REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
PublicaçãoOficialdaSociedadeBrasileiradeAnestesiologiawww.sba.com.br
SCIENTIFIC
ARTICLE
Non-invasive
mechanical
ventilation
after
the
successful
weaning:
a
comparison
with
the
venturi
mask
Esra
Adıyeke,
Asu
Ozgultekin,
Guldem
Turan
∗,
Altay
Iskender,
Gamze
Canpolat,
Abdullah
Pektas
¸,
Osman
Ekinci
HaydarpasaNumuneTeachingandResearchHospital,DepartmentofICU,Istanbul,Turkey
Received6April2014;accepted11November2014 Availableonline20October2015
KEYWORDS
Artificialrespiration;
Weaning;
Criticalcare
Abstract
Backgroundandobjectives: Thisstudycomparedtheratesofacuterespiratoryfailure, rein-tubation,length ofintensive care stay andmortality inpatients inwhom thenon-invasive mechanicalventilation(NIMV)wasappliedinsteadoftheroutineventurifacemask(VM) appli-cationafterasuccessfulweaning.
Methods:Followingtheapprovalofthehospitalethicscommittee,62patientswhowereunder mechanicalventilationfor atleast48hourswere scheduledforthisstudy.12patients were excludedbecauseoftheweaningfailureduringT-tubetrial.Thepatientswhohadoptimum weaningcriteriaaftertheT-tubetrialof30minuteswereextubated.Thepatientswerekepton VMfor1hourtoobservethehemodynamicandrespiratorystability.Thegroupof50patients whowere successfultoweanrandomlyallocatedtohaveeitherVM (n=25),orNIV(n=25). Systolicarterialpressure (SAP),heart rate(HR),respiratory rate(RR), PaO2,PCO2, andpH
valueswererecorded.
Results:ThenumberofpatientswhodevelopedrespiratoryfailureintheNIVgroupwas sig-nificantlylessthanVMgroupofpatients(3reintubationvs.14NIV+5reintubationintheVM group).ThelengthofstayintheICUwasalsosignificantlyshorterinNIVgroup(5.2±4.9vs. 16.7±7.7days).
Conclusions:TheratiooftherespiratoryfailureandthelengthofstayintheICUwerelower when non-invasive mechanicalventilationwas used after extubation evenif the patient is regardedas‘successfullyweaned’.WerecommendtheuseofNIMVinsuchpatientstoavoid unexpectedventilatorfailure.
©2015SociedadeBrasileiradeAnestesiologia.PublishedbyElsevierEditoraLtda.Thisisan openaccessarticleundertheCCBY-NC-NDlicense( http://creativecommons.org/licenses/by-nc-nd/4.0/).
∗Correspondingauthor.
E-mail:gturanmd@yahoo.com(G.Turan). http://dx.doi.org/10.1016/j.bjane.2014.11.008
PALAVRAS-CHAVE
Respirac¸ãoartificial;
Desmame;
Cuidadosintensivos
Ventilac¸ãomecânicanãoinvasivaapósdesmamebem-sucedido:umacomparac¸ão comamáscaradeVenturi
Resumo
Justificativaeobjetivos: Esteestudocomparouastaxas deinsuficiênciarespiratória aguda, reintubac¸ão,tempodeinternac¸ãoemUTIemortalidadeempacientessobventilac¸ãomecânica não invasiva(VMNI)em vezdahabitualmáscarafacialdeVenturi(MV)apósdesmame bem-sucedido.
Métodos: Apósa aprovac¸ãodo Comitêde Ética dohospital, 62 pacientesqueestavam sob ventilac¸ão mecânica porno mínimo 48 horasforam inscritosneste estudo.Doze pacientes foramexcluídosdevidoàfalhadedesmameduranteotestedetubo-T.Ospacientesque apre-sentaramcritériosdedesmameótimosapósotestedetubo-Tde30minutosforamextubados. OspacientesforammantidosemMVpor1horaparaobservac¸ãodaestabilidadehemodinâmica erespiratória.Ogrupode50pacientesqueobtiveramsucessonodesmameventilatórioforam alocadosaleatoriamenteparaMV(n=25)ouVNI(n=25).Osvaloresdepressãoarterialsistólica (PAS),frequênciacardíaca(FC),frequênciarespiratória(FR),PaO2,PCO2epHforam
registra-dos.
