www.jped.com.br
ORIGINAL
ARTICLE
Cardiac
dysfunction
and
ferritin
as
early
markers
of
severity
in
pediatric
sepsis
夽
,
夽夽
Cristian
T.
Tonial
a,b,∗,
Pedro
Celiny
R.
Garcia
a,b,c,
Louise
Cardoso
Schweitzer
d,
Caroline
A.D.
Costa
b,
Francisco
Bruno
a,
Humberto
H.
Fiori
b,e,
Paulo
R.
Einloft
a,
Ricardo
Branco
Garcia
f,
Jefferson
Pedro
Piva
g,haPontifíciaUniversidadeCatólicadoRioGrandedoSul(PUCRS),HospitalSãoLucas,UnidadedeTerapiaIntensiva,PortoAlegre,
RS,Brazil
bPontifíciaUniversidadeCatólicadoRioGrandedoSul(PUCRS),ProgramadePós-Graduac¸ãoemPediatriaeSaúdedaCrianc¸a,
PortoAlegre,RS,Brazil
cConselhoNacionaldeDesenvolvimentoCientíficoeTecnológico(CNPq),BolsistadeProdutividadeemPesquisa,Brazil
dPontifíciaUniversidadeCatólicadoRioGrandedoSul(PUCRS),HospitalSãoLucas,Servic¸odeCardiologiaPediátrica,Porto
Alegre,RS,Brazil
ePontifíciaUniversidadeCatólicadoRioGrandedoSul(PUCRS),HospitalSãoLucas,UnidadedeTerapiaIntensivaNeonatal,
PortoAlegre,RS,Brazil
fCambridgeUniversityHospitalsNHSTrust,PediatricIntensiveCareUnit,Cambridge,UnitedKingdom
gHospitaldeClínicasdePortoAlegre(HCPA),UnidadedeTerapiaIntensivaPediátrica,PortoAlegre,RS,Brazil
hUniversidadeFederaldoRioGrandedoSul(UFRGS),ProgramadePós-Graduac¸ãoemSaúdedaCrianc¸aeAdolescente,Porto
Alegre,RS,Brazil
Received7April2016;accepted9August2016 Availableonline24January2017
KEYWORDS
Sepsis; Septicshock; Echocardiogram; Outcome;
Pediatricintensive careunit
Abstract
Objective: The aim ofthisstudy was toverify theassociation ofechocardiogram,ferritin,
C-reactiveprotein,andleukocytecountwithunfavorableoutcomesinpediatricsepsis.
Methods: AprospectivecohortstudywascarriedoutfromMarchtoDecember2014,with
pedi-atriccriticalcarepatientsagedbetween28daysand18years.Inclusioncriteriawerediagnosis ofsepsis,needfor mechanicalventilationfor morethan48h,andvasoactivedrugs. Serum levelsofC-reactiveprotein,ferritin,andleukocytecountwerecollectedonthefirstday(D0), 24h(D1),and72h(D3)afterrecruitment.Patientsunderwenttransthoracicechocardiography todeterminetheejectionfractionoftheleftventricleonD1andD3.Theoutcomesmeasured
夽
Pleasecitethisarticleas:TonialCT,GarciaPC,SchweitzerLC,CostaCA,BrunoF,FioriHH,etal.Cardiacdysfunctionandferritinas earlymarkersofseverityinpediatricsepsis.JPediatr(RioJ).2017;93:301---7.
夽夽
StudycarriedoutatPontifíciaUniversidadeCatólicadoRioGrandedoSul(PUCRS),PostgraduatePrograminPediatricsandChildHealth, PortoAlegre,RS,Brazil.
∗Correspondingauthor.
E-mail:cristiantonial@gmail.com(C.T.Tonial).
http://dx.doi.org/10.1016/j.jped.2016.08.006
werelengthofhospitalstayandinthepediatricintensivecareunit,mechanicalventilation duration,freehoursofVM,durationofuseofinotropicagents,maximuminotropicscore,and mortality.
