www.bjorl.org
Brazilian
Journal
of
OTORHINOLARYNGOLOGY
REVIEW
ARTICLE
Proliferative
verrucous
leukoplakia:
diagnosis,
management
and
current
advances
夽
Diogo
Lenzi
Capella
a,
Jussara
Maria
Gonc
¸alves
a,
Adelino
António
Artur
Abrantes
a,
Liliane
Janete
Grando
b,
Filipe
Ivan
Daniel
b,∗aUniversidadeFederaldeSantaCatarina(UFSC),ProgramadePós-graduac¸ãoemOdontologia,Florianopolis,SC,Brazil bUniversidadeFederaldeSantaCatarina(UFSC),DepartamentodePatologia,Florianopolis,SC,Brazil
Received24February2016;accepted8December2016 Availableonline24January2017
KEYWORDS
Leukoplakiaoral; Leukoplakia; Proliferative verrucous leukoplakia; Oralcancer; Squamouscell carcinoma;
Headandneckcancer
Abstract
Introduction:Proliferativeverrucousleukoplakiaisamultifocalandprogressivelesionofthe oral mucosa, with unknown etiology, and commonlyresistant toall therapy attempts with frequentrecurrences.Itischaracterizedbyahighrateoforalsquamouscellcarcinomaand verrucoucarcinomatransformations.
Objective: ToanalyzethestudiesaboutProliferativeverrucousleukoplakiaanddevelopa con-ciseupdate.
Methods:APubmedsearchidentifyingstudies(laboratoryresearch,caseseriesandreviewsof literature)thatexaminedpatientswithProliferativeverrucousleukoplakiawasrealized. Results:TherearenotenoughstudiesaboutProliferativeverrucousleukoplakiainthe litera-ture.Thefewfoundstudiesnotpresentaconsensusaboutitsetiologyanddiagnosiscriteria. Although several treatmentstrategies havebeen proposed,mostofthem still show ahigh recurrencerate.
Conclusion: MoreresearchaboutProliferativeverrucousleukoplakiaisnecessarytounderstand andtreatthisdisease.
© 2017 Associac¸˜ao Brasileira de Otorrinolaringologia e Cirurgia C´ervico-Facial. Published by Elsevier Editora Ltda. This is an open access article under the CC BY license (http:// creativecommons.org/licenses/by/4.0/).
夽
Pleasecitethisarticleas:CapellaDL,Gonc¸alvesJM,AbrantesAA,GrandoLJ,DanielFI.Proliferativeverrucousleukoplakia:diagnosis, managementandcurrentadvances.BrazJOtorhinolaryngol.2017;83:585---93.
∗Correspondingauthor.
E-mails:filipe.daniel@ufsc.br,filipedaniel06@gmail.com(F.I.Daniel).
PeerReviewundertheresponsibilityofAssociac¸ãoBrasileiradeOtorrinolaringologiaeCirurgiaCérvico-Facial.
http://dx.doi.org/10.1016/j.bjorl.2016.12.005
PALAVRAS-CHAVE
Leucoplasiaoral; Leucoplasia;
Leucoplasiaverrucosa proliferativa;
Cânceroral; Carcinoma,Célula escamosa;
Câncerdecabec¸ae pescoc¸o
Leucoplasiaverrucosaproliferativa:diagnóstico,condutaeavanc¸osatuais
Resumo
Introduc¸ão:Leucoplasiaverrucosaproliferativa(LVP)éumalesãomultifocaleprogressivada mucosaoral,cometiologiadesconhecidaecomumenteresistenteatodasastentativas ter-apêuticas,comrecorrênciasfrequentes.Écaracterizadaporumaaltataxadetransformac¸ão emcarcinomadecélulasescamosasecarcinomaverrucosodacavidadeoral.
Objetivo:AnalisarosestudossobreLVPeelaborarumaatualizac¸ãoresumida.
Método: FoirealizadaumapesquisanabasededadosPubmedidentificandoestudos(pesquisas laboratoriais,sériesdecasoserevisõesdeliteratura)queavaliarampacientescomLVP. Resultadosediscussão: NãoháestudossuficientessobreLVPnaliteratura.Ospoucosestudos encontradosnãoapresentamconsensoquantoaoscritériosdeetiologiaediagnóstico.Embora váriasestratégiasdetratamentotenhamsidopropostas,amaioriaaindaapresentaaltataxa derecorrência.
Conclusão:MaispesquisassobreLVPsãonecessáriasparaentenderetratarestadoenc¸a. © 2017 Associac¸˜ao Brasileira de Otorrinolaringologia e Cirurgia C´ervico-Facial. Publicado por Elsevier Editora Ltda. Este ´e um artigo Open Access sob uma licenc¸a CC BY (http:// creativecommons.org/licenses/by/4.0/).
