calcu-latedconsideringaminimumtimedifferenceforintubation
of 21s with a standard deviation of 27s, in a series of
20 obese patients intubated with Macintosh laryngoscope
or AirtraqTM, derived from the experienceof members of
our group in a pilot study. A total of 126 patients were
requiredtoproduce asignificant differencewitha power
of 0.9 and ˛=0.05. Student’s t-tests were used for
com-paringcontinuous variablewithaBonferronicorrection as
appropriate.The Mann---WhitneyUtestwasappliedtothe
Cormack---Lehanescore.Chi-squaredtestswereappliedto
categorical variables. Demographic and anatomical
varia-bles were analyzed to verify their influence on the time
requiredforintubation.Forthispurpose,themultiplelinear
regressionmethodwithdummyvariableswasused,and
cor-relationcoefficient(r)foreachgroupandvariableisshown.
Valuesof p<0.05 were definedasstatistically significant.
The STATISTICA version6, 2001 (StatSoft, Inc.Tulsa,OK),
wasused.
Results
From158initiallyselectedpatients,26wereexcluded.
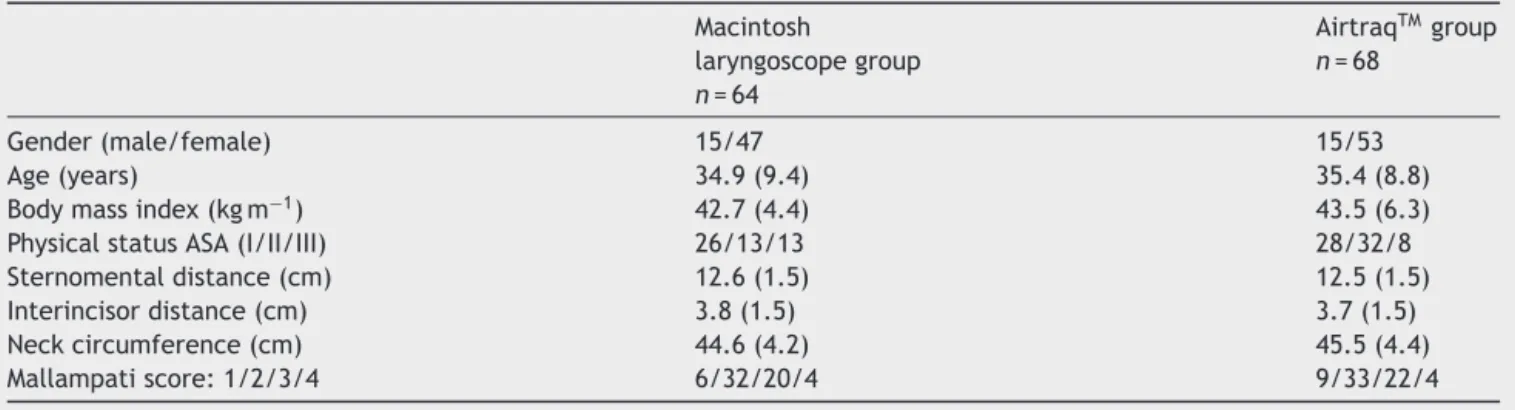
Table1 Demographicdataandairwayanatomicalmeasurements.Valuesareexpressedasthemeans(standarddeviation)or counts(gender,physicalstatus,andMallampatiscore).
Macintosh
laryngoscopegroup
n=64
AirtraqTMgroup
n=68
Gender(male/female) 15/47 15/53
Age(years) 34.9(9.4) 35.4(8.8)
Bodymassindex(kgm−1) 42.7(4.4) 43.5(6.3)
PhysicalstatusASA(I/II/III) 26/13/13 28/32/8
Sternomentaldistance(cm) 12.6(1.5) 12.5(1.5)
Interincisordistance(cm) 3.8(1.5) 3.7(1.5)
Neckcircumference(cm) 44.6(4.2) 45.5(4.4)
Mallampatiscore:1/2/3/4 6/32/20/4 9/33/22/4
requiredsedativesbeforeenteringtheoperatingroom.The AirtraqTMgroupconsistedof68patients,eachofwhomwas
successfullyintubatedwithintheestablishedmaximumtime of120s.TheMacintoshlaryngoscopegroupconsistedof64 patients,but2weretreatedconsideringtheworst-case sce-narioduetofailed trachealintubation (intentiontotreat analysis)(Fig.1).