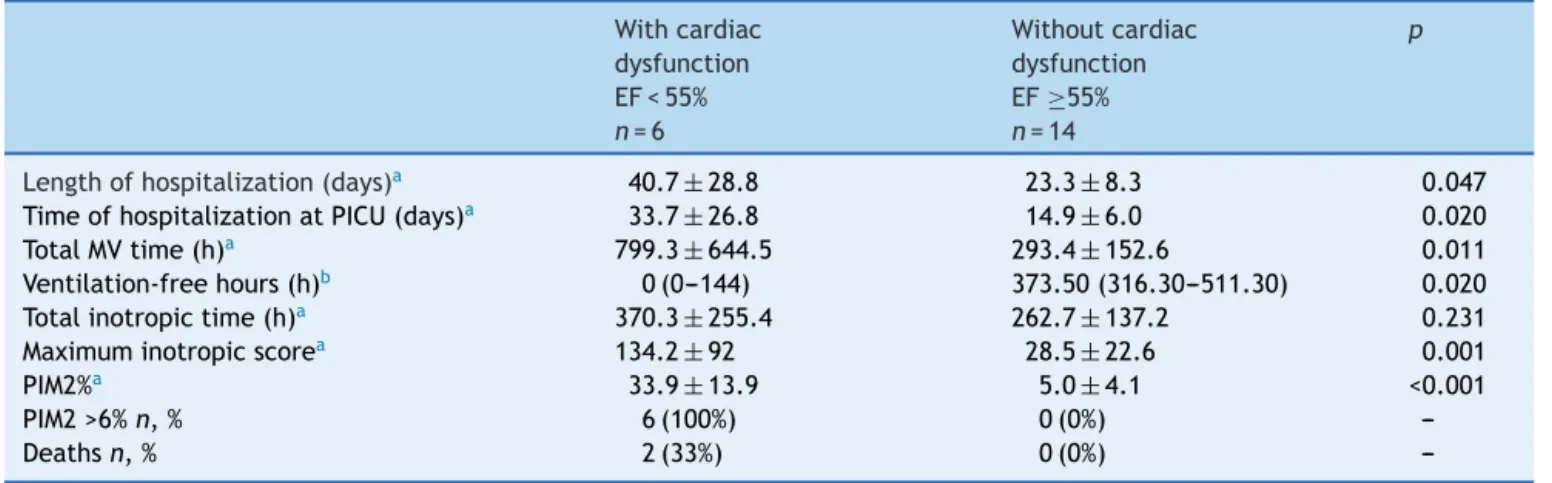
Results: Twentypatientscompletedthestudy.PatientswithelevatedferritinlevelsonD0had
also fewerventilator-freehours(p=0.046)andhighermaximum inotropicscore (p=0.009). PatientswithcardiacdysfunctionbyechocardiogramonD1hadlongerhospitalstay(p=0.047), pediatric intensivecareunitstay(p=0.020),durationofmechanicalventilation(p=0.011), maximuminotropicscore(p=0.001),andfewerventilator-freehours(p=0.020).
Conclusion: Cardiacdysfunctionbyechocardiographyandserumferritinvaluewassignificantly
associatedwithunfavorableoutcomesinpediatricpatientswithsepsis.
©2017SociedadeBrasileiradePediatria.PublishedbyElsevierEditoraLtda.Thisisanopen accessarticleundertheCCBY-NC-NDlicense(http://creativecommons.org/licenses/by-nc-nd/
4.0/).
PALAVRAS-CHAVE
Sepse;
Choqueséptico; Ecocardiograma; Desfecho;
UnidadedeTerapia IntensivaPediátrica
Disfunc¸ãocardíacaeaferritinacomomarcadoresprecocesdegravidadenasepse pediátrica
Resumo
Objetivo: Verificaraassociac¸ãodoecocardiograma,daferritina,daProteínaCReativa(PCR)
edacontagemdeleucócitoscomdesfechosdesfavoráveisnasepsepediátrica.
Métodos: Estudo de coorte prospectivo, no período de marc¸o a dezembro de 2014, com
pacientescríticospediátricosde idadeentre28 diase18anos. Critériosdeinclusãoforam diagnósticodesepse,necessidadedeventilac¸ãomecânica(VM)pormaisde48horaseusode drogasvasoativas.Avaliaram-seosníveis séricosPCR,ferritina, contagemde leucócitos,no recrutamento(D0),24horas(D1)e72horas(D3)apósorecrutamento.NoD1enoD3todos pacientesforamsubmetidosaecocardiogramatranstorácicoparadeterminac¸ãodaFrac¸ãode Ejec¸ão(FE)doventrículoesquerdo.Osdesfechosavaliadosforamtempodeinternac¸ão hospi-talarenaUnidadedeTerapiaIntensivapediátrica(UTIP);durac¸ãodaVM;horaslivresdeVM; durac¸ãodousodeinotrópicos;escoredeinotrópicosmáximoemortalidade.