Introduction
Proliferativeverrucousleukoplakia(PVL)isaveryaggressive andrareformoforalleukoplakia(OL)withhighmorbidity.1
ThefirstdescriptionhasbeenmadebyHansenetal.(1985) asadistinctformofOLwhichdevelopsinitiallyasawhite plaque that eventually becomes multifocal slow-growing lesions resistant to all therapeutic procedures, including surgery,withahighrecurrencerateandanoralcancer trans-formation trend.2 Withthe introduction of theterm PVL,
thepreviously usedterm ‘‘oral floridpapillomatosis’’ has disappearedfromtheliterature.3Actually,theWorldHealth
Organization(WHO)(2005)describedPVLas‘‘ararebut dis-tinctivehigh-riskclinical formof oralprecursorlesions’’.4
Severalstudies have examined PVLcharacteristics and its propensity to develop into oral carcinoma.4 Thirty years
afteritsdiscovery,itis stillachallenging diseasewithno confirmedetiologyandefficienttreatment.Althoughthere arepublishedpapersaboutPVLdiagnosiscriteria,theymay beimpreciseindetectingearlydiseasepresentations,either forclinicalorhistopathologicalview.Theobjectiveofthis paperistoanalyzethePVLliteratureandtodevelopa con-ciseupdate.
Review
methods
APubMed search using the term ‘‘ProliferativeVerrucous Leukoplakia’’ was made from 1985 to 2015 (30 years). Additional papers were included based upon the original literature search and references in the selected papers. Papersconcerninglaboratoryresearch,caseseries,aswell asreviewsofliteraturewerealsoincluded.
Results
and
discussion
Etiology
Hansen et al. (1985) described PVL as a disease with unclearetiology,buttypicallyassociatedwithtobaccouse.2
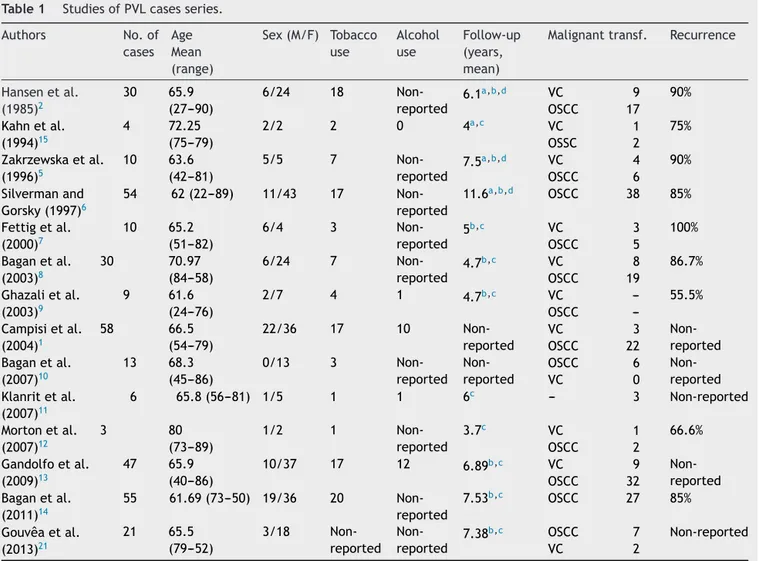
However, the role of tobacco in PVL lesions is unknown since these lesions are seen in smokers and nonsmokers (Table1).1,2,5---15SeveralstudiesevaluatedalcoholusebyPVL
patients,buttherelationbetweenthemwasnotstablished (Table1).1,9,11,13
In recent years, it has been hypothesized that human papillomavirus (HPV) may influence both potentially and already stablished oral malignant lesions.16 Although the
association between oralsquamouscell carcinoma(OSCC) and HPVis already mentioned, itsinfluence onPVL cases is notconfirmed yet.17 Over thelastdecades, some
stud-iesreporteddifferentandcontradictoryfrequenciesofHPV DNAdetectioninPVL(Table2).1,7,10,18,19
About other possible etiologies, there are few studies with PVL that tried to identify the presence of Candida albicans. Silverman et al. (1997) reported 19 of 38 spec-imens with C. albicans positivity, but without correlation betweenthefungalinfectionandPVLoccurrenceor progres-siontocarcinoma,characterizingitasaprobablesecondary infection.6 Similarly, Hansen et al. (1985) observed that
12 of 30 patients were positive for C. albicans.2
Con-cerning to Epstein Barr Virus (EBV), Bagan et al. (2008) was the only one to detect EBV in a PVL group (60% of 6 patients).20 Therefore, none of these studies have yet
Table1 StudiesofPVLcasesseries.
Authors No.of
cases Age Mean (range)
Sex(M/F) Tobacco use Alcohol use Follow-up (years, mean)
Malignanttransf. Recurrence
Hansenetal. (1985)2
30 65.9 (27---90)
6/24 18 Non-reported
6.1a,b,d VC 9 90%
OSCC 17 Kahnetal.
(1994)15
4 72.25 (75---79)
2/2 2 0 4a,c VC 1 75%
OSSC 2
Zakrzewskaetal. (1996)5
10 63.6 (42---81)
5/5 7
Non-reported
7.5a,b,d VC 4 90%
OSCC 6
Silvermanand Gorsky(1997)6
54 62(22---89) 11/43 17 Non-reported
11.6a,b,d OSCC 38 85%
Fettigetal. (2000)7
10 65.2 (51---82)
6/4 3
Non-reported
5b,c VC 3 100%
OSCC 5
Baganetal. (2003)8
30 70.97 (84---58)
6/24 7
Non-reported
4.7b,c VC 8 86.7%
OSCC 19 Ghazalietal.