Resultados: OnúmerodepacientesquedesenvolveuinsuficiênciarespiratórianogrupoVNIfoi significativamente menorqueodo grupoMV (3reintubac¸ões vs.14 VNI+5reintubac¸ões no grupoMV).OtempodepermanênciaemUTItambémfoisignificativamentemenornogrupoNIV (5,2±4,9vs.16,7±7,7dias).
Conclusões: AstaxasdeinsuficiênciarespiratóriaedotempodepermanênciaemUTIforam menoresquandoaventilac¸ãomecânicanãoinvasivafoiusadaapósaextubac¸ão,mesmoseo pacienteforconsideradocomo‘‘desmamebem-sucedido’’.RecomendamosousodeVMNIem taispacientesparaevitarafalhainesperadadoventilador.
©2015SociedadeBrasileiradeAnestesiologia.PublicadoporElsevierEditoraLtda.Este ´eum artigo OpenAccess sobumalicenc¸aCCBY-NC-ND( http://creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
Non-invasiveventilationtakesaroleindifferentstagesof treatmentinintensivecareunits.Thismethodiscommonly usedasanalternativetoinvasiveventilationinpatientswho areclinicallystablebutsufferfromacutehypercapnic respi-ratory failure.1---3 NIV is also usedfor premature weaning andpostextubationrespiratoryfailureandpositiveresults onreintubationand durationof intensivecare unitstayis reported.4
Inthisstudy,weaimedtodetermineifprophylacticNIV appliedto thepatients whowere extubated according to thestandardizedweaningcriteriaandwhowere appropri-ateforfollowingwithventurefacemask(VM)wouldmake anydifferenceintermsofrespiratoryfailureafter extuba-tion,reintubation,durationofintensivecareunitstayand mortality.
Materials
and
methods
Sixty-two patients above18-yearsoldwhowere admitted to intensive care unit with acute respiratory failure and treated with invasive mechanical ventilatory support for morethan48hwereincludedinthestudy.Patientswhose APACHEII(AcutePhysiologyandChronicHealthEvaluation II) score above 25, GCS (Glasgow Coma Scale) below 13 andwhohavecontraindicationsforNIV(patientswith max-illofacial trauma, gastrointestinal obstruction and severe
secretion),severeirreversibleorganfailureandpregnancy were excluded from the study. Demographic data, diag-nosis,comorbidities, andAPACHEII scores of thepatients wererecorded.Weaningwasplannedforthepatientswho haveoptimalconditions:CPAPmodewithinvasivemechanic ventilationsupportwhohaveFiO≤40,PaO2≥60,PEEP≤5, SO2≥90 and not having inotrope support; systolic arte-rial pressurebetween 70 and 180mmHg,peak heart rate between50and140min,respiratoryrate<25min,GCS≥13. Patientswhofulfilledthesecriteriaweretakenunder spon-taneous respiratory trial with T-part for 30min. Arterial bloodgaswasevaluatedafter30minspontaneous respira-torytrial.Ifhemodynamicandrespiratoryparameterswere stable,patientswereextubatedandsupportedwithO2by VM.Patientswerefollowedupforanhourtoobserve suffi-ciencyintermsofweaningandtheoneswhohadSO2≥90, systolicarterialpressurebetween70and180mmHg,peak heartratebetween50and140min,respiratoryrate<25min wereincluded inthestudy.Thepatientswerechoseninto thegroupsaccordingtotheadmissionnumberashavingodd orevennumber.
group. Mechanical ventilation parameters of the patients supportedbyNIVweresetasIPAP:13---15cmH2Ovs.EPAP: 3---5cmH2Oaccordingtopatientcompliance.Differenttypes ofNIVmasks(full-faceandoronasal-foreheador chin sup-ported) were chosen for application in order to provide patientcomfortandcompliance.Duringthefollow-up,low dosedexmedetomidinesedation(0.2---0.5mg/kg/hinfusion) wasplannedtobeinitiatedifthepatient’sincompliancewas preventingNIVtobeeffective.