Resultados: Vintepacientescompletaramoestudo.FerritinaelevadanoD0associou-secom
menortempolivredeventilac¸ão(p=0,046)emaiorescoredeinotrópicosmáximo(p=0,009). Adisfunc¸ãocardíacapeloecocardiogramanoD1relacionou-secommaiortempodeinternac¸ão hospitalar(p=0,047),deUTIP(p=0,020),VMtotal(p=0,011),escoredeinotrópicosmáximo (p=0,001)emenortempolivredeVM(p=0,020).
Conclusão: Adisfunc¸ãocardíacapeloecocardiogramaeovalordeferritinaséricaassociaram-se
significativamentecomdesfechosdesfavoráveisnospacientespediátricoscomsepse. ©2017SociedadeBrasileiradePediatria.PublicadoporElsevierEditoraLtda.Este ´eumartigo OpenAccesssobumalicenc¸aCCBY-NC-ND(http://creativecommons.org/licenses/by-nc-nd/4.
0/).
Introduction
Sepsisremainsanimportantcauseofmorbidityand mortal-ityinthepediatricintensivecareunit(PICU)environment. Findingtoolsthatcananticipateormonitorunfavorable evo-lutioninsepsiscancontributetotheimprovementofcare inthesecritically-illpatients.1,2
Thus,severalbiologicalmarkershaverecentlybeen stud-ied as tools to evaluate disease progression in bacterial infections,sepsis,andsepticshock.1---8Amongthe biomark-ers,themostoftenusedintheauthors’settingareleukocyte count,C-reactiveprotein(CRP),andferritinlevels,thelast twohavinglimited studiesin pediatricscorrelating serum levelswithunfavorableoutcomes.1,4,6---8
In pediatric sepsis, myocardial dysfunction is one of the main causes of clinical deterioration.9 Myocardial
dysfunctionmaybepresentinupto50%ofcasesofsevere sepsisorsepticshock,causingsystolicordiastolic ventric-ulardysfunctionandcontributingtoshockandmortality.10 Theechocardiogramisalreadyusedinthemanagementof patients withseptic shock duringvolumetricresuscitation andtochoosethebestvasoactivedrug.11,12Itisspeculated thatevaluationsobtainedbyechocardiographicassessment canbeusedasmarkersofsepsisevolution.Additionally,few studies have associated these measures with unfavorable outcomesinpediatricsepsis.13
Methods
This prospective cohort study wasdeveloped at the PICU ofHospitalSãoLucasofPontifíciaUniversidadeCatólicado RioGrandedoSul(PUCRS),locatedinPortoAlegre,stateof RioGrandedoSul,southernBrazil,fromMarchto Decem-ber 2014. This unit receives patients aged 28 days to 18 yearswithclinicalandsurgicaldiseasesandhas12bedsfor hospitalization.
All patients hospitalized during the abovementioned periodwhorequiredmechanical ventilation(MV)for more than48husingcardiovascularsupport(exceptfordopamine at a dose <5mcg/kg/min) and who had clinical diagno-sisor suspicionof sepsiswereincluded. Exclusioncriteria were: congenitalheart disease, presence of confirmed or suspected endocrine disease involving the somatotropic and corticotropic axes, need for hemofiltration or any other renal replacement therapy, diagnosis of congenital or acquired immunosuppression, confirmed or suspected congenital glucose metabolism alterations, severe liver impairment,pretermbirth,andweight<4kg.
Sepsis was defined asthe presence of two or more of the following four criteria: tachycardia, tachypnea, tem-peraturechange,leukocytosis,orleukopeniaforageinthe presenceofconfirmedor suspectedinfection.The organic dysfunctionswereclassifiedaccordingtoGoldsteinetal.14 Thepresenceoftwoormoreorganicdysfunctionswas con-sideredasmultiple-organdysfunctionsyndrome.