(2003)9
9 61.6 (24---76)
2/7 4 1 4.7b,c VC --- 55.5%
OSCC ---Campisietal.
(2004)1
58 66.5 (54---79)
22/36 17 10 Non-reported
VC 3
Non-reported OSCC 22
Baganetal. (2007)10
13 68.3 (45---86)
0/13 3
Non-reported Non-reported
OSCC 6 Non-reported
VC 0
Klanritetal. (2007)11
6 65.8(56---81) 1/5 1 1 6c --- 3 Non-reported
Mortonetal. (2007)12
3 80
(73---89)
1/2 1
Non-reported
3.7c VC 1 66.6%
OSCC 2
Gandolfoetal. (2009)13
47 65.9 (40---86)
10/37 17 12 6.89b,c VC 9
Non-reported OSCC 32
Baganetal. (2011)14
55 61.69(73---50) 19/36 20 Non-reported
7.53b,c OSCC 27 85%
Gouvêaetal. (2013)21 21 65.5 (79---52) 3/18 Non-reported Non-reported
7.38b,c OSCC 7 Non-reported
VC 2
VC,verrucouscarcinoma;OSCC,oralsquamouscellcarcinoma.
a Followupuntilthecure.
b Followupduringproliferativeverrucousleukoplakiaprogress. c Followupuntilmalignanttransformation.
d Followupuntildeath.
Table2 StudiesaboutHPVpresenceinPVL.
Author No.ofcases HPVpositive HPVtypes
Palefskyetal. (1995)18
9 8
(88.8%)
HPV16(n=7;77.7%) HPV18(n=1;11.1%) Gopalakrishnan
etal.(1997)19
10 2
(20%)
HPV16(n=1;10%) HPV18(n=1;10%)
Fettigetal.(2000)7 10 0
---Campisietal. (2004)1
58 14
(24.1%)
HPV18(n=10;17.24%) HPV16(n=4;6.8%)
Baganetal.(2007)10 13 0
---HPV,humanpapillomavirus;PVL,proliferativeverrucousleukoplakia.
Epidemiologicalandclinicalcharacteristics
In the studies evaluated in this paper, PVL occurred predominantly in women, with a 2.72:1 (female/male) rate, and a mean age of 66.8 years (Table 1).1,2,5---15,21
The most affected sites were gingiva,8---10,12,14,15 buccal
mucosa,2,5,6 and alveolar ridge,11,13 while the tongue was
lessinvolved.21
initiallypresentsasunifocal, homogeneous,slowand per-sistent growth lesion.9 At this stage, it is extremely
difficult, if not impossible, to distinguish it from oral leukoplakia. PVL has one or more areas of homogeneous leukoplakia, which grows slowly and persistently, and tendstobecome multifocalwithexophytic,verrucous, or
erythematous areas.22 After a long period, commonly six
years, the evolution to carcinoma occurs.23 Areas that
are erythematous, verrucous or have papillary surface are characteristic of malignant transformation, and so these areas should have a histopathological confirmation (Fig.1).23
Hansen et al. (1985) Batsakis et al. (1999)
New suggestion of Batsakis et al.
(1999)
Clinical flat leukoplakia without displasya
Verrucous carcinoma
Verrucous carcinoma
Verrucous carcinoma
0
1
2
3
4
5
6
Intermediate stages
7
8
9
10
Papillary squamous cell
carcinoma
Squamous cell carcinoma
Verrucous hiperplasia
Verrucous hiperplasia
Clinical flat leukoplakia without displasya Normal oral
mucosa
Homogeneous leukoplakia
Squamous cell carcinoma
Squamous cell carcinoma
Figure2 Histologicstagesofprogressiontocarcinoma.AdaptedfromGhazalietal.(2003).9