The groups were homogeneous with respect to
demo-graphicandairwayanatomicalvariables(Table1).
Thetimerequiredforintubationwassignificantlylonger
withthe Macintosh laryngoscope (36.9±22.8s) than with
the AirtraqTM (13.7±3.1s), (p<0.01). In the Macintosh
group, 13, 39, and 10 patients were subjected to
intu-bation with blades of size 3, 4, and 5, respectively. In
eight patients, the first attempt to intubate was
unsuc-cessfulandthe blade wasreplacedwitha largerone;for
fourof these,blade 4waschangedtoblade5,andinthe
remaining4,blade3waschangedtoblade4.Considering
these eight patients, a BURP maneuver was required for
6,andof these,agum elasticbougiewasalsoneededfor
1 patient.For 2 patients in the Macintosh group,
intuba-tioncould not beaccomplished within120s. One patient
required three attempts with blades 4 and 5, and this
patient had a Cormack---Lehane score IV. After facemask
Assessed for eligibility
n=158
Excluded: n=26 Refused to participate: n=19 Other reasons: n=7
Randomisation
Allocated to AirtraqTM group
n=68 Allocated to macintosh
laryngoscope group n=64 Excluded from analysis secondary to intubation fail
n=2 Assigned to final analysis
n=62
Figure1 Patientsflowchart.
ventilation,thispatientwasintubatedwithin30susingthe
AirtraqTM,resultinginaCormack---Lehane scoreI.Another
patient exhibited bronchospasm, received facemask
ven-tilation until spontaneous respiration recovered, and the
procedurewaspostponed.Thedataonairwaymanagement
arepresentedinTable2.
The following factors did not have a significant
influ-ence on the time required for intubation: age (p=0.39),
sex (p=0.07), BMI (p=0.91), and sternomental distance
(p=0.17).Neckcircumference(p<0.01)(Fig.2)and
inter-incisor distance (p<0.05) (Fig. 3) did have a significant
influenceonthetimerequiredforintubationwiththe
Mac-intoshlaryngoscope,butnotfortheAirtraqTM.
Discussion
Inthisstudy,increasedcervicalcircumferencesignificantly
influencedthetimeforintubationwiththeMacintosh
laryn-goscopebutnotfortheAirtraqTM.
The minimum interincisor distance recommended for
AirtraqTM oralintroductionis2cm.7,14 The interincisor
dis-tance only influenced the time required for intubation
with the Macintosh laryngoscope, thus revealing that the
AirtraqTM can be used for patients with a limited mouth
opening.
Table2 Time forintubationexpressedasthe meanand standard deviation.Number oflaryngoscopies attempted, needtoperformtheBURPmaneuver(backuprightposition) andCormack---Lehanescores reportedby the anesthesiolo-gistexpressedastotalnumbersofpatients.
Macintosh
laryngoscopegroup
n=64
AirtraqTMgroup
n=68
Timeforintubation (seconds)*
36.9(22.8)* 13.7(3.1)*
Laryngoscopy attempts:1/2/3
54/6/2 68/0/0
BURPmaneuver 6 0
Cormack---Lehane score:I/II/III/IV
37/20/4/1 65/3/0/0
Airtraq anddifficultairwaypredictorsinobesepatients 193
120
100
80
60
40
20
0
0 34 36 38 40
Macintosh AirtrackTM 42 44 46 48
Cervical perimeter (cm)
Time f
or intubation (seconds)
50 52 54 56
Figure2 Adjustedcorrelationsfortherelationshipbetween cervicalperimeter andintubationtime, accordingto intuba-tionmethodfortheMacintoshlaryngoscopeversustheAirtraqTM (p<0.01).
Studiesthathaveanalyzedintubationinobesepatients
havecomparedvideolaryngoscopeswithasingleMacintosh
laryngoscope blade size.6---8,14 In our study, the
anesthesi-ologistsselected theMacintoshblade sizes basedontheir
experience and clinical judgment,and theyalso had the
option to change the blade as needed. Blade changing
occurredduetotheinability toinsertitproperlyintothe
vallecula;asmanyobeseindividuals arealsotall,blade 3
120
100
80
60
40
20
0
0.0 0.5 1.0 2.0 3.0 4.0
Interincisor distance (cm)
Time f
or intubation (seconds)
5.0 6.0
1.5 2.5 3.5 4.5 5.5 6.5
Macintosh AirtrackTM
Figure3 Adjustedcorrelationsfortherelationshipbetween interincisordistanceandintubationtime,accordingto intuba-tionmethodfortheMacintoshlaryngoscopeversustheAirtraqTM (p<0.05).