AllpatientsinthestudyhadtheirserumlevelsofCRP, fer-ritin,andleukocytecountsassessedatstudyentry(D0),24h (D1),and72h(D3)afterrecruitment.Thesamplewas strat-ified accordingtoCRPvalues(greater than7.6mg/dL and 16.2mg/dL),2ferritin(≥300ng/mL),15andleukocytecount (<5000/Land>15,000/L)forassociationwithoutcomes. On D1 and D3, all patients underwent transthoracic echocardiography to determine left ventricular ejection fraction(EF).TheEFrepresentstheejectedvolume,in per-centage,oftheleftventricularend-diastolicvolume,i.e., howmuchblood is ejected intothe aortaat systole. The Teichholz formula was used and cardiac dysfunction was consideredwhentheEFwas<55%.16
The left ventricular shortening fraction wasalso mea-sured,usingthesameformula,inallpatients.The results obtained were overlapping; therefore, it was decided to use only the EF in the statistical analyses. The device usedwasthe SiemensAcuson Cypress(Siemens®, Munich, Germany), witha 3MHz transducer.All assessments were performedusingthesamedeviceandbythesamepediatric cardiologist, with experience in the Pediatric Cardiology Service of the Hospital São Lucas of PUCRS. Each exami-nation had three consecutive measurements to minimize the effect of respiratory variation, mainly caused by mechanical ventilation. Kappa value was calculated to evaluatetheintraobserveragreementandaKappaof0.80 wasconsideredacceptable.
Thefollowingoutcomeswereevaluated:lengthof hospi-talstay(days),lengthofstayinthePICU(days),timeoftotal MV(hours),timewithoutMV(hours),totaltimeofinotropic use,maximuminotropicscore,andmortality.
To calculate the time without MV, a maximum of 28 daysofmechanicalventilation(672h)wereconsidered,i.e., thevaluecorrespondingtothenumberof hoursfreefrom
mechanical ventilation wascalculated by subtracting the time of total mechanical ventilation (hours) from 672h. Ifthepatientremainedmore than672h withMV,a value equaltozerowasconsidered.17Forthemaximuminotropic score,thehighestvalue,obtainedonanydayofthestudy, was calculated through a summation obtained from the formula: dose of dopamine+dobutamine+(epinephrine× 100)+(noradrenaline×100)+(milrinone×10). All of them were expressed in mcg/kg/min.18 The Pediatric Index of Mortality2(PIM2)wascalculatedonthefirstdayofthePICU, accordingtotheroutineofthisservice.19APIM2valueof6% waschosenasthecutoffpointforseverity,asitistheupper limitofhistoricalmortalityinthisservice.
Regarding the statistical analysis, the numerical data wereexpressedinabsolutevaluesandpercentages. Demo-graphic data such as age, weight, gender, type of organ dysfunction,presenceofinfection,andoriginofthepatient wereobtainedthroughtheelectronicmedicalrecord.The Kolmogorov---Smirnov test was used to verify sample nor-mality, with a sample being considered normal when the value was >0.05. Qualitative (categorical) variables were expressedasabsolutevaluesandpercentages,andwhenthe samplewasstratified,thegroupswerecomparedusing Pear-son’s chi-squared test or Fisher’s exact test. Quantitative variables were expressed as mean and standard devia-tion, and those with asymmetric distribution, as median andinterquartilerange(IQR). Whenthesamplewas strat-ified, the groups were compared using Student’s t-test or ANOVA for variables with normal distribution and the Mann---Whitney---WilcoxonorKruskal---Wallistestforvariables withnon-normaldistribution.Valuesofp<0.05were consid-eredsignificant.DataanalysiswasperformedusingtheIBM StatisticalPackagefor Social Sciences (IBMSPSSStatistics 20).
Thisstudywasapprovedbytheresearchethics commit-tee of Hospital São Lucas of PUCRS, under No. 474,050, issuedon11/27/2013.Authorizationwasrequestedto par-ticipateinthestudythroughaninformedconsentfromthe parentsorguardiansofalltherecruitedpatients.
Results
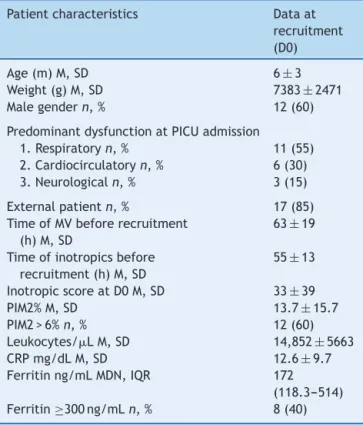
There were 337 hospitalizations during the recruitment periodand,ofthese,41patientswereeligibleforthestudy. Parentalconsentwasnotgrantedinfourcasesandonechild diedbeforethestartoftheexamination.Ofthe36whohad samplescollected,eightchildrenwereexcludedafterthey failedtocomplete the echocardiographic study and eight wereexcluded duetoerror,loss,orinsufficient collection ofsome ofthe study material.The remaining20 children completedtheprotocol.Therewerenobaselinedifferences incharacteristics,severitymeasuredbyPIM2,andmortality betweentheexcludedpatientsandthoseremaininginthe study.The generalcharacteristics of thestudy population aredescribedinTable1.