Recently, aPVLsubtype designatedproliferative verru-cousleukoplakia of thegingiva (PVLG) has been reported asinvolving exclusivelyfreeandattachedgingiva.PVLGis characterizedasa whitishplaque,unifocal, recurrentand progressivelesion.Thecourseisalsounpredictableandmay undergoOSCCorverrucouscarcinoma(VC)transformation.7
As the evolution stages of different sites in multifo-cal lesions are not necessarily the same, patients should be monitored closely, with frequent and repetitive biop-sies whentherearechanges incolor, appearance or size, and when new lesions appear.9,24,25 Patients with whitish
harmless appearanceand recurrenceepisodesshould also be followed up every six months.25 PVL may progress
to VC or OSCC over time in spite of numerous treat-mentinterventions,suggesting thatPVLisassociatedwith diffusesubmicroscopicchangesof theoral mucosa, some-timesdescribedas‘‘fieldcancerization’’.24Therefore,PVL
presentsahighmalignanttransformationrate(Table1).26
Histopathology
Histopathologicalfindingsmayshowacanthosisand hyper-keratosis with an interface lymphocytic infiltrate within the superficial lamina propria. If the lesions continue to growhorizontallyandvertically,therearehistopathological changes that increase roughness of surface with verru-cous aspect, and hyperplasia withor without dysplasia.12
Therefore,over time and without treatment, thereis an inexorableprogressiontoVCorOSCC(Fig.1).5,12,22,27
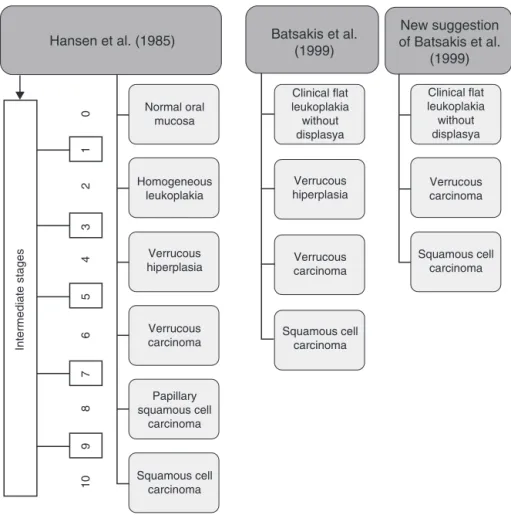
Hansenetal.(1985)describedthehistopathological pro-gression of PVL in 10 stages during its clinical course.2
This classification divided PVL in five groups: hyperker-atosis,verrucoushyperplasia(VH), VC,papillarysquamous cellcarcinomaandOSCCpoorlydifferentiated,with inter-mediatestages. Frequently thelesions move slowlyup in grade,withveryfewrevertingcases.However,Murrahand Batsakis (1999) reduced the number of histologic stages to four, removing the intermediate stages, and proposed a review that omitted papillary squamous cell carcinoma considering it aPVL independent entitymore frequent in theoropharynx.28Batsakisetal.(1999)alsoconsideredthe
possibleremovalofVHsinceithasmuchincommonwithVC, butwithanexophyticgrowthpatterninVHinoppositionto anendophyticgrowthpatterninVC(Fig.2).29
Biomarkers
Recentfindingshaveindicatedthatcarcinogenesisisaresult ofaccumulatedgeneticandepigeneticalterationsthatmay leadtochromosomalinstability,intheformofnumericalor structuralaberrations,whichmight bedetectedas abnor-malDNAcontentoraneuploidy.30PloidyanalysisinPVLwas
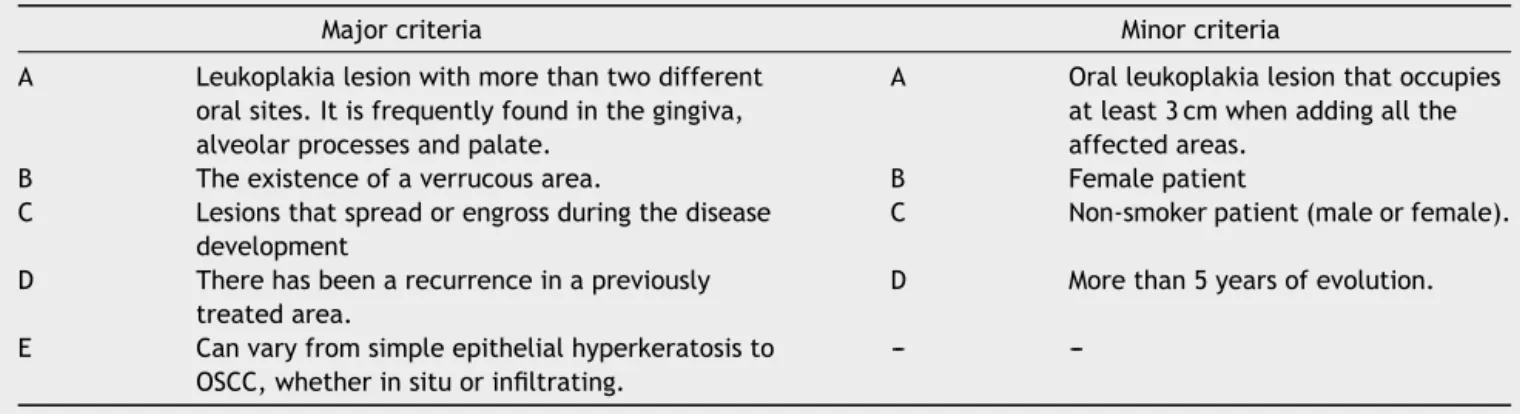
Table3 ProposalofmajorandminordiagnosticcriteriaforPVLrecommendedbyCerero-Lapiedraetal.(2010).23 Adapted
fromCarrardetal.36
Majorcriteria Minorcriteria
A Leukoplakialesionwithmorethantwodifferent oralsites.Itisfrequentlyfoundinthegingiva, alveolarprocessesandpalate.