(andeven blade 4) may not provide adequate vocal cord
visualization.
Onenovel finding fromourstudy is that theincreased
neckcircumference and limitedmouth opening made the
MacintoshlaryngoscopelessefficientthantheAirtraqTMfor
obesepatients.Increasedcervicalcircumferencehasbeen
associated with intubation difficulty using the Macintosh
laryngoscope.4,15
Randomizedtrialswithobesepatientsobservedthatthe
timerequired for intubation wassignificantly longer with
the Macintosh when compared with video laryngoscopes.
Thetimerequiredfortrachealintubationusingthe
Pentax-AWS was significantly longer than that for the Macintosh
laryngoscope(38vs26sonaverage),16 andtheintubation
lasted significantly longer with GlideScope than
Macin-tosh laryngoscope (48 vs 32s).17 Otherwise laryngoscopic
Cormack---Lehaneviewsweresignificantlybetterwithvideo
laryngoscopes. In two patients direct laryngoscopy failed
andtheyweresubsequentlyintubatedwithGlideScope
with-outproblems.
Inthesestudiestimetointubatewasdefinedasthetime
elapsingbetweentheinsertionofthelaryngoscopeintothe
oralcavityandregistrationofexpiredCO2.Inourstudy
dura-tionofintubationwasdefinedasthetimefromgrippingthe
deviceandtrachealtubecuffinflation.Thismayexplainthe
veryshortintubationtimewiththeAirtraqTMinthepresent
report.Recordedstartandendtimesforintubationarenot
consistentamongseveralstudies,soabsolutecomparisons
aredifficult.
The common tests designed to predict difficult
laryn-goscopyareofuncertainrelevancewhenvideolaryngoscopy
isemployedandthenewdeviceswillprobablybesafer.18,19
Wewouldstressthat theCormack&Lehane gradewas
describedwhenMacintoshlaryngoscopewereused,andthe
importancetofindaspecificlaryngealviewgraduationfor
thevideolaryngoscopes.20,21Thesedeviceshave
particular-itiesintheirdesignsandproceduresforintubation
Videolaryngoscopesmaybeadvantageouscomparedto
theMacintoshlaryngoscopebecausetheycanbeusedunder
awakeconditionswithadequatetopicalairwayanesthesia,
orwhenthepatientislightlysedated.22ThustheAirtraqTM
islessexpensiveandeasiertostoreandhandlethan
bron-choscopes.Asvideolaryngoscopesarerigid,theycanpush
awayexcesstissue,secretionsorblood,therebyallowinga
betterviewofthevocalcords.23
Thisstudyhasseverallimitations.Wedidnotuse
Intuba-tionDifficultyScale-IDS,24whichismentionedquiteoftenin
theliterature.WechosetousetheCormack---Lehanescore
and the time required for intubation, which are strongly
relatedtoclinical practiceevaluation.We monitoredonly
clinicallytheintubationconditionswithnonervestimulator
techniqueforneuromuscularblockade.Althoughthestudy
wasrandomized,itwasimpossibletoblindtheoperatorto
theairwaydevicebeingused.
We conclude that in obese patients, some anatomical
characteristics, such ascervical circumference and
inter-incisor distance, do not influence the time required for
intubation with the AirtraqTM, but these factors must be
takenintoaccountwhenusingtheMacintoshlaryngoscope.
The use of the AirtraqTM would be considered when the
Macintoshlaryngoscopeintubationisunsuccessfulforobese
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
Acknowledgments
Prof.LeoLynceprovidedstatisticalsupportforthestudy.
References
1.JuvinP,LavautE,DupontH,etal.Difficulttrachealintubation ismorecommoninobesethaninleanpatients.AnesthAnalg. 2003;97:595---600.
2.DarginJ,MedzonR.Emergencydepartmentmanagementofthe airwayinobeseadults.AnnEmergMed.2010;56:95---104.