Table 1 Overall characteristics of the sample at recruitment.
Patientcharacteristics Dataat recruitment (D0)
Age(m)M,SD 6±3
Weight(g)M,SD 7383±2471
Malegendern,% 12(60)
PredominantdysfunctionatPICUadmission
1.Respiratoryn,% 11(55)
2.Cardiocirculatoryn,% 6(30) 3.Neurologicaln,% 3(15)
Externalpatientn,% 17(85) TimeofMVbeforerecruitment
(h)M,SD
63±19
Timeofinotropicsbefore recruitment(h)M,SD
55±13
InotropicscoreatD0M,SD 33±39
PIM2%M,SD 13.7±15.7
PIM2>6%n,% 12(60)
Leukocytes/LM,SD 14,852±5663
CRPmg/dLM,SD 12.6±9.7
Ferritinng/mLMDN,IQR 172
(118.3---514) Ferritin≥300ng/mLn,% 8(40)
NormalityverifiedbytheKolmogorov---Smirnovtest.
m,months;g,grams;M,mean;MDN,median;IQR,interquartile range;n,number;h,hours;%,percentage;SD,standard devia-tion;MV,mechanicalventilation;D0,dayzero;PIM2,pediatric indexofmortality2;CRP,C-reactiveprotein.
werehigheramongthemostseverecases(meanand stan-darddeviation:454.4±309.7vs.91.9±6ng/mL;p=0.005).
Cardiacoutput(EF)
Allpatientsweresubmittedtoechocardiogramonthefirst andthirdstudy daysafterrecruitment. Overall,EF values increasedin a discreteand non-significant manner during thestudyinterval.Sixpatients(30%)hadEF<55%, charac-terizingcardiacdysfunction.Ofthese,two(10%)recovered cardiacfunctiononD3.Patientswithcardiacdysfunctionon thefirstdayhadhigherPIM2atthePICUadmissionandhad a significant association with unfavorable outcomes. Two patientsfromthisgroupdied(Table2).
Evolutionofinflammatorymarkers
Inflammatorymediatorswereelevatedatrecruitmentand showeddifferentpatternsthroughoutthestudy.Ferritinwas withinnormal limits in most patients, withno significant decreaseonD3.CRPlevelswereextremelyhighat recruit-mentanddecreasedsignificantly,butstillshowedabnormal levelsonD3.Totalleukocytesremainedelevatedthroughout thestudyperiod(Table3).
Patientswithhyperferritinemia(≥300ng/mL)at recruit-ment(D0)hadmoreseverediseaseonthefirstdayatthe PICU(higher PIM2)andhad the worstoutcomes. The two patientswhodiedbelongedtothisgroup(Table4).
Discussion
This was one of the few cohort studies that jointly ana-lyzed sepsis biomarkers, echocardiogram measurements, evolution,andoutcomesincriticallyillpediatricpatients. The inclusion criteria were strict; all patients were on mechanicalventilationforatleast48handrequired vasoac-tive drugsupport. PIM2washigherthan6% in12 patients (60%), indicating high severity of the recruited individu-als. Themortalityratewas10%,whichis compatiblewith the literature.18,20 The present study demonstrated a sig-nificant associationbetweenlowcardiacsystolicfunction, representedbyEF,andhyperferritinemiawithunfavorable outcomes.