A Oralleukoplakialesionthatoccupies atleast3cmwhenaddingallthe affectedareas.
B Theexistenceofaverrucousarea. B Femalepatient C Lesionsthatspreadorengrossduringthedisease
development
C Non-smokerpatient(maleorfemale).
D Therehasbeenarecurrenceinapreviously treatedarea.
D Morethan5yearsofevolution.
E Canvaryfromsimpleepithelialhyperkeratosisto OSCC,whetherinsituorinfiltrating.
---
---PVL,proliferativeverrucousleukoplakia.
found DNA aneuploid in all cases.15 Klanrit et al. (2007)
analyzed6paraffin-embeddedPVLsamplesanddetected4 (66.6%)caseswithabnormalploidystatuspriortomalignant transformation.11 Gouveaetal.(2013)analyzedDNAof20
patients withPVL and 19 (95%) cases showedaneuploidy, with abnormal DNA observed even in the more indolent lesions.21
Therefore,severalstudieshavebeenconductedto deter-minewhetherimprovedexpressionlevelsofsomemolecular markersinvolvedindifferentcellularpathwayscanbe valu-ableindicatorsofclinicalbehavior.31Gopalakrishnanetal.
(1997)studiedp53expressionin10samplesandfound min-imalmarkupinnormaloralmucosa,butpositivityin8(80%) ofthecasesofPVL,andin7(70%)ofthecasesofOSCC.19
Fettigetal.(2000)identifiedp53expressionin 4(40%)of the10 analyzed cases.7 Gouveaet al.(2013) showed p53
immunoreactivityin14(77.7%)ofthe18cases.32Inthesame
studyKi-67expressionwassimilartotheoneobservedwith p53protein progressionof epithelial dysplasia in PVL. Ki-67isanuclearproteinassociatedwithcellularproliferation withpotentialpredictivebiomarkerinearlystagesofOSCC andcanbeusedin additiontoconventional tumorstaging foroptimaltherapeuticmanagement.33 Akrishetal.(2015)
realizedaretrospectivereviewof11patientswithPVL,38 withcarcinomaarisinginpatientswithPVL(P-SCC)and49 withconventionalsquamouscellcarcinoma(C-SCC).34
Over-expressionofp53wasmorecommoninP-SCC,butwithout ki-67orp16overexpression.Krest etal.(2014) evaluated cellcycle regulatory genes in 20 PVL cases and detected deletion or mutation event involving both p16INK4a and p14ARFgenesin45%ofthecases.35
Diagnosticcriteria
Hansenetal.(1985)determinedthatlesionsdiagnosedas PVLcouldhaveinitiallyahomogeneousaspect,without dys-plasia,followedbywartyappearanceofsurfaceareasand multiplediscreteor confluentlesionsinsingleor multiple intra-oralsites.2
AccordingtoCerero-Lapiedraetal.(2010),studies pub-lishedonPVL followedthe diagnosticcriterionpostulated byHansenetal.(1985).2,23 Itisa pioneeringand
compre-hensivedescription,butstillneedsupdates.Therefore,the
sameauthorsproposedthereformulationofthecriteriaby dividingthemintomajor(fivecriteria)andminor(four crite-ria)(Table3).ToPVLdiagnosis,patientshouldhaveoneof thefollowingcombinations:
- Threemajorcriteria(oneofwhichmustincludethe evo-lutionofthehistopathologicallesions).
- Twomajorcriteria(oneofwhichmustincludethe evolu-tionofthehistopathologicallesions)+twominorcriteria. Baganetal.(2011)believedthatthesecriteriaare use-ful only for those with clinical experience with PVL, but can be confusing for beginners.14 Corroborating with this
observation, Carrard et al. (2013) suggested simplifying thediagnosticcriteriabyomittingthedistinctionbetween majorandminorcriteria.However,allfourcriteriashould bemet(Table4).36
Treatmentandrecurrence
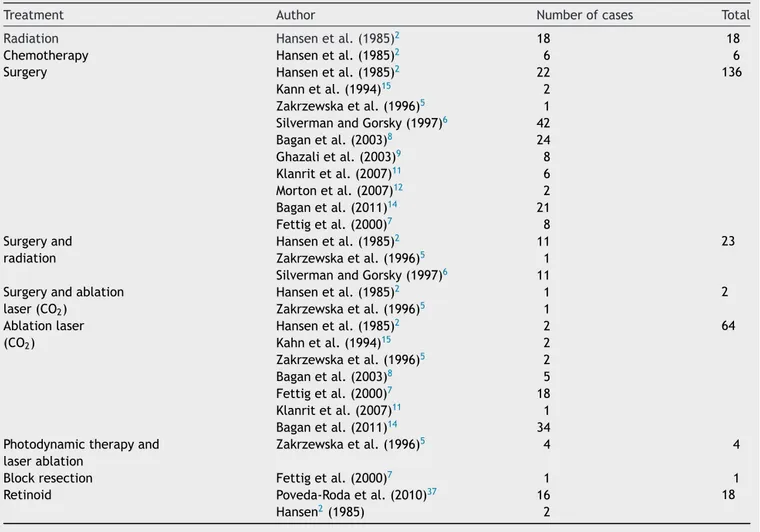
Thisliteraturereview(Table5)showeddifferenttreatments modalities.Surgeryandlaserablationwerethemostused. Ten papersutilized surgeryin 136 cases2,5,6---9,11,12,14,15 and
seven papers used laser ablation in 64 cases.2,5,7,8,11,14,15
According toevaluatedstudies, withatleast 30 patients, wefoundarecurrencemeanrateof85%for alltreatment modalitiesisolatedorassociated.1,2,6,8,13,14
Table4 ModifieddiagnosticcriteriaforPVLrecommended byCarrardetal.(2013).36AdaptedfromCarrardetal.36
1.Leukoplakiashowingthepresenceofverrucousor wartlikeareas,involvingmorethantwooralsubsites. 2.Whenaddingallinvolvedsitestheminimumsizeshould
beatleastthreecentimeters.