Arterial pressure, pulse, respiratory rate and arterial blood gas parameters were recorded before extubation, underIMVinCPAPmode;inthe30thminuteofT-piecetrial; andafterextubationin1st,2nd,3rd,4th,5th,6th,12th, 24th,48th hoursin all patients. Complications(vomiting, airwayobstruction,regurgitation,etc.)wererecorded.
InGroupVM,patientswhodidnothaverespiratoryfailure andintubationindicationbutdevelopedrespiratory deterio-rationandslighthypoxia(respiratoryrate>25min,SO2≤95, PaO2≤70mmHg)weresupportedwithNIV;whilepatientsin bothgroupswhohadrespiratoryfailureandintubation indi-cation (respiratory rate>35min, SO2<90, PaO2<60mmHg andhemodynamicfailure)werereintubated.
Continuityof weaningsuccess,respiratoryfailureafter extubation, reintubation, duration of intensive care unit stay and mortality rates are compared between two groups.
During the evaluation of the data obtained from the study,SPSS(StatisticalPackageforSocialSciences)for Win-dows 20.0 program was used for the statistical analysis. DistributionofvariableswascontrolledbyusingKolmogorov Smirnov Test. During the evaluation of the study data, regardingthe comparisonsof descriptivestatistical meth-ods(frequency,rate,mean,andstandarddeviation)aswell asquantitative data, Studentt test and Mann Whitney U
tests were used. Chi-square test was used regarding the comparisonofthequalitativedata.Pairedsamplettestand Wilcoxontestswereusedforrepetitivemeasurements.The resultsobtainedfromthestudywereevaluatedwithin95% confidenceintervals andat asignificance level ofp<0.05 level.
Results
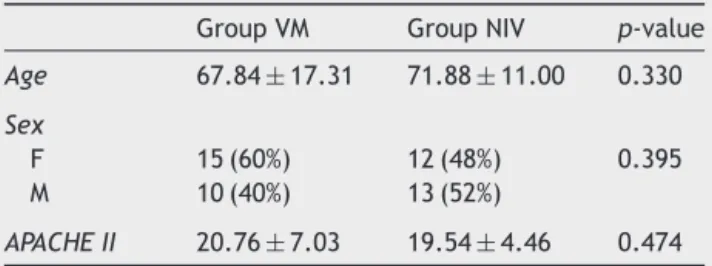
Thestudywasconductedon62patientswithacute respira-toryfailurewhowerehospitalizedintheintensivecareunit ofourclinic andhad invasivemechanical ventilatory sup-portfor morethan48h.Elevenof thesecasesdeveloping respiratoryfailureinthe1sthourofextubationand1case operatedforacuteabdomenonthe12thhourofthestudy wereexcluded fromthe study.The remaining50 patients inbothgroupswhowerefollowed-upwithVMaftera suc-cessfulweaning for 1h were included inthe study.There wasnosignificantdifferencebetweentwogroupsregarding age, gender distribution and APACHE II scores (p>0.05) (Table1).
Thestudyperiodwas48hafterextubation.Systolicblood pressure,peakheartrate,respiratoryrate,PaO2andPaCO2 andpHvalueswererecordedandcomparedatcertaintime intervals.
WhenT-circuitwasatthe30thminuteinGroupVMand Group NIV, there was no significant difference (p>0.05)
Table1 Baselinecharacteristicsofthepatients.