Cardiacdysfunctioninpediatricsepsisisawidelyknown, butnotyetfullyunderstoodcondition.9Thefindingofleft ventricularcardiacdysfunctioninsepticshock (lowEF) of 30% is consistent with studies recently published by Raj etal.,37%;Pulidoetal.,27%;andFurianetal.,33%.9,21,22 The last twoauthors did not findan association between lowEFandunfavorableoutcomesormortalitywhen study-ingadultpatients.However,Carmonaetal.foundincreased mortalityinpediatricpatientswithsepticshockthathadan EF <45% on the firstday of PICU admission, a result sim-ilar to that of the present study.13 None of these studies associatedcardiacdysfunctionmeasured byEF withother clinicaloutcomes.Apossibleexplanationforthesefindings isthatcardiacdysfunction,inseveresepsisorsepticshock, hasagreaterinfluenceontheclinicalpictureof pediatric patientswhencomparedtothatofadultpatients,who pre-dominantly have vasoplegic shock.9,10 Thus, patients who arealreadyreceivingoptimizedinotropictherapyandstill havecardiacdysfunctionwilltendtohaveaworseoutcome. Ferritin was the most prominent inflammatory marker in this study. It is an iron-storing protein,responsible for releasing it in a controlled manner. In inflammatory pro-cesses,agreatproductionofthisproteinoccurs,inducing a decreasein serumiron,believed tominimizethe avail-ability of irontomicroorganisms.Forthis reason,ferritin incriticallyillpediatricpatientsmaybeelevated,anditis associatedwithseverityinsomediseases.6---8Themortality rateinpatientswithferritin>3000ng/mLis3-foldhigher.8
Inthepresentstudy,40%ofthepatientshadhighlevels of this biomarker on D0. When the sample was strati-fied into two groups using the 300ng/mL cutoff point, a significantassociationbetweenhyperferritinemiaand unfa-vorableoutcomeswasobserved,suchasfewermechanical ventilation-freehoursandhighermaximuminotropicscore. Additionally, the two patients who died belonged to this group.Garciaetal.hadpreviouslyassociatedferritin lev-els>500ng/mLwithmortality.6Sustainedhyperferritinemia or very high values of this marker represent an intense inflammatory responsescenario thatshould bebeneficial, butseemstobeanindicatorofunfavorableoutcomes.7The present study used a cut-off point of 300ng/mL, since in apreviousstudybyLaksandGarcia,15 thiswastheclosest medianvalue inpatientswithsepticshock.The reduction ofthecutoffpointto300ng/mLaccentuatestheresultsof thisstudy.
Table2 Cardiacdysfunctionbyechocardiogramonthefirstday(D1)post-recruitmentandoutcomes.
Withcardiac dysfunction EF<55%
n=6
Withoutcardiac dysfunction EF≥55%
n=14
p
Lengthofhospitalization(days)a 40.7±28.8 23.3±8.3 0.047
TimeofhospitalizationatPICU(days)a 33.7±26.8 14.9±6.0 0.020
TotalMVtime(h)a 799.3±644.5 293.4±152.6 0.011
Ventilation-freehours(h)b 0(0---144) 373.50(316.30---511.30) 0.020
Totalinotropictime(h)a 370.3±255.4 262.7±137.2 0.231
Maximuminotropicscorea 134.2±92 28.5±22.6 0.001
PIM2%a 33.9±13.9 5.0±4.1 <0.001
PIM2>6%n,% 6(100%) 0(0%)
---Deathsn,% 2(33%) 0(0%)
---NormalityverifiedbytheKolmogorov---Smirnovtest.
n,number;h,hours;%,percentage;MV,mechanicalventilation;PIM2,PediatricIndexofMortality2.
a Valuesexpressedasmeanandstandarddeviation. b Valuesexpressedasmedianandinterquartilerange.
Table3 Ferritin,CRP,andleukocytecountatD0,D1,andD3.
Dayzero Day1 Day3 p
Ferritin,ng/mLa 172(118.3---514.0)c 173.9(109.8---617)c 158.9(77.8---361.9)c 0.939
CRP,mg/dLb 12.6±9.7c 8.8±6.5d 3.5±1.8e <0.001
Leukocytes/Lb 14,852±5663c 16,874±9599c 15,672±6197c 0.684
a Valuesexpressedasmedianandinterquartilerange. b Valuesexpressedasmeanandstandarddeviation.
c,d,eThesameletterindicatesnodifferencebetweenthegroups.NormalitywasverifiedbytheKolmogorov---Smirnovtest.
CRP,C-reactiveprotein.
Table4 Hyperferritinemiaatrecruitment(D0)andoutcomes.