3.Welldocumentedperiodofdiseaseevolutionofatleast fiveyears,characterizedbyspreadingandenlargingand theoccurrenceofoneormorerecurrencesina
previouslytreatedarea.
4.Therealizationofatleastonebiopsy(toruleoutthe presenceofaVCorOSCC).
Table5 Treatmentsappliedincasesseriesfromliterature.
Treatment Author Numberofcases Total
Radiation Hansenetal.(1985)2 18 18
Chemotherapy Hansenetal.(1985)2 6 6
Surgery Hansenetal.(1985)2 22 136
Kannetal.(1994)15 2
Zakrzewskaetal.(1996)5 1
SilvermanandGorsky(1997)6 42
Baganetal.(2003)8 24
Ghazalietal.(2003)9 8
Klanritetal.(2007)11 6
Mortonetal.(2007)12 2
Baganetal.(2011)14 21
Fettigetal.(2000)7 8
Surgeryand radiation
Hansenetal.(1985)2 11 23
Zakrzewskaetal.(1996)5 1
SilvermanandGorsky(1997)6 11
Surgeryandablation laser(CO2)
Hansenetal.(1985)2 1 2
Zakrzewskaetal.(1996)5 1
Ablationlaser (CO2)
Hansenetal.(1985)2 2 64
Kahnetal.(1994)15 2
Zakrzewskaetal.(1996)5 2
Baganetal.(2003)8 5
Fettigetal.(2000)7 18
Klanritetal.(2007)11 1
Baganetal.(2011)14 34
Photodynamictherapyand laserablation
Zakrzewskaetal.(1996)5 4 4
Blockresection Fettigetal.(2000)7 1 1
Retinoid Poveda-Rodaetal.(2010)37 16 18
Hansen2(1985) 2
Thereare2descriptionsabout theassociationbetween surgery and laser ablation with no improvement.2,5
Zakrzewskaetal.(1996)showedonepatientwithno recur-renceatthelaser-treatedsites,butnewlesionsdeveloped elsewhere.5Baganetal.(2003),aftertreating24patients
(80%)withsurgeryand18(60%)withlaserablation,detected recurrence rate of 86.7% and recognized new lesions in 83.3%.8 Fettig et al. (2000) identified that both simple
excision andlaserexcisionwere ineffectivein eradicating lesions.7 Surgery, despite high recurrencerates, gives the
possibilityof dysplasiahistologic gradingand early detec-tionofmalignanttransformation.Laserablationshouldbe indicatedforlesionswherethesurgerywouldbe contraindi-catedbylesionsizeoraccessdifficulty.Developmentofnew lesionsinthesepatientsisconstant;thus,multiple interven-tionsarealwaysnecessary.
Hansen et al. (1985) utilized radiation in 16 patients and chemotherapy in 6, with only one patient free of PVLat6yearsaftertreatment; therefore,theyconcluded that radiation therapy is not entirely satisfactory in a widespreaddiseasesuchasPVL.2 Inspiteoftheseresults,
others papers reportedthe association between radiation andsurgerytotreatPVL,totaling24casesdescribedinthe literature.2,5,6 Silverman et al. (1997) reported that
radi-ation was not effective in controlling PVL based on the lack of response of the cases treated with radiotherapy.6
Zakrzewska et al. (1996) treated one patient with radio-therapy, but lesions continued to appear throughout the mouth.5 One patient also received a limited course of
chemotherapy, but new lesions appeared, demonstrating the ineffectiveness of these treatment. Radiotherapy or chemotherapydid not show improvementin lesion recur-rence,and showed severe side effects such asmucositis, infection,andsalivaryglandproblems.
Extensivesurgerysuchasresectionwasperformedinonly onecasebyFettigetal.(2000).7Accordingtotheauthors,
localblockresectionwasrequiredtopreventrecurrences.In spiteofthisreport,onecaseisnotsufficienttoconfirmthe potentialofthistherapymodality.Inadditiontoitsradical anddebilitatingcharacteristic,extensiveresectionis only acceptablewhenOSCCtransformationwithboneinvasionis present.