GroupVM GroupNIV p-value
Age 67.84±17.31 71.88±11.00 0.330
Sex
F 15(60%) 12(48%) 0.395 M 10(40%) 13(52%)
APACHEII 20.76±7.03 19.54±4.46 0.474
betweensystolicbloodpressurevaluesinthe1st,2nd,3rd,
4th,5th,6th,12th,24th,48thhours.
WhenT-circuitwasatthe30thminuteinGroupVMand
Group NIV, there was no significant difference (p>0.05)
between peakheartratevaluesin the1st,2nd,3rd,4th,
5th,6th,12th,24th,48thhours.GroupVMhadsignificantly
higherpulserates(p<0.05)thanGroupNIVinthe2ndhour
(98.7±15.1;90.3±13.6;p=0.045).
WhenT-circuitwasatthe30thminuteinGroupVMand
Group NIV, there was no significant difference (p>0.05)
between respiratoryrate(RR)valuesinthe1st,2nd,3rd,
4th,5th,6th,12th,24th,48thhours.
WhenT-circuitwasatthe30thminuteinGroupVMand
Group NIV, there was no significant difference (p>0.05)
betweenPCO2valuesinthe1st,6th,12th,24th,48thhours.
WhenT-circuitwasatthe30thminuteinGroupVMand
Group NIV, there was no significant difference (p>0.05)
betweenPO2valuesinthe1st,12th,24th,48thhours.Group
VMhadsignificantlylowerPO2values(p<0.05)thanGroup
NIVinthe6thhour(90.2±25.6;112±29.2;p=0.015).
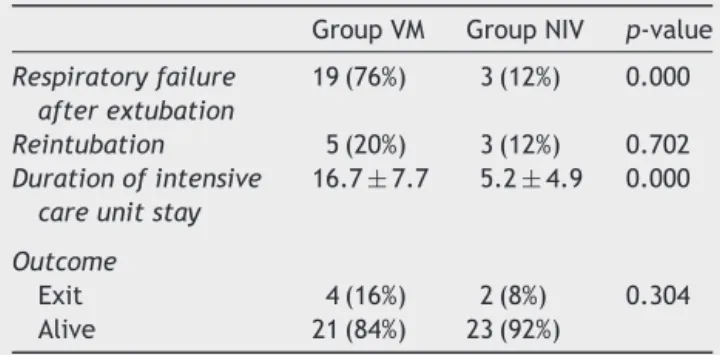
Respiratory failure developed in 19 of the 25 patients
(76%) in Group VM, whereas it developed only in 3 (12%)
ofthe25 patientsinGroupNIV afterextubation.Ingroup
VM,14ofthe19patients(73%)NIVsupportwasinitiated,5
patients(26%)weredirectlyreintubated.Four(80%)ofthe
5 patientswho weredirectly reintubated weredied after
the 48h study period, during their stay in ICU with
pro-gressiverespiratoryfailureduetoCOPD+Pnemoniainone
and with acutecerebral bleeding, malignancy, abdominal
sepsisdevelopedaftercolonperforationintheotherthree
patients.
Respiratoryfailuredevelopedafterextubationinonly3
(12%) of 25 patients of groupfollowed with NIV andthey
werereintubated.Two (66%)oftheseweredied afterthe
study periodbefore weaning. The causes of deaths were
again relatedto theextrapulmonary reasons (acute
cere-brovascularocclusionandacutecoronarysyndrome).
NIVwasprovidedin14patients(56%)inGroupVM
devel-opingrespiratoryfailureduringfollow-upwithventurimask
andtheycouldbedischargedfromthehospitalwithoutany
needofreintubation.IngroupVMpatientswhoneededNIV
support,asignificantdecreasewasobservedinPO2valueat
the6th---12thhoursandasignificantincreaseVM.