Ferritin≥300ng/mLn=8 Ferritin<300ng/mLn=12 p
Lengthofhospitalization(days)a 35.5±26.4 23.8±8.4 0.166
TimeofhospitalizationatPICU(days)a 28.6±24.7 15.1±6.1 0.084
TotalMVtime(h)a 664.0±604.1 299.3±154.1 0.058
Ventilation-freehours(h)a 175.5±258.2 372.6±157.1 0.046
Totalinotropictime(h)a 322.3±240.3 276.8±136.7 0.594
Maximuminotropicscorea 108.6±92.2 27.9±23.1 0.009
PIM2(%)a 28.5±15.5 3.8±3.0 <0.001
PIM2>6%n,% 8(100) 4(33.3) 0.001
Deathsn,% 2(25) 0(0)
---n,number;h,hours;%,percentage;MV,mechanicalventilation;PIM2,PediatricIndexofMortality2. NormalityverifiedbytheKolmogorov---Smirnovtest.
a Valuesexpressedasmeanandstandarddeviation.
inflammatoryresponsesyndrome(SIRS),sepsis,severe sep-sis, and septic shock.2 Similarly to Rey, in the present study,CRPat recruitmentwaselevated asin septicshock (12.6±9.7mg/dL), and showeda significant reduction on subsequentdays.OnD3,patientsstillhadabnormalvalues ofthisbiomarker(3.5±1.8mg/dL).However,therewasno associationbetweenthehighestvaluesofCRPfoundinthis sampleandunfavorableoutcomes.
StudiesthatstratifyCRPvaluesinsepticshockin pedi-atricpatientsarescarce.Leukocytecountwasnotusefulas amarkerofseverityeither,asitsvalueremainedconstant.
Initially, for leukocyte analysis, the authors used normal valuesasreference,aslimit valueswerenotfound inthe literaturethatdefinedprognosisforthismarker.Some stud-ieshavealreadydemonstratedthelowvalidityofleukocyte count as a diagnostic and prognostic marker in pediatric sepsis.2,23
Study
limitations
professional-dependentassessment.This methodwas cho-sen,despite itslimitations,becauseitisavailableinmost PICUservicesinBrazil.ThesecondistheuseofPIM2asan outcome,representingaprognosticindexindicating mortal-ity.Patientswithcardiacdysfunctionandhyperferritinemia hadhigher PIM2.Considering that PIM2is used in patient populationstoestimatemortality,thefindingofthe associ-ationofthismeasureofseveritywithbiomarkersallowsan interestingapplicationofthisindex,whichiswidelyusedin BrazilianPICUs.
Thethirdisthelackofotherbiomarkersalreadystudied inpediatricsepsis.Itwasdecidedtostudytheonesthatare easilyobtainedandmostcommonlyusedinBrazil.Finally, thenumberofpatientswasalimitation.Theauthors stud-iedan expressivegroup of verysevere patients, in whom theinclusionandexclusioncriteriawerestrict.Thesample, whileproducingsignificantdifferencesinresults,hadalow statisticalpower.
In brief, cardiac dysfunction by echocardiogram (EF<55%)onD1andserumferritinvalues(≥300ng/mL)on DO,obtainedinpediatricpatientswithsepsisadmittedto the PICU, were significantly associated with unfavorable outcomes.
Funding
Conselho Nacional de Desenvolvimento Científico e Tec-nológico (CNPq), whose funding wasapproved by process No.485488/2011-6---ResearchProjectSupport---Universal 14/2011.
Conflicts
of
interest
Dr.Pedro Celiny R. Garcia has a grant fromCoordenac¸ão de Aperfeic¸oamento de Pessoal de Nível Superior (CAPES BRASIL).Theothersauthorsdeclarenoconflictsofinterest.
Acknowledgements
ToCAPES,forthesuppliedgrants,andtothePostgraduate PrograminPediatricsandChildHealthofPUCRS,forallowing theauthorstocarryoutthisstudy.
References
1.Simon L, GauvinF,Amre DK,LacroixJ. Serum procalcitonin and C-reactive protein levels as markers of bacterial infec-tion: a systematicreviewand meta-analysis.ClinInfect Dis. 2004;39:206---17.
2.Rey C, Los Arcos M, Concha A, Medina A, Prieto S, Mar-tinez P, et al. Procalcitonin and C-reactive protein as markers of systemicinflammatory response syndrome sever-ity in critically ill children. Intensive Care Med. 2007;33: 477---84.
3.TengChungT,HindsCJ.TreatmentwithGHandIGF-1incritical illness.CritCareClin.2006;22:29---40.