Photodynamic therapy (PDT) associated to laser abla-tionwould appear tooffer slightimprovement prognosis, becauseitmakestreatmentofmultifocalareaspossiblewith acceptablemorbidity,butitdidnotpreventnewlesionsand untilthemomentthereisonlyonestudydemonstratingits efficacy.5
Besides, further studies are needed to assess the safety of these products, because frequent adverse effects can occur. The most frequent adverse effects were cheilitis, desquamation,pruritus, alopeciaandrhinitis, which coin-cidedwiththewell-known retinoidside effects.However, twoofthepatientssufferedseriousproblemsnotdescribed intheSummaryofProductCharacteristicsofthemedication used;theydevelopedintenserectalbleedingandcrampsof theextremities that made standing andwalking difficult. Suppressionofthedrugledtoresolutionofthese manifes-tations.
Conclusion
Although there are not enough studies to determine PVL etiologyandnosimplifieddiagnosis criteria, themost dif-ficult point is PVL treatment. According tothe literature reviewed, PVL seems to be resistant to many therapy attemptsandoftenhashighpropensityfordysplasiaand/or malignancy progression. Modalities such as surgery, laser ablation, photodynamic therapy, retinoid, radiation and chemotherapy are not effective in reducing relapses and malignanttransformation.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
Acknowledgment
WethankProfessorFilipeModoloSiqueirafortechnical assis-tanceinreviewinghistopathologicalfindingsandimages.
References
1.CampisiG,GiovannelliL,AmmatunaP,CapraG,ColellaG,Di LibertoC,etal.Proliferativeverrucousvsconventional leuko-plakia:no significantly increased risk ofHPV infection. Oral Oncol.2004;40:835---40.
2.HansenLS,OlsonJA,SilvermanS.Proliferativeverrucous leuko-plakia.Along-termstudyofthirtypatients.OralSurgOralMed OralPathol.1985;60:285---98.
3.Grinspan D, Abulafia J. Oralflorid papillomatosis (verrucous carcinoma).IntJDermatol.1979;18:608---22.
4.BarnesL,EvesonJW,ReichartP,SidranskyD.Pathology& genet-icsheadandnecktumours.WorldHealthOrganClassifTumours. 2005.
5.ZakrzewskaJM,LopesV,SpeightP,HopperC.Proliferative ver-rucousleukoplakia:areportoftencases.OralSurgOralMed OralPatholOralRadiolEndod.1996;82:396---401.
6.Silverman S,GorskyM.Proliferativeverrucousleukoplakia:a follow-upstudyof54cases.OralSurgOralMedOralPatholOral RadiolEndod.1997;84:154---7.
7.FettigA,PogrelMA,SilvermanS,BramantiTE,CostaMD,Regezi JA.Proliferativeverrucousleukoplakiaofthegingiva.OralSurg OralMedOralPatholOralRadiolEndod.2000;90:723---30.
8.BaganJV,JimenezY,SanchisJM,PovedaR,MilianMA,Murillo J, et al. Proliferative verrucous leukoplakia: high incidence of gingival squamous cell carcinoma. J Oral Pathol Med. 2003;32:379---82.
9.GhazaliN,BakriMM,ZainRB.Aggressive,multifocaloral ver-rucousleukoplakia:proliferativeverrucousleukoplakiaornot? JOralPatholMed.2003;32:383---92.
10.BaganJV,JimenezY,MurilloJ,GavaldáC,PovedaR,ScullyC, etal.Lackofassociationbetweenproliferativeverrucous leuko-plakiaand humanpapillomavirusinfection. JOralMaxillofac Surg.2007;65:46---9.
11.KlanritP,SperandioM,BrownAL,ShirlawPJ,ChallacombeSJ, MorganPR,etal.DNAploidyinproliferativeverrucous leuko-plakia.OralOncol.2007;43:310---6.
12.MortonTH,CabayRJ,EpsteinJB.Proliferativeverrucous leuko-plakiaand itsprogressiontooralcarcinoma:reportofthree cases.JOralPatholMed.2007;36:315---8.
13.GandolfoS,CastellaniR,PenteneroM.Proliferativeverrucous leukoplakia:a potentially malignant disorderinvolving peri-odontalsites.JPeriodontol.2009;80:274---81.
14.BaganJV,Jiménez-SorianoY,Diaz-FernandezJM,Murillo-Cortés J,Sanchis-BielsaJM,Poveda-RodaR,etal.Malignant transfor-mationofproliferativeverrucousleukoplakiatooralsquamous cellcarcinoma:aseriesof55cases.OralOncol.2011;47:732---5.
15.KahnMA,DockterME,Hermann-PetrinJM.Proliferative verru-cousleukoplakia.Fourcaseswithflowcytometricanalysis.Oral SurgOralMedOralPathol.1994;78:469---75.
16.BoudaM,GorgoulisVG,KastrinakisNG,GiannoudisA,Efthymia T,Danassi-AfentakiD,etal.Highrisk’HPVtypesarefrequently detectedinpotentiallymalignantand malignantorallesions, butnotinnormaloralmucosa.ModPathol.2000;13:644---53.