3.Wilson ME. Predicting difficult intubation. Br J Anaesth. 1993;71:333---4.
4.KimWH,AhnHJ,LeeCJ,etal.Neckcircumferenceto thyro-mentaldistanceratio:anewpredictorofdifficultintubationin obesepatients.BrJAnaesth.2011;106:743---8.
5.MaharajCH,O’CroininD,CurleyG,etal.Acomparisonof tra-chealintubationusingtheAirtraqortheMacintoshlaryngoscope inroutineairwaymanagement:arandomised,controlled clini-caltrial.Anaesthesia.2006;61:1093---9.
6.Ndoko SK,Amathieu R, TualL, et al. Tracheal intubationof morbidlyobesepatients:arandomizedtrialcomparing perfor-manceofMacintoshandAirtraqlaryngoscopes.BrJAnaesth. 2008;100:263---8.
7.DhonneurG,NdokoS,AmathieuR,etal.Trachealintubation using theAirtraqinmorbidobesepatientsundergoing emer-gencycesareandelivery.Anesthesiology.2007;106:629---30.
8.RanieriJrD,FilhoSM,BatistaS,etal.Comparisonof Macin-toshandAirtraqTMlaryngoscopes inobesepatientsplacedin therampedposition.Anaesthesia.2012;67:980---5.
9.Mallampati SR, Gatt SP, Gugino LD, et al. A clinicalsign to predictdifficulttrachealintubation:aprospectivestudy.Can AnaesthSocJ.1985;32:429---34.
10.CollinsJS,LemmensHJ,BrodskyJB,etal.Laryngoscopyand morbidobesity:a comparisonofthe‘‘sniff’’and ‘‘ramped’’ positions.ObesSurg.2004;14:1171---5.
11.LemmensHJ,BrodskyJB,BernsteinDP.Estimatingidealbody weight----anewformula.ObesSurg.2005;15:1082---3.
12.KnillRL.Difficultlaryngoscopymadeeasywitha‘‘BURP’’.Can JAnaesth.1993;40:279---82.
13.CormackRS,LehaneJ.Difficulttrachealintubationin obstet-rics.Anaesthesia.1984;39:1105---11.
14.DhonneurG,AbdiW,NdokoSK,etal.Video-assistedversus con-ventionaltrachealintubationinmorbidlyobesepatients.Obes Surg.2009;19:1096---101.
15.GonzalezH,MinvilleV,DelanoueK,etal.Theimportanceof increasedneckcircumferencetointubationdifficultiesinobese patients.AnesthAnalg.2008;106:1132---6.
16.AbdallahR,GalwayU,YouJ,etal.Arandomizedcomparison between thePentax AWSvideolaryngoscope and the Macin-toshlaryngoscopeinmorbidly obese patients.Anesth Analg. 2011;113:1082---7.
17.Andersen LH, Rovsing L, Olsen KS. GlideScope video laryn-goscope vs. Macintosh direct laryngoscope for intubation of morbidlyobesepatients:arandomizedtrial.ActaAnaesthesiol Scand.2011;55:1090---7.
18.MartinF,BuggyDJ.Newairwayequipment:opportunitiesfor enhancedsafety.BrJAnaesth.2009;102:734---8.
19.AmathieuR,CombesX,AbdiW,etal.Analgorithmfordifficult airwaymanagement,modifiedformodernopticaldevices (Air-traqlaryngoscope;LMACTrach):a2-yearprospectivevalidation inpatients for elective abdominal, gynecologic,and thyroid surgery.Anesthesiology.2011;114:25---33.
20.FerckCM,LeeG.laryngoscopy:timetochangeourview. Anaes-thesia.2009;64:351---4.
21.Mines R, Ahmand I. Can you compare the views of video laryngoscopes to the Macintosh laryngoscope. Anesthesia. 2011;66:315---6.
22.UakritdathikarnT, AsampinawatT, WanasuwannakulT, et al. AwakeintubationwithAirtraqLaryngoscopeinamorbidlyobese patient.JMedAssocThai.2008;91:564---7.
23.Moore AR,Schricker T, Court O. Awakevideo laryngoscopy----assistedtrachealintubationofthemorbidlyobese.Anaesthesia. 2012;67:232---5.