4.VilaPérezD,JordanI,EstebanE,García-SolerP,MurgaV,Bonil V,etal.Prognosticfactorsinpediatricsepsisstudy,fromthe SpanishSocietyofPediatricIntensiveCare.PediatrInfectDisJ. 2014;33:152---7.
5.VanLeeuwenHJ,HeeziusEC,DallingaGM,vanStrijpJA,Verhoef J,vanKesselKP.Lipoproteinmetabolisminpatientswithsevere sepsis.CritCareMed.2003;31:1359---66.
6.GarciaPC, LonghiF,BrancoRG,PivaJP, LacksD,TaskerRC. Ferritinlevelsinchildrenwithseveresepsisandsepticshock. ActaPaediatr.2007;96:1829---31.
7.Demirkol D, Yildizdas D, Bayrakci B, Karapinar B, Kendirli T, Koroglu TF, et al. Hyperferritinemia in the critically ill child with secondary hemophagocytic lymphohistiocyto-sis/sepsis/multiple organ dysfunction syndrome/macrophage activation syndrome: what is the treatment? Crit Care. 2012;16:52.
8.RaschkeRA,Garcia-OrrR.Hemophagocytic lymphohistiocyto-sis: a potentially underrecognized association with systemic inflammatory response syndrome, severe sepsis, and septic shockinadults.Chest.2011;140:933---8.
9.Raj S, Killinger JS, Gonzalez JA, Lopez L. Myocardial dys-function in pediatric septic shock. J Pediatr. 2014;164: 72---7.
10.SmedingL,PlötzFB, GroeneveldAB, KneyberMC.Structural changesoftheheartduringseveresepsisorsepticshock.Shock. 2012;37:449---56.
11.Deep A, Goonasekera CD, Wang Y, Brierley J. Evolu-tion of haemodynamics and outcome of fluid-refractory septic shock in children. Intensive Care Med. 2013;39: 1602---9.
12.Ranjit S, Kissoon N. Bedside echocardiography is useful in assessingchildrenwithfluidandinotroperesistantsepticshock. IndianJCritCareMed.2013;17:224---30.
13.CarmonaF,MansoPH,SilveiraVS,CunhaFQ,deCastroM, Car-lottiAP.Inflammation,myocardialdysfunction,andmortality inchildrenwithsepticshock:anobservationalstudy.Pediatr Cardiol.2014;35:463---70.
14.Goldstein B, Giroir B, Randolph A. International consensus conference on pediatric sepsis. International pediatric sep-sis consensus conference: definitions for sepsis and organ dysfunction in pediatrics. Pediatr Crit Care Med. 2005;6: 2---8.
15.Laks D [Thesis] Ferritina como marcador de resposta infla-matória sistêmica de crianc¸as criticamente doente. Porto Alegre(RS):ProgramadePós-Graduac¸ãoemMedicina/Pediatria eSaúde da Crianc¸a. PontifíciaUniversidade Católica do Rio GrandedoSul;2010.
16.LangRM,BierigM,DevereuxRB,FlachskampfFA,FosterE, Pel-likkaPA.Recommendationsfor chamberquantification.EurJ Echocardiogr.2006;7:79---108.
17.SchoenfeldDA,BernardGR, ARDSNetwork.Statistical evalu-ationofventilator-freedaysasanefficacymeasureinclinical trialsoftreatmentsforacuterespiratorydistresssyndrome.Crit CareMed.2002;30:1772---7.
18.BrierleyJ,CarcilloJA,ChoongK,CornellT,DecaenA,Deymann A, etal. Clinicalpractice parametersfor hemodynamic sup-portofpediatricandneonatalsepticshock:2007updatefrom theAmericanCollegeofCriticalCareMedicine.CritCareMed. 2009;37:666---88.
19.Slater A, Shann F, Pearson G, Paediatric Index of Mor-tality (PIM) Study Group. PIM2: a revised version of the Paediatric Index of Mortality. Intensive Care Med. 2003;29: 278---85.
20.ChoongK,BohnD,FraserDD,GabouryI,HutchisonJS,Joffe AR,etal.Vasopressininpediatricvasodilatoryshock:a multi-centerrandomizedcontrolledtrial.AmJRespirCritCareMed. 2009;180:632---9.
22.FurianT,AguiarC,PradoK,RibeiroRV,BeckerL,MartinelliN, etal.Ventriculardysfunctionanddilationinseveresepsisand septicshock:relationtoendothelialfunctionandmortality.J CritCare.2012;27,319.e9-e15.