TheuseofNIVsupportdecreasedrespiratoryfailureratio
afterextubationby64%,andreintubationandmortalityrate
by 8%. Comparing the twogroups in terms of respiratory
failure after extubation a significant difference wasseen
(p<0.05).Nosignificantdifferencewasdetectedregarding
Table2 Nosignificantdifferencewasdetectedregarding reintubationandmortalityratios.
GroupVM GroupNIV p-value
Respiratoryfailure afterextubation
19(76%) 3(12%) 0.000
Reintubation 5(20%) 3(12%) 0.702 Durationofintensive
careunitstay
16.7±7.7 5.2±4.9 0.000
Outcome
Exit 4(16%) 2(8%) 0.304 Alive 21(84%) 23(92%)
Discussion
Currentroutineclinicalpracticeof theweaningprocessis
toextubate thepatients eligiblefor weaning criteriaand
follow-upthegroupwhoseemtobestabilizedintermsof
respirationwithVM.
While this process is well tolerated by some patients
andweaningprocesscan easilybecompleted,during
pro-longed VM period, some patients may need respiratory
supportdue to insufficiency of ventilation capacity, rapid
superficialbreathing,inabilitytoprotectairway,secretion
collectionandatelectasisformationintheadvancinghours
eventhoughtheyseemtobestabileinthefirsthoursofthe
process.4---7TobeinsistentonVMfollow-upforthesegroups
ofpatientsmaycausethepatienttolosetheopportunityfor NIVleadingtothereintubationprocesswithaccompanying risks.
Weperformedourstudyonthepatientswhofulfilledthe weaning criteria, kept respiratory and hemodynamic sta-bility after 30min T-piece trial and then extubated. We aimed to observe the effects of NIV support on respira-toryfailuredevelopment,durationofstay intheintensive care unit and mortality rates in this patient group who were allowable for follow-up with venturi mask, namely thepatientsforwhomrespiratoryfailurewerenotforeseen undernormalconditions.Wepreferredtouse NIVsupport continuouslyfor48hinourpatients.However,wealso car-riedout a protocol basedoncare, feeding andshortrest intervals considering patient comfort. When the patients withoronasalmaskwereobservedtohavenasalpressure, full-facemaskalternativewasusedtopreventnasalinjury. None of the patients sufferedfrom complications suchas gastricdistension,regurgitationandvomitingandtherewas noneedforsedationinanygroup.
Nava et al. investigated NIV use in patients fulfilling weaning criteria but at risk for respiratory failure after extubationalsousedasimilarmethod(successiveNIV appli-cations in the first 48h). In this study, 97 patients were dividedintotwogroupsasstandardmedicaltreatment(VM) or NIVuse. While12 of49 patientsin controlgroup were reintubated,4of48patientsinNIVgroupwerereintubated (p=0.027). Hence, the use of NIV decreased reintubation by16%andtheriskofintensivecareunitmortalityby10% (p<0.01).Besides these,need for reintubationwasfound tobe associatedwitha 60% increasein the risk of inten-sive careunitmortality (p<0.01).When durations ofstay intheintensivecareunitofthepatientswithreintubation
needwerecomparedwiththeother patients, itwasseen thatitwasstatisticallysignificantlylonger(28.3±29.5vs. 8.6±5.1).Theseresearchersconcludedthattheinhibitory use of NIV decreased the requirement of reintubation in patientsubgroupspassing spontaneousbreathingtrialsbut havingrespiratoryfailureriskafterextubation.5
Similarresults were found in another study performed byFerrer etal.6 In this study,like ours, NIV wasused as anpreventivetreatmentmethodforthepatientswhowere successfullyweanedaftertheT-piecetrial,andcomparedto thecontrolgroupwhohadventurimaskinstead.Asaresult ofthestudyperformedon162patients,researchersfound thattheuseofNIVdecreased theincidenceofrespiratory failureafterextubationconsiderablyandintensivecareunit mortalityratealsodecreased.However,theycouldnotfind asignificantdifferencebetween90-daysurvivalratesofthe twogroups.