17.Ostwald C,Rutsatz K, Schweder J, SchmidtW, Gundlach K, Barten M. Human papillomavirus 6/11, 16 and 18 in oral carcinomasand benignorallesions. Med MicrobiolImmunol. 2003;192:145---8.
18.Palefsky JM, Silverman S Jr, Abdel-Salaam M, Daniels TE, Greenspan JS. Association between proliferative verrucous leukoplakiaandinfectionwithhumanpapillomavirustype16.J OralPatholMed.1995;24:193---7.
19.GopalakrishnanR,WeghorstCM,LehmanTA,CalvertRJ,Bijur G,SabourinCLK,etal.Mutatedandwild-typep53expression andHPVintegrationinproliferativeverrucousleukoplakiaand oralsquamouscellcarcinoma.OralSurgOralMedOralPathol OralRadiolEndod.1997;83:471---7.
20.BaganJ,JiménezY,MurilloJ,PovedaR,DíazJM,GavaldáC, etal.Epstein-Barrvirusinoralproliferativeverrucous leuko-plakiaandsquamouscellcarcinoma:apreliminarystudy.Med OralPatolOralCirBucal.2008;13:110---3.
21.GouvêaAF,SantosSilvaAR, SpeightPM,HunterK,CarlosR, Vargas PA, et al. High incidence of DNA ploidy abnormali-ties and increased Mcm2 expression may predict malignant changeinoralproliferativeverrucousleukoplakia. Histopath-ology.2013;62:551---62.
22.BaganJ,ScullyC,JimenezY,MartorellM.Proliferative verru-cousleukoplakia:aconciseupdate.OralDis.2010;16:328---32.
23.Cerero-Lapiedra R, Balade-Martinez D, Moreno-Lopez L, Esparza-GomezG,BaganJ.Proliferativeverrucousleukoplakia: aproposalfordiagnosticcriteria.MedOralPatolOralCirBucal. 2010;15:839---45.
24.BagánJ,MurilloJM,PovedaR, GavaldáC,JiménezY, Scully C.Proliferativeverrucousleukoplakia:unusuallocationsoforal squamouscellcarcinomas,andfieldcancerizationasshownby theappearanceofmultipleOSCCs.OralOncol.2004;40:440---3.
25.BishenK,SethiA. Proliferativeverrucousleukoplakia--- diag-nosticpitfallsandsuggestions.MedOralPatolOralCirBucal. 2009;14:263---4.
26.LiuW, WangYF,ZhouHW,ShiP,ZhouZT,TangGY.Malignant transformationoforalleukoplakia:aretrospectivecohortstudy of218Chinesepatients.BMCCancer.2010;10:685---91.
27.CabayRJ,MortonTH,EpsteinJB.Proliferativeverrucous leuko-plakiaanditsprogressiontooralcarcinoma:a reviewofthe literature.JOralPatholMed.2007;36:255---61.
29.Batsakis JG, Suarez P, El-naggar AK. Proliferative verrucous leukoplakiaanditsrelatedlesions.OralOncol.1999;35:354---9.
30.Torres-RendonA, RoyS, Craig GT, SpeightPM.Expression of Mcm2,gemininandKi67innormaloralmucosa,oralepithelial dysplasiasandtheircorrespondingsquamous-cellcarcinomas. BrJCancer.2009;100:1128---34.
31.Pitiyage G, Tilakaratne WM, Tavassoli M,Warnakulasuriya S. Molecularmarkersinoralepithelialdysplasia:review.JOral PatholMed.2009;38:737---52.
32.GouvêaAF,VargasPA,ColettaRD,JorgeJ,LopesMA. Clinico-pathologicalfeaturesandimmunohistochemicalexpressionof p53,Ki-67,Mcm-2andMcm-5inproliferativeverrucous leuko-plakia.JOralPatholMed.2010;39:447---52.
33.YuYH,MoralesJ,FengL,LeeJJ,El-NaggarAK,VigneswaranN. CD147andKi-67overexpressionconferspoorprognosisin squa-mouscellcarcinomaoforaltongue:atissuemicroarraystudy. OralSurgOralMedOralPatholOralRadiol.2015;119:553---65.
34.AkrishS,Ben-IzhakO,SaboE,RachmielA.Oralsquamouscell carcinomaassociatedwithproliferativeverrucousleukoplakia comparedwithconventionalsquamouscellcarcinoma----a clin-ical,histologicandimmunohistochemicalstudy.OralSurgOral MedOralPatholOralRadiol.2015;119:318---25.
35.KrestyL,MallerySR,KnoblochTJ,LiJ,LloydM,CastoBC,etal. Frequentalterationsofp16INK4aandp14ARFinoral prolifera-tiveverrucousleukoplakia.CancerEpidemiolBiomarkersPrev. 2008;17:3179---87.
36.Carrard V, BrounsE, Vander WaalI. Proliferative verrucous leukoplakia;acriticalappraisalofthediagnosticcriteria.Med OralPatolOralCirBucal.2013;18:411---3.