We chose our study group from the patients in whom respiratoryfailurewasnotforeseenafterextubation.Ifany deteriorationduring the follow-up periodoccurs; that is: respiratoryrateabove25breaths/min,SO2:90%andbelow; PO2:70mmHgandbelow;NIVappliedtothepatientunder VM.Iftherespiratoryrateabove35breaths/min,SO2:90% andbelow;PO2:60mmHgandbelowor thehemodynamic parameterswereimpaired,thepatientsinbothgroupswere directly intubated to have invasive mechanical ventilator support.NIVwasprovidedin14patients(56%)inGroupVM developingrespiratoryfailureduringfollow-upwithventuri maskandthesepatientscouldbedischargedfromhospital withoutanyneedofreintubation.
Intheirstudyperformedon158patients,Medurietal.7 showedthatNIVcouldbeaneffectivemethodtotreat respi-ratoryfailureafterextubationand65---70%ofthepatients whosereintubationwasunavoidablecouldbenefitfromNIV. Thirty-nineofthesepatientsweresupportedwithNIVdueto respiratoryfailureafterextubationandanimprovementwas observedinarterialbloodgasvaluesof88%ofthem. There-fore,the need for reintubation removed in 65% of these patients.
NIV support could beused carefully in patients devel-opingrespiratoryfailureafterextubationbut itshouldbe takenintoconsiderationthatdangerousdelaysin reintuba-tionduringtreatmentofrespiratoryfailureafterextubation withNIV supportcouldresultinadverse outcomesforthe patients.Intheirmeta-analysisperformedbyreviewingthe studiesonthissubject,Agarwaletal.concludedthatitis suggestedthatprotocolsshouldbedevelopedforNIVusein thepatientsatriskfordevelopingrespiratoryfailureafter extubation.8
Inourstudy,weobservedthatprovisionofprophylactic NIV support for at least 48h after weaning under opti-malconditionsinthepatientswhohadinvasivemechanical ventilatorysupportfor morethan48hdue toacute respi-ratory failure and for whom respiratory failure were not foreseen after extubation decreased the duration of stay in the intensive care unit and risk for respiratory fail-ure that could develop. Although the use of NIV is not suggested except the patients at high risk for extuba-tion success; based onthe results we obtained from our study,weconsiderthattheprophylacticuseofNIVcanbe beneficial.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.DemauleA,GiraouE,RichardJC,etal.Increaseduseof nonin-vasiveventilationinFrenchintensivecareunits.IntensiveCare Med.2006;32:1747---55.
2.Esteban A, Frutos-Vivar F, Ferguson ND, et al. Noninvasive positive-pressureventilationfor respiratoryfailureafter extu-bation.NEnglJMed.2004;350:2452---60.
3.KeenanSP,PowersC,McCormackDG,etal.Noninvasive positive-pressure ventilation for postextubation respiratory distress: a randomizedcontrolledtrial.JAMA.2002;287:3238---44.
4.NavaS,AmbrosinoN,CliniE,etal.Noninvasivemechanical ven-tilationintheweaningofpatientswithrespiratoryfailuredueto chronicobstructivepulmonarydisease.Arandomized,controlled trial.AnnInternMed.1998;128:721---8.
5.NavaS,GregorettiC,FanfulaF,etal.Noninvasiveventilationto preventrespiratoryfailureafterextubationinhigh-riskpatients. CritCareMed.2005;33:2465---70.
6.FerrerM,ValenciaM,NicolasJM,etal.Earlynoninvasive venti-lationavertsextubationfailureinpatientsatrisk:arandomized trial.AmJRespirCritCareMed.2006;15:164---70.
7.MeduriGU, Turner RE,Abou-Shala N, et al.Noninvasive posi-tivepressure ventilationviafacemask. First-lineintervention inpatientswithacutehypercapnicand hypoxemicrespiratory failure.Chest.1996;109:179---93.